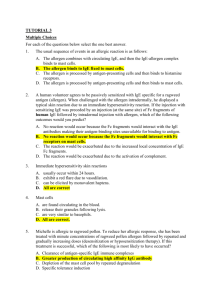
THE IMMUNE SYSTEM, FOURTH EDITION CHAPTER 14: IgE-MEDIATED IMMUNITY AND ALLERGY 14–1 a. b. c. d. e. Which of the following are matched correctly? (Select all that apply.) type I hypersensitivity: IgE type II hypersensitivity: IgG type III hypersensitivity: immune complexes type IV hypersensitivity: IgG type IV hypersensitivity: delayed-type hypersensitivity. 14–2 a. b. c. d. e. Which of the following are associated with soluble antigen? (Select all that apply.) type I hypersensitivity type II hypersensitivity type III hypersensitivity type IV hypersensitivity mast-cell activation. 14–3 Match the term in column A with its description in column B. Column A ___ a. delayed-type hypersensitivity Column B 1. innocuous environmental antigen ___ b. hygiene hypothesis 2. type IV hypersensitivity ___ c. allergy 3. a state of hypersensitivity ___ d. immediate hypersensitivity 4. type I hypersensitivity ___ e. allergen 5. epidemic of allergy 14–4 a. b. c. d. Which of the following is not mediated by antibodies? type I hypersensitivity type II hypersensitivity type III hypersensitivity type IV hypersensitivity. 14–5 a. b. c. d. Which of the following is associated with type III hypersensitivity? nickel recombinant human insulin plant oil mouse-derived monoclonal antibody 1 e. helminth infection. 14–6 _____ hypersensitivity reactions interact with soluble epitopes and not cell-surface associated epitopes. a. type I and II b. type I and III c. type I and IV d. type II and III e. type II and IV f. type III and IV. 14–7 Identify four different ways in which an individual may come into contact with an allergen and provide two examples of allergens for each type of contact. 14–8 A. Describe in detail the mechanism responsible for mast-cell activation during a type I hypersensitivity reaction. B. What are the products of mast-cell activation? 14–9 Adaptive immune responses targeted at infections by helminth worms and other parasitic multicellular animals employ all of the following except _____. (Select all that apply.) a. CD8 T cells b. IgE c. eosinophils d. mast cells e. CD4 TH2 cells f. basophils g. neutrophils h. IL-4. 14–10 During a primary immune response IgM sometimes switches to IgE. Which of the following best describes the consequence of this early switch? a. The B cell would switch again to IgG3. b. The B cell would remain in the germinal center but would not differentiate into a plasma cell. c. The B cell would die by apoptosis. d. The IgE produced would have low affinity for antigen. 14–11 a. b. c. d. e. Which of the following regarding FcεRI is false? It is expressed on the surface of mast cells and basophils. It is a low-affinity receptor involved in type I hypersensitivity reactions. It binds to IgE in the absence of antigen. It is a membrane-bound tetramer. It contains signaling components that re activated following antigen cross-linking. 14–12 A. Explain why it is essential that FcεRI and Fcε RII are not able to bind simultaneously to 2 the same IgE molecule. B. Why does simultaneous binding not occur? 14–13 The sheddase _____ cleaves FcεRII on the cell surface, resulting in the production of monomeric and trimeric forms of FcεRII. a. cathepsin G b. CR2 c. eotaxin d. major basic protein e. ADAM10. 14–14 All of the following are released immediately by mast cells after FcεRI cross-linking except _____. a. heparin b. eicosanoids c. neutral proteases d. histamine e. TNF-α. 14–15 Lipid mediators produced by activated mast cells include which of the following? (Select all that apply.) a. platelet-activating factor b. cathepsin G c. chymase d. leukotrienes e. carboxypeptidase f. prostaglandins. 14–16 All of the following are biological effects mediated by the products of mast cells except _____. a. chemotaxis of neutrophils, eosinophils, and effector T cells b. growth factor secretion c. smooth muscle contraction d. connective tissue remodeling e. All of the above are mediated by mast cells. 14–17 a. b. c. d. e. Identify the mismatched pair. TNF-α: immediate release from mast cells mucosal mast cell production: T-cell immunodeficiencies connective tissue mast cells: chymotryptase lipid mediator: prostaglandins leukotrienes: increase vascular permeability. 14–18 Prostaglandin D2 (PGD2) enhances all of the following except _____. a. smooth muscle contraction b. chemotaxis of neutrophils 3 c. d. increased vascular permeability vasodilation. 14–19 Which of the following directly inhibits the cyclooxygenase pathway by inhibiting the activity of prostaglandin synthase? a. ADAM10 b. experimental anti-IgE c. aspirin (acetyl salicylate) d. chymotryptase e. ADAM33. 14–20 a. b. c. d. e. _____ released by TH2 cells promotes an elevated level of eosinophils in the circulation. IL-4 IL-13 TNF-α FcγRII IL-5. 14–21 A. Explain the importance of allergens having protease activity in the context of antigenspecific T-cell activation. B. Provide a specific example of a major allergen that has protease activity. 14–22 Match the physical effects of IgE-mediated mast-cell degranulation in column A with the tissue exposed to the allergen in column B. Column A Column B ___ a. decrease in blood pressure 1. respiratory tract ___ b. diarrhea 2. heart and vascular system ___ c. swelling of tissues 3. gastrointestinal tract ___ d. constriction of the throat ___ e. wheezing ___ f. vomiting ___ g. violent bursts of sneezing 14–23 Explain briefly how penicillin initiates a type I hypersensitivity response. 14–24 A. Explain how erythrocytes become coated with complement component C3b during an 4 allergic reaction to penicillin. B. Why is this important to the mechanism by which IgE antibodies are produced? 14–25 Why are antihistamines used to treat allergic rhinitis and allergic asthma? What symptoms of each disease, respectively, do they alleviate. 14–26 A. Describe two ways in which the immunoglobulins acting as antigen receptors on the surface of a mast cell differ from the immunoglobulins acting as the antigen receptors on the surface of a B cell. B. What is the essential difference in response of these two cell types when antigen binds to these surface immunoglobulins. 12–27 Some allergies can be treated by a procedure called desensitization. A. Explain two current approaches to desensitization. B. Explain the main disadvantage associated with each. 14–28 Give three ways in which a susceptible person can help to minimize the risk of having an allergic reaction. 14–29 How do mast cells contribute to innate immunity? 14–30 What are the effects of histamine binding to the H1 receptor on smooth muscle, mucosal epithelia, and the endothelial cells of blood vessels. 14–31 a. b. c. d. e. The antigens that provoke hypersensitivity reactions are referred to as T-independent antigens superantigens subunit vaccines attenuated vaccines allergens. 14–32 a. b. c. d. e. Which of the following allergens is not likely to be encountered through inhalation? plant pollen metals animal dander mold spores house dust mite feces. 14–33 _____ express FcεRI and contain granules containing inflammatory mediators. (Select all that apply.) a. macrophages b. activated eosinophils c. mast cells d. natural killer cells e. basophils. 5 14–34 Match the mast cell product in column A with its biological effect in column B. Column A Column B ___ a. IL-4 1. activates endothelium ___ b. CCL3 2. amplifies TH2-cell response ___ c. TNF-α 3. increases vascular permeability ___ d. histamine 4. connective tissue matrix remodeling ___ e. tryptase 5. chemotaxis 14–35 Aspirin (acetyl salicylate) inhibits prostaglandin synthesis by binding irreversibly to prostaglandin synthase, the first enzyme in the _____ pathway. a. cyclooxygenase b. carboxypeptidase c. metalloprotease d. lipooxygenase e. peroxidase. 14–36 a. b. c. d. e. Which of the following is associated with eosinophilia? (Select all that apply.) IL-5-induced proliferation endocardium damage neuropathy B-cell lymphoma decreased bone marrow function. 14–37 Which of the following genetic polymorphisms is associated with a predisposition to asthma? (Select all that apply.) a. promoter variants of IL-5 b. structural variant of IgG receptor c. HLA class II allotypes d. β2-adrenergic receptor variant e. ACOX5 (5-lipoxygenase). 14–38 a. b. c. d. e. The wheal-and-flare inflammatory reaction is an example of an immediate type I allergic response a late-phase type I allergic response a late-phase type IV allergic response an immediate type III allergic response a late-phase type III allergic response. 14–39 Which of the following tests is used to determine whether a particular allergen is responsible for asthma? a. measure wheal-and-flare diameter after intradermal injection of allergen b. measure Arthus reaction diameter after intradermal injection of allergen c. inject a controlled amount of allergen intradermally and observe urticaria d. measure peak expiratory flow rate (PEFR) following inhalation of allergen e. measure eosinophils in nasal secretions following inhalation of allergen. 6 14–40 a. b. c. d. e. Which of the following are consequences of anaphylactic shock? (Select all that apply.) smooth muscle contraction immune complex deposition on blood vessels loss of blood pressure constriction of airways complement activation. 14–41 During the course of a successful desensitization process, the patient’s antibodies will change from an _____isotype to an _____ isotype. a. IgG4:IgE b. IgE:IgM c. IgA:IgM d. IgG1:IgG4 e. IgE:IgG4. 14–42 Which of the following are potential means by which type I allergic reactions can be managed or treated? (Select all that apply.) a. Use antihistamines to block histamine binding to H1 histamine receptors. b. Use corticosteroids to suppress inflammation. c. Desensitize the patient by feeding them allergen and skewing the immune response from an IgE to an IgA response. d. Anergize allergen-specific T cells through vaccination with allergen-derived peptides. e. Administer Il-4, IL-5, or IL-1β to promote TH1 responses. f. Block high-affinity IgE receptors to prevent mast-cell degranulation. 14–43 Anita Garcia, 17 years old, and her roommate Rosa Rosario were celebrating a friend’s birthday at a dessert buffet at a local restaurant when Anita developed acute dyspnea, and angioedema. She complained of an itchy rash, and then had difficulty swallowing. Rosa drove Anita to the emergency room two blocks away rather than wait for an ambulance. As they approached the hospital, Anita lost consciousness. This medical emergency would most probably result in immediate _____ before any subsequent treatment. a. subcutaneous injection of epinephrine b. intravenous injection of corticosteroids c. intravenous injection of antihistamine d. intravenous injection of antibiotics e. intravenous injection of a nonsteroidal anti-inflammatory drug. 14–44 Look again at Question 14–43. What do you think Anita was suffering from? Given the circumstances in which the episode occurred, suggest a likely cause. ANSWERS 7 14–1 a, b, c, e 14–2 a, c, d, e 14–3 a—2; b—5; c—3; d—4; e—1 14–4 d 14–5 d 14–6 b 14–7 (i) Inhalation: house dust mite feces, animal dander. (ii) Injection: drugs administered intravenously, wasp venom. (iii) Ingestion: peanuts, drugs administered orally. (iv) Contact with skin: poison ivy, nickel in jewelry. 14–8 A. If an individual becomes sensitized to antigen by making antibodies of the IgE isotype during first exposure, then a type I hypersensitivity reaction may result if antigen is encountered again. The IgE made initially binds stably via its Fc region to very high-affinity FcεRI receptors on mast-cell surfaces. When antigen binds to this IgE, cross-linking of FcεRI occurs, delivering an intracellular signal that activates the mast cell. B. Mast cells contain preformed granules containing a wide range of inflammatory mediators that are triggered to be released extracellularly through an exocytic mechanism called degranulation. The inflammatory mediators contained in the granules and released immediately include histamine, heparin, TNF-α, and proteases involved in the remodeling of connective tissue matrix. The proteases include tryptase and chymotryptase (expressed by mucosal and connective mast cells, respectively), cathepsin G, and carboxypeptidase. Additional inflammatory mediators are generated after mast-cell activation, including IL-3, IL-4, IL-5, IL-13, GM-CSF, CCL3, leukotrienes C4 and D4, and platelet-activating factor. 14–9 a, g 14–10 d 14–11 b 14–12 A. Armed mast cells and basophils become activated when IgE molecules bound to FcεRI on their cell surface become cross-linked. Normally this occurs when antigen is bound to IgE. If IgE were able to bind to FcεRI using one domain, and at the same time bind to FcεRII using a different domain, then IgE itself would mediate cross-linking of FcεRI and cause cellular activation in the absence of antigen. B. This does not occur because IgE has two distinct binding sites for FcεRI and FcεRII, and when one or the other of these binding sites is occupied, the conformation of IgE is altered so that it is unable to bind to the other receptor. 8 14–13 e 14–14 b 14–15 a, d, f 14–16 e 14–17 b 14–18 a 14–19 c 14–20 e 14–21 A. Particles containing proteins that stimulate allergic responses will be more easily broken down by proteolysis, enabling more effective release of the allergen. Proteolytic degradation results in the formation of peptides that will bind to MHC class II molecules and consequently stimulate TH2 cells. B. Present in the feces of the house dust mite Dermatophagoides pteronyssimus is a cysteine protease that is an allergen responsible for 20% of human allergies in North America. 14–22 a—2; b—3; c—2; d—1; e—1; f—3; g—1 14–23 The reactive bond in the β-lactam ring of penicillin reacts with proteins on the surface of human cells, with erythrocytes most commonly being involved. This modification generates a foreign epitope to which TH2 cells and B cells respond. 14–24 A. C3b becomes deposited on the cell surface of penicillin-modified erythrocytes because a bacterial infection is ongoing (the reason that penicillin was administered in the first place). The erythrocyte becomes coated as a bystander effect of complement activation. B. C3b on the penicillin-modified erythrocyte binds to CR1 on macrophages in the spleen, which facilitates receptor-mediated endocytosis and the subsequent processing and presentation of the penicillin–protein conjugate peptide. Then TH2 cells interact with the peptide:MHC class II complexes, become activated, and provide help to B cells with IgE B-cell receptors specific for the penicillin–protein conjugate. 14–25 Mast cells activated by inhaled allergens in the type I hypersensitivity reaction that causes allergic rhinitis or asthma release histamine. Histamine binding to its receptors on smooth muscle causes the bronchial constriction typical of asthma and the difficulty in breathing. Histamine binding to receptors on vascular endothelium causes increased permeability of the 9 epithelium and inflammation of nearby tissue, causing the runny nose and swollen eyes typical of allergic rhinitis, and also an accumulation of mucus and fluid in the bronchi typical of allergic asthma. By blocking histamine action, antihistamines help alleviate these symptoms. 14–26 A. (i) The immunoglobulin on a mast cell is an IgE antibody that has become bound to the mast cell’s FcεRI receptor, whereas the immunoglobulin on a B cell is a transmembrane form made by the cell itself. (ii) A B cell might have any class of immunoglobulin on its surface, whereas mast cells have only IgE. (iii) IgE molecules of many different antigen specificities can be bound to the surface of an individual mast cell, whereas an individual B cell carries immunoglobulin molecules of only one specificity. B. After binding to antigen, mast cells become operational as effector cells without the need to undergo proliferation or differentiation. In contrast, after antigen binds to a surface immunoglobulin on a B cell, the cell must proliferate and differentiate to produce effector cells (antibody-secreting plasma cells). 14–27 A. (i) One approach to desensitization is the subcutaneous injection of the allergen itself into sensitized individuals with the aim of skewing the immune response from an IgE to an IgG4 isotype. This is achieved by gradually increasing the subcutaneous allergen concentration over time, which favors IgG over IgE production. When antigen is encountered subsequently, IgG will compete with IgE for binding and inhibit IgE cross-linking on mast-cell surfaces. (ii) The second approach involves vaccination with allergen-derived peptides designed to be bound by HLA class II molecules and presented to allergen-specific TH2 cells with the aim of inducing anergy in these T cells. This would prevent them from giving help to allergen-specific naive B cells, thus preventing the production of more IgE antibody on repeated exposures to the environmental allergen. B. (i) A risk of the first approach is the possibility of activating a systemic anaphylactic response after mast-cell activation. Because the patient was previously sensitized, IgE antibodies against allergen are present and, if bound to mast cells, will induce mast-cell degranulation. In the event of an anaphylactic response to an allergy shot, the patient will have epinephrine administered immediately by the attending physician or nurse practitioner. (ii) With the peptide vaccination approach, allergen-specific T cells are rendered anergic and there is no risk of triggering an anaphylactic reaction. However, the disadvantage of this approach is that because the HLA class II genes are highly polymorphic, the vaccine would have to include sufficient peptides able to bind to most HLA class II allotypes, or it would need to be custom made for each individual on the basis of their HLA class II type. 14–28 (i) Avoid contact with allergens as much as possible by modifying their behavior and their home environment. (ii) Use pharmacological agents that inhibit allergic responses. (iii) Undergo desensitization therapy to divert immune responses from IgE to IgG4 isotype. 14–29 Mast cells express Toll-like receptors, which can bind to pathogen-associated molecules and stimulate the production of cytokines and chemokines that participate in innate immune responses. 10 14–30 When smooth muscle cells bind histamine using H1 receptors, they contract. In combination with increased mucus production by mucosal epithelium this produces a variety of effects, for example, wheezing due to bronchial constriction, coughing, sneezing, watery eyes, nasal discharge, itchiness, and, if the reaction occurs in the gut, vomiting and diarrhea. When endothelial cells of blood vessels bind histamine, an increase in vascular permeability enables the entry of fluid (edema) and leukocytes into affected tissues. 14–31 e 14–32 b 14–33 b, c, e 14–34 a 2; b 5; c 1; d 3; e 4 14–35 a 14–36 a, b, c 14–37 c, d, e 14–38 a 14–39 d 14–40 a, c, d 14–41 e 14–42 a, b, d, f 14–43 Rationale: The correct answer is a. This is a case of anaphylactic shock caused by a food allergy. Anita’s sudden onset of shortness of breath, swelling of mucosal tissues causing difficulty in breathing, and rash are characteristic of a type I hypersensitivity reaction after the rapid absorption of allergen into the bloodstream and systemic activation of mast cells in the connective tissue of blood vessels. Given the life-threatening nature of this medical emergency, where asphyxiation due to constriction of the airways and swelling of the epiglottis may occur, immediate suppression of Anita’s hyperactive response is warranted. Subcutaneous injection of epinephrine will bring the most immediate effect, not corticosteroids, antihistamines, antibiotics, or nonsteroidal anti-inflammatory agents. Epinephrine will relax bronchial constriction, stimulate the heart, and induce the reformation of tight junctions between vascular endothelial cells, which will alleviate swelling and restore blood pressure. 14–44 Anita was suffering from acute anaphylactic shock almost certainly caused by an allergic reaction to something she had just eaten at the buffet. Given that it was a dessert buffet, nuts or peanuts would be one of the most likely suspects, because they or their oils are ingredients or 11 contaminants in many prepared foods, and they are well known to provoke severe anaphylactic reactions in susceptible people. 12