Path macro-micro
advertisement
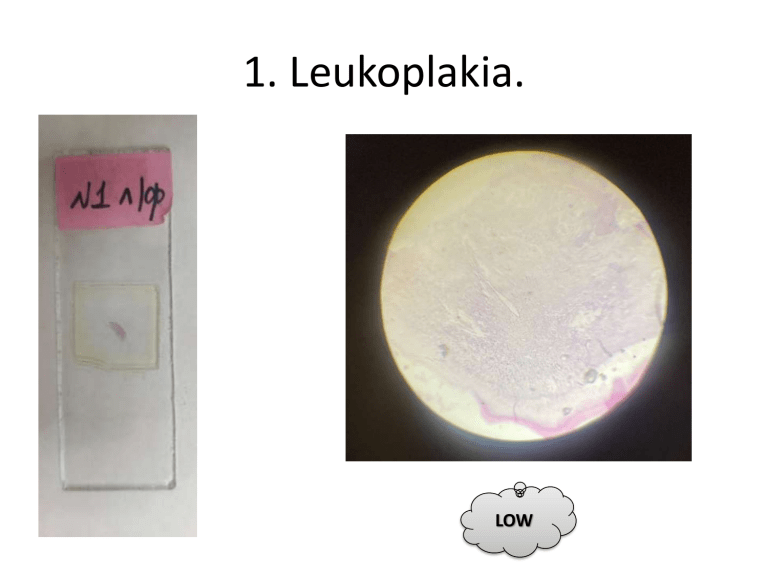
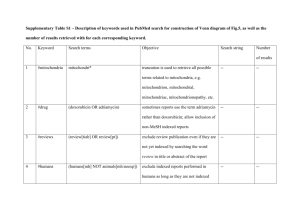
1. Leukoplakia. LOW HIGH 2. Fatty liver LOW HIGH 3. Kidney amyloidosis (Congo-red staining) LOW HIGH 4. Nutmeg liver (liver in chronic venous congestion). LOW HIGH 5. Lung hemosiderosis. LOW HIGH 6. Myocardial infarction LOW HIGH 7. Liver infarction. LOW HIGH 8. Mixed thrombus. LOW HIGH 9. Liver hemosiderosis in hemolytic anemia. LOW HIGH 10. Metastatic calcification in myocardium. LOW HIGH 11. Pigmented nevus of skin. LOW HIGH 12. Endometrial adenomatous hyperplasia. LOW HIGH 13. Bronchopneumonia (focal pneumonia). LOW HIGH 14. Lobar pneumonia. LOW HIGH 15. Duodenal ulcer. LOW 16. Suppurative (phlegmonous) appendicitis LOW 17. Echinococcus multilocularis in liver (alveolar hydatid disease) LOW 18. Trichinella in skeletal muscle. LOW 19. Miliary tubercles in lung. LOW 20. Seleroma of larynx. LOW 21. Hemangioma. LOW 22. Non-keratinizing squamous cancer. LOW 23. Gastric adenocarcinoma. LOW 24. Polymorphocellular sarcoma (rhabdomyosarcoma). LOW 25. Melanoma LOW 26. Coronary artery atherosclerosis. LOW 27. Alterative-productive myocarditis. LOW HIGH 28. Pulmonary emphysema. LOW 29. Miliary tuberculosis of kidney. LOW 30. Portal cirrhosis. LOW 31. Liver in lymphoid leukemia. LOW 32. Hodgkin's lymphoma. LOW HIGH 33. Primarily contracted kidney. LOW HIGH 34. Extracapillary (rapidly progressive) glomerulonephritis. LOW 35. Chronic pyelonephritis ("thyroid kidney") LOW 36. Thyroid gland in Graves' (Basedow's) disease. LOW 37. Diabetic glomerulosclerosis. LOW 38. Kidney in septicopyemia ("embolic purulent nephritis"). Multiple abscesses in the kidney cortex, marked congestion in surrounding tissue. Microbial emboli in the center of some of abscesses. LOW 39. Purulent meningitis. LOW 40. Focal cardiosclerosis. LOW 41. Diphtheritic tonsillitis. LOW 42. Liver lipofuscinosis ("brown atrophy"). LOW 43. Hashimoto's thyroiditis. LOW 44. Kidney in cytomegalovirus infection. LOW 45. Hyaline membrane disease. LOW 46. Liver in hemolytic disease of the newborn. LOW 47. Spleen in listeriosis. LOW 48. Kidney cortical necrosis in DIC. LOW 49. Polycystic kidney disease. LOW 50. Breast cancer Metastasis to lungs. LOW LIST OF GROSS SPECIMENS FOR THE QUIZ 1. Amyloid-lipoid nephrosis Amyloidosis is a rare disease characterized by a buildup of abnormal amyloid deposits in the body. Amyloid deposits can build up in the heart, brain, kidneys, spleen and other parts of the body Lipoid nephrosis is a disease characterized by an insidious onset, a chronic course, edema, oliguria, albuminuria, changes in the protein and lipoids of the blood, and the deposit of lipoids in the kidney. It occurs alone, or in combination with diffuse glomerulonephritis, or with amyloid degeneration of the kidney By definition, there are not glomerular histologic changes or these are subtle (slight mesangial proliferation) When there is hypercellularity is more probable to find IgM deposits (IgM nephropathy) 2. Hyalinosis of splenic capsule HYALINOSIS is hyaline degeneration. Colloquially referred to as “sugar-coated spleen” or “icing-sugar spleen”, it results from the deposition of collagen on the capsular surface of the spleen, which may occur secondarily to inflammation of the peritoneal cavity. The spleen is commonly affected and often referred to as sugar-coated spleen. The liver and heart are also sometimes affected and referred to as frosted liver (or sugar-coated liver) and frosted heart respectively. 3. Pulmonary hemosiderosis Hemosiderosis is a term used for excessive accumulation of iron deposits called hemosiderin in the tissues. The lungs and kidneys are often sites of hemosiderosis. Pulmonary hemosiderosis (PH) is characterized by repeated episodes of intra-alveolar bleeding that lead to abnormal accumulation of iron as hemosiderin in alveolar macrophages and subsequent development of pulmonary fibrosis and severe anemia 4. Erosive gastritis Erosive gastritis is gastric mucosal erosion caused by damage to mucosal defenses. It is typically acute, manifesting with bleeding, but may be subacute or chronic with few or no symptoms. Erosion: loss of superficial epithelium above muscularis mucosa, accompanied by hemorrhage Variable changes include acute inflammatory infiltrate, extrusion of fibrinopurulent exudate into lumen, mucosal sloughing, regenerative changes in nearby epithelium Severe erosive disease may cause acute GI bleeds 5. Calculous cholecystitis Calculous cholecystitis develops when the main opening to the gallbladder, the cystic duct, gets blocked by a gallstone or a substance known as biliary sludge. Biliary sludge is a mixture of bile, a liquid produced by the liver that helps digest fats, and small cholesterol and salt crystals. Variety of histologic findings, including variable amounts of mononuclear cell predominant inflammation, mucosal changes including metaplasia, muscular hypertrophy and transmural fibrosis. 6. Fatty liver (“goose liver”, “foie gras”) Fatty liver disease (steatosis) is a common condition caused by having too much fat build up in your liver. There are two types of fatty liver disease: non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease. The primary risks include alcohol, type 2 diabetes, and obesity. Other risk factors include certain medications such as glucocorticoids, and hepatitis C. Fatty change represents the intracytoplasmatic accumulation of triglycerides (neutral fats). At the beginning, the hepatocytes present small fat vacuoles (liposomes) around the nucleus (microvesicular fatty change). In this stage, liver cells are filled with multiple fat droplets that do not displace the centrally located nucleus. In the late stages, the size of the vacuoles increases, pushing the nucleus to the periphery of the cell, giving characteristic signet ring appearance (macrovesicular fatty change). These vesicles are well-delineated and optically "empty" because fats dissolve during tissue processing. Large vacuoles may coalesce and produce fatty cysts, which are irreversible lesions. Macrovesicular steatosis is the most common form and is typically associated with alcohol, diabetes, obesity, and corticosteroids 7. Nutmeg liver (liver in chronic venous congestion) Nutmeg liver is the pathological appearance of the liver caused by chronic passive congestion of the liver secondary to right heart failure. The liver appears "speckled" like a grated nutmeg kernel, from the dilated, congested central veins (dark spots) and paler, unaffected surrounding liver tissue. When severe and longstanding, hepatic congestion can lead to cirrhosis, a state described as cardiac cirrhosis. Increased pressure in the sublobular branches of the hepatic veins causes an engorgement of venous blood, and is most frequently due to chronic cardiac lesions, especially those affecting the right heart, the blood being dammed back in the inferior vena cava and hepatic veins. Macroscopically, the liver has a pale and spotty appearance in affected areas, as stasis of the blood causes pericentral hepatocytes (liver cells surrounding the central venule of the liver) to become deoxygenated compared to the relatively better-oxygenated periportal hepatocytes adjacent to the hepatic arterioles. This retardation of the blood also occurs in lung lesions, such as chronic interstitial pneumonia, pleural effusions, and intrathoracic tumor. 8. Echinococcal liver cyst Cystic echinocccosis (CE), also known as hydatid disease, is caused by infection with the larval stage of Echinococcus granulosus, a ~2–7 millimeter long tapeworm found in dogs (definitive host) and sheep, cattle, goats, and pigs (intermediate hosts). Larval oncospheres are released from eggs and are transported to liver by portal vein, Oncospheres grow into cysts enlarging at slow pace of about 10 - 15 mm per year. Cysts are composed of protoscolices and daughter cysts. Hydatid cysts located most often in the liver and lungs, and less frequently in the bones, kidneys, spleen, muscles and central nervous system. Liver The histological picture of the hydatid cyst in liver resembled to that in the lung. The cyst had a laminated membrane revealing presence of numerous protoscolices from within or outside the brood capsule. The cyst wall was surrounded by the adventitial layer which in turn was surrounded by the inflammatory cells comprising of eosinophils, mononuclear cells and a few fibroblasts. The adjacent liver parenchyma showed haemorrhages. The laminated cysts wall was soetimes surrounded immediately by macrophage cell layer followed by a layer of infiltrating cells of eosinophils and mononuclear cells and then followed by fibroblastic cell layer 9. Cerebral cysticercosis Cerebral cysticercosis is the result of infestation of the brain with the larval stage of the intestinal tape worm Taenia Solium. Cysticerci may develop in skeletal and heart muscle, skin, subcutaneous tissues, the lungs, liver, and other tissues, including the oral mucosa. Grossly these cysts are variably sized ranging from few mm to few cm. and contain clear fluid. The cyst wall is pearly white and pulpy. Appears like soft coconut pulp. Scolex may be visible inside the cyst as tiny white nodule. The fluid later turns opaque as the cyst degenerates and finally can be calcified 10. Scleroma Systemic sclerosis (SSc) is a complex autoimmune connective tissue disease characterized by chronic and progressive tissue and organ fibrosis with broad patient-to-patient variability. Some risk factors are known and include combination of persistent Raynaud's phenomenon, steroid hormone imbalance, selected chemicals, thermal, or other injuries. A scleroma is a hardened patch of tissue in the skin or mucous membranes. It most often forms in the head and neck. The nose is the most common location for scleromas, but they can also form in the throat and upper lungs rinous pericarditis (“hairy heart”). Systemic sclerosis is characterized by three distinct pathologic processes: fibrosis, cellular/humoral autoimmunity, and specific vascular changes. Characterized by fibrosis, inflammation, increased collagen and vasculitis, Can be part of CREST syndrome (Calcinosis, Raynaud phenomenon, Esophageal involvement, Sclerodactyly, Telangiectasia) 11. Fibrinous pericarditis (“hairy heart”) In fibrinous pericarditis, the pericardial texture is rough, granular, and has many fibrous adhesions. There are a number of possible causes of fibrinous pericarditis, including myocardial infarction, uraemia, rheumatic fever, systems lupus erythematosis, irradiation of the chest, trauma and (rarely) infections. The pericardium has been opened to display its visceral and parietal layers and an enlarged heart. Both layers of pericardium are thickened and covered by a thick shaggy fibrinous exudate. 12. Primarily contracted kidney A diffusely scarred kidney in which the presence of abnormal fibrous tissue and ischemic atrophy leads to a reduction in its size. Causes of contracted kidney• Chronic GN (granular appearance) • Chronic pyelonephritis (U-shaped scars) • Benign nephrosclerosis (V-shaped scars). • Amyloidosis of the kidney. Irregular scarred cortical surface usually at poles, dilated and blunted calyces, Dilated ureter; retraction and destruction of papillae with "U” shaped scars 13. Hydronephrosis Hydronephrosis is swelling of one or both kidneys. Kidney swelling happens when urine can't drain from a kidney and builds up in the kidney as a result. This can occur from a blockage in the tubes that drain urine from the kidneys (ureters) or from an anatomical defect that doesn't allow urine to drain properly. Thin cortical rim of renal cortex due to atrophy, more calyceal dilation if incomplete obstruction, since glomerular filtration is not suppressed. 14. Scirrhous gastric cancer A rare type of stomach cancer that begins in the lining of the stomach and spreads to the muscles of the stomach wall. This causes the wall of the stomach to become thick, hard, and rubbery, which leads to trouble digesting food. Also called linitis plastica. The tumor demonstrates an infiltrative behavior, which instead of forming a bulky mass, rather causes thickening and stiffening of the intestinal wall with foreshortening, luminal stenosis, rigidity and lack of peristaltic activity (linitis plastica). 15. Uterine cancer Endometrial cancer is a type of cancer that begins in the uterus. The uterus is the hollow, pear-shaped pelvic organ where fetal development occurs. Endometrial cancer begins in the layer of cells that form the lining (endometrium) of the uterus. Endometrial cancer is sometimes called uterine cancer. Endometrial carcinoma most frequently arises in the corpus proper, but it may also originate in the lower uterine segment. There are no distinctive gross appearances to differentiate individual subtypes (cell type). In low-volume disease, it is common to find no evidence of residual disease after diagnostic endometrial curettage. Localized disease manifests as round, polypoid expansile masses that are friable and often hemorrhagic. Diffuse involvement of the endometrium may show an indurated-appearing surface without a visible exophytic component. Necrosis and hemorrhage may be seen. Foci of myometrial invasion generally appear grossly as well-demarcated gray-white areas that are lighter in color than the surrounding uninvolved myometrium. Extension from the surface lesion is commonly demonstrated. 6. Hodgkin lymphoma in para-aortic lymph nodes Hodgkin's lymphoma is a type of cancer that affects the lymphatic system, which is part of the body's germ-fighting immune system. In Hodgkin's lymphoma, white blood cells called lymphocytes grow out of control, causing swollen lymph nodes and growths throughout the body. 4 subgroups (nodular sclerosis, mixed cellularity, lymphocyte rich, lymphocyte depleted) with distinct clinical, morphologic and epidemiologic characteristics. nvolves lymph nodes (cervical > axillary, mediastinal, paraaortic). Section description: Effacement of nodal architecture Nodularity Mixed inflammatory background (small lymphocytes, neutrophils, eosinophils, histiocytes) May see scattered large Reed-Sternberg cells with multilobated nuclei and prominent nucleoli 17. Spleen in chronic myeloid leukemia Splenomegaly is the most common physical finding in patients with chronic myelogenous leukemia (CML). In more than 50% of the patients with CML, the spleen extends more than 5 cm below the left costal margin at time of discovery. Splenomegaly, most likely because of extramedullary hematopoiesis, remains one of the most important prognostic factors in CML patients at diagnosis. While the exact mechanisms leading to hypersplenism vary somewhat based on the causative aetiology, the underlying pathophysiologic changes are the same, including splenic congestion and hyper-functioning/hypertrophy. In the case of myeloproliferative disorders, this is due to a combination of 1) pooling of higher numbers of circulating red blood cells; and 2) extramedullary haemopoeisis (also known as myeloid metaplasia), which leads to an expansion of splenic reticular elements. 18. Melanoma metastases in liver Melanoma usually spreads through the blood circulation to the liver. The majority of liver metastases present as multiple tumors. Liver metastases are sometimes present when the primary cancer is diagnosed, or it may occur months or even years after the primary tumor is removed. Metastatic melanoma most often spreads to the lymph nodes, brain, bones, liver or lungs, and the additional symptoms experienced at this late stage will depend on where the melanoma has spread. Liver metastases may appear several years after resection of the primary tumor. FNA smears will show pleomorphic cells with intranuclear inclusions, prominent nucleoli, and cytoplasmic melanin (absent in amelanotic melanomas). Immunohistochemistry is sensitive and specific for the diagnosis of metastatic melanoma. Useful markers include HMB-45, S-100 protein, MART-1, and tyrosinase. 19. Aortic atherosclerosis and thrombosis Thromboembolism may occur when an atherosclerotic plaque from large or medium arteries becomes unstable, and superimposed thrombi embolize. The thromboemboli tend to be single and tend to lodge in small or medium arteries, resulting most often in stroke or transient ischemic attack. The surface is somewhat irregular, and there are areas of pale tan to white admixed with dark red areas. The thrombus often has the outlines of the artery in which it formed. Development of atherosclerosis follows a predictable path from initiation phase to progression and development of lipid rich atheromatous plaque to complications leading to ischemic events. Fatty streaks are flat yellow discoloration in the intima surface Early plaque is raised yellow, well defined lesion, focal in distribution and irregular in shape Complicated plaques show ulcers, protrusions and thrombus ( 20. Acute myocardial infarction Acute myocardial infarction is myocardial necrosis resulting from acute obstruction of a coronary artery. This is usually the result of a blockage in one or more of the coronary arteries. In the clinical context, myocardial infarction is usually due to thrombotic occlusion of a coronary vessel caused by rupture of a vulnerable plaque. While the vascular pathogenic mechanism is able to induce mainly coagulative necrosis, which is the specific necrosis of the acute myocardial infarction, the toxic action of the smoking compounds develops all types of necrosis with myocardial alterations variably combined among themselves. The gross morphologic appearance of a myocardial infarction can vary. Patterns include: • Transmural infarct - involving the entire thickness of the left ventricular wall from endocardium to epicardium, usually the anterior free wall and posterior free wall and septum with extension into the RV wall in 15-30%. Isolated infarcts of RV and right atrium are extremely rare. • Subendocardial infarct - multifocal areas of necrosis confined to the inner 1/3-1/2 of the left ventricular wall. These do not show the same evolution of changes seen in a transmural MI. Gross morphologic changes evolve over time as follows: Time from Onset Gross Morphologic Finding 18 - 24 Hours Pallor of myocardium 24 - 72 Hours Pallor with some hyperemia 3 - 7 Days Hyperemic border with central yellowing 10 - 21 Days Maximally yellow and soft with vascular margins 7 weeks White fibrosis 21. Chronic cardiac aneurysm A ventricular aneurysm is a blood-filled bulge that occurs as a result of an area of weakened tissue in the heart wall. In most cases, ventricular aneurysms form as a result of damage from a previous heart attack, though they may also be caused by defects present from birth. Most commonly, the pathogenesis of the aneurysms is due to noninflammatory, medial degeneration of the elastic aortic wall. However, inflammatory destruction secondary to syphilis, bacterial infection, noninfectious aortitis, or atherosclerosis can also be causative. Increased proteolysis of extracellular matrix proteins is probably the mechanism of aneurysm formation, Matrix metalloproteinase 1(interstitial collagenase), matrix metalloproteinase 2 (gelatinase A), matrix metalloproteinase 3 (stromelysin 1), matrix metalloproteinase 9 (gelatinase B), and matrix metalloproteinase 12 (macrophage metalloelastase) are capable of degrading essentially all components of arterial wall matrix (elastin, collagen, proteoglycans, laminin, fibronectin, etc.), and are present in elevated concentrations in aortic aneurysms, while there are decreased levels of tissue inhibitors of matrix metalloproteinases Gross description- An aneurysm is commonly defined as a localized dilatation exceeding the diameter of adjacent normal segments by 50%, 22. Concentric myocardial hypertrophy Concentric left ventricular hypertrophy is an abnormal increase in left ventricular myocardial mass caused by chronically increased workload on the heart, most commonly resulting from pressure overload-induced by arteriolar vasoconstriction as occurs in, chronic hypertension or aortic stenosis. Concentric cardiac hypertrophy occurs in response to pressure overload and is characterized by thickening of the left ventricle walls and minimal LV dilatation. Pressure overload occurs during isometric exercises, such as resistance training. There is marked concentric thickening of the left ventricular wall causing reduction in lumen size 23. Cyst after cerebral hemorrhage Arachnoid cysts are the most common type of brain cyst. They are often congenital, or present at birth (primary arachnoid cysts). Head injury or trauma can also result in a secondary arachnoid cyst. The cysts are fluid-filled sacs, not tumors. Gross description Variable size but may be vary large Thin transparent wall with clear, colorless fluid Cyst is distinct from leptomeninges and dura 24. Fibroplastic rheumatic endocarditis This is an infection of the inner lining of the heart, and may occur when rheumatic fever has damaged the heart valves. a post-infectious sequel of acute rheumatic fever resulting from an abnormal immune response to a streptococcal pharyngitis that triggers valvular damage. 25. Renal infarctions in periarteritis nodosa Polyarteritis nodosa is a rare multi-system disorder characterized by widespread inflammation, weakening, and damage to small and medium-sized arteries. Blood vessels in any organ or organ system may be affected, including those supplying the kidneys, heart, intestine, nervous system, and/or skeletal muscles. Although the exact cause of polyarteritis nodosa is not known, it is clear that an attack may be triggered by any of several drugs or vaccines or by a reaction to infections (either bacterial or viral) such as strep or staph infections or hepatitis B virus. PAN is characterized by segmental, transmural necrotizing inflammation of muscular arteries, most commonly at points of bifurcation. Unlike other vasculitic disorders, PAN does not involve postcapillary venules or veins. Lesions in all stages of development and healing are usually present. 26. Focal pneumonia, fibrinous pleuritis Depending on which lung lobe is affected, the pneumonia is referred to as upper, middle or lower lobe pneumonia. If there are several multi-lobe focal inflammations in the lungs, the term focal pneumonia is used. multifocal pneumonia can be caused by the same things that cause other types of pneumonia—viruses, bacteria, and fungi. The development of pneumonia requires that a pathogen reach the alveoli and that the host defenses are overwhelmed by microorganism virulence or by the inoculum size. Fibrinous pleuritis is the most common form of pleuritis. Viral- and bacterialinduced pneumonias will show a fibrinous pleuritis at the beginning and also localized to the areas of the underlying pneumonia. In viral infections, hemorrhage can occur later on, leading to fibrinous-hemorrhagic pleuritis 27. Lobar pneumonia (gray hepatization stage) Lobar pneumonia is a form of pneumonia characterized by inflammatory exudate within the intra-alveolar space resulting in consolidation that affects a large and continuous area of the lobe of a lung. Most cases of lobar pneumonia are community acquired and caused by Streptococcus pneumoniae. Other causes include Klebsiella pneumoniae, Legionella pneumophila, Haemophilus influenzae, and Mycobacterium tuberculosis. Lobar pneumonia is diffuse consolidation involving the entire lobe of the lung. Its evolvement can be broken down into 4 stages as follows: Congestion: This stage is characterized by grossly heavy and boggy appearing lung tissue, diffuse congestion, vascular engorgement, and the accumulation of alveolar fluid rich in infective organisms. There are few red blood cells (RBC) and neutrophils at this stage. Red hepatization: Marked infiltration of red blood cells, neutrophils, and fibrin into the alveolar fluid is seen. Grossly, the lungs appear red and firm akin to a liver, hence the term hepatization. Gray hepatization: The RBC break down and is associated with fibrinopurulent exudates causing a red to gray color transformation. Resolution: Characterized by clearing of the exudates by resident macrophages with or without residual scar tissue formation. 28. Chronic obstructive pulmonary emphysema Emphysema, or pulmonary emphysema, is a lower respiratory tract disease, characterised by air-filled spaces (pneumatoses) in the lung, that can vary in size and may be very large. The spaces are caused by the breakdown of the walls of the alveoli and they replace the spongy lung parenchyma. Smoking (the main cause) Exposure to air pollution, such as chemical fumes, dust, and other substances. Irritating fumes and dusts at work. A rare, inherited form of the disease called alpha 1-antitrypsin (AAT) deficiency-related pulmonary emphysema or early onset pulmonary emphysema. Emphysema is pathologically defined as an abnormal permanent enlargement of air spaces distal to the terminal bronchioles, accompanied by the destruction of alveolar walls and without obvious fibrosis. Gross description Hyperinflation or ballooning due to entrapment of the air from airway obstruction Lungs may be overlapping the heart Upper lobes are more involved Centriacinar: sparse empty spaces with pigmentation (anthracosis) corresponding enlarged airspaces Panacinar: airspaces are more or less evenly inflated throughout the secondary lobules Paraseptal: inflated subpleural airspaces with thin walls Bullous emphysema Descriptive term regarding emphysematous lung with visible bullae upon gross examination Bulla: an air filled space of 1 cm in diameter within the lung which has developed because of emphysematous destruction of the lung parenchyma 29. Chronic gastric ulcer A peptic ulcer is a sore on the lining of your stomach, small intestine or esophagus. A peptic ulcer in the stomach is called a gastric ulcer. The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stress and spicy foods do not cause peptic ulcers. The continuous mucosal injury due to long-standing infection, leads to atrophy of stomach. This continuous pathological process results in erosion or ulceration of the mucosa leading to the destruction of the glandular layer and followed by fibrous replacement. 30. Phlegmonous appendicitis When an inflamed appendix perforates, the infection is localized by the omentum and bowel loops which present as an appendiceal mass or phlegmon. Appendiceal phlegmon is considered to be sequelae to acute appendicitis which presents as an appendiceal mass composed of the inflamed appendix, the adjacent bowel loops, and the greater omentum. Appendicitis is thought to result from obstruction of the appendiceal lumen, typically by lymphoid hyperplasia but occasionally by a fecalith, foreign body, or even worms. Gross description Gross and microscopic extent of inflammation may not correlate Inflammation may involve entire appendix or only a segment Appendix may appear grossly normal when inflammation is limited to the mucosa and submucosa Appendix appears swollen and erythematous when inflammation extends into the muscularis propria When the serosa is affected, a purulent exudate appears Cut surface may show hyperemia or intraluminal or intramural abscess Appendiceal wall may be completely necrotic in gangrenous appendicitis Perforation in severe cases 31. Macronodular cirrhosis Cirrhosis is a condition in which your liver is scarred and permanently damaged. Scar tissue replaces healthy liver tissue and prevents your liver from working normally. As cirrhosis gets worse, your liver begins to fail. MACRONODULAR CIRRHOSIS: Larger nodules separated by wider scars and irregularly distributed throughout the liver usually due to an infectious agent such as viral hepatitis which does not diffuse uniformly throughout the liver. Gross description Multiple regenerative nodules throughout the entire liver, separated by bridging fibrosis 32. Biliary cirrhosis Primary biliary cholangitis, previously called primary biliary cirrhosis, is a chronic disease in which the bile ducts in your liver are slowly destroyed. Primary biliary cirrhosis is considered an autoimmune disease, which means it is caused by the body's own immune system mistakenly attacking itself. Gross description Hepatomegaly early; cirrhosis late 33. Esophageal varices in portal hypertension Esophageal varices are enlarged veins in the esophagus. They're often due to obstructed blood flow through the portal vein, which carries blood from the intestine, pancreas and spleen to the liver. Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach (esophagus). Causes of esophageal varices include: Severe liver scarring (cirrhosis). A number of liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cirrhosis — can result in cirrhosis. Blood clot (thrombosis). Esophageal varices develop when normal blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren't designed to carry large volumes of blood. The vessels can leak blood or even rupture, causing life-threatening bleeding. Gross description Varices may protrude into lumen, mucosa may be normal or inflamed 34. Kidney in acute renal failure Acute kidney injury (AKI), also known as acute renal failure (ARF), is a sudden episode of kidney failure or kidney damage that happens within a few hours or a few days. AKI causes a build-up of waste products in your blood and makes it hard for your kidneys to keep the right balance of fluid in your body. Causes of kidney failure. Kidney failure can be the result of several conditions or causes. According to the National Kidney Foundation, the two most common causes are high blood pressure and diabetes. 35. Chronic pyelonephritis Chronic pyelonephritis is continuing pyogenic infection of the kidney that occurs almost exclusively in patients with major anatomic abnormalities. Chronic forms of the condition are more common in people with urinary obstructions. These can be caused by UTIs, vesicoureteral reflux, or anatomical anomalies. Chronic pyelonephritis is associated with progressive renal scarring, which can lead to end-stage renal disease (ESRD). For example, in reflux nephropathy, intrarenal reflux of infected urine is suggested to induce renal injury, which heals with scar formation Gross description Irregular scarred cortical surface usually at poles, dilated and blunted calyces Dilated ureter; retraction and destruction of papillae with "U” shaped scars 36. Rapidly progressive glomerulonephritis (“large mottled kidney”) Rapidly progressive glomerulonephritis (RPGN) is a disease of the kidney characterized clinically by a rapid decrease in the glomerular filtration rate (GFR). The most common occurrence is in systemic lupus erythematosus. Other associated diseases include inflammatory bowel disease, sclerosing cholangitis, autoimmune hepatitis, rheumatoid arthritis, and Felty syndrome. Pathophysiology comprises a specific set of renal diseases in which an immunologic mechanism triggers inflammation and proliferation of glomerular tissue that can result in damage to the basement membrane, mesangium, or capillary endothelium. 37. Purulent meningitis Purulent meningitis refers to inflammation of leptomeninges occurring along with infection of the subarachnoid space by various purulent bacteria. Clinically, purulent meningitis usually manifests as fever, vomiting, headache, and meningeal irritation. The most common pathogens are Pneumococcus, Hemophilus influenzae, and Staphylococcus. Bacterial meningitis is characterized by the entry of bacteria into the cerebrospinal fluid (CSF) and bacterial growth in this compartment leading to inflammation within the CSF and the adjacent brain tissue. 38. Adrenal hemorrhage (Waterhouse-Friderichsen syndrome) Waterhouse-Friderichsen syndrome (WFS) is a group of symptoms resulting from the failure of the adrenal glands to function normally as a result of bleeding into the gland. WFS is caused by severe infection with meningococcus bacteria or other bacteria, such as: Group B streptococcus. Pseudomonas aeruginosa. Streptococcus pneumoniae. • Hemorrhagic necrosis of adrenal glands, usually due to bacteremia, classically Neisseria meningitides; also Pseudomonas aeruginosa, pneumococci, staphylococcus and historically Haemophilus influenzae • Less common causes are burns, cardiac failure, hypothermia and birth trauma Gross description Glands are enlarged and hemorrhagic with extensive cortical and medullary necrosis 39. Pneumatosis of small intestine in E. coli infection Pneumatosis intestinalis (PI) refers to the presence of gas within the wall of the small or large intestine. Pneumatosis is found secondary to mucosal disruption presumably due to over-distention from peptic ulcer, pyloric stenosis, annular pancreas, and even to more distal obstruction. Disruption can also be caused by ulceration, erosions, or trauma, including the trauma of child abuse. Gross description Polypoid grape-like masses protrude through mucosa Soft, bluish and often sessile, "bubble wrap" crackling noise while handling the specimen 40. Diphtheritic colitis in dysentery Colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease (IBD) and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon. Pseudomembranous colitis is inflammation (swelling, irritation) of the large intestine. In many cases, it occurs after taking antibiotics. Using antibiotics can cause the bacterium Clostridium difficile (C. diff) to grow and infect the lining of the intestine, which produces the inflammation Gross description Yellow-white mucosal plaques or pseudomembranes; may resemble polyps or aphthoid ulcers of Crohn's disease 41. Septic endocarditis Endocarditis occurs when germs, usually bacteria, enter your bloodstream, travel to your heart, and attach to abnormal heart valves or damaged heart tissue. Fungi or other germs also may cause endocarditis The pathophysiology of infective endocarditis comprises at least three critical elements: preparation of the cardiac valve for bacterial adherence, adhesion of circulating bacteria to the prepared valvular surface, and survival of the adherent bacteria on the surface, with propagation of the infected vegetation. Gross description Vegetations are seen attached to atrial aspect of AV valves and ventricular aspect of semilunar valves in relation to the line of apposition Large vegetations may extend into adjacent parts of cusp or leaflets, chordae tendinae or sinus of valsalva Largest vegetation is seen in fungal infections Colour varies from red to pink to yellow and may be soft or friable or firm Surface is smooth, often irregular granular Lesions may calcify with time after antibiotic treatment 42. Catheter sepsis: thrombo-endocarditis of right atrium предсердия Non-bacterial thrombotic endocarditis (NBTE) is an uncommon pathological situation, which involves the presence of bland, fibrin-platelet thrombi. It usually occurs at the endocardium of cardiac valves, in association with endothelial injury and a hypercoagulative state. Pathological findings showed that NBTE caused by an operative scar on the endocardium of the right atrium and sustained rheological stress in the right atrium due to compression from pectus excavatum lead to recurrent thrombus formation. 43. Primary pulmonary tuberculosis complex with a mixed type of progression and formation of primary cavity Primary tuberculosis is characterized by a pulmonary parenchymal focus of infection that is typically associated with regional hilar or mediastinal lymphadenopathy and that develops after initial exposure to tuberculosis. You can get TB by breathing in air droplets from a cough or sneeze of an infected person. The resulting lung infection is called primary TB. Most people recover from primary TB infection without further evidence of the disease. The infection may stay inactive (dormant) for years. TB cavity formation occurs usually in the apices of the lungs or in the apical segment of the lower lobes. 44. Miliary tuberculosis Miliary tuberculosis is a potentially life-threatening type of tuberculosis that occurs when a large number of the bacteria travel through the bloodstream and spread throughout the body. Caused by the airborne bacteria Mycobacterium tuberculosis. Following exposure and inhalation of TB bacilli in the lung, a primary pulmonary complex is established, followed by development of pulmonary lymphangitis and hilar lymphadenopathy. Mycobacteremia and hematogenous seeding occur after the primary infection. 45. Tuberculosis of kidney Renal TB is typically a disease of young and middle-aged adults. Most cases of renal TB arise by secondary hematogenous spread of bacilli to the renal cortex from pulmonary lesions either at the time of initial TB infection or due to late breakdown of an old caseous focus. Tuberculosis of the kidney and urinary tract is, like other forms of the disease, caused by members of the Mycobacterium tuberculosis complex. The pathogenesis of renal tuberculosis begins with the initial localization of the tubercle bacilli in the cortical glomeruli causing mechanical stress which lead to alteration in cell morphology, increased rate of protein synthesis and proliferation of resident glomerular cells as well as the infiltrating blood borne cells. Gross description Multiple cavities filled with yellow friable necrotic material 46. Infantile polycystic kidney disease ("sponge kidney") Medullary sponge kidney, also known as Cacchi-Ricci disease, is a birth defect where changes occur in the tubules, or tiny tubes, inside a fetus' kidneys. Consists of fluid-filled kidney cysts that may make the kidneys too big, or enlarged. caused by a genetic change in the PKHD1 gene and is inherited in an autosomal recessive manner. ARPKD is caused by mutation in the PKHD1 gene which codes for a protein called fibrocystin. Fibrocystin is thought to have a role in renal collecting duct and biliary duct differentiation. Gross description Markedly enlarged kidneys with smooth surface Small cysts in cortex and medulla Dilated channels are perpendicular to cortical surface Cysts are present in medulla (collecting ducts) 47. Multiple congenital malformations Multiple congenital anomalies (MCAs) are defined as two or more unrelated major structural malformations that cannot be explained by an underlying syndrome or sequence. The two most common genetic causes of congenital anomalies are single-gene defects and chromosomal abnormalities. 48. Hydro-microcephaly in toxoplasmosis Congenital toxoplasmosis is a disease that occurs in fetuses infected with Toxoplasma gondii, a protozoan parasite, which is transmitted from mother to fetus. It can cause miscarriage or stillbirth. gondii occurs primarily from ingestion of inadequately cooked meat containing cysts or from ingestion of oocysts derived from food or water contaminated with cat feces. Toxoplasma gondii infects a variety of vertebrate hosts, including humans. Transplacental passage of the parasite leads to congenital toxoplasmosis. A primary infection during the first weeks of gestation causes vertical transmission at low rate, although it causes major damage to the embryo. Babies born with toxoplasmosis can develop hydrocephalus, when cerebrospinal fluid that normally circulates through the brain's ventricles backs up and damages the brain. 49. Multiple uterine fibromyoma Fibroids range in size from seedlings, undetectable by the human eye, to bulky masses that can distort and enlarge the uterus. You can have a single fibroid or multiple ones. In extreme cases, multiple fibroids can expand the uterus so much that it reaches the rib cage and can add weight. Causes: Genetic changes. Many fibroids contain changes in genes that differ from those in typical uterine muscle cells. 50. Hydatidiform mole A molar pregnancy — also known as hydatidiform mole — is a rare complication of pregnancy characterized by the abnormal growth of trophoblasts, the cells that normally develop into the placenta. There are two types of molar pregnancy, complete molar pregnancy and partial molar pregnancy. A molar pregnancy is caused by an abnormally fertilized egg 51. Fetal asphyxia Perinatal asphyxia, or birth asphyxia, results from an inadequate intake of oxygen by the baby during the birth process — before, during or just after birth. Some causes of birth asphyxia include: Too little oxygen in the mother's blood before or during birth. Problems with the placenta separating from the womb too soon. Very long or difficult delivery. The pathophysiology of asphyxia generally results from interruption of placental blood flow with resultant fetal hypoxia, hypercarbia, and acidosis. 52. Hepatosplenomegaly in hemolytic disease of newborn Hepatosplenomegaly (HPM) is a disorder where both the liver and spleen swell beyond their normal size, due to one of a number of causes. infection, such as hepatitis C, syphilis, or sepsis from a significant bacterial infection. chronic liver disease with portal hypertension. cancers, such as amyloidosis or sarcoidosis. HIV. Hepatosplenomegaly in a young child can be an ominous physical finding, potentially representing a metabolic, malignant, or infectious process. Common causes of hepatosplenomegaly in children can be summarized as follows: newborns: storage disorders and thalassemia. infants: liver unable to process glucocerebroside, which can lead to severe damage to the central nervous system. older children: malaria, kala azar, enteric fever, and sepsis 53. Cephalohematoma Cephalohematoma is an accumulation of blood under the scalp. This type of birth injury occurs when pressure on a baby's head ruptures blood vessels in the scalp. The cause of a cephalohematoma is rupture of blood vessels crossing the periosteum due to the pressure on the fetal head during birth. During the process of birth, pressure on the skull or the use of forceps or a vacuum extractor rupture these capillaries resulting in a collection of serosanguineous or bloody fluid. 54. Wilms’ tumor (nephroblastoma) Wilms tumor (also called Wilms' tumor or nephroblastoma) is a type of childhood cancer that starts in the kidneys. It is the most common type of kidney cancer in children. Doctors have found that some Wilms tumors have changes in specific genes: A small number of Wilms tumors have changes in or loss of the WT1 or WT2 genes, which are tumor suppressor genes found on chromosome 11. Changes in these genes and some other genes on chromosome 11 can lead to overgrowth of certain body tissues. Gross description Usually large, solitary, spherical mass, sharply demarcated from the renal parenchyma, distorting kidneys contours In ~10% multinodular In primarily operated cases, tumor is gray-white or pink-gray in color, lobulated, soft and friable Some tumors may have a prominent cystic appearance In pretreated cases, hemorrhage and necrosis are usually extensive