Airgas template
advertisement

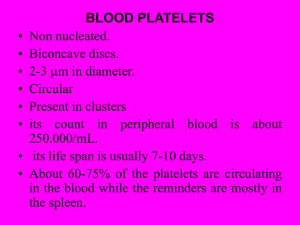
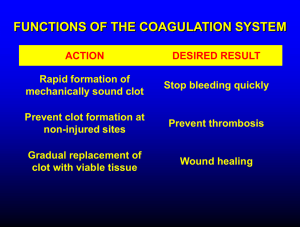
Essentials of Pathophysiology CHAPTER 12 DISORDERS OF HEMOSTASIS PRE LECTURE QUIZ (TRUE/FALSE) F T T T T Platelets are also known as leukocytes. Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disorder that affects the normal function and formation of platelets. Disseminated intravascular coagulation is a condition that results in massive systemic bleeding, but coagulation function remains normal. The use of aspirin and other nonsteroidal antiinflammatory drugs (NSAIDs) has been identified as a cause of impaired platelet function. Bleeding can occur as a result of a decrease in the number of circulating platelets or because of impaired platelet function. PRE LECTURE QUIZ Bleeding K Hemostasis thrombocytopenia VIII _________________ is the orderly, stepwise process for stopping bleeding that involves vasospasm, formation of a platelet plug, and development of a fibrin clot. A decrease in the number of circulating platelets is known as _________________________. Hemophilia A is an X-linked recessive disorder that involves a deficiency of factor _________________. ________________ disorders are caused by defects associated with platelets, coagulation factors, and vessel integrity. Vitamin _______________, a fat-soluble vitamin that is continuously being synthesized by intestinal bacteria, is necessary for normal activity of factors VII, IX, and X and prothrombin. HEMOSTASIS Stopping blood flow Normal: Blood usually fluid Seals broken blood vessels Abnormal: Inappropriate clotting Insufficient clotting PLATELETS (THROMBOCYTES) Thrombopoietin Made in liver, kidney, smooth muscle, bone marrow Megakaryocytes formed in bone marrow Break apart to form many platelets Platelets live 8–9 days in circulation Many are stored in spleen Released when needed PLATELET STRUCTURE QUESTION All but which of the following are true about platelets? a. An enzyme called erythropoietin stimulates their production. b. They are made from megakaryocytes. c. They originate from the bone marrow. d. They are stored in the spleen. ANSWER An enzyme called erythropoietin stimulates their production. Rationale: Erythropoietin stimulates the production of RBCs (erythrocytes). The word literally means erythrocyte production. Platelet formation is stimulated by thrombopoietin (thrombus/clot production). a. CLOTTING CASCADE MEDIATORS OF HEMOSTASIS Chemicals produced by platelets Released at an injury to: Start clotting by reacting with blood proteins Help platelets stick together Stimulate wound healing Help platelets stick to vessel wall Constrict blood vessels COAGULATION FACTORS Plasma proteins Most are synthesized by liver von Willebrand factor made by endothelium Circulate as inactive procoagulation factors Calcium QUESTION What is the effect of von Willebrand disease on the platelets? a. Increased platelet aggregation b. Decreased platelet aggregation c. Increased platelet formation d. Decreased platelet formation ANSWER Decreased platelet aggregation Rationale: Von Willebrand disease is the most common hereditary bleeding disorder. It is caused by a deficiency or defect in vWF (which carries a clotting factor). The result of less clotting factor is an inability to clot. b. VESSEL SPASM CYCLOOXYGENASE ENZYMES (COX) PRODUCE MEDIATORS OF HEMOSTASIS Celebrex is a drug that blocks COX-2 Given to block inflamation arachidonic acid People taking Celebrex develop increased TXA2 COX-1 COX-2 levels What problems thromboxane A 2 Prostacyclin might they have? NSAIDs inhibit both COX 1 &2 Problems here? COX 1 is needed for intestinal mucosa Macrophage Activation & Inflamation mediation INTRINSIC AND EXTRINSIC PATHWAYS Common Pathway PLATELETS Platelet aggregate with fibrin threads Activated platelets Non activated platelet FIBRINOGEN FIBRIN SCENARIO A man had a stroke and the doctor gave him tissue plasminogen activator (TPA). Why? What is the doctor trying to accomplish? One of the man’s relatives wondered why they did not give him heparin or warfarin instead What is the difference? Why might TPA be more appropriate? HYPERCOAGULABILITY Increased platelet number Platelet aggregation Endothelial damage Increased procoagulation factors Decreased anticoagulation factors QUESTION True or False. Hypercoagulability states increase the risk of thrombus formation. ANSWER True Rationale: Hyper- as a prefix means “over” or “too much.” Coagulation/coagulability means “clotting/the ability to clot.” Hypercoagulability means “increased ability to clot or form thrombi.” SCENARIO: A woman with lupus develops breast cancer. She is given radiation therapy She begins to develop nosebleeds and bruising Her menstrual period is abnormally heavy Question: Why did this happen? PLATELET DISORDERS Decreased platelet levels (thrombocytopenia) Decreased production Increased destruction Platelets used up in forming clots Impaired platelet function DIC QUESTION True or False. Platelet disorders are bleeding disorders. ANSWER True Rationale: Because the platelet’s job is to clot, platelet disorders mean that the platelets cannot do that job. An inability to clot results in bleeding/bleeding disorders.