CHAPTER 5: The Integumentary System
advertisement
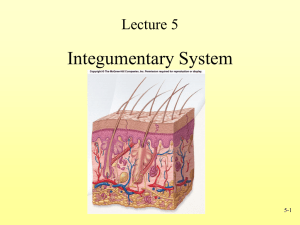
Chapter 5: The Integumentary System BIO 210 Lab Instructor: Dr. Rebecca Clarke Parts of the Integumentary System Cutaneous membrane (integument, skin) (outer) epidermis = superficial epithelium (inner) dermis = underlying area of connective tissues Accessory structures – located primarily in dermis, protrude through epidermis to skin surface Hair Nails (Multicellular) exocrine glands Also Blood vessels throughout dermis Sensory receptors – monitor touch, pressure, temperature, pain Integumentary System Cutaneous membrane = epidermis + dermis Figure 5–1 Layers (Strata) of Epidermis From basal lamina to free surface: stratum germinativum stratum spinosum stratum granulosum stratum lucidum stratum corneum Stratum Germinativum (Basale) Single layer of basal (germinative, stem) cells Site of cell division; replenishes epidermis Attached to basal lamina by hemidesmosomes Forms strong bond between epidermis and dermis Stratum Germinativum Forms epidermal ridges (Fig 5-2) fingerlike projections into dermis underneath; intermesh with dermal papillae ridge-shaped pattern (fingerprint) on surface of skin which is unique for each individual (genetically determined) (Fig 5-4) increase strength and bond between epidermis and dermis Has melanocytes (with melanin pigment) – give skin its color (Fig 5-5) Organization of the Epidermis Figure 5–2 Ridges and Ducts Figure 5–4 Stratum Spinosum “Spiny layer” cells shrink until cytoskeletons stick out (spiny) 8-10 cell layers of keratinocytes Dividing cells from stratum germinativum push up through this layer Still some cell division Stratum Granulosum “Grainy layer” 3-5 cell layers thick Cells stop dividing, start producing proteins grainy appearance keratin: tough, fibrous protein makes up hair and nails water resistant, not waterproof keratohyalin dense granules cross-link keratin fibers tightly interlocked cell layers Cells thinner, flatter, less permeable further from papillary plexus, start to die Stratum Lucidum “Clear layer” Cells flattened, densely packed, filled with keratin barrier to water Only in thick skin (on palms and soles) Stratum Corneum “Horn/hard layer” on exposed surface of skin 15-30 cell layers of dead cells (far from nutrients in dermis); durable, expendable protective function Cells filled with keratin (= keratinized) water-resistance (not waterproof) Cells tightly interconnected by desmosomes so are sloughed off in sheets Cells remain for 2 weeks (total of 6 weeks from origin in stratum germinativum to sloughing) 2 Kinds of Skin Thin skin Has 4 layers of keratinocytes (missing stratum lucidum) Covers most of body Thick skin Has all 5 layers of keratinocytes Covers heavily abraded body surfaces, e.g., palms of hands, soles of feet Dermis Located between epidermis and subcutaneous layer Contains Blood and lymph vessels Nerve fibers and sensory receptors Tactile (Meissner’s) corpuscles – sensitive to light touch; located in dermal papilla Lamellated (Pacinian) corpuscles – sensitive to deep pressure and vibration Accessory organs (of epidermal origin), e.g., hair follicles, sweat glands Components of Dermis 2 major components – boundaries indistinct Papillary layer Reticular layer Associated structures Papillary plexus = branching network of small arteries in papillary layer of dermis which provide blood to capillary loops that follow contours of epidermis-dermis boundary Papillary Layer Has dermal papillae projecting between epidermal ridges Consists of areolar tissue Contains smaller capillaries, lymphatics, and sensory neurons Reticular Layer Deep to papillary layer Consists of dense irregular connective tissue Contains Larger blood vessels, lymph vessels, and nerve fibers Collagen and elastic fibers Strength and elasticity Flexibility Dermatitis An inflammation of the papillary layer Caused by infection, radiation, mechanical irritation, or chemicals (e.g., poison ivy) Characterized by itch or pain Subcutaneous Layer aka hypodermis (“below dermis”), superficial fascia Highly vascularized – contains large arteries and veins; site of subcu injections Separates integument from deep fascia around other organs, e.g., muscles and bones Stabilizes position of skin relative to underlying tissues, e.g., skeletal muscles or other organs, while permitting independent movement Structure of Subcutaneous Layer Consists of Elastic areolar (loose) connective tissue Adipose tissue (energy reserve, shock absorber) Accessory Structures of the Integumentary System Derived from epidermis Located in dermis Extend through epidermis to skin surface Include: Hair follicles and hairs Exocrine glands Nails Structure of a Hair and Follicle Figure 5–10a Hair Follicles Living organs Produce “nonliving” hairs; complex process involving dermis and epidermis Extend deep into/through dermis and into underlying subcutaneous layer Wrapped in dense connective tissue sheath of dermis Follicle Wall Composed of epithelial cells Cells organized into 3 concentric layers (from outside in) Glassy membrane: Thickened basal lamina External root sheath: Widest layer Internal root sheath: Contacts cuticle (outer layer of hair) Structure of a Hair and Follicle Figure 5–10 Structure of a Hair Follicle Hair bulb Bulbous mass of epithelial cells Hair matrix Layer of epithelial cells in central, deepest part of follicle Site where cell division begins that produces hair Cells gradually pushed toward surface as hair gets longer Hair papilla At base of follicle (below matrix) “Peg” of connective tissue that contains capillaries and nerves If damaged, hair will not grow Structure of a Hair and Follicle Figure 5–10 Hair Structure Hair root Lower part of hair Begins at base of hair (bulb) and extends about halfway to skin surface Anchors hair into skin; Hair shaft Upper part of hair Extends from above the root to above the skin surface Structure of a Hair and Follicle Figure 5–10 Layers Within Hair Cuticle Outer surface Layer of overlapping, dead keratinized cells Contains hard keratin hair stiffness Cortex Intermediate layer below cuticle Also contains hard keratin Medulla Middle layer, central core Contains soft keratin Flexible Structure of a Hair and Follicle Figure 5–10 Associated Structures Arrector pili muscle Involuntary smooth muscle Contractions cause hairs to stand up “goose bumps” Exocrine Glands Sebaceous (oil) glands: holocrine glands secrete sebum Sweat (sudoriferous) glands: merocrine glands apocrine glands Types of Sweat Glands Apocrine: Associated with hair follicles Found in armpits, around nipples, and groin Merocrine: Widely distributed on body surface Especially on palms and soles Merocrine Sweat Glands Also called eccrine glands Smaller but more numerous Coiled, tubular glands Watery secretion = sensible perspiration (produced by glands) vs. insensible perspiration which is the loss of fluid by evaporation through the stratum corneum Nails Nonliving structures; made of dead cells packed with keratin Form on dorsal surface of tips of fingers and toes Function = protect fingers and toes Metabolic disorders can change nail structure, e.g., shape, appearance; can assist in diagnosis Nail Structure Nail body - Superficial, visible portion Nail bed – area of epidermis under nail body Nail root – epidermal fold not visible from surface; where nail production occurs Eponychium – extends over exposed nail forming cuticle Hyponychium – skin beneath free edge of nail Lunula (“moons”) pale crescent at base of nail where underlying blood vessels may be obscured Structure of a Nail Figure 5–13