PC SLIDES typical ppt
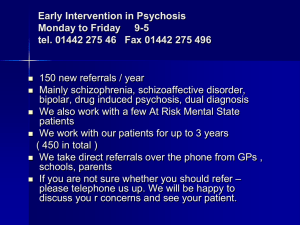
advertisement
Early psychosis: a journey into uncharted waters? A primary care view David Shiers Mo Vaillancourt Rory Byrne Royal Soc Medicine Workshop early detection of psychosis. Sept 16th 2008 Views from some young people attending the EDIT service you can’t even sleep at night, just there thinking someone is going to come, I thought I was in a movie, I’m dreaming, but it’s not a dream I don’t feel close to anyone. I don’t properly fit in anywhere. Alone in a crowd, that’s how I describe it I was just getting worse and worse, hearing noise, I even broke my radio in my bedroom, I just had enough… just can’t take it, I have to speak to someone Dr Kate Hardy (while a trainee psychologist with EDIT Greater Manchester West MH FT) Learning Objectives Gain insights from hearing some personal stories about the experience of psychosis Describe how a young person with an emerging psychosis or family member may present to a GP Understand the benefits of earlier detection and treatment of psychosis ‘Keep the body in mind’ – when thinking about the impact of emerging psychosis My GP ‘journey’ • Rare • Kraepelin’s Dementia Care Model ‘Schizophrenia is like managing the British empire: the orderly management of decline’ Anonymous Some GP views: “I know that I cannot look after people with severe and enduring mental health problems. I do not have the skills or the knowledge. I couldn't do it well" “Sometimes they have to be standing on a bridge before we can get people help and we have to exaggerate symptoms to get the psychiatrist’s attention at an earlier stage” Helen Lester BMJ 2005 Contrasting with patients’ views typified by: "I mean, the GP has to have some understanding of mental health but I don't expect my GP to know all of the issues to do with my illness…. …..I would though expect him or her to refer me to a specialist person. The important thing is that somebody is looking after you so it's not just you on your own. Helen Lester BMJ 2005 GPs see a FEP at an age when other serious mental disorders tend to develop Victoria (Aus) Burden of Disease Study: Incident Years Lived with Disability rates per 1000 population by mental disorder Was it just Mary? • North Staffs Pathways to Care prospective audit n = 45 (Macmillan, Ryles, Shiers & Lee 1998/9) • Sandwell GP interview n = 3 (Alderton 2000 ) • Worcester Pathways to Care retrospective audit n = 30 and GP workshop n = 26 (Smith 2000) • Walsall Pathways to Care review from case notes n = 18 (Rayne 2002) • Gloucester GP Postal questionnaire n = 15 (Davis 2002) Who are they? 50% < 24; youngest aged 13 Average age at onset = 21 75% live with parent(s) or spouse 41% are employed or in fulltime education Pathway players (n = 45) General psychiatrists Family members GP Police CPN A&E SW Psychologist Teacher / Tutor Neighbour Police surgeon Hostel staff Probation officer Prison staff Resource centre 45 37 36 22 18 13 11 5 4 4 4 4 3 3 3 Health visitor Work colleagues Private landlord Church Occupational health Friends OT General physician Learning diff psychiat Forensic psychiatrist Substance misuse Homeless services Solicitor Ambulance services Public Health 3 3 2 2 2 2 2 1 1 1 1 1 1 1 1 Symptoms presented to GPs? 7% - clear evidence of psychosis 37% - physical / somatic symptoms 50% report emotional and psychological changes 25% report changes in work and social functioning Help seeking? Q how did it feel going to a doctor about psychological problems? A. Emmm, bit weird at first, but on the other hand, they know, I thought, because they’ve had other people go in there before with problems Q. was there anybody you’d have spoken to about your psychological problems, confided in? A. Nah, not in my family, not even my nana, not even my Nana… “I’ll tell you why, cos you’ve not got a job, you’ve not got this, you sit in your room, smoking weed all day” …and she doesn’t understand but she’s oldschool me Nana Rory Byrne researched views EDIT Nature of their help-seeking to GP? Prodrome: typically 2 – 6 m ~ 50% seek help <2 wks of psychotic symptoms ~ 20% of individuals have courage to seek help themselves ~75% relied on family members to seek help on their behalf 5 contacts on average to achieve pathway to care GPs are first point of professional contact ~ 65% Plain sailing? • 7-15m treatment delays • Families’ concerns ignored • Dangers ahead • Outcome providential • Can be assisted DANGER AHEAD!!! Pressure wave- trapped • Crisis response – 73–80% hospitalised – 36–59% Mental Health Act – 45% police involved • 50% disengage: likely crisis reengagement • Relapse – 50% < 24m • Many just quietly drift… …. marooned to some backwater? “…can’t get a job, can’t get a girlfriend, can’t get a telly, can’t get nothing… it’s just everything falls down into a big pit and you can’t get out…” Hirschfeld, 2002 “…our overwhelming feeling was of an opportunity missed - to what degree she has been needlessly disabled by those first four years of care we’ll never know” Mother 2002 ….and a path to inequality Excluded 12% with a job In previous 2 weeks (Nithsdale survey) o 39% either had no friends or had met none o 34% had not gone out socially o 50% no interest or hobby other than TV one in four have serious rent arrears 3x divorce rate Dis-ease up to 25 years less life 33% suicide and injury o Lifetime suicide risk 10%; 2/ within first 5yrs, esp around the FEP 3 66% are premature deaths from physical causes o o o o 2-3x rate of CVS, Respiratory or infective disorders Lifestyle adverse factors: smoking; diet; activity Up to 5x rate of diabetes Poorer health care That’s the problem we are trying to solve Aims of EI services 1. Prevent psychosis in the ultra high risk individuals – identify and intervene on cusp of psychosis 2. Reduce DUP (Duration of Untreated Psychosis): – promote early detection & engagement by community agencies – Comprehensive initial mental health assessments & diagnosis 3. Optimise initial experience of acute care & treatment: – ‘Youth friendly’ Acute Home based/Hospital Treatment 4. Maximise recovery & prevent relapse during critical period: – – – – Provide outreach integrated bio/psycho/social interventions focus on functional/vocational as well as symptomatic recovery address co-morbidity and treatment resistance early Support carers and network of community support agencies Stages of Early Intervention in Psychosis Prodrome DUP Acute Recovery & Relapse prevention 88% recover 57% recover 32% recover 1st First episode of psychosis 16 Age 20 2nd 3rd 4th 82% relapse 78% relapse 86% relapse 24 Adapted from Robinson et al, 1999 What helps – some views of young people attending the EDIT service before I was just a jumbled mess – I was anxious, now I know why I’m anxious, what situations lead me to that, why those situations lead me to that, so it’s been a lot of help I do recognise that medication is only a short term solution and hopefully one day I won’t need it it’s a team and I’m part of that team you know, I’m just as important, I’m making decisions, after all I am the only one that knows about what’s going on in my own head Rory Byrne researched views EDIT Clinical Outcomes from Worcestershire EIS (Smith, 2006) National EIS (3y) 2003-6 n=78 12-18m 5-6m % admitted in FEP 80% 41% % FEP using MHA 50% 27% Readmission 50% 27.6% % engaged @ 12m 50% 100% (79% well engaged) Family involved satisfied 49% 56% 91% 71% 8-18% 55% 48% 21% 0% Duration of untreated psychosis Employed Suicide attempted completed Reflection Rapids PC Eddy Distressed Family crisis Family Youth worker Isolated from friends Drop out of Educ’n Suicide attempt Offending behaviour Mental illness Rapids Drugs No job Homeless Rapids No money Using Nature – Eddies Early detection of danger ahead • Pull ashore, get out, take a look and regroup • Use understanding of the nature of the journey and knowledge to stop and even regain some ground Family Eddy Guides White water Rapids Lookout with life ring Safety raft The hazards can be reduced and ultimately negotiated • Timely support. • Thorough preparation • Effective use of well developed evidencebased approaches – for both the young person – and their family. Celebrate and prepare • Have learnt something • Have a guide/mentor – Professional, family, friend or peer • Alert and ready for a next time? – Take remedial action – Seek help Supporting GPs’ to do a difficult job better: Early intervention is everybody’s business • EI psychosis services insufficient by themselves • GPs offer continuity, context and family practice: – Key role in care pathway of emerging psychosis – Listen and act on concerns of the family • Keep the body in mind. – Alongside practice nurses, GPs can be critical players in improving physical health pathways Equipped for the life ahead both for the young person and their family Acknowledgements to: Dr. Roy Morris Dunedin and Dr Maryanne Freer, Newcastle for contributing the white water rafting metaphor to Guzer.com for use of their video clips and to Paddy Power for slides 19 & 20 You don’t need an engine when you have wind in your sails Paul Bate 2004