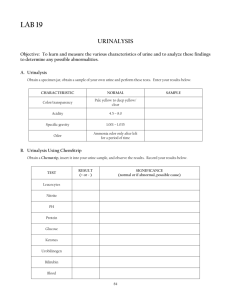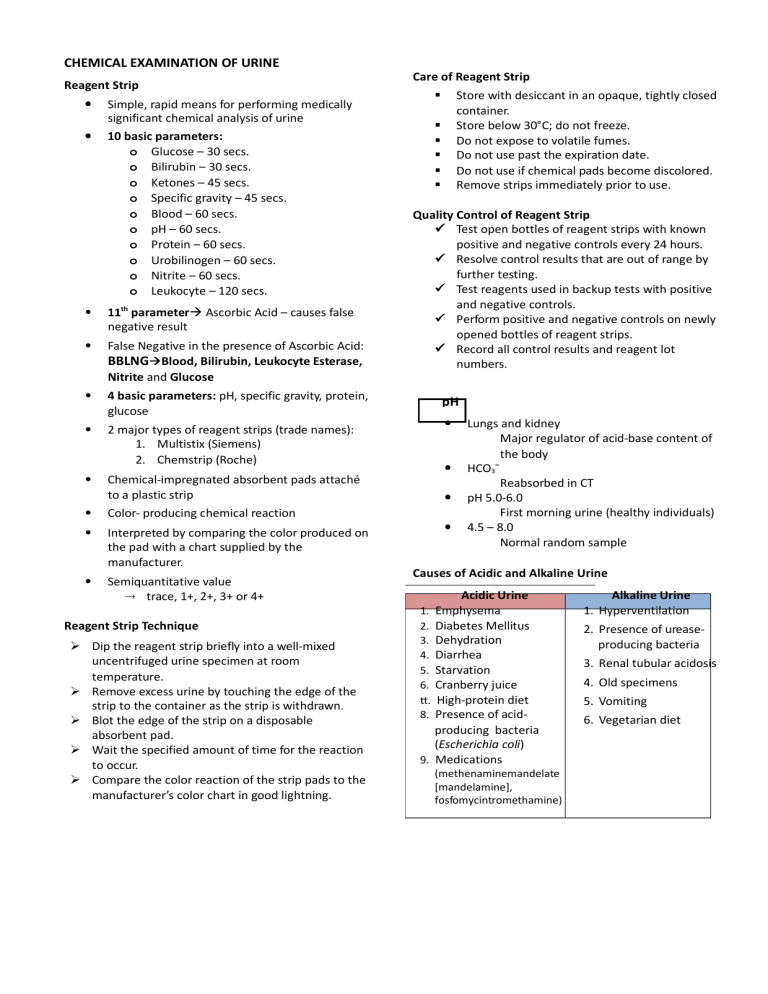
CHEMICAL EXAMINATION OF URINE Reagent Strip Simple, rapid means for performing medically significant chemical analysis of urine 10 basic parameters: o Glucose – 30 secs. o Bilirubin – 30 secs. o Ketones – 45 secs. o Specific gravity – 45 secs. o Blood – 60 secs. o pH – 60 secs. o Protein – 60 secs. o Urobilinogen – 60 secs. o Nitrite – 60 secs. o Leukocyte – 120 secs. 11th parameter Ascorbic Acid – causes false negative result False Negative in the presence of Ascorbic Acid: BBLNGBlood, Bilirubin, Leukocyte Esterase, Nitrite and Glucose 4 basic parameters: pH, specific gravity, protein, glucose 2 major types of reagent strips (trade names): 1. Multistix (Siemens) 2. Chemstrip (Roche) Chemical-impregnated absorbent pads attaché to a plastic strip Color- producing chemical reaction Interpreted by comparing the color produced on the pad with a chart supplied by the manufacturer. Semiquantitative value trace, 1+, 2+, 3+ or 4+ Reagent Strip Technique Dip the reagent strip briefly into a well-mixed uncentrifuged urine specimen at room temperature. Remove excess urine by touching the edge of the strip to the container as the strip is withdrawn. Blot the edge of the strip on a disposable absorbent pad. Wait the specified amount of time for the reaction to occur. Compare the color reaction of the strip pads to the manufacturer’s color chart in good lightning. Care of Reagent Strip Store with desiccant in an opaque, tightly closed container. Store below 30ᵒC; do not freeze. Do not expose to volatile fumes. Do not use past the expiration date. Do not use if chemical pads become discolored. Remove strips immediately prior to use. Quality Control of Reagent Strip Test open bottles of reagent strips with known positive and negative controls every 24 hours. Resolve control results that are out of range by further testing. Test reagents used in backup tests with positive and negative controls. Perform positive and negative controls on newly opened bottles of reagent strips. Record all control results and reagent lot numbers. pH Lungs and kidney Major regulator of acid-base content of the body HCO3– Reabsorbed in CT pH 5.0-6.0 First morning urine (healthy individuals) 4.5 – 8.0 Normal random sample Causes of Acidic and Alkaline Urine Acidic Urine 1. Emphysema 2. Diabetes Mellitus 3. Dehydration 4. Diarrhea 5. Starvation 6. Cranberry juice 7. High-protein diet 8. Presence of acidproducing bacteria (Escherichia coli) 9. Medications (methenaminemandelate [mandelamine], fosfomycintromethamine) Alkaline Urine 1. Hyperventilation 2. Presence of ureaseproducing bacteria 3. Renal tubular acidosis 4. Old specimens 5. Vomiting 6. Vegetarian diet Clinical Significance (pH) Respiratory or metabolic acidosis / ketosis Respiratory or metabolic alkalosis Defects in renal tubular secretion and reabsorption of acids and bases – renal tubular acidosis Renal calculi formation Treatment of urinary tract infections Precipitation / identification of crystals Determination of unsatisfactory specimens I. Pre-renal Proteinuria Caused by the condition affecting the plasma prior to reaching the kidney Not indicative of actual renal disease Frequently transient: o Hemoglobin o Myoglobin o Acute phase reactant due to inflammation Not usually discovered in routine urinalysis Reagent Strip Reaction (pH) Measures pH between 5 – 9 Principle: DOUBLE-INDICATOR SYSTEM OF METHYL RED AND BROMTHYMOL BLUE Bence Jones Protein Seen in case of multiple myeloma Monoclonal immunoglobulin light chain pH range 4 - 6 pH range 6 - 9 pH 5 orange; pH 9 green No known substance to cause interference of pH test Prevent runover between pH and CHON false acidic reading PROTEIN (ALBUMIN) Most indicative of renal disease Proteinuria early renal disease Normal value: <10 mg/dL or 100mg/24h (usually albumin) Other CHON: o Tubular microglobulins, Tamm-Horsfall protein (uromodulin) produced by the tubules, and proteins from prostatic, seminal, and vaginal secretions Clinical Significance (Protein) Proteinuria Does not always signify renal disease Presence requires additional testing Clinical proteinuria ≥ 30 mg/dL or 300 mg/L 3 major categories: o Pre-renal o Renal o Post-renal II. Screening Test: Solubility test o Coagulates at 40-60ᵒC (turbid); dissolves when attempt reaches 100ᵒC (clear) o Filter 100ᵒ C and observe for turbidity as it cools to 40-60ᵒC Confirmatory: Serum electrophoresis / IE Renal Proteinuria True renal disease (glomerular/tubular disease) 1. Glomerular Proteinuria Selective filtration is impaired Increased protein, RBCs, WBCs Causes: o Amyloid material o Toxic substances o Immune complexes found in lupus erythematous and streptococcal glomerulonephritis o Strenuous exercise o Dehydration o Associated with hypertension preeclampsia 2. Tubular Proteinuria Disorders affecting tubular reabsorption Filtered albumin can no longer be reabsorbed Causes: o Exposure to toxic substances and heavy substances o Severe viral infections o Fanconi syndrome Benign Proteinuria: Transient o Strenuous exercise o High fever o Dehydration Exposure to cold 3. Orthostatic (Postural) Proteinuria Seen frequently in young adults Appears in vertical position; disappears in horizontal position Empty bladder before going to bed, collect first morning upon rising Collect second specimen after remaining in vertical position for several hours Results: o Negative (-) 1st sample o Positive (+) 2nd sample o 4. Microalbuminuria Diabetic nephropathy leading to reduced glomerular filtration and eventual renal failure Prevented through better stabilization of blood glucose levels and controlling of hypertension 24-hour urine sample Positive (+): Microalbumin is significant o 30-300 mg/24hr o 20-200 ug/min III. Post-renal Proteinuria Protein can be added to a urine specimen as it passes through the structures of the lower urinary tract (ureters, bladder, urethra, prostate, and vagina) Bacterial and fungal infections ad inflammations The presence of blood as the result of injury or menstrual contamination Presence of prostatic fluid and large amounts of spermatozoa Reagent Strip (Protein) Principle: PROTEIN ERROR OF INDICATORS Chemstrip: 6 mg/dL albumin Interference (Protein) False-Positive Highly buffered alkaline urine Pigmented specimens, phenazopyridine Quaternary ammonium compounds (detergents) Antiseptics, chlorhexidine Loss of buffer from prolonged exposure of the reagent strip to the specimen High specific gravity Reagent: Multistix: Tetrabromphennol blue Chemstrip: 3’,3”,5’,5” tetrachlorophenol 3,4,5,6 tetrabromosulfophthalein Sensitivity: Multistix: 15-30 mg/dL albumin Proteins other than albumin Microalbuminuria Correlations with other tests (Protein) Blood Nitrite Leukocytes Microscopic Other Albumin Qualitative Test General Principle: Precipitation of protein by heat and coagulation by chemical reagents Test Heat and Acetic acid Sulfosalicylic Acid (SSA) / Exton’s Test Heller’s Ring Test Purdy’s Test Picric Acid Test Robert’s Ring Test False-Negative Potassium Ferrocyanide Test Reagent Acetic Acid Sulfosalicylic Acid or Sodium Sulfate Concentrated Nitric Acid 50% Acetic Acid Saturated solution of picric acid Magnesium sulfate or concentrated nitric acid Glacial acetic acid and K ferrocyanide Results White cloudiness White ring at zone of contact White opaque ring White cloudiness Precipitation White ring at zone of contact Cloudiness (proteases) Test Esbach’s Test Shevky and Stafford Test Kingsbury Clark Test Kwilecki’s Test Purdy’s Test Reagent Picric acid and Citric acid Tsuchiya’ 3% SSA 10% Ferric chloride Results GLUCOS PRECIPITATION Grams/24 hr or mg/dL Specimen: 24-hours urine 50% Acetic acid 10% K ferrocyanide Most frequent chemical analysis performed on urine Value: detection and monitoring of DM Most informative glucose results are obtained from specimens collected under controlled conditions Fasting or 2-hour after meal specimen o Advised empty bladder then collect 2nd specimen Clinical Significance (Glucose) Diabetes Mellitus Hyperglycemia Glycosuria Tubular transport of glucose ceases 180 mg/dL Microalbumin Testing Immunologic Tests Micral-Test Gold-labeled antibody, -galactosidase, Principle: Enzyme Chlorophenol red Immunoassay galactoside Immunodip Principle: Immunochromographics Antibody-coated blue latex particles Sensitivity: 0 – 10 mg/dL Interference: False negative dilute urine Sensitiviy: 1.2 – 8.0 mg/dL Interference: False negative dilute urine Albumin:Creatinine Ratio ClinitestMicroa lbumin Strips / Albumin: Sensitivity: DiodoMultistix-Pro Albumin: dihydroxydinitro 10 – 150 mg/dL Principle: -phenyl Creatinine: Sensitive tetrabromosulp 10 – 300 mg/dL, albumin tests honphthalein 0.9 -26.5 mmol/L related to creatinine concentrations to convert for patient hydration Creatinine: Copper sulfate, tetramethylbenzidine and diisopropyl benzene dihyroperoxide Interference: Visibly bloody or abnormally colored urine Creatinine: Cimetidine: False positive Hyperglycemia-Associated Renal – Associated Fanconi syndrome Diabetes Mellitus Advanced renal disease Pancreatitis Osteomalacia Pancreatic cancer Pregnancy Acromegaly Cushing syndrome Hyperthyroidism Pheochromocytoma CNS damge Stress Gestational diabetes Gestational diabetes - hyperglycemia that occurs during pregnancy and disappears after delivery Reagent Strip Reactions (Glucose Oxidase) Mixture of glucose oxidase, peroxidase, chromogen and buffer Principle: DOUBLE SEQUENTIAL ENZYME REACTION Reagents: Multistix: Glucose oxidase & Peroxidase Potassium iodide (green & brown) Chemstrip: Glucose oxidase & Peroxidase Tetramethybenzidine (yellow to green) Sensitivity: Multistix: 75 – 125 mg/dL Chemstrip:40 mg/dL Interference(Glucose Oxidase) False-Positive Contamination by oxidizing agents and detergents Other Sugars: False-Negative High levels of ascorbic acid High levels of ketones High specific gravity Low temperature Improperly preserved specimens Copper Reduction Test (Clinitest) Relies to the ability of glucose and other substances to reduce copper sulfate to cuprous oxide in the presence of alkali and heat. Sugar Fructose: Fructokinase deficiency Pentose: Genetic disorder Xylitol Dehydrogenase deficiency Other Glucose Qualitative Test General Principle: Reduction Principle Test Benedict’s Test Clinitest Tablet Fehling’s Test a.Fehling’s A b.Fehling’s B Osazone Test (phenylhydrazine) Nylander’s Test Moore Heller’s Reagent CuSO4 / Sodium Citrate (buffer) / NaCO3 CuSO4 / Sodium Citrate / NaCO3/ NaOH Positive Results (-): Blue ±: Green, no ppt. 1+: Green with ppt. 2+: Yellow-green w/ ppt. 3+: Muddy-orange w/ yellow ppt. 4+: Orange to brick red Range of Colors (blue to orange/red) Lactose: Lactokinase deficiency Seen in lactating women and long term milk diet Galactose: Inborn error of metabolism Yellow ppt. Cupric salt/dH2O Rochelle Salt/ KOH/ dH2O Phenylhydrazine HCl Sodium acetate Bismuth subnitrite 10% KOH Bright yellow needle crystal Brown – black solution 1% or less: canary yellow 1-2%: wine yellow 2-3%: cherry red 3-4%: rum >4% : dark brown-black Maltose: Test Sellwanoff’s Test Result Borchardt’s Test (Resorcinol an HCl) Red solution / red ppt. Barfoed’s Test Black hue Bial’s Test Cole Test (FeCl3 and charcoal) Green color Tauber’s Test (Benzidine and glacial HAc) Pink-cherry red Tollen’s Test (conc. HCl and phloroglucin) Purple Rubner’s Test (Lead acetate and conc. NH4OH) Red Color Ormsby Test (methylamine HCl and NaOH) Mucin acid test (Conc. HNO3) White Color Mucin acid test (Conc. HNO3) White ppt. Tollen’s Test (Conc. HCl and phloroglucin) Purple ppt. Osazone Test Yellow needle crystals Red Color Barfoed’s Test Other Test for Ketones KETONES Intermediate products of fat metabolism o Acetone (2%) Water soluble Non-reversible spontaneous decarboxylation product of diacetic acid o Acetoacetic acid (20%) Diacetic acid Most abundant in urine o Beta-hydroxybutyric acid (78%) Reversible to diacetic acid Clinical Significance (Ketones) Diabetic ketoacidosis (IDDM) Insulin dosage monitoring Starvation Excessive carbohydrate loss Reagent Strip (Ketones) Principle: Based on SODIUM NITROPRUSSIDE (NITROFERRICYANIDE) REACTION Beta-hydroxybutyric acid is not measured Sensitivity: Multistix: 5-10 mg/dLacetoacetic acid Chemstrip: 9 mg/dLacetoacetic acid; 70 mg/dL acetone Interference (Ketones) False-Positive Phthalein dyes Highly pigmented red urine Levodopa Medications containing free sulfhydryl groups False-Negative Improperly preserved specimens Test Acetest tablet Rothera’s Tube Test TESTS FOR ACETONE Reagents Na Nitroprusside/ Glycine/ Disodium phosphate/Lactose Na Nitroprusside/ Ammonium sulfate Lileben’sIodoform Test Gunning’s Test Frommer’s Test Legal’s Test KOH/ Iodine/ KI Alc. Iodine solution KOH/ salicylaldehyde Na Nitroprusside Results Lavender purple Red – purple ring at the zone of contact Yellow ppt. of iodoform Yellow ppt. of iodoform Purple ring Violet TESTS FOR DIACETIC ACID Test Reagents Results Gerhard’s Test FeCl3 Bordeaux red Lindemann’s 30% Acetic acid/ Reddish violet Iodine and Test chloroform TESTS FOR BETA-HYDROXYBUTYRIC ACID Test Reagents Results Hart’s Test HAc / H2O2 Red ring Ammonium Red Osterberg’s Test sodium hydroxide BLOOD Hematuria – intact RBC (cloudy red) Hemoglobinuria– Clear red > 5 cells / µL urine = clinical significant Chemical tests for hemoglobin most accurate means for determining the presence of blood Microscopic examination differentiate between hematuria and hemoglobinuria Hematuria Disorders of renal or genitourinary origin Bleeding is the result of trauma or damage to the origin Major causes: Renal calculi, glomerular diseases, tumors, trauma, pyelonephritis, exposure to toxic chemicals and anticoagulant therapy Cause of Hematuria Lower UTI Renal Calculi Glomerular disease (LE) Tumor Glomerulonephritis Trauma/ Exposure to toxic chemicals / Anticoagulants Malignant papilloma Comment Presence of RBC, WBC and bacteria in urine Severe back and abdominal pain Result of Ag-Ab reaction that localizes in the kidneys Abnormal swelling in or on part of the body Destroyed glomerular tissue Nipple-like growth on the surface of the skin and other organs Hemoglobinuria Lysis of red blood cells Result from intravascular hemolysis Lysis of red cells in urine Hemosiderin– large yellow-brown granules of denatured ferritin; the result of reabsorption of filtered hemoglobin use of plasma for differentiation of Hemoglobinuria and Myoglobinuria Cause of Hemoglobinuria 1. Transfusion reactions 2. Hemolytic anemia 3. Severe burns 4. Infection 5. Strenuous exercise/ red blood cell trauma 6. Brown recluse spider bites 7. Malaria Comment Hemoglobinuria + hematuria = lysis of RBC in urine Hemoglobinuria alone = intravascular hemolysis Amount of free hemoglobin present exceeds the haptoglobin content Occurs only when is filtered by the glomerulus Black water fever Myoglobinuria Myoglobin – a heme containing protein found in muscle tissue Seen in rhabdomyolosis (muscle destruction) Positive with reagent strip test for blood Produces a clear-red brown urine Cause of Myoglobinuria 1. Muscular trauma/ crush syndromes 2. Prolonged coma 3. Muscle-wasting disease 4. Convulsions 5. Alcoholism/overdose 6. Drug abuse 7. Extensive exertion 8. Cholesterol-lowering stain medications Comment Atrophy involving affected parts, such as damage muscles and its nerves, or lack of use Involuntary muscle contraction Associated with cardiomegaly Reagent Strip (Blood) Principle: PSEUDOPEROXIDASE ACTIVITY OF HEMOGLOBIN Chromogen: tetramethylbenzidine Color reaction: yellow-green – blue Speckled pattern on pad intact RBC (lysed during contact with the pad) BILIRUBIN Interference (Blood) False-Positive Strong oxidizing agents Bacterial peroxidases (E.coli) Menstrual contamination False-Negative High SG/ crenated cells Formalin Captopril High concentrations of nitrite Ascorbic acid >25 mg/dL Unmixed specimens Other Tests for Blood Tests Benzidine Test - most sensitive test in blood Gulac’s Test Occult Blood Benzidine Tablet Test Orthotoluidine Test Telchman’s Test - no color produced Reagents Benzidine/ H2O2 Positive Results Green to Blue Glacial Acetic acid/ H2O2 / Gulac’s gum solution Benzidine/ H2O2 Green to Blue Methyl alcohol/ acetic acid / peroxidase Saline solution/ glacial HAc Green to Blue 100/mm3 = greenish-blue 300-500/mm3 = deep blue for 1 minute 1000/mm3 = deep blue for 2 minutes Crystallization of hemine Clinical Significance (Bilirubin) 1. Hepatitis 2. Cirrhosis – scarring of the liver 3. Other liver disorders 4. Biliary obstruction (gallstones, carcinoma) Condition Bile duct obstruction Liver damage Hemolytic disease Urine Bilirubin +++ Urine Urobiinogen Normal + or Negative ++ +++ Reagent Strip (Bilirubin) Principle: DIAZO REACTION Reagent: Multistix: 2,4-dichloroaniline diaonium salt Chemstrip: 2,6-dichlorobenzene diazonium Salt Color reaction: Tan or pink to violet Sensitivity: Multistix: 0.4 – 0.8 mg/dL bilirubin Chemstrip: 0.5 mg/dL bilirubin Clinical Significance (Urobilinogen) 1. Early detection of liver disease 2. Liver disorders, hepatitis, cirrhosis, carcinoma 3. Hemolytic disorders Absence of urobilinogen in stool Indication of bile obstruction (pale stool) Reagent Strips (Urobilinogen) Multistix: EHRLICH REACTION Interference (Bilirubin) False-Positive Highly pigmented urines(phenazopyridine) Indican (intestinal disorders) Metabolites of Lodine False-Negative Specimen exposure to light Ascorbic acid >25 mg/dL High concentrations of nitrite Correlation with other test (Bilirubin) Urobilinogen Ultzman’s Test Foam Test Icto Test Sensitivity: 0.05-0.10 mg/dL Harrison Spot Fouchet’s Test Reagents Ethanol solution of Iodine Concentrated HNO3 KOH/HCl p-nitrobenzenediazonium-ptoluenesulfonate, SSA, sodium carbonate, and boric acid BaCl2 / Fouchet’s reagent BaCl2 / FeCl3 UROBILINOGEN Interference (Urobilinogen) Multistix (Ehrlich’s reaction) Other Tests for Bilirubin (Bilirubin) Tests Smith’s (Iodine Test) Gmelin’s Test Chemstrip: DIAZO REACTION Positive Results Emerald-green Green (biliverdin) Violet (choletin) Yellow/Red (Bili) Blue-green (bilicyanin) Green Yellow foam Bluish-purple Blue-green Greenish-blue spot Chemstri p (Diazo reaction) False-Positive Porphobilinogen Indican p-aminosalicylic acid Sulfonamides Methyldopa Procaine Chlorpromazine Highly pigmented urine Highly pigmented urine False-Negative Old specimens Preservation in formalin High concentrations of nitrite Ehrlich Tube Test 1 part of Ehrlich reagent + 10 part of urine Positive (+) : Cherry red color Watson – Schwartz Differentation Test Tube 1 2 mL urine 2mL chloroform 4 mL sodium acetate Tube 2 2mL urine 2mL butanol 4mL sodium acetate Hoesch Screening Test for Porphobilinogen Rapid test Hoesch Reagent: Ehrlich’s reagent dissolved in 6M HCl 2 drops urine + 2mL Hoesch Reagent Positive(+): Red Color Sensitivity: 2 mg/dL Interference: o False (+): methyldopa, indicant, highly pigmented urine o False (-): acidic pH NITRIT Watson – Schwartz Test Interpretation Rapid screening test for the presence of urinary tract infection (UTI) Clinical Significance (Nitrite) Cystitis – inflammation of urinary bladder Pyelonephritis – inflammation of kidney Evaluation of antibiotic therapy Monitoring patients at high risk for UTI Screening of urine culture specimens Reagent Strip (Nitrite) Principle: GREISS REACTION Basis of test: Ability of a certain bacteria to reduce nitrate to nitrite Reporting: Positive or negative only Interference (Nitrite) Urobilinogen is soluble in both chloroform and butanol, and porphobilinogen is soluble in neither. If both urobilinogen and porphobilinogen are present, both layers are red. Before reporting the test as both are positive for both substances, an additional chloroform extraction should be performed on the red urine (upper) layer in Tube 1 to ensure that the red color is not due to excess urobilinogen. False-Positive Improperly preserved specimen Highly pigmented specimen False-Negative Nonreductasecontaining bacteria Insufficient contact time between bacteria and urinary nitrate Lack urinary nitrate Large quantities of bacteria converting nitrite to nitrogen Presence of antibiotics High concentrations of ascorbic acid High specific gravity SPECIFIC GRAVITY LEUKOCYTE ESTERASE Detects the presence of esterase in the granulocytic WBCs and monocyte Detects the presence of leukocytes that have been lysed, particularly in dilute alkaline urine, and would not appear in the microscopic examination Positive LE is often accompanied by the presence of bacteria Leukocyturia without bacteriuria = Trichomonas, Chlamydia, Yeast infection and inflammation of renal tissues (interstitial nephritis) Reagent Strip (LE) Based on the action of LE to catalyze the hydrolysis of an acid ester to produce an aromatic compound and acid Reagent Strip (Specific Gravity) Principle: pKa CHANGE (Dissociation constant) OF A POLYELECTROLYTE IN AN ALKALINE MEDIUM Blue (1.000) to shades of green-yellow (1.030) Reagent: Multistix: Poly (methyl vinyl ether/ maleic anhydride) bromthymol blue Chemstrip: Ethyleneglycoldiaminoethylethertetraacetic acid, bromthymol blue Measures only ionic solutes Elevated protein can elevate the result Specimens with pH 6.5 or higher decreased readings due to bromthymol blue indicator interference Corrected by adding 0.005 Automated strip readers automatically corrects the reading Interference (Specific Gravity) Sensitivity: Multistix: 5 -15 WBC/hpf Chemstrip: 10 – 25 WBC/hpf Interference (LE) False-Positive Strong oxidizing agents Formalin Highly pigmented urine Nitrofurantoin False-Negative High concentrations: o Protein o Glucose o Oxalic acid o Ascorbic acid o Gentamicin o Cephalosporins o Tetracyclines Inaccurate timing False-Positive High concentrations of protein False-Negative Highly alkaline urine (greater than pH 6.5)