THE COMMUNITY MENTAL HEALTH NURSES
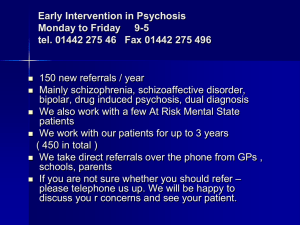
advertisement
THE COMMUNITY MENTAL HEALTH NURSES EXPERIENCES IN UTILISING RELAPSE PREVENTION FOR PERSONS WITH PSYCHOSIS ELIZABETH WYCHERLEY RPN, DipN, B.Sc, Post Grad Dip in Acute & Enduring Mental Health Problems Post Grad Dip in Psychosocial Intervention in Mental Health Care. Background It is understood that psychosis is associated with a diversity of contributing factors such as biological, psychological and social factors. Depending on the contributing factors, the length of the resulting psychosis can vary from hours to years (Sainsbury Centre for Mental Health, 2003). Psychosis has a cyclical nature and therefore most service users endure episodes of relapse and remission. Traditionally, persons with psychosis were predominantly treated with pharmacological interventions. However this has not been effective in all cases as there are high relapse rates in persons following their first episode of psychosis. Even though a therapeutic dose of anti-psychotic medication is essential, psychosocial interventions are also vital in order to reduce the risk of relapse. The provision of psychosocial interventions for persons with psychosis is recognised to be an important part of treatment (Brooker & Bradden, 2003). Nationally and internationally the effectiveness of psychosocial interventions have been supported and endorsed (Department of Health 2006, National Institute of Clinical Excellence, 2009) (NICE). Recommendations for Service Provision Psychosocial interventions for persons diagnosed with an enduring mental illness are viewed as being fundamental to the provision of a proficient and responsive mental health service. NICE (2009) recommends psychosocial interventions should be routinely implemented in the treatment of psychosis. Environmental stress and the individual’s vulnerability to mental distress could contribute to exacerbation of the person’s psychotic symptoms (Healy et al, 2006). The management of potential environmental stress may alleviate the chances of triggering the person’s psychotic symptoms. Programmes of family intervention were developed to reduce the risks of relapse of psychotic symptoms and re-hospitalisation, enhance the persons social functioning, curtail family burden and to increase quality of life for the family as a whole. Concordance with anti-psychotic medication is of utmost importance in preventing relapse in persons with psychosis (Harris, 2002). As previously discussed there is a high incidence of non-concordance of medication resulting in increased relapse rates and the “revolving door phenomenon” (Kemp et al, 1997). The provision of psychosocial interventions have been proven to be effective to enhance medication concordance in persons with psychosis. The aim of CBT for psychosis is to change the thoughts, behaviours and emotions of individuals by providing them with psycho-education on skills to confront and alter their beliefs, which they have regarding their symptoms. Managing emotional distress and environmental stress are important in preventing an exacerbation of psychotic symptoms. Therefore CBT is central to the management of psychotic symptoms. The purpose of relapse prevention is to educate the person who is working on changing their behaviour, preempt and manage the difficulties of the setback or relapse. The principles of relapse prevention are underpinned in the social learning theory, in that it comprises of a combination of behavioural skills, cognitive interventions and lifestyle adjustments. Relapse prevention strategies are paramount in the treatment of psychosis to promote early recognition and early intervention, alleviate distress and potential disability and enhance social inclusion. Proposed Study Aim: To explore the community mental health nurse’s experiences in utilising relapse prevention for persons with psychosis. Objectives: To examine current literature available on this area of interest. To explore the models of care that nurses provide in utilising relapse prevention. To consider any concerns, which arise for nurses in their provision of this intervention. Identification of any educational requirements in relation to relapse prevention for persons with psychosis. Design: A qualitative descriptive methodology will be applied to answer this research question. Up to eight community mental health nurses who work within one Health Service Executive region who meet the inclusion/exclusion criteria will be interviewed individually. It is proposed that interviews will be guided by a semi-structure, tape recorded, transcribed and analyses by utilising Burnard’s (1991) thematic content analysis. ADMISSIONS OF PERSONS WITH PSYCHOSIS IN NORTH LEE MENTAL HEALTH SERVICE 2005-2008 Year F23.x Admissions only 1st Admissions Male Female 2005 4 0 1 3 2006 6 2 2 4 2007 14 8 10 4 2008 21 12 13 8 F23.x Admissions by Age 0-15 years 16-17 years 18-35 years 36+ years Total 0 0 4 0 4 0 0 3 3 6 0 0 9 5 14 0 1 9 11 21 References Department of Health and Children (2006) A Vision for Change: Report of the Expert Group on Mental Health Policy, Dublin: Department of Health and Children. Harris, N., Williams, S., Bradshaw, T. (2002) Psychosocial interventions for people with schizophrenia: a practical guide for mental health workers, Hampshire: Palgrave Macmillan. Healy, H., Reader, D., Midence, K. (2006) ‘An introduction to and rationale for psychosocial intervention’ in Gamble, C., Brennan, G., eds., Working with serious mental illness: a manual for clinical practice, 2 nd ed., Edinburgh: Elsevier, 55-70. Kemp, R., Haywood, P., David, A. (1997) Compliance therapy manual, London: Bethlem and Maudsley NHS Trust. National Institute of Clinical Excellence (2009) Schizophrenia: core interventions in the treatment and management of schizophrenia in primary and secondary care, London: National Institute of Clinical Excellence. Sainsbury Centre for Mental Health (2003) A window of opportunity: a practical guide for developing early intervention in psychosis services, London: Sainsbury Centre for Mental Health.