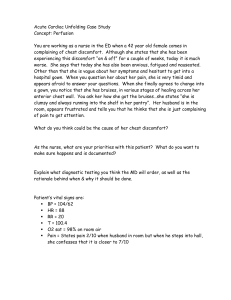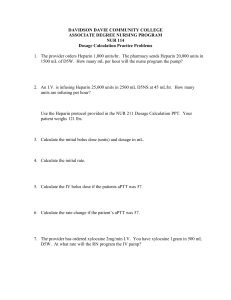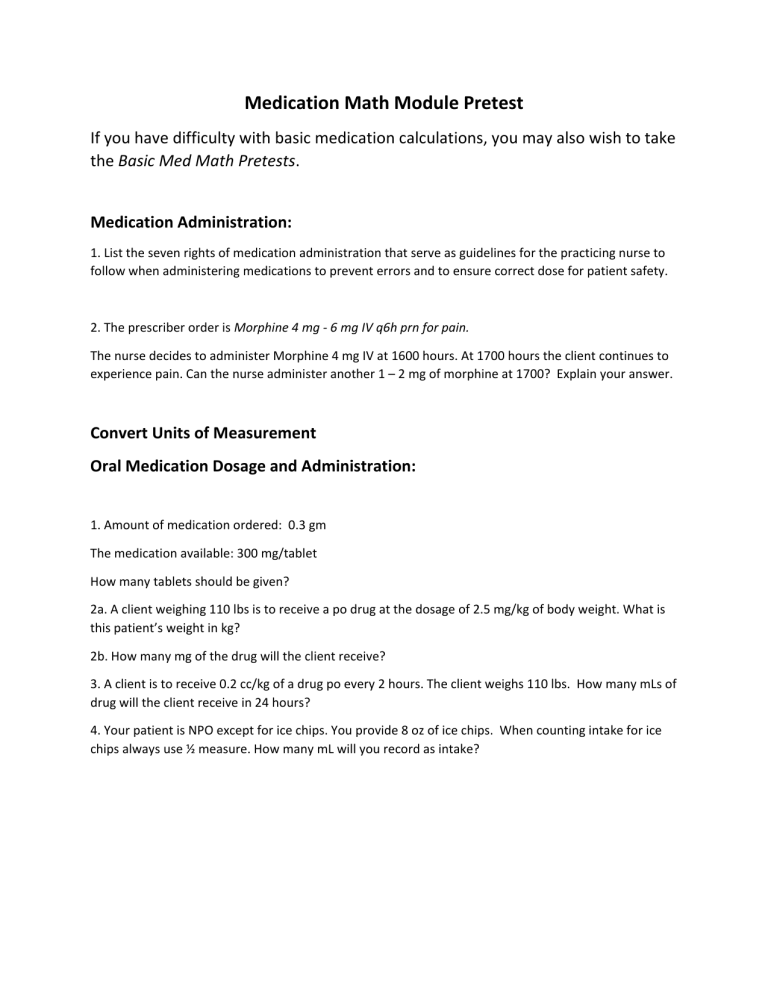
Medication Math Module Pretest If you have difficulty with basic medication calculations, you may also wish to take the Basic Med Math Pretests. Medication Administration: 1. List the seven rights of medication administration that serve as guidelines for the practicing nurse to follow when administering medications to prevent errors and to ensure correct dose for patient safety. 2. The prescriber order is Morphine 4 mg - 6 mg IV q6h prn for pain. The nurse decides to administer Morphine 4 mg IV at 1600 hours. At 1700 hours the client continues to experience pain. Can the nurse administer another 1 – 2 mg of morphine at 1700? Explain your answer. Convert Units of Measurement Oral Medication Dosage and Administration: 1. Amount of medication ordered: 0.3 gm The medication available: 300 mg/tablet How many tablets should be given? 2a. A client weighing 110 lbs is to receive a po drug at the dosage of 2.5 mg/kg of body weight. What is this patient’s weight in kg? 2b. How many mg of the drug will the client receive? 3. A client is to receive 0.2 cc/kg of a drug po every 2 hours. The client weighs 110 lbs. How many mLs of drug will the client receive in 24 hours? 4. Your patient is NPO except for ice chips. You provide 8 oz of ice chips. When counting intake for ice chips always use ½ measure. How many mL will you record as intake? Percentages and Fractions: 1. Joe’s weight prior to surgery was 80 kg. Following two weeks of bed rest, his weight was 84 kg. What is the percentage increase in Joe’s weight? a) Calculate the increase of weight in kilograms (kg). b) Calculate the percent of change. c) Change ¼% to a fraction. 2. The prescriber orders Ensure nutritional supplement: 1000 mL at 3/4 strength of Ensure via percutaneous endoscopic gastrostomy (PEG) to be given over 12 hours. How much of the Ensure (in mL) will you use to prepare the 1000 mL 3/4 strength solution? Round answer to a whole number. Calculate Intake and Output: At the end of your day shift, you are calculating the intake and output for your patient. Your patient went for an early morning chest x-ray so you completed your initial assessment at 0800 hours and it is now 1400 hours. At the time of your assessment, your patient had an IV of Lactated Ringer’s at 100 ml/hr. You reduced the rate to 30 ml/hr at 1200 hours as per the nurse practitioners (NP) orders. The patient also had one IV medication at 1000 hours with a volume of 100 ml and another IV medication at 1200 hours with a volume of 50ml. The patient had a cup of coffee at breakfast (125 ml) and a glass of orange juice (140ml). For lunch, the patient drank 2 glasses of water (250 ml/one glass). You checked the urinary catheter drainage bag at 1400 hours and there was 650 ml of urine in the drainage bag. 1. What is the patient’s total intake (ml) from 0800-1400 hours? 2. What is the patient’s total output (ml) from 0800-1400 hours? 3. What is the net volume (ml)? 4. What percentage (%) of the patient’s total intake from 0800-1400 hours is from the IV Lactated Ringer’s infusion (round answer to whole number)? 5. What is the patient’s average hourly urine output (ml/hr) from 0800-1400 hours? Round answer to the nearest whole number. Parenteral Medications: 1. The prescriber orders Vitamin B12 (cyanocobalamin) 0.5 mg IM. The medication is provided in a vial containing 1000 mcg/mL. How many mLs is required for the doctor’s order of 0.5 mg? 2.What size of syringe will you use 1mL or 3mL? 3. A vial of epinephrine is labeled “1:1000” (Buchholtz, 2016, figure 8-8). What does the ratio 1:1000 indicate? Reconstitution of Medication: Use the instructions below for reconstitution of cefazolin (Buchholz, 2016, figure 5-6). 1. You will be giving cefazolin 0.3 g IM. The only supply that you have is the 500mg gram vile size. What is the total available volume in the 500 mg vial? 2. What diluent will you use to reconstitute, and how much diluent will you add? 3. Once mixed with the diluent, how long is this drug stable for in a refrigerator? 4. How many mL of the drug will you give as per order of 0.3g IM if you reconstituted the vial size of 500 mg. Round answer to one decimal place. Intravenous Flow Rates: 1. Calculate the intravenous flow rate of 500mL in 12 hr. 2. Calculate the flow rate for ceftriaxone 1500 mg IV in 100 mL mini-bag over 45 minutes. 3. Infuse IV medication in 50 mL NS in 20 minutes. The drop factor is 60 gtts/mL. What flow rate (in drops per minute) should the IV be set? 4. An IV of 1000 mL NS is to infuse from 0700 to 1500 (8hr) the flow rate is ordered at 125 mL/hr. In 5 hours, you notice that 700 mL has infused. Recalculate the flow rate for the remaining solution. 5. Determine the percentage of change. Weight-based Calculations: The medication order reads: Dopamine 2 mcg/kg/min. The solution available is 400 mg in 250 mL D5W. The patient weighs 200 lbs. Calculate the IV flow rate in mL/hr. 1. Convert the patient’s weight to kg. 2. Determine the dosage in mcg per minute. 3. Convert mcg per minute to mcg per hour. 4. Convert mcg/hr to mg per hour. Round answer to one decimal place. 5. Determine the IV flow rate in mL/hr. Titration/Heparin: A patient weighing 80 kg has an order for heparin 3500 units in 500 mL of D5W to infuse at a rate of 40 mL per hour. 1. What is the concentration of heparin per mL of D5W? 2. How many units of heparin will the patient receive in one hour? A patient with a swollen left leg has been diagnosed with a deep vein thrombosis. The patient weighs 80kg. The patient is prescribed heparin therapy according the venous thromboembolism (VTE) heparin protocol. Heparin Protocol: For patients who have a venous thromboembolism (VTE) or pulmonary embolism 1. Prior to commencing therapy: PTT, INR, CBC, platelet count. 2. Heparin bolus 80 units/kg 3. Start initial maintenance Heparin infusion 25,000 units in 500 ml D5W (50 units/ml) at 18 units/kg/hr. 4. PTT 6 hours after bolus administered. 5. Adjust Heparin infusion according to nomograph below. 6. CBC daily (while on Heparin). Notify physician if platelets < 100X10x9/L 7. PTT every 6 hours until 2 consecutive therapeutic PTT(s), then PTT daily. 8. Warfarin daily as ordered. If not started, why not? 9. Daily PT(INR) while on Warfarin. 10. Physician or designate to consider discontinuing Heparin when PT(INR) has been HEPARIN ADJUSTMENT NOMOGRAPH PTT (seconds) < 35 46 – 57 58 – 98 RATE CHANGE +4 Units/kg/hr. Rebolus with 80 IU/kg +2 Units/kg/hr. Rebolus with 40 IU/kg +1 Units/kg/hr. No change 99 – 120 >120 -1 Units/kg/hr. -2 Units/kg/hr 35 – 45 REPEAT PTT 6 hours 6 hours Repeat q6h Repeat q6h until 2 consecutive therapeutic PTT, then PTT daily 6 hours 6 hours 1. Calculate the heparin bolus dosage in units. 2. Calculate the initial infusion rate in units per hour. 3. Calculate the initial infusion rate in mL per hour. 4. Adjust the hourly infusion rate up or down based on subsequent PTT results. The current PTT result is 37 seconds, 6 hours after heparin therapy was initiated. What should the nurse do now? 5. Calculate the dosage of heparin re-bolus. How many units will the re-bolus be? 6. Calculate the infusion rate increase for this patient according to the protocol. How many units per hour should the increase be? 7. Calculate the adjustment in the hourly infusion rate (mL/hr). 8. What is the new heparin infusion rate?