Preparation for the CSA - Dr Allison Law
advertisement
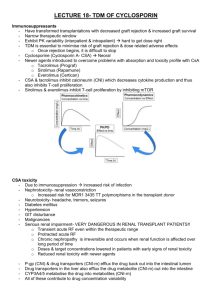
Preparation for the CSA How to make it an integral part of education and work in the practice Dr Allison Law FRCGP Course organiser Glasgow North District What do we do now?? What methods\tools do we use to teach CSA to our GPSTs and How do we do it? Can we teach GPSTs how to do well in the CSA exam? What skills are required? What areas of the curriculum are tested? Recognition of what goes wrong & why GPSTs fail Identify your GPSTs weaknesses Tailor teaching to individual needs What skills are required? Data gathering - Gathering & using data for clinical judgement, choice of examination, investigations & their interpretation. Demonstrating proficiency in performing physical examinations & using diagnostic and therapeutic instruments Clinical management - Recognition & management of common medical conditions in primary care. Demonstrating a structured & flexible approach to decision-making. Demonstrating the ability to deal with multiple complaints and co-morbidity. Demonstrating the ability to promote a positive approach to health Interpersonal skills - Demonstrating the use of recognised communication techniques to gain understanding of the patient's illness experience and develop a shared approach to managing problems. Practising ethically with respect for equality & diversity issues, in line with the accepted codes of professional conduct Curriculum areas tested in CSA Primary Care Management - recognition and management of common medical conditions in primary care. Problem Solving Skills - gathering and using data for clinical judgment, choice of examination, investigations and their interpretation. Demonstration of a structured and flexible approach to decision making. Comprehensive Approach - demonstration of proficiency in the management of co-morbidity and risk. Person-centred Care - communication with patient and the use of recognised consultation techniques to promote a shared approach to managing problems. Attitudinal Aspects - practising ethically with respect for equality and diversity, with accepted professional codes of conduct. The CSA will also test: Clinical Practical Skills - demonstrating proficiency in performing physical examinations and using diagnostic/therapeutic instruments. Why GPSTs Fail Under prepared Sit too early - timing Insufficient knowledge base – see patients, regular review of consultations, tutorial and application of knowledge base Cant cope with 10 min appointments – regular and enough exposure prior to exam Poorly prepared Not enough assessment of skills – use Video to assess 3 Domains areas & forget COT domains Time management – how to move the patient along, close the consultation (second half checklist)* Formulaic use of stock phrases and unable to use sensitively or appropriately Bad day Housekeeping (Neighbour) Ignore examiner – focus on the patient (joint consultations) Getting there – reduce unnecessary stress Not good enough “cut out” to be a GP Likely already aware – failed WPBA CSA – Just like a good story Introduction – sets the scene and context. Why are they there, what do they want (ICE) How is it affecting them in their life (Psychosocial) Middle – What’s wrong with them, do I know, How do I find out more (examination), have I missed anything (red flags), what do I tell them is wrong (diagnosis) End – explanation & Management. Have I told them what is wrong or addressed their concerns, have I decided what to do, do I need to do anything else (tests, referral). Do they know what I’m talking about and what to do (understanding) Safety net & follow up Summarising – what do we do? Regular review of consultations Videos (& COTs) Educate them about the CSA exam, RCGP website, give some direction Ensure they have sufficient knowledge base – tutorials, case review, RCA Joint consultations 10 min consultations – get them up to speed Time management (see later) Identify and address individuals weaknesses What else can we do? GPST to write cases, identify from real patient contacts, review with trainer or role play with shared GPST tutorials Role play in GPST groups (Care!!) Case scenarios – Pennine, Bradford website RCGP DVDs ( Wessex Deanery) Case cards (Wessex Deanery) Books – RCGP – CSA scenarios for MRCGP, Get through MRCGP Clinical skills Case Cards Communicate Articulate Simplify Explain 120 cards – explanation of new diagnoses, drugs and practical advice Can be used as “quick fire” questions in tutorials or to stimulate CSA scenario cases Practice explaining common medical conditions Pennine GP Training Series of you tube videos explaining common medical conditions, treatments in 3 mins Can do similar with CASE cards or random case analysis, video review Use with score cards Score card scoring each domain 1-5 where 0= poor and 5= outstanding GPST Name Condition Compre hension No medical jargon Use of analogy Use of diagram Use of PILs Timing Total Time management Get slick at explaining common medical conditions but not rehearsed Practice focused clinical examination (<2 mins) Direct the consultation to a conclusion – close the consultation and have a management plan focused in the second half Second half checklist Check which of the following tasks were achieved and make a note of the exact phrases used (Pennine) Summary Explaining Revisiting ICE Checking understanding Sharing options Agree a management plan Refer/prescribe/do nothing etc. Plan for follow-up Safety netting Time management Watch videoed consultations stopping at 10 mins – helps GPST identify what gets lost and therefore cant be examined Use of watch\clock – no matter what aim to “round up” the consultation at latest 8 mins Set screen saver timer to 8 mins What else?? Be prepared for what you don’t see in practice Males – gynaecology Females – male problems, prostate Drug & social problems Worried well Telephone consultations (speaker phone) Identify consultations where GPST felt uncertain – what if it had been a CSA Training Groups Day\Half day release CSA sessions Mock CSAs – real experience 6-8 cases Sharing difficult experiences in consultations – increases exposure to different situations