Histology of the Skin
Kelli A. Hutchens, MD, FCAP
Director of Dermatopathology
Assistant Professor
Loyola University Medical Center
Assistant Director of Mechanisms of Human Disease
Loyola Stritch School of Medicine
•
•
•
•
Objectives
Identify the epidermis, dermis, and subcutis of the skin
Name and label the layers five layers of the of the epidermis
Compare and contrast the anatomic and histologic differences between thick and
thin skin
Identify (when possible) / or know the location of the following cells:
–
–
–
–
•
Describe the general function and location of the following components of the
dermal epidermal junction and intercellular space.
–
–
–
–
–
•
•
Keratinocyte
Melanoycte
Merkel cell
Langerhan cell
Hemidesmosomes
Basement membrane
Basal layer keratinocytes
Anchoring fibrils
Desmosomes
Name and identify the two regions of the dermis
Identify and classify the following:
– Eccrine gland
– Sebaceous gland
– Apocrine gland
•
Compare and contrast the histologic appearance, function, and location of
Pacinian corpuscles versus Meissner’s corpuscles.
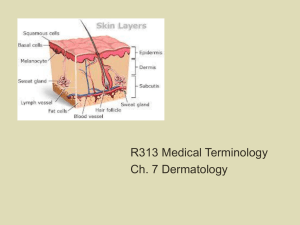
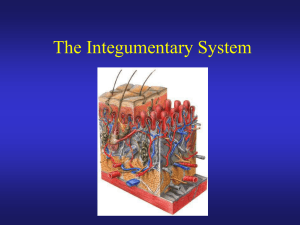
Overview of the Skin
Epidermis
Dermis
Subcutis
Epidermis
• Most superficial layer of the skin
• Composed of multiple layers of keratin
containing epithelial cells = keratinocytes with
Melanocytes, merkel cells, and Langerhans
dispersed throughout
• Major functions:
– Maintenance of fluid and electrolyte balance
– Protection from ultraviolet light
– Sensory and immune function
Epidermis : Layers
• Cancel Lab Get Some Beer
Stratum
Corneum
Stratum Granulosum
Stratum Lucidum
Stratum Spinosum
Stratum Basale
Thin Skin
Rete ridge
Thick Skin
Differences between thin & thick skin
Thin Skin
• Entire body except thick
skin areas.
• Less than 5 layers of
stratum corneum with no
stratum lucidum
• Hair follicles present except
lips, labia minora, and glans
penis
Thick Skin
• Palms of hands and soles of
feet = acral skin
• 5 layers thick stratum
corneum with increased
granular layer
• More sensory receptors
• Lack sebaceous glands and
increased eccrine glands
• No hair follicles
Epidermis
• Desquamatization:
– Layers of epidermis represent vertical maturation
from undifferentiated basal cells to fully differentiated
cornified cells
– From basal cell to cornified cell takes about 25 days
• Shorter maturation periods seen in inflammatory conditions
such as psoriasis
• Keratin production also changes as the cell matures and
disruption in the mechanism can effect the integrity of the
keratinocytes such as in Haily-Haily and Darier’s Disease.
Epidermis
Cell to Cell Adherence
Zona occludens: tight junctions
prevent diffusion across cells
Zona adherens: Ca++ dependent
cadherins that connect to actin
Macula adherens: Made of
desmosomes
Gap junctions: communication for
electric / metabolic function
Basement Membrane
Hemidesmosomes:
connect cells to BM
Epidermis
Desmosome = Intercellular Bridges
Epidermis: Melanocytes
Melanocytes: clearish
cells in basal layer
with dark nuclei ; ratio
of 1: 10.
Langerhans’s Cells: dendritic cells of the epidermis. Sit in the mid-spinous. Not
visible by light microscopy.
Merkel Cells: located in the stratum basale. Also not visible by light microscopy.
They are receptor cells that establish synaptic contacts with sensory nerves and
contain granules of neurotransmitters.
Dermal-Epidermal Junction
• Connects the epidermis and dermis
• It is composed of proteins which provide a
firm connection
– Hemidesmosome: connects basal keratinocytes to
basement membrane
– Basement membrane
• Lamina lucida = collagen types XVII, XIII, laminin 5 & 6
• Lamina densa = collagen type VII
– Anchoring fibrils attach the basement membrane
to the dermis hooking on to collagen VII and
collagen I.
Basement Membrane
Hemidesmosomes
Basal layer keratinocytes
of epidermis
Lamina Lucida
Collagen Type VII
Lamina Densa
Laminins 5 & 6
Basement Membrane
Collagen type XVII, XIII
Anchoring Fibrils
Dermis
Collagen type I
Dermis
• Everything below the dermal epidermal
junction / basement membrane
– Connective tissue layer with contains blood
vessels, nerves, sensory receptors, adnexal
structures
Dermis
– Two layers
• Papillary dermis = includes the dermal papilla which
project into the epidermis
– The increases contact area preventing epidermal detachment
» Also results in an undulating pattern which vary by
anatomic location and individual resulting in grooves in
the epidermis =dermatoglyphics (fingerprints)
– Capillaries, free nerve endings and encapsulated sensory
receptors called Meissner’s corpuscles.
• Reticular dermis = area between the papillary dermis
and subcutis
Papillary Dermis
Capillaries
Papillary
Dermis
Dermis
• The dermis is composed of two major types of
fibers:
– Type I Collagen
– Elastic fibers: three types based on microfiber and
elastin content
Sebaceous
Glands
Reticular
Dermis
Erector Pili
muscle
Hair Follicle
Dermal Appendages
Sebaceous
Glands
Eccrine Glands
Hair Follicle
Pilar Muscle
Sebaceous Glands
• Usually associated with
hair follicles
• Simple branched acinar
glands
– Several acini that empty
into single duct
• Holocrine secretion
• Empty “sebum” into hair
follicle
Hair Follicle
cross section
(above the level of the bulb)
Connective Tissue Sheath
Outer Root Sheath
Inner Root Sheath
Hair Cuticle
Hair Cortex
Bulb
Hair Medulla
Papilla
Matrix
Eccrine Glands
• Merocrine sweat glands
• Release to adjust body
temperature
• Three cell types
– Dark cells: pyramid shaped
with secretory granules line
lumen of tubule
– Clear cells: located toward
basement membrane
– Myoepithelial cells: spindle
shaped contractile cells
Apocrine Glands
• Apocrine glands
– Similar to eccrine glands but
larger lumens and ducts empty
onto superficial regions of hair
follicle
– Release product by shedding of
part of cytoplasm = apocrine
snouting
– Influenced by hormones (sexual
scent glands)
– Only found on axilla, areola,
perianal and genital area
Subcutis
• Subcutis
– Area deep to the
dermis
– Includes the
hypodermis
• Loose connective tissue
containing adipose
tissue, nerves, sensory
receptors, arteries and
veins
• Provides a flexible
attachment to the
underlying muscle and
fascia
Pacinian Corpuscle
Adipocytes
Hair bulb in the subcutis of
the scalp.