Person-Centered Planning as a Tool for
Systems Transformation
Janis Tondora, Psy.D.
New Jersey Psychiatric Rehabilitation Association
Annual Conference, November 21, 2013
Person First Makes a Difference
Video clip…The Gestalt Project
http://www.youtube.com/watch?v=QficvVNIxTI&feature=youtu.be
Questions for Consideration
• What stood out for you in the clip and why?
• How did you feel emotionally MID-WAY through the clip? How
did you feel at the end?
• What did you learn? And how might this relate to personcentered recovery planning?
• What if YOU were defined largely by ONE part of yourself – a
part you really struggle with…maybe an illness, maybe a
difficult experience in your life. What if that was what others
focused on most all the time? What would that be like?
• Are these the types of “stories” of the whole person that you
tend to know about people you serve? If not, how can we use
PCP to know people in different kids of ways?
What we hope for THEM…
What we value for US…
Compliance with treatment
Life worth living
Decreased symptoms/Clinical stability
A spiritual connection to God/others/self
Better judgment
A real job, financial independence
Increased Insight…Accepts illness
Being a good mom…dad…daughter
Follows team’s recommendations
Friends
Decreased hospitalization
Fun
Abstinent
Nature
Motivated
Music
Increased functioning
Pets
Residential Stability
A home to call my own
Healthy relationships/socialization
Love…intimacy…sex
Use services regularly/engagement
Having hope for the future
Cognitive functioning
Joy
Realistic expectations
Giving back…being needed
Attends the job program/clubhouse, etc.
Learning
5
Beyond US and THEM
• People with mental health and addictions
issues generally want the exact same
things in life as ALL people.
• People want to thrive, not just survive…
• Recovery-oriented care challenges us to
move past the maintenance of clinical
stability to the true pursuit of
RECOVERY!
6
In other words…
• “You keep talking about getting me in the
‘driver’s seat’ of my treatment and my
life… when half the time I am not even in
the damn car!”
Person in Recovery as Quoted in CT DMHAS Recovery Practice Guidelines,
2005
7
Recovery-Oriented Care
…a fuzzy concept?
• Consumers demand it, public service
systems endorse it, medical and
professional programs are encouraged
to teach it, and researchers investigate
it. Yet, people struggle to understand
exactly what “It” is and what “It”
might look in practice.
• Tondora et al., 2005,
Implementation of PersonCentered Care and Planning: How
Philosophy Can Inform Practice
A Consumer and Family Driven System…
Recommendation 2.1
• The plan of care will be at the core of the consumercentered, recovery oriented system
• Providers should develop customized plans in full
partnership with consumers
The PLAN is a window of
opportunity to promote CONCRETE
recovery-practice change!
9
A Passing fad…flavor of the month?
10
The Person-Centered Train:
Who’s on Board?
National Perspective
IOM
CARF
JCAHO
AACP
Bazelon
12
ACA
First-Person Perspective
• It made such a huge difference to have my pastor there
with me at my planning meeting. He knows me better
than anyone else in the world and he had some great
ideas for me.
• I had been working on my recovery for years. Finally, it
felt like I was also working on my LIFE!
• When I have a voice in my own plan, I feel a
responsibility to “work it” in my recovery.
Person-centered planning
• is a collaborative process resulting in a recovery
oriented care plan
• is directed by persons in recovery in partnership
with care providers and natural supporters
• is reflected in the co-created written
Recovery Plan which outlines the
person’s most valued recovery goals
and how all will work together to
achieve them
14
Is it REALLY any different?
YES!
In the experience of the
persons served
when we “take stock” of
current planning
practices
and in the written
recovery plan itself…
Person-Centered Care Questionnaire: Tondora & Miller 2009
http://www.ct.gov/dmhas/lib/dmhas/publications/PCCQprovider.pdf
http://www.ct.gov/dmhas/lib/dmhas/publications/PCCQperson.pdf
And how do all the pieces come
together in the written recovery plan?
…and in a way that balances the spirit
of person-centered care with the rigor
required in clinical documentation?
Regulations
Required Paperwork
Medical Necessity
Compliance
Collaborative
Person-Centered
Strengths-based
Transparent
and in a way that doesn’t BURY us!!
“Apparently, Smith’s desk just couldn’t withstand the weight
of the paperwork we piled on his desk.”
Mr. Gonzalez, a 31-year-old married Puerto Rican man, is living with
bipolar disorder and a co-occurring addiction to alcohol that he
often uses to manage distressing symptoms. During a recent period
of acute mania, Mr. Gonzalez was having increasingly volatile
arguments with his wife in the presence of his two young sons. On
one occasion, he pushed his wife across the room that prompted
her to call the police. When the police arrived, Mr. Gonzalez was
initially uncooperative and upset. After he calmed down, Mrs.
Gonzalez agreed not to press charges, but insisted her husband
leave the house and meet with his clinician the following morning.
19
Mr. Gonzalez’s wife is actively involved in his recovery and
treatment, and she is open to reconciliation. However, she
made it clear that he would not be allowed to live at home,
or visit with his sons, until he “gets control of himself.” Upon
visiting the Community Mental Health Center the following
morning, Mr. Gonzalez tells his clinician repeatedly that his
love for his family and his faith in God are the only things
that keep him going when things are rough and he does not
know what he will do without them. More than anything, he
wants to be able to reunite with his family and be a good
role model for his sons. He feels that the only person who
understands this is the Center Peer Specialist with whom he
has a close relationship.
20
Snapshot: A Traditional Treatment Plan
• Goal(s):
• Achieve and maintain clinical stability; reduce assaultive
behavior; comply with medications; achieve abstinence
• Objective(s):
• Patient will attend all scheduled groups in program; patient
will meet with psychiatrist and take all meds as prescribed;
patient will complete anger management program; patient
will demonstrate increased insight re: clinical symptoms;
patient will recognize role of substances in exacerbating
aggressive behavior
• Services(s):
• Psychiatrist will provide medication management; Social
Worker will provide anger management groups; Nursing
staff will monitor medication compliance; Psychologist will
provide individual therapy
Uh, excuse me…
I’m here to return YOUR goals.
You left them on MY recovery plan!
• Comply with meds
• Stop drinking
• Reduce aggressive
behavior
• Increase insight
22
Recovery Goal:
I want to get my family back.
I don’t want the kids to ever be afraid of me.
Strengths to Draw Upon:
Devoted father; motivated
for change; supportive
wife; Catholic faith and
prayer are source of
strength/comfort; positive
connection to Center Peer
Specialist; intelligent
23
Barriers Which Interfere:
Acute symptoms of mania
led to violence in the home;
lack of coping strategies to
manage distress from
symptoms; abuse of alcohol
escalates behavioral
problems
23
Sample Short-Term Objective(s)
Within 30 days, Mr. Gonzalez will apply learned coping strategies
to have a minimum of two successful visits with wife and children
as reported by Mrs. Gonzalez in family therapy sessions.
Services & Other Action Steps
- Center doc to provide med management to reduce irritability & acute
manic sx
-Psychologist to provide family therapy sessions to discuss Mrs.
Gonzalez’s expectations and feelings re: future reunification
- Rehab Specialist to provide Communication and Coping Skills training to
teach/coach skills that will foster successful visits with wife and children
-Center chaplain to promote use of faith/daily prayer as a positive coping
strategy to manage distress
-Wellness Recovery Action Plan with Peer Specialist to promote daily
wellness through the use of24self-directed strategies
24
A More Hopeful Proposition…
• We can balance person-centered approaches
with medical necessity/regulations in creative
ways to move forward in partnership with
persons in recovery.
• We can create a plan that honors the person
and satisfies the chart!
• In other words: PCP is not soft!
What does all this mean for service
users and their loved ones?
• PCRP is about making sure the services
you receive help you achieve goals that are
important to YOU!
• Change is coming and
YOU can be a part of it!
• Consider today an
invitation to get involved
Systems Transformation:
Lessons learned from the field…
27
LL # 1: Nothing about us, without us
(REALLY!)
Primacy of meaningful
participation in ALL aspects of
system from design to delivery
to evaluation
Research showing we typically
UNDERESTIMATE consumers’ desire to be
involved (Chinman et al, 1999) – NH example
And… that consumer involvement often has the
single-most critical impact on recovery-oriented
systems transformation
28
• http://www.yale.edu/PRCH/documents/toolkit.draft.3.5.11.pdf
LL#2:
Listen & Respond To Common Concerns
1.
2.
3.
4.
5.
If given choice, people will make BAD ones
Payers won’t let us do this; regs prohibit this
The forms don’t have the right fields
Consumers aren’t interested/motivated
It devalues clinical expertise; violates professional
boundaries
6. Its what the clubhouse does…
7. Lack of time/caseloads too high
8. “My clients are sicker”
9. It doesn’t fit with focus on EBPs
10. Don’t we already do ROC?
Is this what’s on YOUR mind… in your way??
A Word of Caution…
“We want to include you in this decision without letting you affect it.”
LL # 3: Be clear on what
PCRP is NOT
PCRP is NOT an “add-on” or “special”
new program
•Avoid “initiative fatigue”
•Avoid “compartmentalizing” task of
transformation
•Rehab and peers are often natural
leaders but…
•Change must be embedded across
the organization as a whole!
The Person-Centered Plan as an
Integrating Framework for Quality in a
Changing Healthcare Climate
Incorporates
EBPS, including IMR
Encourages PeerBased Services
Maximizes SelfDetermination & Choice
Derived from a
Comprehensive
Assessment of Needs &
Strengths
Promotes Cultural
Responsiveness
Focuses on Natural
Supporters/Community
Settings
Informed by Stages of
Change & MI Methods
Respects Both Professional &
Personal Wellness Strategies
Emphasis on the
Attainment of
Meaningful
OUTCOMES
Consistent w/ Standards of
Fiscal & Regulatory Bodies,
e.g., CMS, JCAHO, CARF
33
LL # 3: Be clear on what
PCRP is NOT
PCRP is NOT “anti-clinical/anti-tx”
• PCRP respects the value of clinical expertise but also
emphasizes the value of lived experience
• There is a critical, but changed, role for practitioners
•
providers of hope
•
assessment / formulation
•
knowledge of the wide range of EBPs
•
…and emerging recovery/rehab practices
•
Skilled in practice of shared decision-making
•
knowledge of the illness and possible solutions
•
teachers/trainers/coaches
34
If the person is in the driver’s seat of
their care, where does that leave me?
•
PCRP is based on
a model of
PARTNERSHIP…
•
Respects the
person’s right to be
in the driver’s seat
but also recognizes
the value of
professional copilot(s) and natural
supporters
LL # 3: Be clear on what
PCRP is NOT
PCRP is NOT only for people who are “highfunctioning” or well on their way to recovery
Move beyond belief that some are
“too sick” to engage in recovery
Communicate a message of hope
and a belief that life can be
different
Understand sources of perceived
“resistance” or lack of motivation
Flex as needed/ be creative in how
we listen to/solicit preferences
Davidson, L, Harding, C., & Spaniol, L.
(Eds). (2006). Recovery from severe
mental illnesses: Research evidence
and implications for practice.
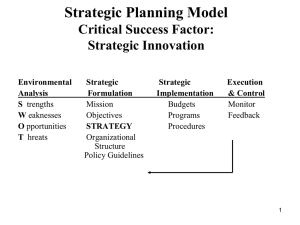
LL # 4: “Training” is necessary, but
not sufficient
Competency
knowledge, skills and abilities
Transformation
Change Model
Culture
Management
Project
Management
behavior and
attitude
work / business
flow
LL # 5: Attend to (real) external barriers
Competency
knowledge, skills and abilities
“When you pit a bad
Transformation
Change Model
system against a good
performer, the system
always wins…
(Rummler, 2004).
Culture
Management
Project
Management
behavior and
attitude
Work flow /
business practice
LL # 5: Attend to (real) external barriers
• Many administrators DO feel stuck between a
rock and a hard place… as they struggle to
reconcile (seemingly) competing tensions
• Clinical gate keeping vs.
direct access
• “Eligibility criteria” for voc
services
• Offering copies of plans
• Compliance and billing
issues
40
LL # 6: But, be prepared for red herrings
While attention to
organizational
factors is important,
sometimes this
EXTERNAL focus
can mask more
complex change
barriers…
41
People may resist change in subtle, and
“not-so-subtle” ways!
42
LL # 6: Be prepared for red herrings
• Based on misunderstanding, or biases/assumptions?
• Can’t do PCP because we won’t get paid for it…
• We aren’t allowed to give people a hard copy of
their plan because our Medical Records
department prohibits it…
• Peer staff can’t have access to confidential
material…
• Make it possible, see what happens, then hold
people accountable to deliver!
43
LL # 7: Different arguments
appeal to different audiences…
•Personal stories
•Outcomes data
•Values imperative
•Fiscal benefits of systems
transformation
What is the evidence behind PCRP?
Emerging research shows PCRP has a significant IMPACT
on OUTCOMES
• greater engagement in services as evidenced by reduced noshow rates & higher rates of medication adherence (Stanhope
et al., 2013)
• Significant improvements in wide range of recovery outcomes,
e.g., Sense of Community, positive coping, therapeutic
relationship with primary practitioner; QOL, self-esteem,
psychotic symptoms (Tondora et al, in press)
• New York Care Coordination Program*:
• 43% decrease in emergency room visits per
enrollee
• 44% reduction in days spent in a hospital
• 56% decrease in self harm among
• 51% reduction in harm to others
*http://www.carecoordination.org/results.aspx
What is the evidence behind PCRP?
Emerging evaluation data shows PCRP is COSTEFFECTIVE
• Comparison of Medicaid costs for Case Management and
ACT populations in WYCCP counties to same populations
in 6 comparison counties shows WNYCCP costs
significantly LOWER in:
• inpatient services; outpatient services; and community
support programs
• Enhanced employee
satisfaction led to significant
reductions in STAFF
TURNOVER and re-training
costs
LL # 8: Provide clarity in expectations
Promote increasing accountability among
providers and system as a whole
Provide a road-map for trainees/providers
who WANT to make changes, but are
unsure which direction to move
Help prioritize state training & consultation
objectives
Implications for range of HR protocols, e.g.,
hiring decisions
Educate consumers and families re: what
they can/should expect from the system
Manuscript available for download at:
www.ct.gov/dmhas/lib/dmhas/publications/practiceguidelines.pdf
http://www.ct.gov/dmhas/lib/dmhas/publications/practiceguidelines.pdf
LL # 9: SOME risk IS necessary at
individual and systems level
Is the system organized to perpetuate the
“status quo”
How tolerant of risk/change is the system as a
whole?
How is the burden of risk shared across all
stakeholders – including PIR?
Who is held accountable when things
don’t work out as planned?
Just as in individual recovery, taking risks
opens door to new opportunities!
49
“We’ve considered every potential risk
except the risks of avoiding all risks.”
LL # 10: Plan thoughtfully…don’t be
paralyzed by the pursuit of “perfection”
Many MH systems change efforts
get derailed by perpetual efforts
to help people “get it”
“We don’t think ourselves into a
new way of acting, we act ourselves
into a new way of thinking.”*
Sometimes you just have to dive in and do it/live it!!
My challenge to you: What is ONE thing you might
do different from this moment forward?
Miller, K. (2009). Stop Complaining and Do It!: The three phases of any transformation.
51
http://www.governing.com/column/stop-complaining-and-do-it
A Take Home Message:
We just need to stop accepting
what is and start creating
what should be
Dale DiLeo
For more information:
Janis Tondora:
janis.tondora@yale.edu