Chapter 16: Hypersensitive Reactions
advertisement
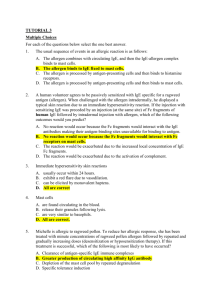
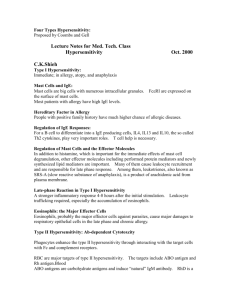
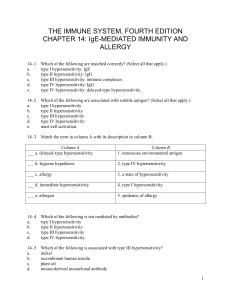
Chapter 16: Hypersensitive Reactions • Typically, inflammatory responses rid the body of Ag and resolves the infection within days • In some cases, the inflam response can have harmful effects – even result in death! -this type of IR is called ‘hypersensitivity’ or ‘allergy’ • Hypersensitive reactions develop during the course of either: – Humoral IR response or – Cell-mediated IR response Those reactions initiated by Ab or Ab-Ag complexes are called Immediate Hypersensitivities Those initiated by cell-mediated response are called Delayedtype Hypersensitivities Gell and Coombs Classification • Four categories of hypersensitivity were proposed by G&C which recog differences in the effector molecules generated. They include: • IgE mediated – Type I • IgG mediated – Type II • Immune complex mediated – Type III • Cell mediated (DTH) – Type IV General descriptions of the 4 types of hypersensitivity Figure 16-1 IgE-Mediated (Type I) Hypersensitivity • Antibody class produced is different than the normal 1° response • IgE is produced vs an “allergen”(not vs parasite) • IgE binds to mast cells/basophils sensitized • 2nd exposure to allergen cross-links IgE’s and triggers degranulation of mast cells/basophils • Effects may be systemic or localized depending.. Components of Type I Rxns: 1. 6. 3. 2. Figure 16-2 4. 5. Type I Rxns: 1. Allergens • IgE produced in response to parasites, typically • Atopic individuals produce IgE vs common environmental Ag’s; genetic predisposition • More susceptible to: hay fever, asthma, etc. • Most rxns take place on mucus membranes • Allergens are multi-antigenic; although only several are allergenic (E and K fractions)* • Allergenicity is a function of dose, sensitizing route, possible adjuvant, and genetics** Type I Rxns: 2. and 3. Reaginic Ab, Mast Cells and Basophils • IgE also called “reagin”, larger than typical Ig due to extra H chain domain, low serum[c] • IgE Fc binds to glycoprotein on Mast/Baso • Baso’s – 0.5-1.0% of circ WBC; granulocytes! • Mast’s – in conn tiss, near bv’s and lv’s – Skin and mucus memb (esp resp & gi tracts) – Upon activation, granules are released effects! Type I Rxns: 4. IgE Crosslinkage by allergen • Cross-linking 2 FcRI receptors initiates degranulation of Mast/Basophils. This may occur several ways: Typical trigger Mast/Basophil Cell Activation and Degranulation Type I Rxns: 5. Release of Pharmacologically active agents • Substances released from cell granules • Substances act on: a) nearby tissue b) 2° effector cells • Substances (chemical mediators) are categorized as either 1° or 2° : • 1° are substances released from granules • 2° are synthesized after activation or product(s) of membrane destruction Type I Hypersensitivity: Main Bio effectors 1. Histamine – major portion of granules - decarboxylation of histidine -specific receptors (H1, H2, H3) on target cells *H1 - >permeability of b.v.’s >contraction of intest/bronchial smooth muscles >mucus secretion Goblet cells H2 >vasc perm and vasodilation -suppression of degran if bound to Mast/Baso – neg feedback Type I Hypersensitivity: Main Bio effectors 2. Leukotrienes and prostaglandins – -produced from P-lipid breakdown -longer lasting and more potent than histamine as effector chemicals -promote further contraction of smooth muscles 3. Cytokines – -various cytokines (IL-4,5,6, TNF-α) released from Mast/Baso -attract neut’s/eosino’s >IgE production from B cells -TNF may contribute to systemic anaphylaxis Type I Responses may be Systemic or Localized Systemic response (Anaphylaxis): • occurs w/i minutes; symptoms include: difficult resp. BP drop, smooth muscle contraction, massive edema • Treat with epinephrine Localized response (Atopy): • Inherited; occurs in ~20%; rxn limited to target tissue • often @ epithelial surfaces Type I Rxns: Localized allegic responses 1. Allergic rhinitis (hay fever) – 2. Asthma – • • Early response Late response 3. Food allergy 4. Atopic dermatitis (eczema) - Type I Hypersensitivity: Late-Phase Reactions • Caused by pharmacologic/vasoactive mediators -> induce local inflammation….causes tissue damage • Occurs 4-6 hrs after initial rxn; can persist 1-2 days • TNF-α and IL-1 increase CAM’s on endothelia promote tethering/migration of: – – – – Neutrophils Eosinophils Monocytes Basophils Cytokines from Mast cells also contribute! • Eosino’s exhibit Fc receptors for IgE -> triggers degran. • Neutro’s release lytic enzymes, PAF, leukotrienes Type I Hypersensitivity: Regulatory factors • The following factors influence IgE response to allergens: – Level of Ag dose – Mode of antigen presentation – Relative presence of TH1 and TH2 titres • TH2’s release IL-3,4,5, and 10 • TH1’s release IFN-γ • Atopic vs non-atopic individuals express qualitatively different Type I responses to allergens… – Atopic responses involve TH2 production of IgE from B cells – Non-atopic responses involve TH1 production of IgM or IgG Type I Hypersensitivity: Detecting allergies Skin tests- injections or scratchings -Stim local Mast cells -Produces P-K rxn (wheal and flare) -Inexpensive and quick -May sensitize one to new Ag’s -May stim late-phase rxn in some Immunoassays for serum IgE -Radioimmunosorbent test (RIST) -Radioallergosorbent test (RAST) Immunoassays for IgE RIST RAST Type I Hypersensitivity: Treatment methods Immunotherapy • Antibody therapy – Injected monoclonal antiIgE Ab binds free and mIgE on B cells • Hyposensitization – Repeated injections of allergen causes a shift in Ig response Drug treatments