Volume 27
Number 2
April 2014
Baylor University Medical Center Proceedings
Multipatient Studies
79 Validation of Rules of TwoTM as a paradigm for assessing asthma
control
83
M. Millard, M. Hart, and S. Barnes
Impact of a surveillance screening program on rates of methicillinresistant Staphylococcus aureus infections with a comparison of
surgical versus nonsurgical patients
125 Triple-hit lymphoma
Improving hospital staff compliance with environmental cleaning
behavior
L. Ramphal, S. Suzuki, I. M. McCracken, and A. Addai
92
Ethnic disparities in the prevalence of the metabolic syndrome in
American adults: data from the Examination of National Health and
Nutrition Examination Survey 1999–2010
L. Ramphal, J. Zhang, and S. Suzuki
96
A cohort analysis of the cardiovascular risk factors in the employees of
a pediatric hospital from 2009 to 2012
L. Ramphal, J. Zhang, and S. Suzuki
100
Volume 27, Number 2 • April 2014
Baylor University Medical Center, Dallas, Texas
Factors affecting adherence to a quality improvement checklist on an
inpatient hepatology service
E. B. Tapper and M. Lai
103
Characteristics of Native Americans with HIV and implications for
care
C. Connel, J. S. Stroup, J. R. Stephens, and E. Martin
106
Comparison of the frequency and level of serum total cholesterol
>300 mg/dL in patients at the same Texas hospital in a single
month in 1993 and in 2013
W. C. Roberts, J. M. Ko, and R. Benavides Jr.
D. L. Glancy and D. L. Prout Jr.
N. Pemmaraju, J. Gill, S. Gupta, and J. R. Krause
128 Small bowel intussusception causing a postoperative bowel obstruction
following laparoscopic low anterior resection in an adult
A. S. Hussain, R. Warrier, and H. T. Papaconstantinou
131 Fatal abdominal hemorrhage associated with gallbladder perforation
due to large gallstones
L. R. Soto, H. R. Levine, S. A. Celinski, and J. M. Guileyardo
133 Methemoglobinemia precipitated by benzocaine used during
intubation
A. Afzal, R. Collazo, A. Z. Fenves, and J. Schwartz
136 Where is that hemodialysis catheter (superior vena cava or aorta)?
A case of intraarterial catheter placement
V. Tan and J. C. Schwartz
139 Renal failure due to Capnocytophaga canimorsus generalized
Shwartzman reaction from a dog bite (DF-2 nephropathy)
V. Tan and J. C. Schwartz
141 Imaging manifestations of a dreaded obstetric complication in the
immediate postpartum period
H. Levine, M. Zarghouni, and W. Cannon
143 Fetal demise due to cord entanglement in the early second trimester
R. N. Ergin, M. Yayla, and A. S. Ergin
145 Ingrown toenails (unguis incarnatus): nail braces/bracing treatment
Case Studies
108 Opsoclonus myoclonus syndrome: an unusual presentation for West
Nile virus encephalitis
A. Afzal, S. Ashraf, and S. Shamim
111
Fatal Clostridium septicum infection in a patient with a hematological
malignancy
R. Panikkath, V. Konala, D. Panikkath, E. Umyarova, and F. Hardwicke
113
Pages 77–196
Bilateral diaphragmatic paralysis associated with the use of the tumor
necrosis factor-alpha inhibitor adalimumab
M. M. Benjamin, A. W. Martin, and R. L. Rosenblatt
116
Celiac artery disease and fatal rupture of a hepatic artery aneurysm in
the Ehlers-Danlos syndrome
A. Nat, T. George, G. Mak, A. Sharma, A. Nat, and R. Lebel
118
120
To access Baylor’s physicians, clinical services, or
educational programs, contact the Baylor Physician
ConsultLine: 1-800-9BAYLOR (1-800-922-9567)
D. L. Glancy and M. Singh
124 Inverted P waves, QRS complexes, and T waves in lead I in a 64-yearold woman
A. Jennings, M. Bennett, T. Fisher, and A. Cook
88
123 Irregular cardiac rhythm with wide QRS complexes
The most common cause of hemoptysis worldwide: a fluke?
Editorials, Tributes, Book Review
150 Tributes to George J. Race, MD, PhD
W. L. J. Edwards, J. W. Fay, M. Ramsay, A. D. Roberts Jr., and M. J. Stone
153 Cardiologist in the shadow of Angkor Wat: a medical mission to
Cambodia
J. D. Cantwell
156 A tale of Congress, continuing medical education, and the history of
medicine
C. Partin, H. I. Kushner, and M. E. Kollmer Horton
161 Mentoring: a tale of two poems, filling graveyards, and learning the art
of medicine
C. Partin
A. Nat, A. Nat, A. Sharma, G. Shastri, and M. C. Iannuzzi
163 HIPAA: a flawed piece of legislation
Stress-induced (takotsubo) cardiomyopathy following thoracic epidural
steroid injection for postherpetic neuralgia
166 Book review: Selected Roberts Papers from Seven Generations
N. P. McKernan, B. J. Rondeau, and R. K. McAllister
122
A. Chiriac, C. Solovan, and P. Brzezinski
Invited commentary: Takotsubo cardiomyopathy following epidural
steroid injection: yet another way to break the heart
A. B. Weisse
F. D. Winter Jr.
168 From the editor: Facts and ideas from anywhere
W. C. Roberts
J. M. Schussler
www.BaylorHealth.edu/Proceedings
Indexed in PubMed, with full text available through PubMed Central
Baylor University Medical Center
Proceedings
The peer-reviewed journal of Baylor Health Care System, Dallas, Texas
Volume 27, Number 2 • April 2014
Editor in Chief
William C. Roberts, MD
Associate Editor
Michael A. E. Ramsay, MD
Founding Editor
George J. Race, MD, PhD
Dennis R. Gable, MD
D. Luke Glancy, MD
L. Michael Goldstein, MD
Paul A. Grayburn, MD
Bradley R. Grimsley, MD
Joseph M. Guileyardo, MD
Carson Harrod, PhD
H. A. Tillmann Hein, MD
Daragh Heitzman, MD
Priscilla A. Hollander, MD, PhD
Ronald C. Jones, MD
Roger S. Khetan, MD
Göran B. Klintmalm, MD, PhD
Sally M. Knox, MD
John R. Krause, MD
Joseph A. Kuhn, MD
Zelig H. Lieberman, MD
Jay D. Mabrey, MD
Michael J. Mack, MD
Peter A. McCullough, MD, MPH
Gavin M. Melmed, JD, MBA, MD
Robert G. Mennel, MD
Dan M. Meyer, MD
Michael Opatowsky, MD
Joyce A. O’Shaughnessy, MD
Dighton C. Packard, MD
Gregory J. Pearl, MD
Robert P. Perrillo, MD
Daniel E. Polter, MD
Irving D. Prengler, MD
Chet R. Rees, MD
Randall L. Rosenblatt, MD
Lawrence R. Schiller, MD
W. Greg Schucany, MD
wc.roberts@BaylorHealth.edu
Editorial Board
Jenny Adams, PhD
W. Mark Armstrong, MD
Raul Benavides Jr., MD
Joanne L. Blum, MD, PhD
C. Richard Boland Jr., MD
Jennifer Clay Cather, MD
Evangeline T. Cayton, MD
James W. Choi, MD
Cristie Columbus, MD
Barry Cooper, MD
R. D. Dignan, MD
Gregory G. Dimijian, MD
Michael Emmett, MD
Andrew Z. Fenves, MD
Giovanni Filardo, PhD
Adrian E. Flatt, MD
James W. Fleshman, MD
Editorial Staff
Managing Editor
Cynthia D. Orticio, MA, ELS
Administrative Liaison
Dana M. Choate, MBA, RHIA, CHP
Jeffrey M. Schussler, MD
S. Michelle Shiller, DO
Michael J. Smerud, MD
Marvin J. Stone, MD
C. Allen Stringer Jr., MD
William L. Sutker, MD
Gary L. Tunell, MD
Beverlee Warren, MA, MS
Wilson Weatherford, MD
Lawrence S. Weprin, MD
F. David Winter Jr., MD
Larry M. Wolford, DMD
Scott W. Yates, MD, MBA, MS
Residents/Fellows
Mina Benjamin, MD
Kyle Gummelt, DO
Design and Production
Aptara, Inc.
Cynthia.Orticio@BaylorHealth.edu
Baylor University Medical Center Proceedings (ISSN 0899-8280), a peer-reviewed
journal, is published quarterly (January, April, July, and October). Proceedings is
indexed in PubMed and CINAHL; the full text of articles is available both at www.
BaylorHealth.edu/Proceedings and www.pubmedcentral.nih.gov. The journal’s mission is to communicate information about the research and clinical activities, continuing education, philosophy, and history of the Baylor Health Care System.
Funding for the journal is provided by the following:
• Baylor Health Care System Foundation
• Helen Buchanan and Stanley Joseph Seeger Endowment for Surgery
Funding is also provided by donations made by the medical staff and subscribers. These donations are acknowledged each year in the April or July issue. For
more information on supporting Proceedings and Baylor Health Care System
with charitable gifts and bequests, please call the Foundation at 214-820-3136.
Donations can also be made online at http://give.baylorhealth.com/.
Statements and opinions expressed in Proceedings are those of the authors and
not necessarily those of Baylor Health Care System or its board of trustees.
Guidelines for authors are available at http://www.baylorhealth.edu/Research/
Proceedings/SubmitaManuscript/Pages/default.aspx.
Subscriptions are offered free to libraries, physicians affiliated with Baylor, and
other interested physicians and health care professionals. To add or remove your
name from the mailing list, call 214-820-9996 or e-mail Cynthia.Orticio@
BaylorHealth.edu. POSTMASTER: Send address changes to Baylor Scientific
Publications Office, 3500 Gaston Avenue, Dallas, Texas 75246.
Advertising is accepted. Acceptance of advertising does not imply endorsement
by Baylor University Medical Center. For information, contact Cindy Orticio
at Cynthia.Orticio@BaylorHealth.edu.
Permission is granted to students and teachers to copy material herein for
educational purposes. Authors also have permission to reproduce their own
articles. Written permission is required for other uses and can be obtained
through Copyright.com.
Copyright © 2014, Baylor University Medical Center. All rights reserved. Printed
in the United States of America on acid-free paper. Press date: March 7, 2014.
To access Baylor’s physicians, clinical services, or educational programs, contact
the Baylor Physician ConsultLine: 1-800-9BAYLOR (1-800-922-9567).
77
Clinical research studies enrolling patients through
Baylor Research Institute
Currently, Baylor Research Institute is conducting more than 800 research projects. Studies open to enrollment are listed in
the Table. To learn more about a study or to enroll patients, please call or e-mail the contact person listed.
Table. Clinical research studies conducted through Baylor Research Institute that are enrolling patients
Research area
Asthma and
pulmonary disease
Specific disease/condition
Contact information (name, phone number, and e-mail address)
Chronic obstructive pulmonary disease, asthma (adult)
Rose Boehm, CCRC, RRT, RCP
Jana Holloway, RRT, CRC
214-820-9772
214-820-9772
RoseB@BaylorHealth.edu
janahol@baylorhealth.edu
Breast, ovarian, endometrial, prostate, brain, lung, bladder, colorectal, pancreatic,
and head and neck cancer; hematological malignancies, leukemia, multiple
Grace Townsend
myeloma, non-Hodgkin’s lymphoma; melanoma vaccine; bone marrow transplant
214-818-8472
cancer.trials@BaylorHealth.edu
Treatment-naive colorectal cancer
Allison Cox
214-820-6779
marya.cox@baylorhealth.edu
Type 1 and type 2 diabetes, cardiovascular events
Kris Chionh
214-820-3416
kristen.chionh@BaylorHealth.edu
Pancreatic islet cell transplantation for type I diabetics, who either have or
have not had a kidney transplant
Kerri Purcell, RN
817-922-4640
kerrip@BaylorHealth.edu
Type 2; cardiac events
Trista Bachand, RN
817-922-2587
trista.bachand@baylorhealth.edu
Pancreatic islet cell transplantation for type I diabetics, who either have or
have not had a kidney transplant
Kerri Purcell, RN
817-922-4640
kerrip@BaylorHealth.edu
Crohn’s disease
Fabrienne English
214-818-9688
fabrienne.english@baylorhealth.edu
Healthy subjects needing colonoscopies
Allison Cox
214-820-6779
marya.cox@baylorhealth.edu
Heart and vascular
disease (Dallas)
Aortic aneurysms, coronary artery disease, hypertension, poor leg circulation,
heart attack, heart disease, congestive heart failure, angina, carotid artery
disease, familial hypercholesterolemia, renal denervation for hypertension,
diabetes in heart disease, cholesterol disorders, heart valves, thoracotomy pain,
stem cells, critical limb ischemia, cardiac surgery associated with kidney injury,
pulmonary hypertension
Merielle Boatman
214-820-2273
MeriellH@BaylorHealth.edu
Heart and vascular disease
(Fort Worth)
Atrial fibrillation, carotid artery stenting
Deborah Devlin
817-922-2575
Deborah.Devlin@BaylorHealth.edu
Heart and vascular disease
(Legacy Heart)
At risk for heart attack/stroke; previous heart attack/stroke/PAD; cholesterol
disorders; atrial fibrillation; overweight/obese; other heart-related conditions
Angela Germany
214-800-6469
lhcresearch@baylorhealth.edu
Heart and vascular
disease (Plano)
Aneurysms; coronary artery disease; surgical renal denervation, or stent,
for uncontrolled hypertension; poor leg circulation; heart attack; heart
disease; heart valve repair and replacement; critical limb ischemia; repair
Natalie Settele, PA-C
of AAA, TAA, and dissections with endografts; thoracic surgery leak
repair; atrial fibrillation; carotid artery disease; congestive heart failure;
left atrial appendage and stroke; gene profiling
469-814-4712
natalie.settele@BaylorHealth.edu
Hepatology
Liver disease
Jonnie Edwards
214-820-6243
jonnie.edwards@baylorhealth.edu
HIV/AIDS
Bryan King, LVN
214-823-2533
bryan.king@ntidc.org
Cancer
Diabetes (Dallas)
Diabetes (Fort Worth)
Gastroenterology
Infectious disease
Hepatitis C, hepatitis B
Jonnie Edwards
214-820-6243
Jonnie.edwards@baylorhealth.edu
Homocysteine and kidney disease, dialysis fistulas, urine/protein disorders
in cancer patients
Dallas Clinical Trials Office
214-818-9688
Fabrienne.english@baylorhealth.edu
Stroke
Dion Graybeal, MD
214-820-4561
Dion.Graybeal@BaylorHealth.edu
Multiple sclerosis
Annette Okai, MD
214-820-4655
annette.okai@BaylorHealth.edu
Neurosurgery
Cerebral aneurysms
Kennith Layton, MD
214-827-1600
KennithL@BaylorHealth.edu
Rheumatology (9900 N.
Central Expressway)
Rheumatoid arthritis, psoriatic arthritis, lupus, gout, ankylosing spondylitis
Krystine Cethoute
214-987-1249
krystine.cethoute@baylorhealth.edu
Bone marrow, blood stem cells
Grace Townsend
214-818-8472
Grace.Townsend@BaylorHealth.edu
Solid organs
Jonnie Edwards
214-820-6243
jonnie.edwards@baylorhealth.edu
Obesity
Kris Chionh
214-820-3416
kristen.chionh@BaylorHealth.edu
Endometriosis and endometrial ablation
Theresa Cheyne, RN
817-922-2579
theresa.cheyne@BaylorHealth.edu
Interstitial cystitis/bladder pain syndrome
Cathy Frisinger
817-922-2574
cathy.frisinger1@baylorhealth.edu
Nephrology
Neurology
Transplantation
Weight management
Women’s health (Fort Worth)
Baylor Research Institute is dedicated to providing the support and tools needed for successful clinical research. To learn more
about Baylor Research Institute, please contact Kristine Hughes at 214-820-7556 or Kristine.Hughes@BaylorHealth.edu.
78
Proc (Bayl Univ Med Cent) 2014;27(2):78
Validation of Rules of TwoTM as a paradigm for assessing
asthma control
Mark Millard, MD, Mary Hart, MS, RRT, AE-C, and Sunni Barnes, PhD
Assessing asthma control at each patient encounter is an essential
task to determine pharmacologic requirements. Rules of Two (Ro2) was
created from the original 1991 National Asthma Education Program
guidelines to determine the need for controller therapy. This study determined the degree of agreement between Ro2 and the Expert Panel
Report (EPR-3) definition of “in control” asthma and compared that
value with the Asthma Control Test (ACT) in a group of asthmatics for
the purpose of validating this tool. Patients with documented asthma
were randomized to complete Ro2 or ACT prior to being assessed for
asthma control by certified asthma educators using an EPR-3 template.
Assessments occurred in either a specialty asthma clinic or at a local
health fair. Patients were also queried for their personal assessment
of asthma control. The primary statistical methodology employed was
the degree of agreement (kappa) between each survey tool and the
EPR-3 template. Of 150 patients, 72% did not have their asthma in
control, based on the EPR-3 template. Ro2 identified 58% of patients
not in control of their asthma, whereas ACT identified 36%, with kappa
scores of 0.41 for Ro2 and 0.37 for ACT compared with the EPR-3
template. These were not significantly different. Of the 150 patients,
75% considered their asthma in control based on self-assessments,
with a kappa of 0.23. In 14 of 73 ACT questionnaires, scores were not
added or were misadded. Eliminating evaluation of static lung function
significantly improved both kappa scores of Ro2 and ACT. In conclusion, Ro2 identifies patients with uncontrolled asthma as well as ACT
and may be useful to the primary assessing clinician in determining
asthma control.
he assessment of asthma control drives therapeutic decisions in patients with asthma, as articulated in the
2007 edition of the National Asthma Education and
Prevention Program (NAEPP) (1), also referred to as
the Expert Panel Report (EPR-3). That assessment reflects the
contributions of two related domains, impairment and risk, and
consists of patient-reported symptoms and symptom frequency,
documentation of health care encounters, medication use, and
objective measurement of lung function. The decision to step
up, step down, or maintain any specific therapy rests upon the
determination of asthma control.
Rules of TwoTM (Ro2) was created in 1992 as a tool to signal
the need for controller therapy according to the first National
T
Proc (Bayl Univ Med Cent) 2014;27(2):79–82
Asthma Education Program (NAEP) guidelines published in
1991. At that time, the use of controller therapy for patients
with persistent asthma had not been generally accepted within
the primary care community, and there was a need to develop
an easily remembered synopsis of the NAEP criteria for mild
persistent asthma, which was the point at which antiinflammatory therapy for asthma was first recommended. While abstracts demonstrating the impact of Ro2 educational efforts were
presented at annual American Thoracic Society conferences in
1999 (2) and 2000 (3), no specific validation of Ro2 was ever
attempted, primarily because the syntax of Ro2 was taken directly from NAEP and no specific need for separate validation
was perceived.
By contrast, the well-validated Asthma Control TestTM
(ACT) (4) introduced in 2004 followed a methodical development beginning with focus groups of asthma experts to identify
specific issues relevant to the assessment of asthma control and
then proceeding to demonstrate the most robust of these items,
ultimately resulting in a validation for both adult and pediatric
communities of the ACT as a standardized patient-reported
questionnaire to assess asthma control. Multiple studies have
since demonstrated ACT’s relevance in predicting asthma morbidity (5, 6), and the 2007 NAEPP guidelines identified ACT
as one of three validated patient-reported evaluations that could
be used to assess asthma control.
The 2007 EPR-3 published a table enumerating multiple
determinants of asthma control using the two domains of impairment and risk (Table 1) (1). Using this table as a template
for good control, the current study compared the agreement
between this standard and either the Ro2 (Figure 1) or the ACT
(Figure 2) in predicting asthma control in a cohort of patients
with documented asthma.
METHODS
This study recruited subjects with healthcare professional–
diagnosed asthma who were taking prescription asthma
From the Baylor Martha Foster Lung Care Center, Baylor University Medical
Center at Dallas (Millard, Hart), and the STEEEP Global Institute, Dallas, Texas
(Barnes).
Corresponding author: Mark Millard, MD, Baylor Foster Lung Care Center, 4004
Worth Street, Dallas, TX 75246 (e-mail: markmi@baylorhealth.edu).
79
Table 1. Assessing asthma control and adjusting therapy in youths ≥12 years of age and adults*
Classification of asthma control (≥12 years of age)
Components of control
Well controlled
Not well controlled
>2 days/week or multiple times
on ≤2 days/week
Throughout the day
Nighttime awakenings
≤1x/month
≥2x/month
≥2x/week
Interference with normal activity
None
Some limitation
Extremely limited
>2 days/week
Several times per day
>80% predicted/personal best
>80%
60−80% predicted/personal best
75−80%
<60% predicted/personal best
<75%
Exacerbations requiring oral systemic
corticosteroids
0−1/year
≥2/year (see note)
Reduction in lung growth
Evaluation requires long-term followup.
Treatment-related adverse effects
Medication side effects can vary in intensity from none to very troublesome and worrisome. The level of
intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk.
Short-acting beta2-agonist use for
≤2 days/week
symptom control (not prevention of EIB)
Lung function
• FEV1 or peak flow
• FEV1/FVC
Risk
Very poorly controlled
≤2 days/week but not more
than once on each day
Impairment Symptoms
Consider severity and interval since last exacerbation
*Reprinted from Expert Panel Report 3 (1).
EIB indicates exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
Notes:
• The level of control is based on the most severe impairment or risk category. Assess impairment domain by patient’s/caregiver’s recall of previous 2–4 weeks and by
spirometry or peak flow measures. Symptom assessment for longer periods should reflect a global assessment, such as inquiring whether the patient’s asthma is better or
worse since the last visit.
• At present, there are inadequate data to correspond frequencies of exacerbations with different levels of asthma control. In general, more frequent and intense exacerbations
(e.g., requiring urgent, unscheduled care, hospitalization, or intensive care unit admission) indicate poorer disease control. For treatment purposes, patients who had ≥2
exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have not-well-controlled asthma, even in the absence of
impairment levels consistent with not-well-controlled asthma.
medications, excluding those with known chronic obstructive pulmonary disease, pulmonary fibrosis, or other complicating lung disease. Patients with diagnosed asthma were
randomized in a 1:1 fashion to complete either Ro2 or ACT.
These self-reported tests were completed before assessment by
certified asthma educators, who used a template taken directly
from the EPR-3 guidelines to determine asthma control and
had no prior knowledge of patient responses to either Ro2 or
ACT. Not-well-controlled asthma was defined by the Ro2 as
any positive response to the four-item questionnaire and by
the ACT as a score of ≤19. The degree of agreement (kappa)
between the more comprehensive EPR-3 template and Ro2
or ACT, in addition to patient self-perception of control, was
calculated (7). A power analysis determined that a sample
size of 150 was needed to detect a true kappa value of 0.70
based on a significance level of 0.05. This study was approved
by the Baylor Health Care System institutional review board
(IRB #009-084).
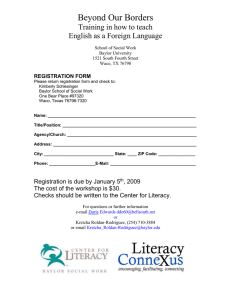
Please check the proper box. Thank you.
Do you have asthma symptoms or use your quick relief inhaler more
than two times per week?
Yes ___ No ___
Do you awaken at night with asthma symptoms more than two
times per month?
Yes ___ No ___
Do you refill a canister of quick relief medication more than two
times per year?
Yes ___ No ___
When you have asthma symptoms, does your peak flow
vary more than two times 10 (20%) from baseline?
Y e s __ _ N o _ __ I d o n ’ t k no w_ _ _
Figure 1. Rules of Two patient asthma questionnaire.
80
Baylor University Medical Center Proceedings
RESULTS
Of the 150 patients who participated in this study, 130 were
surveyed at the Baylor Martha
Foster Lung Care Center, an outpatient facility that is a part of Baylor
University Medical Center at Dallas, Texas, and provides specialized
asthma care. The remaining 20
patients were assessed at a local
women’s health fair. Spirometry
was performed on each patient.
The age of patients assessed ranged
from 14 to 86, with a median age
Volume 27, Number 2
individuals were judged “in control” by ACT but “not in control”
by EPR-3 (false-negative), yielding
Score
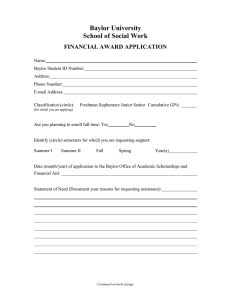
In the past 4 weeks, how much of the time did your asthma keep you from
1.
an overall agreement rate of 64%.
getting as much done at work, school or at home?
In comparison, the false-positive
1. All of the time 2. Most of the time 3. Some of the time
rate for “not in control” asthma for
4. A little of the time 5. None of the time
the Ro2 instrument was 5 out of
During the past 4 weeks, how often have you had shortness of breath?
2.
77 patients, and the false-negative
rate was 16 out of 77 patients. The
1. More than once a day 2. Once a day 3. 3 to 6 times a week
4. Once or twice a week 5. Not at all
overall agreement between Ro2 and
EPR-3 was 73%.
During the past 4 weeks, how often did your asthma symptoms (wheezing,
3.
coughing, shortness of breath, chest tightness or pain) wake you up at night or
Disagreements in the determiearlier than usual in the morning?
nation of asthma control by Ro2
1. 4 or more nights a week 2. 2 or 3 nights a week 3. Once a week
and ACT when compared with the
4. Once or twice 5. Not at all
EPR-3 template occurred primarDuring the past 4 weeks, how often have you used your rescue inhaler or
4.
ily in patients with lung function
nebulizer medication (such as albuterol)?
(forced expiratory volume in 1 sec1. 3 or more times per day 2. 1 or 2 times per day 3. 2 or 3 times per week
ond [FEV1] or FEV1/forced vital
4. Once a week or less 5. Not at all
capacity [FVC]) that was abnorHow would you rate your asthma control during the past 4 weeks?
5.
mal. Ten of the 16 patients judged
“in control” by Ro2 but not EPR-3
1. Not controlled at all 2. Poorly controlled 3. Somewhat controlled
4. Well controlled 5. Completely controlled
had abnormal lung function. Seventeen of 26 patients erroneously
Total
considered “in control” by ACT
likewise had abnormal pulmonary
Figure 2. Asthma Control Test.
function tests, although 7 of those
of 42 years; 33% were male and 67% female, which reflects the
17 patients had other positive responses to EPR-3 questions
increased adult female incidence of asthma in addition to incluthat would have resulted in a “not in control” determination,
sion of participants in the women’s health fair. In addition, 74%
despite an ACT score of >20. If resting lung function was not
were Caucasian, 17% African American, and 9% Hispanic.
used to determine asthma control in the EPR-3 tool, then the
As shown in Table 2, 109 of the entire group of 150 patients
kappa for both Ro2 and ACT would have been much higher
(72%) assessed using a template taken directly from EPR-3 were
(0.63 and 0.49, respectively). While not the primary endpoint
identified as having uncontrolled asthma, compared with 45 of
of this study, 14 of 73 ACT questionnaires failed to add up or
77 patients (58%) assessed with the Ro2 and 26 of 73 patients
misadded scores. For determination of kappa, additions were
(36%) assessed with the ACT. The degree of agreement, as ascompleted or corrected prior to analysis.
sessed using a kappa statistic, was 0.41 for Ro2 and EPR-3 and
0.37 for ACT and EPR-3. There was no statistical difference in
DISCUSSION
the agreement with EPR-3 between the Ro2 and ACT tools.
The fundamental concept of asthma “control” has been a
By contrast but as expected, agreement with patient perception
consistent element in the series of reports issued by the NAEP(P),
of self-control when compared to the EPR-3 assessment was
first in 1991, revised in 1997, and most recently in 2007 with
poor, with only 25% of patients feeling their asthma was “not
EPR-3. Delineation of impairment and risk domains is articuin control” (kappa 0.23).
lated in EPR-3, but the need for a comprehensive evaluation of
There were no false-positive ACT questionnaires when
specific aspects of asthma symptomatology and physiology is
compared to the EPR-3 template. However, 26 out of 73
longstanding and has been widely accepted as the standard for
asthma assessment. In this study, we used
the specific elements of control articulatTable 2. Determinations of in-control asthma based on different tests
ed in EPR-3 as the basis of comparison
for both Ro2 and ACT and overall deterAsthma in Asthma not in Agreement with
Agreement
mined “fair” agreement (8).
Test
control (%)
control (%)
EPR-3 (kappa) with EPR-3 (%)
A consistent finding of multiple paEPR-3 (n = 150)
28
72
–
–
tient
surveys is the discordance between
Ro2 (n = 77)
42
58
0.41
73
self-assessment of asthma control and the
ACT (n = 73)
64
36
0.37
64
assessment derived from asthma-specific
Patient self-assessment (n = 151)
75
25
0.23
37
questionnaires. The Asthma in America
EPR-3 indicates Expert Panel Report-3; Ro2, Rules of Two; ACT, Asthma Control Test.
Survey (1998) (9) quantified the discrepancy between patient perception of asthma
Please complete the following form about your asthma and add up your scores.
April 2014
Validation of Rules of TwoTM as a paradigm for assessing asthma control
81
control and reality from in-depth questionnaires. Our group demonstrated that discordance in a group of self-identified asthmatics
attending a state fair in the late 1990s (3). Subsequent follow-up
surveys have continued to demonstrate this disconnect (10). In
this study, as noted with earlier ones, a much higher percentage
of patients felt they were “in control” by self-assessment than were
considered by using an 8-question template drawn from EPR-3.
The baseline finding that over three fourths of patients assessed
with the EPR-3 tool were considered not in good control of their
asthma is consistent with other studies (9, 11) and not a unique
finding in our surveyed population. Both ACT and Ro2 identified patients who were “not in control,” but at a lower frequency
than the standard from EPR-3. Even so, Ro2 appeared to be a
slightly better tool than ACT for identifying patients who were
judged as “not in control.”
A number of other asthma self-report questionnaires exist,
such as the Asthma Therapy Assessment Questionnaire (12)
and Asthma Control Questionnaire (13), which have likewise
been validated and are used for clinical research purposes and
are mentioned in EPR-3. We chose to compare the kappa of
R02 and ACT with a template taken directly from EPR-3, to
determine the degree to which both correlate with a more robust
set of determinants of control.
The most significant explanation for the reduced kappa
scores of both Ro2 and ACT with the EPR-3 comparator in
our studied population relates to the objective measurements of
static lung function, which classified more patients with asthma
as not well controlled by EPR-3 criteria. EPR-3 assumes an
abnormal FEV1 or FEV1/FVC to be reflective of uncontrolled
asthma (1). Our clinic population that attends a specialty asthma management center may include a more severe asthmatic
population, more likely to have chronically reduced lung function, an observation that might explain the lower kappa for
both assessment tools. A certain proportion of this population
may indeed manifest airway remodeling, which is unresponsive
to even more aggressive asthma therapy, according to EPR-3,
despite minimal symptomatology (1). At least one author has
written that using lung function as a marker of uncontrolled
asthma is misleading (14). In our studied population, the kappa
scores for Ro2 and ACT improve quite significantly if lung
function measurements are not considered part of the equation
of good asthma control; in fact, excluding static lung function
scores improves agreement to “substantial” in the case of R02
and “moderate” with ACT (8).
In this study, Ro2 was more likely to be completed than
ACT. Indeed, an advantage of Ro2 over ACT lies in the fact
that no computation is needed to come up with a score, which
makes it easier for patients to complete and for clinicians to
interpret. The specific contents of Ro2 help frame the conversation between clinician and patient about asthma, move beyond
reported self-perceptions of asthma control, and allow for a brief
but potent clinical encounter to determine asthma control and
the potential need for changes in therapy.
In conclusion, the current study shows that both Ro2 and
ACT identified patients with out-of-control asthma with similar agreement when compared to an EPR-3 assessment (Ro2
82
kappa = 0.41; ACT kappa = 0.37). Ro2 had a higher rate of
agreement with EPR-3 in the classification of patients in control
vs. out of control when compared with ACT (73% vs. 64%).
Removing the measurement of static lung function significantly
improves both kappa scores. While both Ro2 and ACT share
statistically similar agreement with an EPR-3 template for good
asthma control, Ro2 is more likely to be completed by patients
and shows a slightly higher level of agreement with the standard
EPR-3 assessment.
Acknowledgments
The authors would like to thank the Baylor Martha Foster
Lung Center team of certified asthma educators who assessed each
patient: Erika Abmas, RRT, AE-C, Rose Boehm, RRT, AE-C,
Laura Blundell, BS, RRT, AE-C, Lynn Burleson, RRT, AE-C, and
Grace Hernandez, BS, RRT, AE-C. Grateful thanks are also given
to Cynthia Orticio for her help in preparing this document for
publication. Funding was provided by Baylor University Medical
Center at Dallas and Baylor Research Institute. Rules of TwoTM
is a registered trademark of Baylor Health Care System. ACTTM
is a registered trademark of QualityMetrics Inc.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
National Asthma Education and Prevention Program. Expert Panel Report
3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD:
National Heart, Lung and Blood Institute, 2007. Available at http://www.
nhlbi.nih.gov/guidelines/asthma/.
Millard M. The Dallas Asthma Consortium. Am J Respir Crit Care Med
1999;159:A126.
Millard M. Health fair awareness initiatives: an outcomes report. Am J
Respir Crit Care Med 2000;161:A405.
Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray
JJ, Pendergraft TB. Development of the asthma control test: a survey for
assessing asthma control. J Allergy Clin Immunol 2004;113(1):59–65.
Shirai T, Furuhashi K, Suda T, Chida K. Relationship of the asthma control test with pulmonary function and exhaled nitric oxide. Ann Allergy
Asthma Immunol 2008;101(6):608–613.
Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, Kosinski
M, Pendergraft TB, Jhingran P. Asthma Control Test: reliability, validity,
and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol 2006;117(3):549–556.
Altman DG. Practical Statistics for Medical Research. London: Chapman
& Hall, 1991: 404.
Viera A, Garrett J. Understanding interobserver agreement: the kappa
statistic. Fam Med 2005;37(5):360-363.
GlaxoSmithKline. The state of asthma in America: two landmark surveys.
As discussed in http://www.mainehealth.org/workfiles/mh_professional/
Asthma/ACTJournal.pdf.
Shering-Plough. Asthma Insight and Management (AIM) national survey:
Executive summary. Available at CHEST 2010.
Nathan RA, Meltzer EO, Blais MS, Murphy KR, Doherty DE, Stoloff
SW. Comparison of the Asthma in America and Asthma Insight and
Management surveys: Did asthma burden and care improve in the United
States between 1998 and 2009? Allergy Asthma Proc 2012;33(1):65–76.
Vollmer WM, Markson LE, O’Connor E, Sanocki LL, Fitterman L, Berger
M, Buist AS. Association of asthma control with health care utilization
and quality of life. Am J Respir Crit Care Med 1999;160(5 Pt 1):1647–
1652.
Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development
of a questionnaire for use in clinical trials. Thorax 1992;47(2):76–83.
Stempel DA, Fuhlbrigge AL. Defining the responder in asthma therapy.
J Allergy Clin Immunol 2005;115(3):466–469.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Impact of a surveillance screening program on rates of
methicillin-resistant Staphylococcus aureus infections with a
comparison of surgical versus nonsurgical patients
Andrew Jennings, MD, Monica Bennett, PhD, Tammy Fisher, RN, BBA, and Alan Cook, MD
Methicillin-resistant Staphylococcus aureus (MRSA) is a significant cause of
health care–associated infection. The overall effectiveness of surveillance
screening programs is not well established. A retrospective cohort study
was performed to evaluate the impact of a surveillance screening program
on the rates of health care–associated MRSA infection (HA-MRSA-I) at a
single institution. A subset of surgical patients was analyzed separately.
Multivariate regression techniques were used to identify predictors of the
desired outcomes. The overall MRSA infection rate was 1.3% in the before
cohort and 3.2% in the after cohort. After excluding patients with a history of MRSA infection or MRSA colonization, HA-MRSA-I decreased from
1.2% to 0.87%. There was a similar overall increase in the surgical group,
1.4% to 2.3%, and decrease in HA-MRSA-I, 1.4% to 1.0% (P < 0.001).
For all patients, surgery, African American race, and increased length of
stay conferred an increased likelihood of HA-MRSA-I. Females and patients
in the after cohort had a lower risk of HA-MRSA-I (P < 0.01). In the after
cohort, the results were similar, with surgery, African American race, and
length of stay associated with an increased risk, and female sex associated
with a decreased risk (P < 0.05). African American race and increased
age had a higher likelihood of screening positive for MRSA colonization,
while the surgical group, females, and Hispanic patients were less likely
(P < 0.05). HA-MRSA-I was associated with a higher mortality among all
patients (P < 0.001). Mortality rates were similar with HA-MRSA-I for all
patients (10.8% vs 9.5%, P = 0.55) and in the surgical group (8.3% vs
6.8%, P = 0.58). In conclusion, surveillance programs may be effective
in decreasing HA-MRSA-I. Further studies are needed to determine how
to reduce transmission, particularly among African Americans and those
with increased lengths of stay.
ethicillin-resistant Staphylococcus aureus (MRSA) is a
significant cause of health care–associated infection (1)
and is associated with increased hospital mortality (2,
3). In addition, MRSA is the leading cause of surgical
site infection (4, 5). In 2003, the Society of Healthcare Epidemiology of America released guidelines strongly supporting the
use of active surveillance cultures and contact isolation programs
(6). A decrease in overall health care–associated MRSA infections
(HA-MRSA-I) has since been demonstrated across a wide range
of clinical and geographical settings in the United States (7).
Surveillance programs have also proven to be effective in MRSA
outbreaks in the intensive care unit (ICU) setting (8). Despite a
M
Proc (Bayl Univ Med Cent) 2014;27(2):83–87
decrease in overall HA-MRSA-I rates after implementation of
active surveillance culture programs, the effect of HA-MRSA-I
rates on specific patient populations, including patients undergoing
invasive surgical procedures, is not well established (9, 10).
The purpose of this study was to evaluate rates of HA-MRSAI before and after implementation of a hospitalwide screening
program at a large teaching hospital with a high surgical volume.
We examined the effect of this infection control initiative in the
overall hospital population as well as for patients undergoing a
wide range of common surgical procedures among a variety of
specialties. We hypothesized that rates of HA-MRSA-I would
decrease after implementation of a screening program, both
hospitalwide and for patients undergoing surgical procedures.
METHODS
This institutional review board–approved retrospective cohort
study took place at Baylor University Medical Center at Dallas, a
1000-bed academic medical center and level I trauma center in a
large metropolitan area. Our current practice involves performing
nasal swab MRSA polymerase chain reaction (PCR) screens on all
patients who meet one of the following screening criteria: a prior
history of MRSA colonization or infection (patient is placed in contact isolation); hospitalization within the preceding year; transfer
from an extended care facility; presence of open or draining skin
wounds (patient is placed in contact isolation); current admission
to ICU; or current hemodialysis. Standard barrier and isolation
precautions, including gown and gloves, are applied to all patients
with a positive screen. With the exception of several four-bed pods
in the surgical intensive care unit, all rooms are single rooms.
A hospitalwide MRSA surveillance program was implemented in January 2009. Prior to this initiative, standard barrier
and isolation practices were implemented only if patients had a
documented MRSA infection or if the patient or patient’s history
indicated prior MRSA infection. For purposes of this study, the
term “MRSA infection” is used if a positive MRSA culture was
From the Department of Surgery, Baylor University Medical Center at Dallas.
Dr. Jennings is now with the Department of Surgery at The University of Texas
Southwestern Medical Center, Dallas, Texas.
Corresponding author: Andrew Jennings, MD, Department of Surgery, The
University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard,
Dallas, TX 75390-9158 (e-mail: andrewjenningsmd@gmail.com).
83
obtained on a patient from any source. The term “positive screen”
is used for patients who had a positive nasal PCR screen denoting
MRSA colonization, but not an active MRSA infection.
All inpatient hospital admissions from October 1st to
September 30th for 2007 to 2008 (before cohort) and 2010
to 2011 (after cohort) were analyzed. The 12-month interval
between cohorts was included to allow full implementation
across all units of the hospital. All patients in the after cohort underwent nasal MRSA PCR screening under the criteria
mentioned above. Patients with a previous MRSA infection,
as well as those readmitted with a previous positive screen for
MRSA, were excluded. Patients who initially screened negative
and subsequently developed an MRSA infection were considered to have HA-MRSA-I. A subset of patients undergoing a
wide array of surgical procedures across multiple specialties in
the before and after cohort were analyzed separately. These included general surgical, gynecologic, orthopedic, cardiothoracic,
transplant, oral-maxillofacial, plastics, and urologic procedures.
International Classification of Diseases, Clinical Modification,
ninth revision (ICD-9) procedure codes were used to identify
procedures by those specialties. Procedures were included in
the analysis if at least 50 were performed during the study period. Logistic regression analysis was performed to determine
which factors contributed to predicting HA-MRSA-I and how
HA-MRSA-I affected patient mortality. P values <0.05 were
considered significant.
Our primary endpoint was the incidence of HA-MRSA-I.
The secondary endpoint was the impact of HA-MRSA-I on
patient mortality. Multivariate regression techniques were used
to elucidate predictors of these outcomes.
RESULTS
There were 36,244 patients in the before cohort, of whom
16,740 underwent a surgical procedure, and 36,068 in the
after cohort, of whom 15,044 underwent a
surgical procedure. Patient characteristics are
Table 1. Patient characteristics for all patients and patients in the surgical group
shown in Tables 1 and 2.
The overall MRSA infection rate was
Combined
Before
After
1.3% (453 patients) in the before cohort and
All patients
3.2% (1136 patients) in the after cohort (P <
N
72,312
36,244
36,068
0.001). When patients with previous MRSA
infection or colonization were excluded, those
Age at admit, mean ± SD (years)
54.2 ± 19.2
54.1 ± 19.1
54.2 ± 19.3
with HA-MRSA-I decreased from 1.2% to
Male
29,465 (41%)
15,020 (41%)
14,445 (40%)
0.87% (Table 3). Similarly, there was an inFemale
42,837 (59%)
21,216 (59%)
21,621 (60%)
crease in the rate of overall MRSA infection
Race
in the surgical group, from 1.4% to 2.3%,
White
43,215 (60%)
22,609 (63%)
20,606 (57%)
along with a decrease in HA-MRSA-I, from
African American
18,473 (26%)
8,712 (24%)
9,761 (27%)
1.4% to 1.0% (Table 3).
Hispanic
8,324 (12%)
3,770 (10.5)
4,554 (12.7%)
For the total patient population, including both before and after cohorts, patients in
Asian
705 (1%)
289 (0.8%)
416 (1.2%)
the surgical group, African Americans, and
Other
1047 (1.5%)
431 (1.2%)
616 (1.7%)
patients with an increased length of stay had
Length of stay, median (IQR) (days)
3.8 (2.3, 6.8)
3.8 (2.2, 6.8)
3.8 (2.3, 6.9)
an increased likelihood of developing HADischarged alive
69.761 (97%)
34,917 (96%)
34,844 (97%)
MRSA-I. Female patients and patients in the
Died
2,551 (4%)
1,327 (4%)
1,224 (3%)
after cohort were less likely to develop HASurgical group
MRSA-I (Table 4). When only patients in the
after
cohort were analyzed, the results were
N
31,784
16,740
15,044
similar, with surgery, African American race,
Age at admit, mean ± SD (years)
50.7 ± 18.5
51.1 ± 18.2
50.3 ± 18.8
and length of stay associated with an increased
Male
11,667 (37%)
6,416 (38%)
5,251 (35%)
risk of HA-MRSA-I, and female sex associFemale
20,109 (63%)
10,317 (62%)
9,792 (65%)
ated with a decreased risk (Table 4).
Race
With regards to the likelihood of screenWhite
21,021 (67%)
11,460 (70%)
9,561 (64%)
ing positive for MRSA colonization, African
American race and increased age were assoAfrican American
5,820 (19%)
2,901 (18%)
2,919 (20%)
ciated with a higher likelihood of screening
Hispanic
3,705 (12%)
1,727 (11%)
1,978 (13%)
positive, while patients in the surgical group,
Asian
373 (1.2%)
151 (1%)
222 (1.5%)
female patients, and Hispanic patients were
Other
473 (1.5%)
183 (1.1%)
290 (2%)
less likely to screen positive (Table 5). HALength of stay, median (IQR) (days)
3.6 (2.3, 6.8)
3.7 (2.3, 6.7)
3.5 (2.3, 6.9)
MRSA-I was associated with a higher morDischarged alive
31,239 (98%)
16,430 (98%)
14,809 (98%)
tality for both the entire patient population
Died
545 (1.7%)
310 (2%)
235 (2%)
and surgical group in both cohorts (Table 5).
There was no significant difference in the overSD indicates standard deviation; IQR, interquartile range.
all mortality of patients with HA-MRSA-I
84
Baylor University Medical Center Proceedings
Volume 27, Number 2
by 27.5% for the overall patient population
and 28.6% for the patients in the surgery
group. Patients with MRSA nasal colonizaVariable
Surgical (N = 31,784) Nonsurgical (N = 40,528) P value
tion are at a significant increased risk for the
Age at admit, mean ± SD (years)
50.7 ± 18.5
56.9 ± 19.3
<.0001
development of MRSA infections. Stenehjem
Male
11,667 (37%)
17,798 (44%)
and colleagues demonstrated this regardless
Female
20,109 (63%)
22,728 (56%)
<.0001
of the quantitative burden detected on PCR
screening. During their study period, 4.3%
Race
of noncarriers developed a MRSA infection
White
21,021 (67%)
22,194 (55%)
compared with 18.5% and 17.2% of low- and
African American
5,820 (19%)
12,653 (31%)
high-burden patients, respectively (12).
Hispanic
3,705 (12%)
4,619 (11%)
Previous studies have demonstrated a
Asian
373 (1.2%)
332 (0.8%)
greater than twofold increased incidence of
Other
473 (1.5%)
574 (1.4%)
<.0001
MRSA infections among African Americans,
66.5 per 100,000, versus the standardized
Length of stay, median (IQR) (days)
3.6 (2.3, 6.8)
3.9 (2.2, 6.8)
<.0001
incidence rate of 31.8 per 100,000. Male
Discharged alive
31,239 (98%)
38,522 (95%)
patients had slightly higher infection rates
Died
545 (1.7%)
2006 (5%)
<.0001
at 37.5 per 100,000, while patients older
SD indicates standard deviation; IQR, interquartile range.
than 65 years of age had rates of 127.7 per
100,000 (13). Our study showed that African American patients and patients with
for all patients (10.8% vs 9.5%, P = 0.55) as well as the surgical
increased lengths of stay were at increased risk of developing
group (8.3% vs 6.8%, P = 0.58).
MRSA infection, and that female patients had a decreased
risk. Graffunder and colleagues identified previous surgery
DISCUSSION
and longer lengths of stay before infection as independent risk
Our data indicate that the overall MRSA infection rate infactors for developing MRSA infection, along with previous
creased during the study period for the entire patient population
hospitalization, enteral feedings, and macrolide and levofloxaas well as for patients in the surgical group. This occurred despite
cin use (14).
implementation of the screening program. This is consistent
The major limitation of this study is its retrospective design.
with an overall increase in community-acquired MRSA infecTherefore, the majority of patients with a positive screen will
tions, which Mera and colleagues demonstrated as an increase
be in the after cohort when the policy became hospitalwide.
from 22.3% in 1998 to 66.1% in 2007 (11). The purpose of
Since these patients are known to be at increased risk of develthe MRSA screening program is to protect patients without
oping MRSA infection and were omitted from the final analyprevious colonization from acquiring an MRSA infection while
sis by our study criteria, this could potentially create a falsely
in the hospital (HA-MRSA-I). While the desired outcome is to
elevated rate of HA-MRSA-I in the before group. However,
decrease MRSA infection rates hospitalwide, surveillance progiven the retrospective observational nature of the study, the
grams can also have a positive impact on HA-MRSA-I, despite
data pertaining to the rate of nasal carriage in the before group
an overall increase in MRSA infection rate.
were not available. Nonetheless, the method of documenting
When excluding patients with a history of MRSA infection
HA-MRSA-I is consistent between the groups. Furthermore,
or MRSA colonization, the overall HA-MRSA-I rate decreased
no data regarding compliance with the screening protocol were
available for our analysis. Suboptimal compliance with hand hygiene (52%, range 27%–
86%), glove use (62%, range 11%–98%), and
Table 3. MRSA infection rates for patients in both cohorts
the use of gown or other protective clothing
Cohort
Infection
Time
Yes
No
P value
(57%, range 8%–93%) was reported by
All
All positive cultures
Before
453 (1.3%)
35,791 (98.8%)
Gammon et al (15).
Improved MRSA infection rates have
After
1136 (3.2%)
34,932 (96.9%)
<.001
been
demonstrated in certain patient popuOnly HA-MRSA-I
Before
426 (1.2%)
35,791 (98.8%)
lations where more aggressive measures were
After
307 (0.87%)
34,932 (99.1%)
<.001
taken than standard barrier and isolation
Surgical
All positive cultures
Before
236 (1.4%)
16,504 (98.6%)
practices. MRSA infection rates decreased
After
345 (2.3%)
14,699 (97.7%)
<.001
by 93% in cardiac surgical wounds after a
Only HA-MRSA-I
Before
229 (1.4%)
16,504 (98.6%)
program was initiated that not only screened
patients, but included additional intervenAfter
148 (1.0%)
14,699 (99.0%)
0.002
tions such as decolonizing hospital staff
HA-MRSA-I indicates health care–associated methicillin-resistant Staphylococcus aureus infection.
who screen positive, providing vancomycin
Table 2. Comparison of surgical versus nonsurgical patients
April 2014
Impact of a surveillance screening program on rates of MRSA
85
Table 4. Factors associated with health care–associated methicillin-resistant
Staphylococcus aureus infection
Category
Variable
Odds ratio
95% CI
P value
(0.63, 0.85)
<.001
In all patients
Cohort
Before
After
Surgery
0.73
No (referent)
—
Yes
1.3
(1.12, 1.51)
<.001
1
(1.00, 1.01)
0.07
Male (referent)
—
Age
Sex
—
HA-MRSA-I remains a serious problem
in the modern health care environment. Our
study suggests that surveillance programs are
effective in decreasing these infections, both
hospitalwide and among surgical patients. We
also confirm the increased mortality associated
with HA-MRSA-I. Further studies are needed
to aid in the reduction of the transmission of
this disease among hospitalized patients, with
particular focus on African American patients
and those with increased lengths of stay.
1. Shorr AF. Epidemiology of staphylococcal resistance.
Clin Infect Dis 2007;45(Suppl 3):S171–S176.
2.
Cosgrove
SE, Sakoulas G, Perencevich EN, Schwaber
Race
White (referent)
—
MJ, Karchmer AW, Carmeli Y. Comparison of morAfrican American
1.31
(1.1, 1.55)
0.002
tality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia:
Hispanic
0.99
(0.77, 1.28)
0.15
a meta-analysis. Clin Infect Dis 2003;36(1):53–59.
Asian
0.29
(0.07, 1.18)
0.10
3. Blot SI, Vandewoude KH, Hoste EA, Colardyn FA.
Other
0.65
(0.31, 1.38)
0.65
Outcome and attributable mortality in critically ill
patients with bacteremia involving methicillin-susLength of stay
1.05
(1.05, 1.06)
<.001
ceptible and methicillin-resistant Staphylococcus auIn the after cohort
reus. Arch Intern Med 2002;162(19):2229–2235.
4. Anderson DJ, Sexton DJ, Kanafani ZA, Auten G,
Surgery
No (referent)
—
Kaye KS. Severe surgical site infection in commuYes
1.33
(1.05, 1.70)
<.0167
nity hospitals: epidemiology, key procedures, and
Age
1.00
(1.0, 1.01)
0.3334
the changing prevalence of methicillin-resistant
Staphylococcus aureus. Infect Control Hosp Epidemiol
Sex
Male (referent)
—
2007;28(9):1047–1053.
Female
0.49
(0.39, 0.62)
<.0001
5. Hidron AI, Edwards JR, Patel J, Horan TC, Sievert
DM, Pollock DA, Fridkin SK; National HealthRace
White (referent)
—
care Safety Network Team; Participating National
African American
1.48
(1.45, 1.91)
0.0212
Healthcare Safety Network Facilities. NHSN annual
Hispanic
1.00
(0.69, 1.47)
0.7821
update: antimicrobial-resistant pathogens associated
with healthcare-associated infections: annual sumAsian
0.69
(0.17, 2.79)
0.5864
mary of data reported to the National Healthcare
Other
0.73
(0.27, 1.98)
0.5479
Safety Network at the Centers for Disease Control
Length of stay
1.05
(1.03, 1.04)
<.0001
and Prevention, 2006–2007. Infect Control Hosp
Epidemiol 2008;29(11):996–1011.
6. Muto CA, Jernigan JA, Ostrowsky BE, Richet HM,
Jarvis WR, Boyce JM, Farr BM; SHEA. SHEA
prophylaxis for patients who screen positive, and adminguideline for preventing nosocomial transmission of multidrug-resistant
strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epiistering mupirocin calcium nasal ointment for all patients
demiol 2003;24(5):362–386.
regardless of screening status (16). MRSA infections at per7. Kallen AJ, Mu Y, Bulens S, Reingold A, Petit S, Gershman K, Ray SM,
cutaneous gastrostomy sites decreased from 12% to 29% over
Harrison LH, Lynfield R, Dumyati G, Townes JM, Schaffner W, Patel PR,
a 33-month period to 2% after a screening and decontaminaFridkin SK; Active Bacterial Core surveillance (ABCs) MRSA Investigation program was initiated. The protocol involved screening
tors of the Emerging Infections Program. Health care-associated invasive
MRSA infections, 2005–2008. JAMA 2010;304(6):641–648.
for MRSA from multiple sites, nasal treatment with mupiro8. Thompson RL, Cabezudo I, Wenzel RP. Epidemiology of nosocomial
cin, and daily skin decontamination prior to the procedure
infections caused by methicillin-resistant Staphylococcus aureus. Ann Intern
(17). MRSA infection rates among ICU patients decreased
Med 1982;97(3):309–317.
from 3.0% to 1.5% when enhanced cleaning procedures were
9. Parvez N, Jinadatha C, Fader R, Huber TW, Robertson A, Kjar D, Corneused in rooms previously occupied by patients with MRSA. A
lius LK. Universal MRSA nasal surveillance: characterization of outcomes
at a tertiary care center and implications for infection control. South Med
similar reduction in vancomycin-resistant enterococci infecJ 2010;103(11):1084–1091.
tion rates from 3.0% to 2.2% was also demonstrated (18).
10. Harbarth S, Fankhauser C, Schrenzel J, Christenson J, Gervaz P,
However, Camus and colleagues did not show a reduction in
Bandiera-Clerc C, Renzi G, Vernaz N, Sax H, Pittet D. Universal screening
MRSA acquisition in the ICU setting with more aggressive
for methicillin-resistant Staphylococcus aureus at hospital admission and nosointervention protocols, including repeated MRSA screening,
comial infection in surgical patients. JAMA 2008;299(10):1149–1157.
11. Mera RM, Suaya JA, Amrine-Madsen H, Hogea CS, Miller LA, Lu EP,
contact and droplet isolation precautions, and decontaminaSahm DF, O’Hara P, Acosta CJ. Increasing role of Staphylococcus aureus and
tion with nasal mupirocin and chlorhexidine body wash for
community-acquired methicillin-resistant Staphylococcus aureus infections
MRSA-positive patients (19).
Female
86
0.56
(0.48, 0.65)
<.001
Baylor University Medical Center Proceedings
Volume 27, Number 2
Table 5. Odds ratio of screening positive for MRSA colonization
and of death for patients with health care–associated MRSA
infection
Category
Variable
Odds ratio
95% CI
12.
13.
P value
Screening positive for MRSA colonization
Surgery
No (referent)
Yes
Age
Sex
Male (referent)
Female
Race
0.53
(0.45, 0.62) <.0001
1.02
(1.02, 1.03) <.0001
—
0.77
White (referent)
—
African American
1.41
(0.67, 0.89)
0.0003
(1.21, 1.64)
0.0312
Hispanic
0.70
(0.53, 0.92)
0.0003
Asian
1.50
(0.81, 2.76)
0.2783
Other
1.31
(0.79, 2.17)
0.5250
14.
15.
16.
17.
Death for patients with health care–associated MRSA infection
All patients
Surgical patients
Before
3.27
(2.40, 4.46) <.0001
After
3.12
(2.12, 4.60) <.0001
Before
5.06
(3.12, 8.21) <.0001
After
4.84
(2.51, 9.32) <.0001
MRSA indicates methicillin-resistant Staphylococcus aureus.
April 2014
18.
19.
in the United States: a 10-year trend of replacement and expansion. Microb
Drug Resist 2011;17(2):321–328.
Stenehjem E, Rimland D. MRSA nasal colonization burden and risk of
MRSA infection. Am J Infect Control 2013;41(5):405–410.
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, Harrison
LH, Lynfield R, Dumyati G, Townes JM, Craig AS, Zell ER, Fosheim GE,
McDougal LK, Carey RB, Fridkin SK; Active Bacterial Core surveillance
(ABCs) MRSA Investigators. Invasive methicillin-resistant Staphylococcus
aureus infections in the United States. JAMA 2007;298(15):1763–
1771.
Graffunder EM, Venezia RA. Risk factors associated with nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection including previous
use of antimicrobials. J Antimicrob Chemother 2002;49(6):999–1005.
Gammon J, Morgan-Samuel H, Gould D. A review of the evidence for
suboptimal compliance of healthcare practitioners to standard/universal
infection control precautions. J Clin Nurs 2008;17(2):157–167.
Walsh EE, Greene L, Kirshner R. Sustained reduction in methicillinresistant Staphylococcus aureus wound infections after cardiothoracic
surgery. Arch Intern Med 2011;171(1):68–73.
Thomas S, Cantrill S, Waghorn DJ, McIntyre A. The role of screening
and antibiotic prophylaxis in the prevention of percutaneous gastrostomy
site infection caused by methicillin-resistant Staphylococcus aureus. Aliment
Pharmacol Ther 2007;25(5):593–597.
Datta R, Platt R, Yokoe DS, Huang SS. Environmental cleaning intervention and risk of acquiring multidrug-resistant organisms from prior room
occupants. Arch Intern Med 2011;171(6):491–494.
Camus C, Bellissant E, Legras A, Renault A, Gacouin A, Lavoué S, Branger
B, Donnio PY, le Corre P, Le Tulzo Y, Perrotin D, Thomas R. Randomized
comparison of 2 protocols to prevent acquisition of methicillin-resistant
Staphylococcus aureus: results of a 2-center study involving 500 patients.
Infect Control Hosp Epidemiol 2011;32(11):1064–1072.
Impact of a surveillance screening program on rates of MRSA
87
Improving hospital staff compliance with environmental
cleaning behavior
Lilly Ramphal, MD, MPH, Sumhiro Suzuki, PhD, Izah Mercy McCracken, and Amanda Addai, MPH
Reducing the incidence of healthcare-associated infections requires
proper environmental cleanliness of frequently touched objects within
the hospital environment. An intervention was launched in June 2012
and repeated in February 2013 and August 2013 to increase hospital
room cleanliness with repeated education and training of nursing and
environmental services staff to reduce healthcare-associated infections
at Cook Children’s Medical Center. Random rooms were tested, staff were
trained about proper cleaning, rooms were retested for surface cleanliness, and preintervention and postintervention values were compared.
The percentage of cleaned surfaces improved incrementally between the
three trials—with values of 20%, 49%, and 82%—showing that repeat
training favorably changed behavior in the staff (P = 0.007). During the
study period, during which other infection control interventions were
also introduced, there was a decline from 0.27 to 0.21 per 1000 patient
days for Clostridium difficile infection, 0.43 to 0.21 per 1000 patient
days for ventilator-associated infections, 1.8% to 1.2% for surgical site
infections, and 1.2 to 0.7 per 1000 central venous line days for central
line–associated bloodstream infections.
he Centers for Disease Control and Prevention (CDC)
estimated that in 2002, healthcare-associated infections
(HAIs) contributed to 1.7 million infections and 99,000
deaths; 33,269 infections were in high-risk newborns,
19,059 in well-baby nurseries, 417,946 among adults and children in intensive care units, and 1,266,851 in adults and children outside of intensive care units. The overall annual direct
medical costs of HAIs to US hospitals ranges from a low of
$28.4 billion to a high of $45 billion (after adjusting to 2007
dollars using the Consumer Price Index for inpatient hospital
services) (1–4). Prevention of HAIs could save an estimated
$5.7 to a high of $31.5 billion in inpatient hospital services.
For this reason, HAIs have been identified by the US Department of Health and Human Services as a top priority for cost
reduction. Over 11,500 healthcare facilities in all 50 states use
the CDC’s National Healthcare Safety Network to track HAIs.
Thirty states and the District of Columbia require reporting of
HAIs using this network (1).
The CDC has documented that HAIs are caused by many
pathogenic organisms present on floors, bedding, mops, and
furniture in the hospital environment (1, 2, 5–8)—what the
T
88
CDC has called “high-touch points/objects” (HTOs). Through
clinicians’ hands and the environment, patients may be exposed
to pathogenic bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) and enterococcus (6, 7, 9, 10). Several studies
have documented the importance of cleaning and disinfecting
and its impact in preventing transmission of pathogens from
the environment to providers and patients in a broad range of
US healthcare settings (2). This study evaluated whether training interventions would be effective in changing the behavior
in nurses and environmental services (EVS) staff in cleaning
patient rooms after discharge. Baseline results suggested that
several interventions were needed. The ultimate goal was to
decrease the rate of HAIs.
METHODS
This research was considered a quality improvement project and so was exempt from review by the institutional review board at Cook Children’s Hospital. After patients were
discharged from their rooms, a public health student entered
random rooms on the medical and surgical floors and lightly
swabbed HTOs with clear Glo Germ gel before EVS staff or
nurses performed routine cleaning duties in each room. The
staff was blinded with respect to which rooms were going to be
sampled for inclusion in the study. HTOs were marked with a
fluorescent marking gel (invisible to the naked eye) evaluated
with ultraviolet blue light and then interpreted with Ecolab
Recording software after the patients were discharged from the
rooms and before the staff came to clean. After the cleaning,
the HTOs were evaluated with blue light. If the gel mark was
completely wiped off, then the cleaning was recorded as pass. If
any surface gel was still present, then the cleaning was recoded
as fail. For trial 1, 747 random HTOs were sampled; for trial
2, 1322; and for trial 3, 2188. The percentage of clean surfaces
was calculated. This procedure was completed in June 2012,
From Cook Children’s Hospital, Fort Worth, Texas (Ramphal); and the Departments
of Environmental Health (Ramphal, Addai) and Biostatistics (Suzuki, McCracken),
the University of North Texas School of Public Health. Dr. Ramphal is now with
Blue Cross Blue Shield.
Corresponding author: Lilly Ramphal, MD, MPH, Department of Environmental
Health, University of North Texas School of Public Health, 3500 Camp Bowie
Boulevard, Fort Worth, TX 76107-2699 (e-mail: lramphal@yahoo.com).
Proc (Bayl Univ Med Cent) 2014;27(2):88–91
February 2013, and August 2013, following training for nurses
and EVS staff on infection control principles, HTOs, and methods for environmental cleaning and disinfecting.
Data were collected before and after the intervention for
each of the three evaluation periods. Statistical analysis was
performed offsite using an independent sample t test to compare the pre- and postintervention means of surfaces cleaned.
Pearson’s chi-square test was used to determine if there was a
relationship between the cleaning and training for each HTO
object individually. The overall percentage of cleaned surfaces
was compared among the three evaluation periods, and the
overall percentage of cleaned surfaces was compared by buildings and floor levels. The goal was to evaluate the relationship
between interventions and cleaning behavior from trial to trial.
The significance level was set at P = 0.05.
RESULTS
The Table and Figure show the proportion of surfaces cleaned
before and after the intervention for each of the three periods.
Overall, the proportion of surfaces cleaned increased incrementally from 20% in June 2012 to 49% in February 2013 and 81%
in August 2013 (P = 0.007, df 25). In the third trial in August
2013, when some preintervention values were already improved
based on prior and ongoing training, there were still significant
improvements for three HTOs—the toilet seat, flush handle,
and bedpan (P = 0.03, 0.003, and 0.027, respectively).
DISCUSSION
An important component to reducing the incidence of HAIs
is getting buy-in from the staff to address the importance of
labor-intensive cleaning of HTOs (9–12). This study shows that
ongoing training followed by blinded monitoring with transparent reporting of the results in a positive, engaging manner will
motivate staff to improve cleaning behavior. Intense strategies
to reduce HAIs were ongoing in the hospital during the period
from June 2012 to August 2013; therefore, it is not surprising
that the overall rate of HAIs decreased substantially. During the
study period, there was a decline from 0.27 to 0.21 per 1000
patient days for Clostridium difficile infection, 0.43 to 0.21 per
1000 patient days for ventilator-associated infections, 1.8% to
1.2% for surgical site infections, and 1.2 to 0.7 per 1000 central
venous line days for central line–associated bloodstream infections. Other strategies to reduce HAIs were implemented during
the same time period to increase healthcare providers’ awareness
of hand washing during procedures and to supply them with
better kits for line-changing procedures. What portion of the
Table. Percentage of high-touch objects cleaned before and after three training interventions
June 2012
High-touch room surfaces
Surfaces
tested (n)
Surfaces
Surfaces
cleaned (n) cleaned (%)
February 2013
August 2013
Surfaces Surfaces
Surfaces
tested (n) cleaned (n) cleaned (%)
Surfaces Surfaces
Surfaces
tested (n) cleaned (n) cleaned (%)
Bed rail
44
18
41.0
43
21
49
132∗
83
63
TV control
22
1
4.5
20
15
75
71
50
70
Tray table
24
21
88
24
15
63
99
92
93
IV pole (grab area)
19
2
11
19
10
53
99
70
71
120∗
83
69
Nurse call button
28
5
18
20
12
60
Bed angle button
Telephone
28
4
14
28
14
50
39
27
70
23
16
70
23
19
83
108
67
62
Bedside table handle
26
3
12
26
10
38
83
58
70
Game controller side
42
10
24
40
22
55
143
100
70
Cubby handle
48
5
10
48
23
58
131∗
92
71
Chair arm
82
17
21
78
42
54
176
100
57
Chair headrest
39
5
13
32
9
28
99
58
59
Diaper scale top
15
5
33
15
5
33
91
78
86
Diaper scale button
21
3
14
19
10
53
246*
192
78
Light switch
58
3
5
58
21
36
119
75
63
75
72
4
42
17
40
104∗
1
4
25
14
56
37
28
75
7
28
25
13
52
32
30
93
2
8
24
8
33
56
50
90
44
Door knob
47
2
Computer mouse
25
Computer table
25
Computer keyboard
24
Computer pull-out tray
Total
18
0
658
130
0
18
8
20%
627
308
49%
34
27
1900
1435
80
76%
*Grouped data
April 2014
Improving hospital staff compliance with environmental cleaning behavior
89
Figure. Percentage of high-touch objects cleaned after a training intervention for the three trial periods.
decrease in HAIs was due to environmental cleaning is difficult
to calculate; however, decreasing the contribution of pathogens
from the environment surely had an impact, as established by
the CDC and various studies. Current accomplishments in HAI
eradication have been encouraging, but much more needs to be
done to promote the elimination of HAIs due to environmental
contamination (13–24).
Other studies have also shown that targeted efforts to reduce
HAIs, including environmental cleaning, can have significant results. The Jewish Hospital (Mercy Health) in Cincinnati, Ohio,
formed a multidisciplinary task force that included physicians,
nurses, pharmacists, experts, administrators, and EVS staff. The
group concentrated on standardization of clinical care, broadspectrum antibiotic use, and environmental cleaning to reduce
the rate of C. difficile (primarily in the older population) from
25.27 per 10,000 to 3.08 per 10,000 in less than 2 years. The
emphasis on environmental cleaning had an instant effect on C.
difficile rates. The EVS staff changed curtains during cleaning of
rooms, cleaned bathrooms twice daily, used bleach, used soap
and water for handwashing instead of alcohol gel products, and
used laundry sanitizer to kill bacteria on microfiber mop strips
and clothes. They also used a real-time adenosine triphosphate
to detect any residual left behind after the room was cleaned,
which provided quick feedback that helped with effectively
cleaning HTOs after patient discharge (25).
Commonly, the focus of infection control is to prevent
provider or patient-to-patient transmission of infectious
microorganisms. A presentation at the annual meeting of the
Association of Operative Registered Nurses reported on a study
conducted in 79 operating rooms across five hospitals showing
that best practices, accurate products and tools, an unbiased
environmental monitoring tool, and timely staff feedback advance the value of disinfection cleaning (24). Successful strategies to control HAIs have been used in Colorado, Florida,
Wisconsin, Oregon, and Minnesota to reduce infections with
carbapenem-resistant Enterobacteriaceae with increased surveillance, increased antibiotic stewardship, and isolation precautions. Tennessee and Colorado have reduced infections in
90
central line–associated bloodstream infections through increased
training and guidance, improved data collection, improved
communication during transfer of patients between facilities,
and improved tracking. Massachusetts, New York, and Illinois
have reduced the rate of infections with C. difficile by having statewide full-day regional workshops and using uniform
measurement and reporting tools. Improvements are patient
focused, and sampling of the environment is rarely mentioned
(1). The participation of the entire hospital staff and the use of
constructive methods to approach staff are critical for the success
of these public health achievements (1, 8, 14, 15, 19–22, 26).
Centers for Disease Control and Prevention. Healthcare-associated infections.
Available at http://www.cdc.gov/hai/.
2. Carling PC, Bartley JM. Evaluating hygienic cleaning in health care settings: what you do not know can harm your patients. Am J Infect Control
2010;38(5 Suppl 1):S41–S50.
3. Sehulster L, Chinn RY; CDC; HICPAC. Guidelines for environmental
infection control in health-care facilities. MMWR Recomm Rep 2003;52
(RR-10):1–42.
4. Siegel JD, Rhinehart E, Jackson M, Chiarello L; Healthcare Infection Control
Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Atlanta, GA: CDC.
Available at http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf
5. Mayo Clinic. C. difficile: Intervention drops hospital infection rate by a
third. ScienceDaily 2010 (March 30). Available at www.sciencedaily.com/
releases/2010/03/100319142658.htm.
6. Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory
Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force.
Guideline for hand hygiene in health-care settings. MMWR Recomm Rep
2002;51(RR-16):1–45.
7. Dancer SJ. Importance of the environment in meticillin-resistant Staphylococcus aureus acquisition: the case for hospital cleaning. Lancet Infect Dis
2008;8(2):101–113.
8. Dancer SJ. The role of environmental cleaning in the control of hospitalacquired infection. J Hosp Infect 2009;73(4):378–385.
9. Otter JA, French GL. Survival of nosocomial bacteria and spores on
surfaces and inactivation by hydrogen peroxide vapor. J Clin Microbiol
2009;47(1):205–207.
10. French GL, Otter JA, Shannon KP, Adams NM, Watling D, Parks MJ. Tackling
contamination of the hospital environment by methicillin-resistant Staphylococcus
aureus (MRSA): a comparison between conventional terminal cleaning and
hydrogen peroxide vapour decontamination. J Hosp Infect 2004;57(1):31–37.
1.
Baylor University Medical Center Proceedings
Volume 27, Number 2
11. Worthy B, Galan B. A strategy for pathogens: how ES can help
drive infection prevention efforts. Environmental Services 2012
(July). Available at http://www.hfmmagazine.com/hfmmagazine/jsp/
articledisplay.jsp?dcrpath=HFMMAGAZINE/Article/data/07JUL2012/
0712HFM_FEA_EnviromentServices&domain=HFMMAGAZINE.
12. Gould C, McDonald C; Division of Healthcare Quality and Promotion,
Centers for Disease Control and Prevention. Clostridium difficile (CDI) Infections Toolkit: Activity C: ELC Prevention Collaboratives. Atlanta, GA: CDC,
2009. Available at http://www.cdc.gov/hai/pdfs/toolkits/CDItoolkitwhite_
clearance_edits.pdf.
13. Hartmann B, Benson M, Junger A, Quinzio L, Röhrig R, Fengler B,
Färber UW, Wille B, Hempelmann G. Computer keyboard and mouse
as a reservoir of pathogens in an intensive care unit. J Clin Monit Comput
2004;18(1):7–12.
14. Illinois Department of Public Health. Illinois Hospital Report Card and
Consumer Guide to Health Care. Available at http://www.healthcarere
portcard.illinois.gov/contents/view/health_care_associated_infections.
15. Jefferson J, Whelan R, Dick B, Carling P. A novel technique for identifying
opportunities to improve environmental hygiene in the operating room.
AORN J 2011;93(3):358–364.
16. Kleinpell RM. The role of the critical care nurse in the assessment and
management of the patient with severe sepsis. Crit Care Nurs Clin North
Am 2003;15(1):27–34.
17. Klevens RM, Edwards JR, Richards CL Jr, Horan TC, Gaynes RP,
Pollock DA, Cardo DM. Estimating health care-associated infections
and deaths in U.S. hospitals, 2002. Public Health Rep 2007;122(2):
160–166.
April 2014
18. Reed D, Kemmerly SA. Infection control and prevention: a review of
hospital-acquired infections and the economic implications. Ochsner J
2009;9(1):27–31.
19. Illinois Hospital Association. Better to Best: 2011 Quality Excellence
Achievement Award Compendium. Available at https://www.ihatoday.org/
uploadDocs/1/2011-Quality-Awards-Compendium.pdf.
20. Rutala WA, Weber DJ. Current principles and practices; new research;
and new technologies in disinfection, sterilization, and antisepsis. Am J
Infect Control 2013;41(5 Suppl):S1–S118.
21. Healthcare Infection Control Practices Advisory Committee. Updating the
Guideline Methodology of the Healthcare Infection Control Practices Advisory Committee. Atlanta, GA: CDC, December 2009. Available at http://www.cdc.gov/
hicpac/pdf/guidelines/2009-10-29HICPAC_GuidelineMethodsFINAL.pdf.
22. Rutala WA, White MS, Gergen MF, Weber DJ. Bacterial contamination
of keyboards: efficacy and functional impact of disinfectants. Infect Control
Hosp Epidemiol 2006;27(4):372–377.
23. Rutala WA, Weber DJ. Sterilization, high-level disinfection, and environmental cleaning. Infect Dis Clin North Am 2011;25(1):45–76.
24. Wolf B, Homan L. A programmatic approach to improve environmental
cleaning in the OR. AORN 59th Annual Congress, New Orleans, LA,
March 24–29, 2012.
25. Eisler P. Hospital successfully battles C. diff. USA Today, August 16, 2012.
Available at http://usatoday30.usatoday.com/news/health/story/2012-08-16/
cincinnati-hospital-clostridium-difficile/57079520/1.
26. Howie R, Alfa MJ, Coombs K. Survival of enveloped and non-enveloped
viruses on surfaces compared with other micro-organisms and impact of
suboptimal disinfectant exposure. J Hosp Infect 2008;69(4):368–376.
Improving hospital staff compliance with environmental cleaning behavior
91
Ethnic disparities in the prevalence of the metabolic syndrome
in American adults: data from the Examination of National
Health and Nutrition Examination Survey 1999–2010
Lilly Ramphal, MD, MPH, Jun Zhang, MPH, and Sumhiro Suzuki, PhD
Data from the National Health and Nutrition Examination Survey were
stratified by weight, gender, and ethnicity for six survey years from 1999
to 2010 for variables that satisfy the criteria for metabolic syndrome
(MS). Results showed that 34% of the US adult population had MS. No
significant gender disparities in MS prevalence were found. Black men
had a significantly lower prevalence of MS than Black women and White
men from 1999 to 2008 (P < 0.05). Women had a 60% higher abdominal
adiposity than men in the US population (P = 0.00048; pregnant females
were excluded). Although there seem to be ethnic differences in the
prevalence of MS, the expression of MS is not a sufficient risk to culminate
in cardiovascular disease; rather, nutritional, genetic, and environmental
factors are necessary to finalize its expression into overt disease.
ndividuals with the metabolic syndrome (MS) are at increased
risk for cardiovascular disease. Multiple definitions based on
different organizations’ guidelines are used to define MS. In
2007, the International Diabetes Federation (IDF) provided
a definition of MS that differed from that of the National Cholesterol Education Program (NCEP) (Table 1). This study used
the IDF’s definition of MS because it is more stringent (1).
MS is a major health problem globally and can vary in some
ethnic groups (2). Limited information is available regarding
the prevalence of MS and its trend using IDF’s definition in
the US. To date, most population-based studies using IDF’s
criteria were conducted outside the US (3). Previous studies cite
some ethnic disparity in the prevalence of MS and its various
components. Papoutsakis et al found that non-Hispanic Black
adolescent males had lower odds of having MS (4). Palaniappan et al showed that Asian Americans had a greater prevalence
of MS despite having a low body mass index (BMI) and a
lower prevalence of being overweight or obese (2). Fitzpatrick
et al demonstrated that African American adolescents are less
likely to have MS compared with non-Hispanic White groups
(5). Cardiovascular risk factors that define MS are associated
with weight status, and differences exist among African Americans and Hispanics when compared with White ethnic groups
(5–11). Ford et al estimated the prevalence of MS in the US as
defined by Adult Treatment Panel (ATP) reports based on National Health and Nutrition Examination Survey (NHANES)
surveys from 1988 to 1994 (7). Ervin et al examined individual
I
92
Table 1. Varying definitions of the metabolic syndrome
Criteria
NCEP
NCEP revised
IDF
Waist circumference >102 in men
(cm)
>88 in women
>102 in men
>88 in women
≥94 in men
≥80 in women
Triglyceride (mmol/L) ≥1.7
≥1.7
≥1.7
HDL cholesterol
(mmol/L)
<1.03 in men
<1.03 in men
<1.03 in men
<1.29 in women <1.29 in women <1.29 in women
Systolic cuff blood
pressure (mm Hg)
≥130
≥130
≥130
Diastolic cuff blood
pressure (mm Hg)
≥85
≥85
≥85
Fasting glycemia
(mmol/L)
≥6.1
≥5.6
≥5.6
Definition
Meet 3 or more Meet 3 or more Meet waist
criteria
criteria
circumstance
criterion and 2 or
more other criteria
NCEP indicates National Cholesterol Education Program; IDF, International Diabetes
Foundation; HDL, high-density lipoprotein.
risk factors for MS defined by NCEP criteria using NHANES
data from 2003 to 2006 (8). No recent study has been done
that examines MS as defined by the IDF among adult ethnic
groups in the US.
Obese individuals are more likely to have MS compared
with normal-weight individuals. Vakil et al demonstrated that
waist circumference is independently associated with an increased prevalence of coronary artery disease and thus is heavily weighted with risk factors for cardiovascular risk (9). Few
studies have been done to show how weight status and MS are
distributed among different ethnicities in the US adult population. The purpose of this study was to identify trends in the
prevalence of MS in the US population as defined by the IDF
From the Departments of Environmental Health (Ramphal) and Biostatistics (Zhang),
the University of North Texas School of Public Health, Fort Worth, Texas.
Corresponding author: Lilly Ramphal, MD, MPH, Department of Environmental
Health, University of North Texas School of Public Health, 3500 Camp Bowie
Boulevard, Fort Worth, TX 76107-2699 (e-mail: lramphal@yahoo.com).
Proc (Bayl Univ Med Cent) 2014;27(2):92–95
Table 2. The proportion of the US population with the metabolic syndrome stratified by ethnicity and gender
based on data from the National Health and Nutrition Examination Survey
1999–2000
(n = 4693)
Ethnicity
2001–2002
(n = 5266)
2003–2004
(n = 5050)
2005–2006
(n = 4980)
2007–2008
(n = 5938)
2009–2010
(n = 6292)
Female Male Female Male Female Male Female Male Female Male Female Male
% (SD) % (SD) % (SD) % (SD) % (SD) % (SD) % (SD) % (SD) % (SD) % (SD) % (SD) % (SD)
Mexican
American
36.17
(2.95)
26.21
(2.51)
38.35
(2.96)
27.90∗∗
(2.43)
41.08
(3.58)
23.27∗∗
(2.62)
37.57
(3.30)
24.73∗∗
(2.59)
40.44
(3.02)
32.84
(2.78)
40.44
(2.75)
37.32
(2.64)
Other
Hispanic
39.76
(5.50)
33.35
(5.35)
29.31
(6.67)
27.86
(5.89)
26.57
(7.47)
24.60
(7.14)
27.47
(7.27)
28.99
(7.27)
38.09
(3.58)
32.57
(3.51)
34.62
(3.45)
28.91
(3.29)
Non-Hispanic
White
34.16
(2.06)
31.43
(1.91)
32.95
(1.37)
37.05
(1.77)
34.30
(1.87)
34.51
(1.83)
31.19
(1.90)
34.81
(1.84)
37.43
(1.89)
36.17
(1.78)
33.42
(1.73)
31.58
(1.72)
Non-Hispanic
Black
38.89
(3.23)
17.03∗∗
(2.16)
34.11
(2.99
20.97∗∗
(2.21)
34.81
(3.00)
20.13∗∗
(2.28)
34.82
(2.81)
24.22∗∗
(2.28)
39.24
(2.74)
18.3∗∗
(1.93)
39.54
(2.92)
25.03∗
(2.25)
Other race,
incl. multiple
47.28
(8.60)
21.18
(5.56)
37.81
(6.86)
25.23
(6.15)
30.54
(5.93)
23.32
(5.77)
22.63
(5.09)
32.17
(6.75)
32.85
(6.41)
21.98
(5.2)
25.93
(4.39)
17.35
(4.07)
Total†
35.82
(1.63)
29.14∗
(1.44)
33.40
(1.41)
33.52
(1.37)
34.27
(1.49)
30.98
(1.41)
31.26
(1.48)
32.38
(1.42)
37.60
(1.45)
32.87
(1.32)
34.12
(1.37)
30.23
(1.59)
∗
P < 0.05 comparing MS prevalence between genders.
P < 0.05 compared with White Americans.
†Percentages are weighted estimates in each category; therefore, column totals do not add up to 100%.
∗∗
criteria from 1999 to 2010. The secondary purpose was to find
ethnic disparities of the prevalence of MS in the adult US population when stratified by abdominal adiposity, ethnicity, weight
status, and gender.
METHODS
The study was approved with minimal review by the University of North Texas institutional review board since NHANES
is a public database. Our study examined prevalence and trends
using six surveys from 1999 to 2010. NHANES is a crosssectional health and nutrition survey representative of the
American population conducted by the Centers for Disease
Control and Prevention’s National Center for Health Statistics. The survey design involves a complex, stratified, multistage
sample of noninstitutionalized US civilians. The data sampled
low-income people, adolescents 12 to 19 years of age, people
60 years of age and over, African Americans (Blacks), Mexican
Americans, Other Hispanics (non-Mexican Hispanics), nonHispanic Whites (Caucasians or Whites), and other ethnicity
(mixed race and Asians). Subjects aged 18 and above were included, and pregnant women were excluded from the sample.
Data on glucose measurements (defined as 8 hours fasting
glucose), serum triglycerides, high-density lipoproteins, systolic and diastolic blood pressure, and waist circumference were
extracted from the database as components of the IDF criteria
for MS. Missing data were marked as missing. There were 4693
eligible observations in the 1999–2000 NHANES data, 5266 in
2001–2002, 5050 in 2003–2004, 4980 in 2005–2006, 5938 in
2006–2007, and 6292 in 2009–2010. We used the IDF definition for MS and calculated MS prevalence from this database.
April 2014
BMI was available in the dataset, which made it possible to
calculate MS distribution, which was then stratified by weight
status, gender, and ethnicities. Data were analyzed using SAS
statistics, and Student’s t test was used to compare differences in
the prevalence of MS in each ethnic and gender category.
RESULTS
Overall, 34% of the US population studied had MS, and
there was no significant difference in the prevalence of MS
between men and women overall (P = .20). Table 2 lists the
prevalence of MS stratified by gender and ethnicity. Black men
consistently had a significantly lower prevalence of MS compared with Black women and Whites in most years (1999–
2008) (P < 0.05). Mexican American men consistently had a
significantly lower prevalence of MS than Mexican American
women from 2001 to 2006 (P < 0.05). Other ethnicities did
not show a consistently significant difference in the prevalence
of MS between genders in any survey year. Black women had a
consistently higher (but insignificant) prevalence of MS when
compared with White women. Similar findings were present
for Mexican American women. No overall trend was noted in
the prevalence of MS for the US population over the 12 years
of the study period.
Table 3 shows the conditional distribution of oversized waist
circumference when stratified by ethnicity, weight status, and
gender. Women had consistently larger abdominal obesity than
men (P = 0.00048), which was most notable in the normal
weight category. For Mexican American or White ethnicities,
a person in the obese category had a high waist circumference 100% of the time. In the underweight category, very few
Ethnic disparities in the prevalence of the metabolic syndrome in American adults
93
Table 3. Conditional proportion of US population with oversized waist circumference in each ethnic group, stratified by
weight category and gender distribution, based on data from the National Health and Nutrition Examination Survey
% Oversized waist circumference
Ethnicity
Mexican
American
Weight
category
Male
Female
Female
Male
Female
2007–2008
Male
Female
2009–2010
Male
Female
9.4
50.6
9.5
53.1
8.8
59.4
7.3
57.0
9.0
55.7
Obese
100.0
100.0
100.0
100.0
100.0
100.0
100.0
100.0
99.4
100.0
100.0
100.0
Overweight
67.2
94.0
65.5
96.6
74.2
99.4
68.4
98.0
67.8
100.0
75.2
99.0
Underweight
0.0
8.3
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
56.0
78.9
51.5
80.6
58.6
85.3
59.4
87.8
62.2
86.3
67.2
88.1
Normal
16.7
34.9
8.3
50.0
5.0
53.1
9.5
44.4
8.8
47.7
6.5
54.1
Obese
100.0
100.0
100.0
100.0
91.7
100.0
100.0
100.0
98.8
100.0
99.0
100.0
Overweight
66.7
92.7
69.0
97.0
58.8
96.2
68.0
95.7
74.4
99.2
64.9
100.0
Underweight
0.0
0.0
0.0
0.0
0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
53.2
76.3
53.2
83.6
48.3
76.7
83.6
59.2
82.2
Overweight
Underweight
Subtotal∗
Non-Hispanic Normal
Black
Obese
Overweight
Underweight
—
78.5
—
19.9
49.1
16.6
47.4
20.2
56.9
17.7
49.9
20.2
57.3
17.6
58.5
100.0
100.0
100.0
100.0
99.4
100.0
100.0
100.0
100.0
100.0
99.8
100.0
81.8
96.8
85.1
97.1
85.0
98.3
83.4
98.2
83.2
99.5
81.2
99.2
0.0
0.0
0.0
2.3
4.3
3.4
61.8
76.4
66.0
73.8
68.2
79.2
0.0
6.0
41.6
3.6
35.0
7.7
41.1
4.9
32.4
100.0
100.0
98.4
100.0
98.0
100.0
100.0
64.7
91.8
59.0
90.8
52.6
97.8
53.1
—
0.0
6.7
2.9
0.0
2.3
80.2
68.5
81.5
8.9
56.8
5.3
44.3
100.0
99.0
100.0
96.5
100.0
96.4
59.6
98.8
63.4
99.2
76.5
0.0
0.0
0.0
0.0
0.0
0.0
45.3
85.2
46.0
81.6
52.4
86.9
Normal
8.3
52.9
2.9
43.6
8.3
44.0
0.0
48.3
Obese
Subtotal∗
—
0.0
83.3
0.0
—
0.0
5.3
0.0
0.0
87.8
53.8
87.9
6.7
44.0
17.3
52.6
—
100.0
100.0
90.9
100.0
100.0
100.0
100.0
100.0
100.0
100.0
100.0
100.0
Overweight
50.0
92.3
57.1
96.7
61.8
100.0
75.0
90.5
63.2
100.0
58.7
95.8
Underweight
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
44.1
69.8
37.9
69.0
48.4
61.1
67.5
47.0
68.2
Subtotal∗
—
64.6
—
are weighted estimates of the population in each ethnic category; therefore, columns do not add up to 100%.
individuals had abnormal waist circumference (P = 0.000). In
the “other ethnicity category,” which included Asians and multiracial individuals, a low abdominal obesity was present as well,
but not at a significant level (P = 0.38), which reflected a lower
prevalence of MS in this group.
DISCUSSION
The IDF definition of MS places emphasis on the waist
circumference and is highly associated with cardiovascular risk.
Although women have a greater chance of having high abdominal obesity and have a higher prevalence of MS, they are at lower
statistical risk for heart disease than men. The prevalence of
MS was four times higher in women in earlier years, although
the last two surveys show an equal prevalence of MS for men
and women. These last two survey years were heavily weighted
with underweight women in all ethnicities in the US popula94
Male
2005–2006
46.8
Non-Hispanic Normal
White
Obese
∗Percentages
Female
2003–2004
7.0
Subtotal∗
Other
Male
2001–2002
Normal
Subtotal∗
Other
Hispanic
1999–2000
tion. Women had better health status than men in most of the
MS indicators, including blood pressure, fasting glucose, and
triglycerides in 2008 to 2010. A similar finding was confirmed
in Erin et al’s study using NCEP criteria (7, 8). MS disparity in
genders was consistently significant among African Americans.
Black men had a significantly lower prevalence of MS than any
other group, including Black women for 12 years and Whites
and Mexican Americans from 1999 to 2008. Mexican American women and Black women were more likely than White
women to have higher waist circumference and MS. The “other
ethnicity” group, including multiracial individuals and Asians,
had the lowest prevalence of abdominal obesity but not the
lowest prevalence of MS. Based on these findings, adiposity
can be expressed with varying distributions among different
ethnicities yet affect the prevalence of MS and cardiovascular
disease differently.
Baylor University Medical Center Proceedings
Volume 27, Number 2
MS is not the gold standard for cardiovascular risk, as
evidenced by the fact that morbidity and mortality are high in
Black and Hispanic Americans and lower in women (8–10).
As noted elsewhere, genetic, nutritional, and environmental
factors that influence the expression of MS and promote and
suppress the expression of full-blown heart disease, coronary
heart disease, and congestive heart disease are essential in the
expression of disease (12–15). It is important to acknowledge
MS as a precursor to cardiovascular risk that can be addressed
in primary prevention efforts. Evidence of a decline in MS
achieved in wellness programs is an indicator of interventional
success; smoking cessation, weight loss, loss of abdominal girth,
and change in eating patterns are some strategies that can be
used to mitigate inherited factors. The interplay of MS with
genetic and behavioral factors on the risk for cardiovascular
disease should be explored in future studies.
1.
2.
3.
4.
5.
Yoon YS, Lee ES, Park C, Lee S, Oh SW. The new definition of metabolic
syndrome by the International Diabetes Federation is less likely to identify
metabolically abnormal but non-obese individuals than the definition by
the revised National Cholesterol Education Program: the Korea NHANES
study. Int J Obes (Lond) 2007;31(3):528–534.
Palaniappan LP, Wong EC, Shin JJ, Fortmann SP, Lauderdale DS. Asian
Americans have greater prevalence of metabolic syndrome despite lower
body mass index. Int J Obes (Lond) 2011;35(3):393–400.
Riediger ND, Clara I. Prevalence of metabolic syndrome in the Canadian
adult population. CMAJ 2011;183(15):E1127–1134.
Papoutsakis C, Yannakoulia M, Ntalla I, Dedoussis GV. Metabolic syndrome in a Mediterranean pediatric cohort: prevalence using International
Diabetes Federation-derived criteria and associations with adiponectin
and leptin. Metabolism 2012;61(2):140–145.
Fitzpatrick SL, Lai BS, Brancati FL, Golden SH, Hill-Briggs F. Metabolic
syndrome risk profiles among African American adolescents: National
Health and Nutrition Examination Survey, 2003–2010. Diabetes Care
2013;36(2):436–442.
April 2014
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Haffner SM, D’Agostino R, Saad MF, Rewers M, Mykkänen L, Selby J,
Howard G, Savage PJ, Hamman RF, Wagenknecht LE, Bergman RN.
Increased insulin resistance and insulin secretion in nondiabetic AfricanAmericans and Hispanics compared with non-Hispanic whites. The Insulin Resistance Atherosclerosis Study. Diabetes 1996;45(6):742–748.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome
among US adults: findings from the third National Health and Nutrition
Examination Survey. JAMA 2002;287(3):356–359.
Ervin RB. Prevalence of metabolic syndrome among adults 20 years of
age and over, by sex, age, race and ethnicity, and body mass index: United
States, 2003–2006. Natl Health Stat Report 2009;(13):1–7.
Su C, Fang C, Chen J, Po HL, Chou LP, Chiang CY, Ueng KC. Prevalence of metabolic syndrome and its relationship with cardiovascular
disease among hypertensive patients 55–80 years of age. Acta Cardiol Sin
2011;27(4):229–237.
National Institutes of Health. Morbidity & Mortality: 2007 Chart Book
on Cardiovascular, Lung, and Blood Diseases. Bethesda, MD: NHLBI.
Available at www.nhlbi.nih.gov/resources/docs/07-chtbk.pdf.
Cherqaoui R, Kassim TA, Kwagyan J, Freeman C, Nunlee-Bland G, Ketete
M, Xu S, Randall OS. The metabolically healthy but obese phenotype in
African Americans. J Clin Hypertens (Greenwich) 2012;14(2):92–96.
King KE, Morenoff JD, House JS. Neighborhood context and social disparities
in cumulative biological risk factors. Psychosom Med 2011;73(7):572–579.
Geronimus AT, Hicken MT, Pearson JA, Seashols SJ, Brown KL, Cruz
TD. Do US black women experience stress-related accelerated biological
aging? A novel theory and first population-based test of black-white differences in telomere length. Hum Nat 2010;21(1):19–38.
Fox CS, Liu Y, White CC, Feitosa M, Smith AV, Heard-Costa N, Lohman
K; GIANT Consortium; MAGIC Consortium; GLGC Consortium,
Johnson AD, Foster MC, Greenawalt DM, Griffin P, Ding J, Newman AB,
Tylavsky F, Miljkovic I, Kritchevsky SB, Launer L, Garcia M, Eiriksdottir
G, Carr JJ, Gudnason V, Harris TB, Cupples LA, Borecki IB. Genomewide association for abdominal subcutaneous and visceral adipose reveals a
novel locus for visceral fat in women. PLoS Genet 2012;8(5):e1002695.
Heid IM, Jackson AU, Randall JC, and 298 more authors. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals
sexual dimorphism in the genetic basis of fat distribution. Nat Genet
2010;42(11):949–960.
Ethnic disparities in the prevalence of the metabolic syndrome in American adults
95
A cohort analysis of the cardiovascular risk factors in the
employees of a pediatric hospital from 2009 to 2012
Lilly Ramphal, MD, MPH, Jun Zhang, MS, and Sumihiro Suzuki, PhD
A retrospective longitudinal cohort regression analysis was completed in
853 of the 3435 employees of Cook Children’s Hospital who participated
all 4 years (2009 to 2012) in an employer wellness program. The presence of the metabolic syndrome (MS) was used as an outcome measure
for the success of the wellness program. Data were stratified by weight,
gender, and ethnicity. The odds ratios and regression analysis showed
a significant decline in MS over the 4 years of the study (P = 0.008), as
well as a significant association between MS and obesity and overweight
status (P < 0.0001), male gender (P = 0.0018), and all ethnic categories
(P < 0.05) except African American ethnicity and the multiple ethnicity
category. Age was strongly associated with risk for MS. Overall, the study
showed that the wellness program significantly decreased the incidence
of MS (P < 0.05).
he metabolic syndrome (MS) is a serious public health
concern defined by interconnected factors that directly
impact the risk of coronary heart disease. MS has been
defined by the International Diabetes Federation (IDF)
and the National Cholesterol Education Program (3). Both
groups present similar criteria for MS, but for purposes of this
study the IDF definition, which put more emphasis on waist
circumference, was used. Waist circumference, independent
of other parameters of MS, is the most significant predictor of
cardiovascular risk (1–3). This study identified trends in the
prevalence of MS in 853 employees who consistently participated in a hospital wellness program from 2009 to 2012.
T
METHODS
The study was approved by the Cook Children’s Hospital
institutional review board. A retrospective longitudinal cohort
regression analysis was completed on 853 (24.8%) volunteers
who had participated in all 4 years of a hospital wellness program
from 2009 to 2012 and had submitted complete demographic
records. A total of 2582 employees were excluded from the
study because they participated inconsistently during the study
period. Participants in the wellness program were incentivized
with an annual monetary award to reduce their cardiovascular
risk by reducing four or more of the measured criteria in 2
consecutive years. Each participant’s demographic information
was obtained from survey health questionnaires collected by the
96
employer’s wellness coordinator. Measured parameters such as
weight, waist circumference, height, and systolic and diastolic
blood pressures were obtained annually by registered nurses. No
formal instruction on how to reduce these parameters was given
to participants. They were referred to their personal doctors for
direction or sought out resources to improve their health.
All data were analyzed by statisticians using SAS. Two
models were used to analyze the variables affecting MS risk:
a conventional logistic regression and a longitudinal generalized estimated equation (GEE) model. Model 1 for the output
analysis is shown below:
Logit[P(MS = 1)] = β0 + β1 ∗ √t + β3 ∗ WeightStatus + β4
∗ Gender + β5 ∗ Ethnicity
Odds ratio estimates were used to evaluate risk. Both analyses
molded in risk factor variables including square root of time,
gender, weight status (normal, overweight, and obese), ethnicities (American Indian, Asian, Black, Hispanic other, Hispanic
White, Multiple, and White), and age groups (18–30, 30–40,
40–50, 50–65, and 65+). In both regression models, 2009 was
the baseline. Normal weight was used as the baseline and compared with overweight and obese categories. The underweight
were excluded due to the very small numbers in this category.
Caucasian (White) ethnicity was set as the baseline and compared to Asian, African American (Black), Hispanic Other, Hispanic White, American Indian, and Pacific Islander ethnicities.
For age, the 18–30 age group was used as the reference group,
and all other age categories were compared to it. All analyses
were performed using SAS (V9.2).
RESULTS
Table 1 presents the demographic characteristics of the 853
participants who were eligible for longitudinal study. More
From Cook Children’s Hospital, Fort Worth, Texas (Ramphal); and the Departments
of Environmental Health (Ramphal) and Biostatistics (Zhang, Suzuki), the University
of North Texas School of Public Health. Dr. Ramphal is now with Blue Cross Blue
Shield.
Corresponding author: Lilly Ramphal, MD, MPH, Department of Environmental
Health, University of North Texas School of Public Health, 3500 Camp Bowie
Boulevard, Fort Worth, TX 76107-2699 (e-mail: lramphal@yahoo.com).
Proc (Bayl Univ Med Cent) 2014;27(2):96–99
Table 1. Demographic characteristics of the 853 hospital
employees in the cohort
Category
Variable
Female
Male
All
Gender
Employee gender
788 (92%)
65 (8%)
853
Ethnicity
American Indian∗
4
Standard Wald ChiParameter∗ DF estimate error square Significance
<.0001
1
–1.031
0.15
45.85
68
Square root of
time†
1
–0.15
0.079
3.7
1 (2%)
53
Obesity
0
1
1.46
0.083 309.4
<.0001
108 (93%)
8 (7%)
116
Overweight
1
1
0.43
0.085
24.5
<.0001
15 (94%)
1 (6%)
16
0.33
0.085
15.4
<.0001
2 (10%)
20
African American (Black)
67 (98%)
1 (2%)
Hispanic other
52 (98%)
Hispanic White
1 (100%)
0.06
Gender
0
1
1
Asian
0
1
1.29
0.30
18.4
<.0001
52 (9%)
575
Black
1
1
–0.77
0.178
18.7
<.0001
2
1
0.19
0.179
1.0
0
Caucasian (White)
523 (91%)
18–30
166 (98%)
3 (2%)
169
Hispanic other
30–40
253 (91%)
26 (9%)
279
Hispanic white
3
1
0.28
0.14
3.9
0.05
40–50
206 (91%)
24 (9%)
230
4
1
–0.71
0.35
4.2
0.04
50–65
159 (94%)
10 (6%)
169
Multiple
ethnicities
65+
4 (67%)
2 (33%)
6
from the study due to small size.
than 90% of participants were women, and 575 of 853 (67%)
were Caucasian. At baseline, the mean age was 39 years for the
women and 42 years for the men. Because of the small sample
in the ethnic groups of American Indian and Pacific Islander,
these individuals were excluded from the analysis. We found
that more obese individuals migrated to the overweight category than overweight individuals migrated towards the obese
category. The normal weight rate kept stable over the 4 years.
The logistic regression model validated a decline of MS over
time (P = 0.02), showing that the program was effective in reducing MS over time in the entire cohort (Table 2). There was an
increased risk of MS in both the obese and overweight categories
(P < 0.0001) compared with the normal weight group. MS risk
increased in men using women as a reference (P < 0.0001), as
well as in Asians (P < 0.0001), Blacks (P < 0.0001), Hispanic
Whites (P = 0.0495), and multiple races (P = 0.04).
The data were also analyzed to determine odds ratios (OR).
There was an overall decrease in the odds of MS in this cohort
from 2009 to 2012 (OR = 0.84, P = 0.02). The odds of having MS were the highest in the obese category (OR = 20.37,
P < 0.0001), followed by the overweight category (OR = 7.42,
P < 0.0001). Men were almost twice as likely to have MS
(OR = 2.02, P < 0.0001) as women. If all other factors were
controlled, several ethnicities had an increased odds of having
MS, including Hispanic other (OR = 2.02, P = 0.0001), Hispanic White (OR = 1.87, P < 0.0001), and Asians, who had
the highest risk for MS (OR = 4.46, P < 0.0001). In contrast,
African Americans had a decreased odds of having MS (OR =
0.69, P = 0.03). Age groups older than the 18–30 year reference group had increased odds of having MS, including the
April 2014
Variable
Intercept
18 (90%)
Pacific Islander∗
∗Excluded
0
Asian
Multiple
Age group
4 (100%)
Table 2. Regression analysis of the metabolic syndrome from
2009 to 2012, stratified by weight, gender, and ethnicity in 853
employees of a pediatric hospital
0.3
∗Weight = 0 for obese and 1 for overweight vs normal; gender = 0 for males vs females;
G = 0, 1, 2, 3, 4 for Asian, Black, Hispanic other, Hispanic White, and Multiple vs White.
†Square root of time = year 2009 to 2012.
40–50 year group (OR = 1.66, P = 0.0015) and the 50–65 year
group (OR = 2.22, P = 0.0001).
The results using the longitudinal GEE logistic model on
the right side of Table 3 confirm a significant decline of MS
over the 4 years of the study (P = 0.004). The same significant association between MS and the obese and overweight
groups was found (P < 0.0001), as well as the increased MS in
men (P = 0.0008) when compared to women. Furthermore,
a significant association between MS and most ethnicities
(P < 0.0001) except for the African American and American
Indian categories (P = 0.23 and 0.4, respectively) was found.
This model also showed that all subjects older than 30 years
had a significantly increased risk for MS, including the 40–50
year group (P < 0.0086) and 50–65 year group (P < 0.0001),
when compared to baseline.
DISCUSSION
There are not many cohort studies that follow MS over time.
Even fewer longitudinal studies have been conducted that focus
on MS and ethnicity factors. Due to limited data, we could not
evaluate the effect of smoking status on the model. However,
smoking status has been found to have a significant effect on
MS in other studies (2). Having a high risk of MS in older age
is consistent with Sun’s finding in 2012 (3).
Our finding on the different risks in ethnicities and possible
protective factors in African Americans in one model of the
longitudinal study is new in the research of MS. It suggests that
African Americans can have better health if obesity and other
factors are better controlled. More research is needed to evaluate
what these protective factors are, since it was not corroborated
A cohort analysis of the cardiovascular risk factors in the employees of a pediatric hospital from 2009 to 2012
97
Table 3. The impact of a wellness program over time on the metabolic syndrome parameters in 853 employees of a pediatric
hospital, stratified by weight, gender, and ethnicity
95% confidence
Parameter
Estimate
GEE standard error
Parameter error
Estimates
Z
Pr> |Z|
Intercept
–3.16
0.19
–3.53
–2.7929
Square root of time*
–0.17
0.063
–0.29
–0.044
–2.65
0.008
–16.8
<.0001
Obese
0
2.78
0.21
2.37
3.19
13.17
<.0001
Overweight
1
1.93
0.20
1.54
2.31
9.84
<.0001
Normal weight
2
0
0
0
0
Male
0
0.71
0.23
0.26
1.16
3.11
0.002
Female
1
0
0
0
0
Asian
0
1.29
0.44
0.42
2.14
2.92
0.003
Black
1
–0.39
0.26
–0.90
0.12
–1.49
0.13
Hispanic other
2
0.54
0.27
0.004
1.08
1.98
0.05
2.74
0.006
Hispanic white
3
0.58
0.21
0.17
0.99
Multiple ethnicity
4
–0.34
0.69
–1.70
1.01
White
5
<30 y
0
–0.52
0.24
–0.99
30–40 y
1
–0.34
0.15
–0.63
>40 y
2
0.00
0.00
0.00
0.00
0
0
0
–0.5
0.62
0.05
–2.17
0.03
–0.05
–2.26
0.03
0
*Square root of time = year 2009 to 2012.
GEE indicates generalized estimated equation.
by the second model, to assess if these are true factors, whether
genetic, nutritional, or environmental.
The study showed an overall decline of MS over time in the
obese and overweight categories during the 4 years of the study,
which indicates movement away from increased cardiovascular
risk. Certainly, the differences in MS in different ethnicities warrant more research to assess whether there are genetic, cultural,
or environmental factors that are worth studying for future
interventional strategies. Night shift employees—those who do
not work in daytime hours—comprise 20% of the US workforce
and are more predisposed to have MS (3). Hospitals depend on
shift workers. Factors associated with rapid progression toward
getting MS for middle-aged workers include persistent daynight rotating shift work, shift duration, education, length of
employment, age, differences in diet, body mass index, total
cholesterol, triglycerides, job strain, sedentary activity, dietary
style, and smoking (4–12, 15, 16). Educational level may be
a confounding factor in MS as it impacts shift work. Animal
studies indicate that shifts in usual mealtimes which impact the
diurnal rhythms of carbohydrate and lipid metabolism pose
critical implications for MS risk in shift workers (12). Socioeconomic factors such as income have unknown effects on shift
work and MS.
Criteria for MS are used in many wellness programs to
generate information about cardiovascular health for employees. Yet the longitudinal success of wellness programs is rarely
98
followed over time despite substantial monetary investments by
employers. Measuring grouped criteria outcomes and providing
feedback such as provided by this study to employees is vital to
initiating change within an employee base (13–15).
1.
Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular
disease. J Occup Health 2005;47(2):89–95.
2. Mohebbi I, Shateri K, Seyedmohammadzad M. The relationship between
working schedule patterns and the markers of the metabolic syndrome:
comparison of shift workers with day workers. Int J Occup Med Environ
Health 2012;25(4):383–391.
3. Yoon YS, Lee ES, Park C, Lee S, Oh SW. The new definition of metabolic
syndrome by the International Diabetes Federation is less likely to identify
metabolically abnormal but non-obese individuals than the definition by
the revised National Cholesterol Education Program: the Korea NHANES
study. Int J Obes (Lond) 2007;31(3):528–534.
4. Lin YC, Hsiao TJ, Chen PC. Persistent rotating shift-work exposure
accelerates development of metabolic syndrome among middle-aged
female employees: a five-year follow-up. Chronobiol Int 2009;26(4):740–
755.
5. Copertaro A, Bracci M, Barbaresi M, Santarelli L. Role of waist circumference in the diagnosis of metabolic syndrome and assessment
of cardiovascular risk in shift workers [article in Italian]. Med Lav
2008;99(6):444–453.
6. Pietroiusti A, Neri A, Somma G, Coppeta L, Iavicoli I, Bergamaschi A,
Magrini A. Incidence of metabolic syndrome among night-shift healthcare
workers. Occup Environ Med 2010;67(1):54–57.
7. Jermendy G, Nádas J, Hegyi I, Vasas I, Hidvégi T. Assessment of cardiometabolic risk among shift workers in Hungary. Health Qual Life Outcomes
2012;10:18.
Baylor University Medical Center Proceedings
Volume 27, Number 2
8.
Kobayashi T, Suzuki E, Takao S, Doi H. Long working hours and metabolic syndrome among Japanese men: a cross-sectional study. BMC Public
Health 2012;12:395.
9. Biggi N, Consonni D, Galluzzo V, Sogliani M, Costa G. Metabolic
syndrome in permanent night workers. Chronobiol Int 2008;25(2):443–
454.
10. Li Y, Sato Y, Yamaguchi N. Shift work and the risk of metabolic syndrome:
a nested case-control study. Int J Occup Environ Health 2011;17(2):154–
160.
11. Esquirol Y, Bongard V, Mabile L, Jonnier B, Soulat JM, Perret B.
Shift work and metabolic syndrome: respective impacts of job strain,
physical activity, and dietary rhythms. Chronobiol Int 2009;26(3):544–
559.
12. Yoon JA, Han DH, Noh JY, Kim MH, Son GH, Kim K, Kim CJ, Pak YK,
Cho S. Meal time shift disturbs circadian rhythmicity along with metabolic and behavioral alterations in mice. PLoS One 2012;7(8):e44053.
13. Kang DR, Ha Y, Hwang WJ. Prevalence and associated risk factors of the
metabolic syndrome in the Korean workforce. Ind Health 2013;51(3):256–
265.
14. Basei Rossa CE, Avancini Caramori PR, Manfroi WC. Metabolic syndrome in workers in a university hospital [article in Portuguese]. Rev Port
Cardiol 2012;31(10):629–636.
15. Fulgoni VL 3rd, Dreher M, Davenport AJ. Avocado consumption is associated with better diet quality and nutrient intake, and lower metabolic
syndrome risk in US adults: results from the National Health and Nutrition Examination Survey (NHANES) 2001–2008. Nutr J 2013;12:1.
Proceedings’ annual editorial board meeting
B
aylor University Medical Center Proceedings held its
annual editorial board meeting on February 12,
2014. Some of the main points discussed were as
follows:
• In 2013, published 107 manuscripts and 448 pages (Table),
with an acceptance rate of 83% (107/129). The number of
submissions was an all-time high.
• Received 78% of the published manuscripts from Baylor
Health Care System physicians.
• Signed an agreement with CNKI, the largest aggregator and
distributor of academic digital resources in China. We have
agreements with numerous US aggregators as well, including
Ebsco, Gale, and ProQuest.
• Began using Twitter for journal announcements
(@BaylorHealth.edu).
• Printed 7100 copies of each issue.
• Had a budget of about $180,000.
• Received nearly 2 million visits to our PubMed Central
website in 2013, representing about 1.2 million unique
visitors.
April 2014
Table. Numbers of articles and pages published in BUMC
Proceedings in 2013
Jan 13
Apr 13
Jul 13
Oct 13
Content
Art Pp
Art Pp
Art Pp
Art Pp
Case reports
Original articles
Reviews
Editorials, tributes
Interviews
Historical articles
Facts and ideas
Book reviews
18 51
2 7
15
6
3
4
16
6
4
40
27
16
11 29
4 19
2
18
1
2
6
14
3
10
1 6
1 10
2 2
8 18
60 161
18 78
7 38
8 22
2 18
3 10
4 45
5
7
27 69
31 128
21 88
107 448
Miscellaneous∗
Total
2 10
1 11
6 13
23 92
2
1
1
7
41
25
22
8
4
10
2
28
32 140
2
4
Total
Art
Pp
∗Miscellaneous
includes the copyright page, Baylor news, obituaries, journal notices,
abstracts, guidelines for authors, ads, index, and publications list. Not included are
items that appear at the end of articles. The miscellany items are not included in
the total article count.
A cohort analysis of the cardiovascular risk factors in the employees of a pediatric hospital from 2009 to 2012
99
Factors affecting adherence to a quality improvement
checklist on an inpatient hepatology service
Elliot B. Tapper, MD, and Michelle Lai, MD, MPH
Given the increasing emphasis on measuring quality indicators such as
adherence to practice guidelines, we sought to determine the factors
and address the barriers affecting guideline adherence on an academic
inpatient hepatology service. We performed a single-center, prospective observational study. Physicians were given a handheld checklist
to complete daily. We first measured the adherence rate and studied
factors affecting adherence by performing surveys. We then modified
the program to address the factors affecting adherence and reassessed
the adherence rate. There was a baseline 46% checklist adherence rate.
Reasons given for nonadherence fell into two categories: ease of task and
physician commitment from both attending physicians and housestaff.
Specific reasons given were that the attending did not prompt (39%),
the adherence sheet was not in the chart (35%), the individual forgot
(12%), as well as lack of time, unclear protocol, “too difficult,” and “didn’t
pay attention” (4% each). Each of these factors was addressed with a
multimodal approach. Thereafter, the adherence rate rose from 46% to
83% (P < 0.001). Maintaining checklist adherence is time intensive and
requires commitment from the whole medical team.
ay for performance is here to stay, and central to the
evolving reimbursement schema is the measurement
of quality indicators, including adherence to practice
guidelines. In the field of liver disease, low rates of guideline adherence represent a collective call to action. Prophylactic
measures with proven mortality benefits are not being provided:
3% of patients eligible for primary prophylaxis of esophageal
variceal hemorrhage receive optimal therapy, 12% of patients
with cirrhosis receive liver cancer screening, and 30% of patients with a history of spontaneous bacterial peritonitis receive
prophylactic antibiotics (1–3). Using expert consensus, Kanwal
et al proffered a definition of quality care, building a set of “if
. . . then” recommendations to be applied to specific ailments
pertaining to cirrhosis management. For example, “If patients
with cirrhosis present with or develop upper gastrointestinal
bleeding, then they receive at least 1 large-bore intravenous line
at the time of initial evaluation” (4). However, these recommendations require extensive interpretation to be applicable
to daily practice, and measuring adherence to them demands
readily available and complete patient information in a universal
clinical language (5). To study adherence rates to guidelines and
P
100
factors affecting adherence on our inpatient hepatology service,
we examined adherence to a handheld checklist used on daily
rounds (6). Herein, we present our study of the factors affecting
adherence to this daily checklist.
METHODS
This single-center prospective observational quality improvement study took place on the dedicated inpatient hepatology
unit of the Beth Israel Deaconess Medical Center in Boston,
Massachusetts. Medical teams consist of an attending hepatologist, gastroenterology fellow, and two teams of a resident
and intern, all of whom rotate on and off the service in 1- to
4-week blocks. The study tools included a checklist (Figure)
and an adherence sheet. The goal was to review the medication
administration record to ensure that patients were receiving
medications as ordered and to check for medication errors.
Additionally, the team was asked to consider and ensure that
candidates for deep-vein thrombosis prophylaxis and esophageal variceal hemorrhage prophylaxis were receiving appropriate
therapy. Protocols for the treatment of spontaneous bacterial
peritonitis and hepatic encephalopathy were added to the checklist during phase 2. Upon completing the checklist, physicians
were asked to initial an adherence sheet placed in the bedside
chart. A survey was sent by e-mail to all housestaff to determine
factors affecting adherence. The surveys included the questions
“What percentage of the time did you (your team) go through
the checklist on rounds? If it wasn’t done, why?”
This was a two-phase study. During phase 1, which lasted
17 weeks, we implemented the checklist and adherence sheet
and conducted surveys. The checklist components were based
on faculty consensus achieved prior to the project rollout. The
housestaff were informed and educated about the program before their rotation began. The adherence sheets were collected
in the medical records department on discharge or transfer and
From the Division of Gastroenterology (Tapper, Lai) and Department of Medicine
(Tapper), Beth Israel Deaconess Medical Center, Boston, Massachusetts.
Corresponding author: Elliot B. Tapper, MD, Department of Medicine, Beth Israel
Deaconess Medical Center, 330 Brookline Avenue, Boston, MA 02215 (e-mail:
etapper@bidmc.harvard.edu).
Proc (Bayl Univ Med Cent) 2014;27(2):100–102
Medication list review
Is patient receiving medications as ordered
Deep vein thrombosis prophylaxis—subcutaneous heparin or pneumatic boots
if contraindicated (elevated INR unrelated to Coumadin is not a contraindication)
Beta-blocker for known varices or documented contraindications to
beta-blockers
Spontaneous bacterial peritonitis (SBP)
Prophylaxis with either Cipro 500 mg once a day or Bactrim DS once a day for
one of the following:
1. Previous episode of SBP
2. Ascitic fluid protein <1.5 g/dL and one of the following is present:
—serum creatinine >1.2 mg/dL
—blood urea nitrogen >25 mg/dL
—serum sodium <130 mEq/L
—Child-Pugh >9 points with bilirubin >3 mg/dL
Prophylaxis, gastrointestinal bleeding: 7 days of Ceftriaxone 1 g once a day,
Bactrim DS twice a day, or Cipro 500 mg twice a day
Treatment
Antibiotics (Ceftriaxone 1 g twice a day or 2 g once a day, unless allergic)
(Consider vancomycin if hospital acquired)
Albumin (1.5 g/kg on day 1 and 1 g/kg on day 3)
Hepatic encephalopathy
Patient carries a diagnosis: ensure lactulose and rifaximin ordered and received
Acute hepatic encephalopathy:
If low grade (stage 1 or 2)—lactulose 30–45 mL every 2 h orally or by nasogastric tube
If no improvement in 6 hours, convert to lactulose enemas every 2 h
If high grade (stage 3 and 4)—lactulose enemas every 2 h
If improvement in 6 hours, convert to every 2 h lactulose orally or by
nasogastric tube
Figure. The daily rounding checklist.
sent to the study coordinator’s office. These sheets were then
audited to determine the adherence rate (the number of completed adherence sheets divided by the total number of adherence sheets reviewed). The housestaff were surveyed on the day
after the end of their rotations.
Phase 2 was designed to evaluate whether modifying the
factors affecting adherence, discovered from the survey conducted during phase 1, would affect the adherence rate. Phase
2 lasted 5 weeks.
All data were entered into a password-protected Microsoft
Excel database. Data were analyzed using JMP SAS 8 (SAS
Institute Inc, Cary, NC). Statistical analysis included Fisher’s
exact test with a two-tailed P value.
RESULTS
During the 22-week study period, 232 patients were cared
for on the hepatology service, 190 patients in phase 1 and 42 patients in phase 2. Of the 232 patients, 59% were men, and their
mean age was 56 years. They had an average admission Model
for End-Stage Liver Disease score of 17 ± 8, an average length
of stay of 6 ± 7 days, and a 42% 30-day readmission rate.
During phase 1, adherence sheets were completed for 87
of the 190 patients. Accordingly, the overall checklist adherence rate during phase 1 was 46%. Twenty-three of 25 unique
residents who rotated during this phase (two graduated from
residency) responded to the written survey. The principal reasons
for nonadherence were that the attending did not prompt use
of the checklist (39%), the checklist adherence sheet was not
available (35%), and the housestaff forgot to do the checklist
(12%). Other reasons given included lack of time, unclear protocol, “too difficult,” and “didn’t pay attention.”
Based on the feedback, several steps were taken prior to
phase 2 (Table). First, adherence sheets were moved from the
chart used for the permanent record to the bedside chart (used
for the medication administration record). This allowed more
convenient medication reconciliation during bedside rounds.
Second, nurses were recruited to ensure that sheets were in the
chart. Third, the division chief reminded all hepatologists that
checklist completion was mandatory. The phrase “mandatory
checklist” was used during all correspondence. Fourth, the color
of the adherence sheet was changed from white to yellow to
make it more conspicuous. Fifth, data on patient outcome,
length of stay, and readmission rates were presented to housestaff, nurses, and attending physicians.
During phase 2, 42 patients were seen on the inpatient
hepatology, and adherence sheets were completed for 35 out of
the 42 patients. The difference in adherence rates between phase
1 (46%) and phase 2 (83%) was significant, P < 0.001.
DISCUSSION
Two major categories of factors affected guideline adherence: ease of task and physician commitment. Addressing these
factors significantly increased the adherence rate from 46%
to 83%. Workflow was critical to adherence. If the adherence
sheet was not available at the bedside during bedside rounds,
the chance that one would interrupt rounds to find it was low.
Table. Approaches to and solutions for barriers to adherence
Barrier to adherence
Approach
Galvanize institutional support
Physician commitment
• Attending did not prompt
checklist
• Low housestaff enthusiasm
Invigorate support from superiors, foster coownership Presentations on patient outcomes; reminder e-mails; strengthening
of attending involvement
Ease of task
• Adherence sheets hard to find
• Adherence sheets not in chart
April 2014
Solution
Reminders from division chief; reminder e-mails about “mandatory”
checklist
Streamline workflow
Change of sheet location and color
Recruit support for the project from all team members Recruitment of nurses to help keep sheet in chart; presentations to
nurses on patient outcomes
Factors affecting adherence to a quality improvement checklist on an inpatient hepatology service
101
Commitment from the entire team was also key, beginning
with the attending physician. If an attending physician did
not prompt the checklist and the housestaff did not bring it
up, it did not get done. Twenty percent of housestaff provided
reasons for nonadherence that implied a lack of enthusiasm (i.e.,
forgot, did not pay attention, and too difficult). Accordingly,
it is important to educate the members of the team about the
importance of the quality improvement measure for improvement of patient care and patient outcomes. Quality improvement efforts must reach each team member. Our approach was
to foster coownership of healthcare quality by routinely sharing
patient outcomes potentially tied to the checklist with interns,
residents, nurses, floor clerks, and attending physicians.
Guidelines are useful only when they are followed. Applying
guidelines to daily practice can be difficult and resource intense.
In their systematic review, “Why Don’t Physicians Follow Clinical Practice Guidelines,” Cabana et al described three types of
barriers to guideline adherence: deficits in knowledge, attitude,
and behavior (7). Knowledge barriers are addressed by spreading
awareness and familiarity. We addressed this barrier through
e-mails, faculty meetings, presentations at conferences, and oneon-one meetings with the housestaff, which was a time- and
labor-intensive process. Attitude barriers include philosophical disagreements with the guidelines themselves or a culture
against guidelines in general, a lack of confidence in the ability of guidelines to achieve goals, and a lack of motivation or
inertia due to previous practices. We improved attitudes in a
few ways. First, prior to launching the initiative, we achieved
consensus with the hepatology faculty. Second, housestaff were
involved throughout the process and were regularly approached
for feedback and ideas to address any concerns or disagreement.
Behavioral barriers include time, resources, and functionality of
the guideline. Changing the location and color of the adherence
sheet saved time for the team.
102
There are limitations to this study. First, while this study
took place over several months, the period is still short enough
that the rate of adherence could simply reflect the variable personalities and diligence of the housestaff involved. Second, as we
responded to problems with several simultaneous interventions,
it is impossible to disentangle the effect of each intervention.
Third, the potential impact of prophylactic measures started in
the hospital may be lower in resource-poor settings where patients are unable to afford such prescriptions. Fourth, this project presupposes the value of guideline-based checklists, which is
debatable. We believe, however, that the insights gleaned about
the pitfalls of quality improvement with housestaff should prove
generalizable, especially in the era of pay for performance and
the Affordable Care Act.
1.
2.
3.
4.
5.
6.
7.
Maddur H, Naik S, Siddiqui AA, Rockey DC. Adherence and
adequacy of therapy for esophageal varices prophylaxis. Dig Dis Sci
2011;56(11):3129–3136.
Davila JA, Henderson L, Kramer JR, Kanwal F, Richardson PA, Duan
Z, El-Serag HB. Utilization of surveillance for hepatocellular carcinoma
among hepatitis C virus-infected veterans in the United States. Ann Intern
Med 2011;154(2):85–93.
Kanwal F, Kramer JR, Buchanan P, Asch SM, Assioun Y, Bacon BR,
Li J, El-Serag HB. The quality of care provided to patients with
cirrhosis and ascites in the Department of Veterans Affairs. Gastroenterology
2012;143(1):70–77.
Kanwal F, Kramer J, Asch SM, El-Serag H, Spiegel BM, Edmundowicz S,
Sanyal AJ, Dominitz JA, McQuaid KR, Martin P, Keeffe EB, Friedman
LS, Ho SB, Durazo F, Bacon BR. An explicit quality indicator set for
measurement of quality of care in patients with cirrhosis. Clin Gastroenterol
Hepatol 2010;8(8):709–717.
Bassett JT, Volk ML. Can quality of care for patients with cirrhosis be
measured? Dig Dis Sci 2011;56(12):3488–3491.
Lai M, Afdhal NH. Health care quality measurement in the care of patients
with cirrhosis. Clin Gastroenterol Hepatol 2010;8(8):649–650.
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA,
Rubin HR. Why don’t physicians follow clinical practice guidelines? A
framework for improvement. JAMA 1999;282(15):1458–1465.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Characteristics of Native Americans with HIV
and implications for care
Christina Connel, PharmD, BCPS, Jeffrey S. Stroup, PharmD, BCPS, Johnny R. Stephens, PharmD,
and Erica Martin, PharmD, BCPS
Limited data have been published about HIV infections and response to
antiretroviral therapy in the Native American population. We reviewed
baseline characteristics of 112 Native American patients to determine if
there were any shared characteristics that would dictate the best treatment for this population. Metabolic diseases and psychiatric disorders
were common findings among our patients. Native American patients
should be monitored and screened as appropriate for comorbid conditions, and these disease states should be considered when choosing an
antiretroviral regimen.
IV rates vary across ethnic groups in the United States.
Data from 2009 estimated that approximately 3000
Native Americans were living with an HIV diagnosis
in the United States (1). While Native Americans represent <1% of persons living with HIV, the rates of diagnosis
increased in this population from 2007 to 2010 (1). In 2010,
the estimated rates of HIV per 100,000 population of Native Americans was 9.7, which is higher than that for Asian or
Caucasian populations, although lower than that for African
American or Hispanic populations (1). HIV has not been well
studied in the Native American population, leading to limited
data for treatment specific to this group. The present study assessed the baseline characteristics and treatment of patients with
HIV and Native American heritage. Our goal was to determine
if there were any common variables among this population that
would dictate the best treatment options for them. This study
was conducted at a Ryan White clinic that cares for approximately 1100 HIV-positive patients.
H
METHODS
This retrospective study evaluated the baseline characteristics of HIV-positive Native American patients >17 years
of age at their initial visit to the Oklahoma State University Internal Medicine Specialty Clinic. Native American
heritage was defined as either patient-reported ethnicity or
a record of medical care through Indian Health Services.
Data collected included patients’ age at transmission, gender, HIV genotype, baseline CD4 count and viral load,
renal function, home medications (including antiretroviral therapy regimen), comorbid conditions, and mode of
Proc (Bayl Univ Med Cent) 2014;27(2):103–105
transmission of HIV. Use of the clinic electronic medical
record identified 149 patient charts meeting inclusion criteria for the study. Upon review, 21 patients had incomplete
initial documentation, and 16 did not have documentation
of Native American heritage. These charts were excluded,
and 112 charts were reviewed for baseline characteristic data.
Descriptive statistics of the patient population were used to
analyze the data gathered.
RESULTS
Patients’ baseline characteristics at the first visit are shown
in Table 1. Viral loads and CD4 counts of patients already controlled on antiretroviral therapy are not reported. Twenty-seven
patients (24%) entered care with a diagnosis of AIDS based on a
CD4 cell count <200/μL at the time of entry; however, previous
AIDS-defining illnesses were not assessed in this study. Most
patients (83%) were men, and the average age of diagnosis was
33 years. Ages of transmission ranged from birth to 65 years.
One patient had vertical transmission and the other 111 patients
received a diagnosis of HIV at the age of 18 or older. As shown
in the Figure, the most frequent mode of transmission was men
having sex with men, followed by heterosexual intercourse. Two
patients reported intravenous drug use in addition to sexual
activity as a possible mode for acquisition of HIV. Those reporting heterosexual intercourse as the form of transmission were
more likely to be female.
Thirty-five patients (31%) entered the clinic already on
antiretroviral therapy; 20 of them had an undetectable viral
load at entry into care. Eleven patients were continued on
regimens despite evidence of undetectable viral loads, two
did not have viral load recorded, and four had a viral load
<500 copies/mL.
Baseline HIV genotypes were collected when available.
Unfortunately, only nine patients (8%) had resistance
From the Department of Pharmacy Services (Connel, Martin) and the Department
of Medicine (Stroup, Stephens), Oklahoma State University Medical Center, Tulsa,
Oklahoma.
Corresponding author: Jeffrey S. Stroup, PharmD, Chief Pharmacy Officer,
Oklahoma State University Medical Center, Associate Professor of Medicine,
Oklahoma State University Center for Health Sciences, 717 S. Houston Avenue,
3rd Floor, Tulsa, OK 74127 (e-mail: Jeffrey.Stroup@okstate.edu).
103
Table 1. Baseline demographics in 112 Native American
HIV-positive patients
Variable
Table 2. Comorbid conditions in 112 Native American
HIV-positive patients
Mean (range)
Comorbid condition
n (%)
Age at diagnosis (years)
33 (0–65)
Psychiatric disorder
34 (30%)
Men
93 (83%)
Viral load (copies/mL)
CD4 (cells/μL)
Serum creatinine (mg/dL)
137,807 (43–750,000)
374 (2–1142)
0.95 (0.61–1.51)
Height (cm)
175 (150–198)
Weight (kg)
80 (45–182)
Depression
24 (71%)
Anxiety
18 (53%)
Bipolar disorder
2 (6%)
Schizophrenia
1 (3%)
Attention deficit hyperactive disorder
17 (15%)
Dyslipidemia
17 (15%)
Diabetes mellitus
profiles at baseline. Six patients, all of whom were treatment naive, were sensitive to all antiretroviral agents, while
three were resistant to at least one agent. Of the three, one
was treatment naive with conferred resistance to lamivudine.
The other two patients reported having previously been
on therapy, and genotyping showed resistance to nelfinavir
and nucleoside/nucleotide reverse transcriptase inhibitors
(NRTIs), respectively.
The most common comorbid conditions were psychiatric disorders (depression and anxiety being the most
common), hypertension, dyslipidemia, diabetes mellitus,
alcohol abuse, tobacco abuse, and hepatitis (Table 2). Based
on home medication lists, these conditions were being
treated 33% to 50% of the time. Twenty-seven patients
entered our clinic with a CD4 count <200/μL, and nine
of these patients had lower CD4 counts of <50/μL. Prophylaxis for pneumocystis pneumonia and mycobacterium
avium complex was continued or initiated in 70% and
56%, respectively.
1 (3%)
Hypertension
8 (7%)
Alcohol abuse
11 (10%)
Tobacco abuse
29 (26%)
Hepatitis B
4 (4%)
Hepatitis C
9 (8%)
DISCUSSION
Disease states found in our HIV-positive Native
American patients refl ect those reported in national data
for Native American patients. However, there was a lower
prevalence of hypertension, diabetes mellitus, and cardiac
disease than would be anticipated. This could be due to the
overall younger age of the study patient population. Data
including all ethnicities has shown a higher frequency of the
metabolic syndrome among patients between 45 and 64 than
in younger populations (2). Nevertheless, due to the known
increased risk in the Native American population for metabolic disease, patients should be closely monitored for this
disease state and screened as
appropriate. Serum glucose
levels should be monitored
80
with the initiation/change
of antiretroviral therapy and
70
every 6 months thereafter;
60
monitoring should be more
frequent if abnormalities
50
are found (3). The NRTIs
didanosine, stavudine, and
40
Male
zidovudine as well as some
Female
protease inhibitors, particu30
larly those that are ritonavir
20
boosted, have been found to
increase the risk of diabetes
10
mellitus and insulin resistance (3–5). Non-nucleoside
0
reverse transcriptase inhibiMSM
Heterosexual
IVDU
Not
Other
tors (NNRTI) and integrase
Documented
inhibitors do not appear to
Figure. Modes of transmission among 112 Native American HIV-positive patients. MSM indicates men having sex with alter insulin resistance and
men; IVDU, intravenous drug use.
104
Baylor University Medical Center Proceedings
Volume 27, Number 2
would be better choices in a patient with diabetes or a patient
at risk for diabetes.
Adult HIV guidelines list NRTIs (stavudine, zidovudine,
abacavir), the NNRTI efavirenz, and all ritonavir-boosted protease inhibitors as having the risk of increasing lipid levels (3).
A baseline fasting lipid profile should be drawn prior to therapy
initiation, and the risk of dyslipidemia should be assessed. Lipid
levels should be monitored annually, and it is not unreasonable
to check a fasting lipid profile 4 to 8 weeks after starting a new
regimen (3). Due to the risk of cardiovascular disease in Native
Americans, it may be prudent to avoid the above regimens if
possible; however, HIV should be treated despite the risk of
vascular disease (5).
When choosing a regimen for a Native American HIVpositive patient, it is important to assess possible adverse effects as
they will affect or precipitate comorbid conditions (6). Currently,
three of the four preferred regimens supported by adult HIV
treatment guidelines contain a component that could precipitate
diabetes mellitus, dyslipidemia, or psychiatric comorbid issues.
The preferred integrase inhibitor regimen and the alternative
non-efavirenz-containing NNRTI regimens appear to be favorable regimens to use in patients at risk for these conditions. The
risk of precipitating a comorbid adverse event should not deter
treatment of HIV. Monitoring should be done in accordance
with current guidelines to reduce and prevent medication complications. Newer therapies on the market, such as elvitegravir/
cobicistat or dolutegravir, may also have a role in these patients.
Centers for Disease Control and Prevention. HIV Surveillance Report 2010.
Atlanta, GA: CDC, March 2012. Available at http://www.cdc.gov/hiv/
topics/surveillance/resources/reports/.
2. Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics
for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat
2012;10(252):1–207.
3. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and
Adolescents. Rockville, MD: US Department of Health and Human
Services. Available at http://www.aidsinfo.nih.gov/contentfiles/
lvguidelines/adultandadolescentgl.pdf.
4. Bozzette SA, Ake CF, Tam HK, Chang SW, Louis TA. Cardiovascular and
cerebrovascular events in patients treated for human immunodeficiency
virus infection. N Engl J Med 2003;348(8):702–710.
5. Brown TT, Cole SR, Li X, Kingsley LA, Palella FJ, Riddler SA, Visscher
BR, Margolick JB, Dobs AS. Antiretroviral therapy and the prevalence
and incidence of diabetes mellitus in the multicenter AIDS cohort study.
Arch Intern Med 2005;165(10):1179–1184.
6. De Wit S, Sabin CA, Weber R, Worm SW, Reiss P, Cazanave C, El-Sadr
W, Monforte Ad, Fontas E, Law MG, Friis-Møller N, Phillips A; Data
Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. Incidence and risk factors for new-onset diabetes in HIV-infected patients: the
Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study.
Diabetes Care 2008;31(6):1224–1229.
1.
Avocations
Photo copyright © Jed Rosenthal, MD. Dr. Rosenthal is a cardiologist in Dallas, Texas (e-mail: jedr2@sbcglobal.net).
April 2014
Characteristics of Native Americans with HIV and implications for care
105
Comparison of the frequency and level of serum total
cholesterol >300 mg/dL in patients at the same Texas
hospital in a single month in 1993 and in 2013
William C. Roberts, MD, Jong Mi Ko, BA, and Raul Benavides Jr., MD
The clinical pathology laboratory database of a large tertiary hospital
in Dallas, Texas, was searched for patients having a serum total
cholesterol >300 mg in a single month in 1993 and in 2013.
In September 1993, 63 patients had a serum total cholesterol
>300 mg/dL (range 302–1515 [mean 431, median 349]), and in
September 2013, 12 patients had serum total cholesterol levels
>300 mg/dL (range 303–442 [mean 334, median 316.5]), an 81%
decline in the numbers of patients and a 23% decline in the average
total cholesterol levels during the 20-year period.
number of patients whose serum total cholesterol was >300
mg/dL studied at the same hospital in September 2013 was
12 (an 81% reduction in the number of patients with these
levels); the levels ranged from 303 to 442 (mean 334, median
316.5) (a 23% reduction in the mean total cholesterol level);
the serum total cholesterol levels in the 9 women ranged
from 303 to 442 (mean 336), and in the 3 men from 306
to 363 (mean 327). The numbers of patients with serum
total cholesterol levels in May, June, and July 2013 were 9,
5, and 14, respectively.
METHODS
The database in the Division of Clinical Pathology was
searched for the number of patients with serum total cholesterol levels >300 mg/dL in September 1993 and in September 2013. The ranges, means, and medians in the patients
with serum total cholesterol levels >300 mg/dL also were
acquired. In patients with >1 serum total cholesterol level,
the highest level was included in this analysis. Because the
number of patients in September 2013 was small, namely
12, we also examined three other months in 2013 (May,
June, and July).
DISCUSSION
The present study comparing numbers of patients
hospitalized at a single Texas hospital in September 1993
and in September 2013 with serum total cholesterol levels
>300 mg/dL disclosed that the numbers of such patients
had fallen 81% and that the average serum total cholesterol
level had fallen 23% during the 20-year period. The various
reasons for these falls are unclear, but the increased use of
statin drugs during the 20-year interval almost certainly
played a role (1).
The unique feature of the present study is the absence
of such a study previously at the same hospital over a long
interval. The number of licensed beds at BUMC in September 1993 was 1450, and in September 2013, 1000, a
32% reduction, but the average monthly admissions in 1993
was 2820 and in 2013, 2983, an average monthly increase
of 5%. Thus, despite an increase in monthly admissions
between September 1993 and September 2013, the number
of patients with serum total cholesterol levels >300 mg/dL
was much less (81% less).
The limitations of the present study include 1) lack of
information on the illnesses of the patients studied during the
RESULTS
The findings are summarized in the Figure. A total of 63
patients studied in September 1993 at BUMC had serum
total cholesterol levels >300 mg/dL; the levels ranged from
302 to 1515 (mean 431, median 349); the total cholesterol
levels in the 40 women ranged from 302 to 1348 (mean
416) and in the 23 men from 302 to 1515 (mean 456). The
From the Departments of Pathology and Internal Medicine, Division of Cardiology,
and the Baylor Heart and Vascular Institute, Baylor University Medical Center,
Dallas, Texas.
Corresponding author: William C. Roberts, MD, Baylor Heart and Vascular
Institute, 621 North Hall Street, Dallas, TX 75226 (e-mail: wc.roberts@
BaylorHealth.edu).
erum cholesterol levels have fallen in the USA in
recent decades (1). We determined the number of
patients hospitalized at Baylor University Medical
Center at Dallas (BUMC) with serum total cholesterol levels >300 mg/dL in September 1993 and in September 2013. We then compared the mean and median serum
total cholesterol levels in each of the 2 months 20 years
apart. Such a comparison to our knowledge has not been
performed previously.
S
106
Proc (Bayl Univ Med Cent) 2014;27(2):106–107
Number of hospitalized paents with serum total cholesterol >300 mg/dL
70
302-1515
(mean 431)
[median 349]
60
50
Men
37%
Women
40
30
63%
303-363
(mean 320)
[median 312]
20
302-474
(mean 343)
[median 318]
10
303-542
(mean 373)
[median 346]
303-442
(mean 334)
[median 316.5]
0
September 1993
May 2013
June 2013
July 2013
September 2013
Dates Test Done
Figure. The number of hospitalized patients at Baylor University Medical Center at Dallas who had serum total
cholesterol values >300 mg/dL in one month in 1993 and in each of four months in 2013.
April 2014
2 study months; 2) lack of information on the use of lipid-altering drugs
by the patients during the 2 study
months; 3) lack of information on follow-up lipid levels and outcomes in the
study patients; 4) lack of information
on the serum low-density lipoprotein
cholesterol, high-density lipoprotein
cholesterol, and triglyceride levels in
the study patients; and 5) lack of data
on the total number of patients having
lipid values determined during the 2
study months. Nevertheless, as several
population studies have shown (1),
the number of patients with serum
total cholesterol levels >300 mg/dL at
this single tertiary Texas hospital fell
dramatically in the 2 study months
20 years apart, and the average serum
total cholesterol levels in the 2 study
months also fell.
1.
Carroll MD, Kit BK, Lacher DA, Shero ST,
Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988–2010. JAMA
2012;308(15):1545–1554.
Comparison of the frequency and level of serum total cholesterol >300 mg/dL
107
Opsoclonus myoclonus syndrome: an unusual presentation
for West Nile virus encephalitis
Aasim Afzal, MD, Sahar Ashraf, MD, and Sadat Shamim, MD
A record number of West Nile virus (WNV) cases and fatalities seen in
2012 have brought to light the numerous manifestations of neuroinvasive
disease. We report a case of opsoclonus myoclonus syndrome attributed to
WNV and its clinical course after treatment with a combination of steroids
and intravenous immunoglobulin. Our objective is to highlight opsoclonus
myoclonus syndrome as a potential manifestation of WNV encephalitis.
est Nile virus (WNV) is a mosquito-borne
arbovirus belonging to the genus Flavivirus. It is
more common in temperate and tropical regions
of the world. Before the 1990s, it was not considered a big threat to the human population. However, WNV
has now spread all over the world. The first case of WNV in
the United States was reported in New York City in 1999;
over the next 5 years, it spread across the nation (1). The main
mode of transmission is mosquitoes, which are the prime vector, whereas birds are the prime reservoir host. WNV is also
found in ticks, but they are not important vectors. WNV can
also be spread by blood transfusion, organ transplantation, and
breastfeeding (2). WNV infects various mammals, reptilian
species, as well as amphibians (3).
W
CASE PRESENTATION
A 43-year-old Caucasian woman presented to an outside
facility in the fall of 2012 with a 10-day history of dizziness,
worsening headaches, nausea, fever, and myalgias. Early in the
course, she developed a raised nonerythematous rash on her
neck that spread in a craniocaudal fashion. One week after
developing the rash, she started having involuntary multidirectional jerky saccadic eye movements with superimposed fluttering eyelid movements consistent with opsoclonus myoclonus
syndrome (OMS).
The patient’s past medical history was insignificant except
for a cesarean section. She mentioned a family history of
recurrent meningitis in her son, breast cancer in her mother,
and prostate cancer in her father. Her social history was
significant only for exposure to WNV, as she was a rancher
in a neighborhood where others had been diagnosed with
WNV. Her medications included occasional nonsteroidal
antiinflammatory drugs and oral contraceptives.
108
At the time of admission, she appeared very uncomfortable
and kept her eyes closed with myoclonic jerking of the eyelids
whenever she tried to open them. Her vital signs revealed only
low-grade fever, which resolved spontaneously. She had difficulty
keeping her eyes open, and her eyes initially had to be pried
open to examine her severe OMS. She had good muscle strength
but her gait was ataxic. Opening her eyes or any movement
triggered severe nausea and episodes of emesis. She stayed in bed
in a dark room with her eyes clenched shut with a constant look
of distress. However, her cognition remained unaffected.
A thorough evaluation was done for the possibility of
malignancies, paraneoplastic syndromes, autoimmune processes,
and infectious etiologies as the cause of OMS. Her cerebrospinal
fluid (CSF) was xanthochromic with lymphocytic pleocytosis
(Table 1). Among the imaging studies performed at the outside
facility, magnetic resonance (MR) imaging with contrast and
MR angiography of the brain were nonrevealing. Computed
tomography with contrast of the chest, abdomen, and pelvis
Table 1. Results of laboratory tests of the patient’s
cerebrospinal fluid
Test
Result
Color
Xanthochromic 49K RBC
Lymphocyte (per μL)
30
Neutrophil (per μL)
62
Glucose (mg/dL)
47
Protein (mg/dL)
110
Culture
No organisms
Fungal culture
Negative
Paraneoplastic panel
Negative
HSV/HHV6/Coxsackie A-B/GQ1b Ab/VGCC/WNV IgM
Negative
HSV indicates herpes simplex virus; HHV6, human herpesvirus 6; Ab, antibody; VGCC,
voltage-gated calcium channel; WNV, West Nile virus.
From the Division of Neurology, Department of Internal Medicine, Baylor University
Medical Center at Dallas.
Corresponding author: Sadat Shamim, MD, 3600 Gaston Avenue, Suite 1155,
Dallas, TX 75246 (e-mail: SadatSha@BaylorHealth.edu).
Proc (Bayl Univ Med Cent) 2014;27(2):108–110
Table 2. Results of other laboratory tests
Blood test
Results
Antimitochondrial antibody
Absent
Antinuclear antibodies
Absent
Coccidioides/Rocky Mountain spotted fever antibody
Negative
C-reactive protein
<0. 3
Creatine kinase
24
Blood culture
Negative
Paraneoplastic panel
Negative
Enterovirus/herpes simplex virus
Negative
West Nile virus IgM
Positive
showed small bilateral pleural effusions and a small amount of
free fluid in the pelvis but no signs of primary malignancy. Laboratory test results were remarkable for the presence of WNV
immunoglobulin (Ig) M in the blood, with negative IgG and
negative polymerase chain reaction results (Table 2). Although
CSF WNV IgM titers were below the assay cutoff, they were
in fact found to be present at low levels. CSF WNV IgM was
tested after completion of intravenous immunoglobulin (IVIG)
treatment and while on high-dose steroids. Based on the clinical presentation and these laboratory findings, the diagnosis of
acute WNV meningoencephalitis was made. CSF and blood
cultures drawn prior to antibiotics were without any growths.
Prior to transfer to Baylor University Medical Center, the
patient was started on broad-spectrum antibiotics and antiviral coverage with doxycycline, meropenem, vancomycin, and
acyclovir but showed no signs of improvement. She was also
started on gabapentin and diazepam for nystagmus symptom
relief. Nausea and emesis were controlled with promethazine
and ondansetron. Upon transfer, the patient was immediately
started on IVIG with a total of 2 g/kg administered over 3 days.
On day 2 of IVIG, she was started on intravenous methylprednisolone 125 mg twice a day, which was later transitioned to
oral prednisone after 5 days. Within a couple of days of starting
IVIG and intravenous steroids, her symptoms of nystagmus and
ataxia showed visible improvement. On day 5, her symptoms
of headache, nausea, vomiting, and nystagmus had improved
significantly such that she was finally able to open her eyes and
eat. On day 6, oral prednisone, memantine, and oxcarbazepine
were started. Due to drowsiness, memantine and oxcarbazepine
were discontinued fairly quickly after initiation. By day 10, the
patient had full range of motion in all extremities, and OMS
had nearly resolved to the untrained eye.
The patient had become very deconditioned from being
bedbound for nearly 2 weeks with poor nourishment, requiring inpatient rehabilitation. Over the course of a year, she has
improved to the extent of being able to get groceries and take
care of her children. Using her eyes for prolonged tasks will still
cause her to be nauseated and worsen her headache. Although
her opsoclonic-nystagmoid movements are not visible outside of
ophthalmological evaluations, which do show small continued
April 2014
movement not obvious to the naked eye, she does have difficulty with reading. She also has intermittent problems with
urinary retention.
DISCUSSION
West Nile virus
According to the Centers for Disease Control and Prevention, in 2012, there were 5674 WNV cases in the United States
(4). Texas was particularly hit hard, with 1739 (32%) cases
reported (3). Severe cases of neuroinvasive WNV were initially
reported in 2002 and 2003 but have been increasing in frequency over the past several years. Just in 2012 alone, 2873 of
the reported WNV cases were neuroinvasive, with 286 reported
fatalities (4). The risk factors that contribute to the more severe
form of disease are HIV infection, chemotherapy, organ transplant, immunosuppression, young or old age, and pregnancy.
WNV infection usually presents with fever and nonspecific
symptoms such as abdominal pain, nausea, emesis, and diarrhea.
Rash is also often described. These symptoms can last anywhere
from 3 to 6 days to about a month. WNV can cause inflammation in a wide variety of organs in the body with variable
manifestations. Notable complications of WNV are fulminant
hepatitis, pancreatitis, myocarditis, rhabdomyolysis, chorioretinitis, orchitis, nephritis, optic neuritis, cardiac arrhythmias,
and hemorrhagic fever with coagulopathy (5–7). The more severe neuroinvasive form of disease manifests as meningitis or
encephalitis. Seizures are also often seen. Patients can present
with confusion, loss of consciousness, coma, stiff neck, permanent brain damage, and muscle weakness that resembles polio
and on rare occasions with OMS. Neurological complications
are often fatal. Previous reports have suggested that 1 out of 10
patients presenting with encephalitis due to WNV do not survive (2). Therefore, it is prudent to evaluate for WNV exposure
in patients presenting with neurological symptoms in endemic
areas during late summer.
Opsoclonus myoclonus syndrome
OMS is an unusual presentation of WNV infection. Only
two cases of OMS were reported in the 2003 outbreak of WNV,
with another similar case reported in 2006 (8). One of the cases
reported occurred in a patient who was potentially immunocompromised with non–small cell lung cancer, which makes it
difficult to attribute OMS solely to WNV infection (9).
OMS is a rare autoimmune condition characterized by
cerebellar degeneration and is seen in patients with encephalitis
secondary to various etiologies such as cancers, toxins, autoimmune diseases, and viral infections (10). It occurs most often as
a paraneoplastic syndrome when a cancer remote to the brain
induces cerebellar dysfunction that is unrelated to metastasis. Half
of the cases occur in children with neuroblastoma. In some cases,
OMS has been successfully treated with immunotherapy, as the
presence of widespread CNS lymphocytic infiltrates in autopsy
studies indicates that an autoimmune pathogenesis is likely (11).
In some cases of OMS, symptoms are believed to develop after
intracellular and surface binding (IgG3) antibodies in serum and
CSF specifically bind to and damage inhibitory Purkinje cells and
Opsoclonus myoclonus syndrome: an unusual presentation for West Nile virus encephalitis
109
granular neurons in the dorsal vermis of the cerebellum. Because
the antibodies can vary widely and sometimes are not found at
all, the exact mechanism is not entirely clear (10).
OMS has horizontal and vertical saccades. Horizontal saccades are generated by burst neurons in the paramedian pons,
and vertical saccades are caused by burst neurons in the rostral
midbrain. The activity of these burst neurons is controlled by
omnipause neurons in the pontine raphe. It is suggested that
OMS is caused by the failure of omnipause neurons to control burst neurons (8). The omnipause neurons are affected in
brainstem encephalitis and also when there is impaired control
of the brainstem saccade generating network by the cerebellum.
Patients with OMS should undergo a complete evaluation for
cancer and infection. Abnormal immunoglobulin analysis and
other laboratory findings may be nonspecific, since there are
no diagnostic biomarkers for paraneoplastic OMS. Blood or
CSF analysis may assist in identifying an infectious etiology.
While they neither diagnose nor exclude a paraneoplastic or
autoimmune etiology, CSF studies often document paraneoplastic antibodies, mild increases in proteins, and a lymphocytic
pleocytosis consistent with inflammatory changes (10).
The exact role of IVIG and high-dose steroids in the treatment of WNV has not been studied. However, improvements
have been reported in several instances for severe cases of human enteroviral encephalitis. Sequelae such as hearing loss of
infectious aseptic meningitides in general have been shown to
be reduced in children with steroid treatment. IVIG products
prepared in areas where WNV is endemic such as Texas have
been shown to have high titer levels to WNV. The timing and
route of administration of IVIG also appears to be important
(9). In the case presented, IVIG was administered 5 days after
onset of OMS (12 days after the rash and fever), along with
high-dose intravenous steroids and antivirals with initial rapid
improvement followed by very slow improvement and plateauing. It is impossible to determine the exact role of acute use of
IVIG and steroids in the recovery of our patient.
110
In general, neuroinvasive WNV infections can have
numerous presentations. Patients who present with OMS
with signs of an infective process should be checked for WNV
infection especially if they live in endemic areas. Patients
surviving WNV neuroinvasive disease often suffer long-term
neurological sequelae (4), and it is unclear if therapies offered
for other aseptic meningitides would apply. As is the case with
meningitis in general, it may be reasonable to consider steroids
or other immunomodulatory therapies to limit neuronal injury
in WNV neuroinvasive disease as well.
1.
Asnis DS, Conetta R, Teixeira AA, Waldman G, Sampson BA. The West
Nile virus outbreak of 1999 in New York: the Flushing Hospital experience.
Clin Infect Dis 2000;30(3):413–418.
2. Beckhan J, Tyler K. Encephalitis. In Mandell GL, Bennett JE, Dolin R,
eds. Principles and Practice of Infectious Diseases (7th ed. ). Philadelphia:
Elsevier Churchill Livingstone, 2009: 1243–1264.
3. Steinman A, Banet-Noach C, Tal S, Levi O, Simanov L, Perk S, Malkinson
M, Shpigel N. West Nile virus infection in crocodiles. Emerg Infect Dis
2003;9(7):887–889.
4. Murray KO, Mertens E, Despres P. West Nile virus and its emergence in
the United States of America. Vet Res 2010;41(6):67.
5. Bleck T. Arthropod-borne viruses affecting the central nervous system.
In Goldman L, Schafer AI, eds. Goldman’s Cecil Medicine (24th ed.).
Philadelphia: Saunders Elsevier, 2011: chapter 391.
6. Montgomery SP, Chow CC, Smith SW, Marfin AA, O’Leary DR, Campbell
GL. Rhabdomyolysis in patients with West Nile encephalitis and meningitis.
Vector Borne Zoonotic Dis 2005;5(3):252–257.
7. Smith RD, Konoplev S, DeCourten-Myers G, Brown T. West Nile
virus encephalitis with myositis and orchitis. Hum Pathol 2004;35(2):
254–258.
8. Anninger WV, Lomeo MD, Dingle J, Epstein AD, Lubow M. West
Nile virus-associated optic neuritis and chorioretinitis. Am J Ophthalmol
2003;136(6):1183–1185.
9. Shaikh S, Trese MT. West Nile virus chorioretinitis. Br J Ophthalmol
2004;88(12):1599–1600.
10. Alshekhlee A, Sultan B, Chandar K. Opsoclonus persisting during sleep
in West Nile encephalitis. Arch Neurol 2006;63(9):1324–1326.
11. Ramat S, Leigh RJ, Zee DS, Optican LM. Ocular oscillations generated
by coupling of brainstem excitatory and inhibitory saccadic burst neurons.
Exp Brain Res 2005;160(1):89–106.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Fatal Clostridium septicum infection in a patient with a
hematological malignancy
Ragesh Panikkath, MD, DNB, DM, Venu Konala, MD, Deepa Panikkath, MD, Elvira Umyarova, MD,
and Fred Hardwicke, MD
A 49-year-old woman with acute myeloid transformation of myelodysplastic syndrome was admitted with mild erythema and pain in the right
thigh and left forearm. She was doing well and had been discharged the
previous day after consolidation chemotherapy. Examination showed only
mild erythema and tenderness of the right thigh. She was started on broadspectrum antibiotics. Discoloration progressed rapidly, and within hours
the right femoral and left brachial pulses were not palpable. She was
taken to the operating room for a suspicion of embolic arterial occlusion.
Surgical incision, however, revealed extensive necrosis of the tissues with
the presence of gas. Her relatives did not want her to undergo amputation.
The patient developed refractory hypotension and died within 15 hours of
presentation. Blood samples later tested positive for Clostridium septicum.
This case is presented to create awareness about the subtle presentation
and rapid progression of this infection, which can lead to death in less
than 24 hours.
lostridium septicum is an anaerobic gram-positive bacillus that is ubiquitous in the environment and is a resident of normal intestinal flora. It is capable of causing
gas gangrene in the absence of trauma but usually in
the setting of colonic or hematological malignancy (1, 2). This
case report highlights the subtle presentation of this infection,
which progresses within hours with a high mortality rate without early treatment.
C
CASE REPORT
A 49-year-old woman with acute myeloid transformation of
myelodysplastic syndrome was discharged home in an asymptomatic state after the first consolidation chemotherapy regimen
with high-dose cytosine arabinoside. She was otherwise healthy,
and her bone marrow aspirate was clear of blasts after the first
induction chemotherapy. She was admitted the next day with
pain in her right thigh and left forearm. Examination showed
only minimal erythema and tenderness of the right thigh. Her
blood pressure and heart rate were normal. Her abdomen was
soft with normal bowel sounds, without organomegaly. Her
white count was 1100/mm3 with an absolute neutrophil count
of 500/mm3. The chest radiograph was normal. Half an hour
later, however, the redness in her thigh had spread and the skin
had turned blue. Blood cultures were obtained. She was started
Proc (Bayl Univ Med Cent) 2014;27(2):111–112
empirically on cefepime and vancomycin. Three hours later,
she had significant swelling of her right thigh and left forearm
with feeble distal pulses. Embolic occlusion of the right femoral
artery and left brachial artery with compartment syndrome or
necrotizing fasciitis was suspected. An arterial Doppler showed
only feeble flow beyond the right femoral artery and the left
brachial artery, although no thrombus was visualized.
The vascular surgeon decided to do a manual thrombectomy.
After incision of the groin, however, it was evident that she had
necrotic thigh muscles extending posteriorly to the buttocks,
and there was gas formation in the tissue. Exploration of the left
cubital fossa also revealed the same findings. It was evident that
she would require disarticulation of the right hip and amputation of her left arm since limb salvage was not thought to be
possible. The family disagreed with this plan and wanted only
conservative measures. She became profoundly hypotensive
in spite of multiple vasopressors and died within 18 hours of
admission. Blood samples were positive for C. septicum.
DISCUSSION
C. septicum (previously Vibrion septique) is historically important in microbiology, being the first pathogenic anaerobe
cultured by Pasteur and Joubert in 1877 (3). Most of the gas
gangrene in soldiers during the first and second world wars
was attributed to this organism (4). Civilian infections due to
this organism were thought to be extremely rare at that time,
with only 11 cases reported from 1940 to 1967 (5). However,
with better anaerobic culture techniques, this organism is being
isolated in increasing numbers. Fortunately, this infection is still
rare, but it is usually fatal. This infection has been associated
with multiple medical problems including colonic malignancies
(1), hematologic malignancies, peripheral vascular disease, cyclic neutropenia with enterocolitis, and diabetes mellitus. Most
cases, however, are associated with malignancies. The infection
might predate malignant tumors by several years. Hence, follow-up evaluation might be important in patients who survive
(6). Early treatment is vital for this rapidly spreading infection,
From the Departments of Internal Medicine and Oncology, Texas Tech University
Health Sciences Center-School of Medicine, Lubbock, Texas.
Corresponding author: Ragesh Panikkath, MD, 3601 4th Street, MS 9410, Lubbock,
TX 79430 (e-mail: ragesh.panikkath@ttuhsc.edu; drrageshp@gmail.com).
111
with a mortality rate close to 100% if not treated within 12 to
24 hours (7).
C. septicum is a normal commensal of the human intestinal
tract and is ubiquitous in the environment. It is notorious for
causing gas gangrene in the absence of trauma (8), which makes
the diagnosis challenging without a high index of suspicion. It
can produce several toxins including deoxyribonuclease, lecithinase, hyaluronidase, and hemolysins, which can lead to tissue
necrosis, disseminated intravascular coagulation, intravascular
thrombosis, and hemolysis.
Factors causing defective host immunity, such as steroids,
diabetes, neutropenia, and alcohol abuse, might lead to translocation of the bacteria. This organism has been reported to
cause several infections, including clostridial myonecrosis (8),
osteomyelitis, septic arthritis, panophthalmitis, aortitis, intraabdominal abscess, intracranial infections, and abdominal wall
cellulitis. Localized pain, inflammation, crepitation, gas production, disproportionate tachycardia, discolored edematous skin,
and features of systemic toxicity are features that raise clinical
suspicion (9). Gas may be seen in tissues on x-rays and computed tomography scans in cases of gas gangrene and is due to
the production of nitrogen and hydrogen by the organism.
Even with effective treatment, including debridement and
antibiotics, the mortality rate approaches 60% (10). The drug of
choice for this infection is penicillin G. The extended-spectrum
cephalosporins, carbapenems, and metronidazole are the usual
alternatives in patients allergic to penicillins. Clindamycin, being a protein synthesis inhibitor, is believed to help reduce toxin
production by the organism. Amputation might be needed when
limb salvage is not possible. No controlled studies are available
112
regarding the use of hyperbaric oxygen therapy. Another concern
regarding hyperbaric oxygen therapy is that compared with other
clostridia, this organism has more tolerance to oxygen (11).
Factors associated with poor prognosis are presentation with septic
shock, immunosuppression, liver disease, and delay in initiation
of treatment.
Mirza NN, McCloud JM, Cheetham MJ. Clostridium septicum sepsis and
colorectal cancer—a reminder. World J Surg Oncol 2009;7:73.
2. Katlic MR, Derkac WM, Coleman WS. Clostridium septicum infection
and malignancy. Ann Surg 1981;193(3):361–364.
3. Sebald M, Hauser D. Pasteur, oxygen and the anaerobes revisited. Anaerobe
1995;1(1):11–16.
4. Maclennan JD. The histotoxic clostridial infections of man. Bacteriol Rev
1962;26:177–276.
5. Alpern RJ, Dowell VR Jr. Clostridium septicum infections and malignancy.
JAMA 1969;209(3):385–388.
6. Wentling GK, Metzger PP, Dozois EJ, Chua HK, Krishna M. Unusual
bacterial infections and colorectal carcinoma—Streptococcus bovis
and Clostridium septicum: report of three cases. Dis Colon Rectum
2006;49(8):1223–1227.
7. Chew SS, Lubowski DZ. Clostridium septicum and malignancy. ANZ J
Surg 2001;71(11):647–649.
8. Abella BS, Kuchinic P, Hiraoka T, Howes DS. Atraumatic clostridial myonecrosis: case report and literature review. J Emerg Med 2003;24(4):401–405.
9. Furste W, Dolor MC, Rothstein LB, Vest GR. Carcinoma of the large
intestine and nontraumatic, metastatic, clostridial myonecrosis. Dis Colon
Rectum 1986;29(12):899–904.
10. Larson CM, Bubrick MP, Jacobs DM, West MA. Malignancy, mortality,
and medicosurgical management of Clostridium septicum infection. Surgery
118(4):592–597.
11. Hill GB, Osterhout S. Experimental effects of hyperbaric oxygen
on selected clostridial species. II. In-vitro studies in mice. J Infect Dis
1972;125(1):26–35.
1.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Bilateral diaphragmatic paralysis associated with the use of
the tumor necrosis factor-alpha inhibitor adalimumab
Mina Mecheal Benjamin, MD, Alan William Martin, MD, and Randall Lee Rosenblatt, MD
A 51-year-old woman was referred for evaluation of progressive dyspnea
of 3 months’ duration. She had received 3 doses of adalimumab for
treatment of rheumatoid arthritis prior to the onset of her dyspnea. Her
chest examination revealed absent diaphragmatic movement with inspiration. Spirometry showed a severe restrictive defect. Radiologic studies
confirmed the diagnosis of bilateral diaphragmatic paralysis. Laboratory
and radiologic workup excluded other possible causes of the diagnosis.
Adalimumab was discontinued, and she was treated with bilevel positive airway pressure ventilation and intravenous immunoglobulin. Three
months later, the diaphragmatic paralysis persisted. This is the second
reported case of bilateral diaphragmatic paralysis occurring in a patient
who had received adalimumab. Acute neuropathies are rare side effects
of tumor necrosis factor-alpha inhibitors.
umor necrosis factor alpha (TNF-α) inhibitors currently
play a major role in the management of several autoimmune diseases. Infliximab was the first agent to be approved by the Food and Drug Administration (FDA)
in 1998. TNF-α blockers are approved for the management of
moderate to severely active rheumatoid arthritis or psoriatic arthritis, active ankylosing spondylitis, moderate to severely active
Crohn’s disease, and active ulcerative colitis in patients with an
inadequate response to conventional therapy (1). Five anti-TNF
agents have been approved by the FDA: infliximab, adalimumab,
etanercept, golimumab, and certolizumab. These agents have
demonstrated acceptable safety and tolerability profiles. As with
all immunosuppressants and immunomodulating therapies, TNF
inhibitors increase the risk of infections. Several autoimmune
adverse events have been reported, ranging from asymptomatic
immunological alterations to life-threatening autoimmune diseases (2). We report a case of bilateral diaphragmatic paralysis
that occurred following the institution of adalimumab.
T
CASE PRESENTATION
A 51-year-old white woman was referred to Baylor University Medical Center at Dallas for an evaluation of dyspnea.
Approximately 3 months prior to her referral, she experienced
dyspnea and pleuritic chest pain and was seen in a local emergency department, where she was prescribed a short course
of corticosteroids. One year prior to her symptoms, she was
Proc (Bayl Univ Med Cent) 2014;27(2):113–115
diagnosed with rheumatoid arthritis with symptoms of morning stiffness and pain in the metacarpal and shoulder joints.
She was initially treated with prednisone, methotrexate, and
sulfasalazine. However, she failed to respond, and adalimumab
was instituted. After three doses of adalimumab, she began to
experience progressive dyspnea and marked orthopnea. She
had no previous history of any respiratory symptoms and no
other significant medical history. She denied cough, chest pain,
or lower extremity swelling. On examination, she was tachypneic and using her sternocleidomastoid and scalene muscles.
Her chest examination revealed dullness to percussion in both
bases, paradoxical inward movement of the abdominal wall, and
poor diaphragmatic movement with inspiration. Her jugular
veins were not distended, and there was no leg edema. Her
heart sounds were normal. Neurologic examination disclosed
no abnormalities.
A chest radiograph showed small lung volumes and a normal cardiac silhouette. Her computed tomography scan did
not reveal any significant pleural, parenchymal, or mediastinal
abnormalities. Spirometry revealed a forced vital capacity (FVC)
of 0.39 L (12% of predicted), forced expiratory volume in 1
second (FEV1) of 0.38 L (14% of predicted), and FEV1/FVC
of 97%, consistent with a severe restrictive defect. Respiratory
muscle force testing showed a negative inspiratory force of –14
(17% of predicted) and an expiratory force of +24 (16% of
predicted). A fluoroscopy sniff test confirmed the diagnosis of
bilateral diaphragmatic paralysis. Her laboratory workup did
not reveal any findings associated with the known causes of
diaphragmatic paralysis, as shown in the Table. Adalimumab
was stopped, and she was empirically started on monthly intravenous immunoglobulin infusions. Bilevel positive airway
pressure was instituted to be used at night, and intermittent
positive pressure ventilation with a 40 cm pressure limit was
prescribed to assist with chest wall expansion. Three months
later, she continued to show diaphragmatic paralysis but was
less dyspneic.
From the Department of Internal Medicine (Benjamin, Rosenblatt) and the Division
of Neurology (Martin), Baylor University Medical Center at Dallas.
Corresponding author: Mina Mecheal Benjamin, MD, Department of Internal
Medicine, Baylor University Medical Center at Dallas, 3500 Gaston Avenue, Dallas,
TX 75246 (e-mail: mina.benjamin@baylorhealth.edu).
113
Table. Laboratory test results
Laboratory test
Result
Sodium (mEq/L)
135
Potassium (mEq/L)
4.1
Blood urea nitrogen (mg/dL)
Serum creatinine (mg/dL)
9
0.45
CO2 (mEq/L)
29
Alanine aminotransferase (U/L)
23
Aspartate aminotransferase (U/L)
25
Albumin (g/dL)
3.9
Bilirubin (mg/dL)
0.4
Erythrocyte sedimentation rate (mm/hr)
76
C-reactive protein (mg/L)
11.6
Rheumatoid factor (IU/mL)
7
Creatine kinase (ng/mL)
20
Antinuclear antibodies
Negative
Heavy metal screen
Negative
Cyclic citrullinated peptide antibodies
Negative
Acetylcholine receptor antibodies
Negative
Anti–muscle-specific tyrosine kinase antibodies
Negative
HIV 1, 2 antibodies
Nonreactive
Hepatitis panel
Nonreactive
Immunoglobulin A (mg/dL)
164
DISCUSSION
Demyelinating neuropathies have been reported as rare adverse events with anti–TNF-α therapy. The reported culprit has
more often been infliximab than etanercept or adalimumab.
Acute or chronic demyelinating neuropathies may occur a few
months after the institution of TNF-α treatment, very often
associated with conduction blocks on nerve conduction studies.
However, discontinuation of the offending drug and treatment
for demyelinating neuropathies have been associated with improvement in the neuropathy (3–5).
The proposed pathogeneses of TNF-α-blocker–associated
neuropathies include both a T-cell and humoral immune attack
against peripheral nerve myelin and inhibition of vital axonal
signaling functions. Vasculitis-induced nerve ischemia, either
from the underlying condition or enhanced by the drugs, remains
a possibility in some cases. Neuromuscular biopsies in several
patients, especially with mononeuritis simplex or multiplex, have
revealed necrotizing vasculitis (6). The temporal relationship between initiation of TNF-α antagonist therapy and the onset or
progression of vasculitis suggests that TNF-α inhibition triggers
or exacerbates vessel inflammation (6). Proposed mechanisms
whereby TNF-α inhibitors promote vasculitis include 1) development of antidrug or autoantibodies during TNF-α blockade
that form immune complexes that deposit in the walls of small
blood vessels to activate complement and trigger a type III hy114
persensitivity reaction; 2) changes in T-cell cytokine production;
3) elevation of nuclear antigen levels in the blood because of
increased apoptosis of cells targeted by TNF-α inhibitors; and 4)
an increase in the immunogenic load related to downregulation
of C-reactive protein by TNF-α inhibitors (7, 8).
Adalimumab (Humira; Abbott, Abbott Park, IL) is a recombinant human IgG1 monoclonal antibody specific for human
TNF-α. The drug was developed using phage display technology resulting in an antibody with human-derived heavy- and
light-chain variable regions and human IgG-1 constant regions.
Adalimumab binds specifically with TNF-α, blocking its interaction with the p55 and p75 cell surface TNF receptors and thereby
modulating TNF-induced or -modulated biological responses.
Neurologic deficits seen in patients who are receiving adalimumab include Guillain-Barré syndrome (9), wrist drop (10),
progressive sensory demyelinating polyneuropathy (11), and
optic neuropathy (12–14). Alexopoulou et al reported the other
case of acute bilateral phrenic neuropathy following treatment
with adalimumab (15). This patient was treated with adalimumab for psoriasis and developed acute bilateral phrenic neuropathy after the fourth dose. She was treated with oxygen, and
her symptoms resolved 4 weeks following the discontinuation of
adalimumab. This is the second reported case of diaphragmatic
paralysis in association with adalimumab use. In this case, the
temporal association of the phrenic nerve paralysis with the
administration of adalimumab and the absence of any other
known trigger suggest adalimumab to be the culprit agent for
this condition. The patient had no evidence of other causes
of mononeuropathies, including diabetes mellitus, amyloidosis, infections (e.g., HIV), malignancy, myasthenia gravis, and
amyotrophic lateral sclerosis. Although monofocal motor neuropathy with conduction block and electrophysiological evidence of demyelinating neuropathy might be a rare side effect of
adalimumab and other TNF-α blockers, these agents should be
considered in the differential diagnoses of these neuropathies.
1.
2.
3.
4.
5.
6.
7.
8.
Stübgen JP. Tumor necrosis factor-alpha antagonists and neuropathy.
Muscle Nerve 2008;37(3):281–292.
Ramos-Casals M, Brito-Zerón P, Muñoz S, Soria N, Galiana D, Bertolaccini L, Cuadrado MJ, Khamashta MA. Autoimmune diseases induced
by TNF-targeted therapies: analysis of 233 cases. Medicine (Baltimore)
2007;86(4):242–251.
Cocito D, Bergamasco B, Tavella A, Poglio F, Paolasso I, Costa P,
Ciaramitaro P, Isoardo G. Multifocal motor neuropathy during treatment with infliximab. J Peripher Nerv Syst 2005;10(4):386–387.
Singer OC, Otto B, Steinmetz H, Ziemann U. Acute neuropathy with
multiple conduction blocks after TNFα monoclonal antibody therapy.
Neurology 2004;63(9):1754.
Tektonidou MG, Serelis J, Skopouli FN. Peripheral neuropathy in two
patients with rheumatoid arthritis receiving infliximab treatment. Clin
Rheumatol 2007;26(2):258–260.
Richette P, Dieudé P, Damiano J, Lioté F, Orcel P, Bardin T. Sensory
neuropathy revealing necrotizing vasculitis during infliximab therapy for
rheumatoid arthritis. J Rheumatol 2004;31(10):2079–2081.
Jarrett SJ, Cunnane G, Conaghan PG, Bingham SJ, Buch MH, Quinn
MA, Emery P. Anti-tumor necrosis factor-alpha therapy-induced vasculitis:
case series. J Rheumatol 2003;30(10):2287–2291.
Cunnane G, Warnock M, Fye KH, Daikh DI. Accelerated nodulosis and
vasculitis following etanercept therapy for rheumatoid arthritis. Arthritis
Rheum 2002;47(4):445–449.
Baylor University Medical Center Proceedings
Volume 27, Number 2
9. Shin IS, Baer AN, Kwon HJ, Papadopoulos EJ, Siegel JN. GuillainBarré and Miller Fisher syndromes occurring with tumor necrosis
factor alpha antagonist therapy. Arthritis Rheum 2006;54(5):1429–
1434.
10. Alentorn A, Albertí MA, Montero J, Casasnovas C. Monofocal motor
neuropathy with conduction block associated with adalimumab in rheumatoid arthritis. Joint Bone Spine 2011;78(5):536–537.
11. Lozeron P, Denier C, Lacroix C, Adams D. Long-term course of demyelinating neuropathies occurring during tumor necrosis factor-alpha-blocker
therapy. Arch Neurol 2009;66(4):490–497.
12. Chung JH, Van Stavern GP, Frohman LP, Turbin RE. Adalimumabassociated optic neuritis. J Neurol Sci 2006;244(1–2):133–136.
13. Kim A, Saffra N. A case report of adalimumab-associated optic neuritis.
J Ophthalmic Inflamm Infect 2012;2(3):145–147.
14. von Jagow B, Kohnen T. Anterior optic neuropathy associated with adalimumab. Ophthalmologica 2008;222(4):292–294.
15. Alexopoulou A, Koskinas J, Soultati A, Katsaounis P, Kilidireas K, Papageorgiou C, Antoniou C, Katsambas A, Archimandritis A. Acute bilateral
phrenic neuropathy following treatment with adalimumab. Clin Rheumatol 2009;28(11):1337–1140.
Avocations
Perception
He had seen a falling robin in the blooming pansies.
Compelled by an inner urge rushed to his aid.
Flaccid bird was now nestled in the doctor’s palm.
Fetched water from the fountain;
Moistened bird’s beak.
Reflexive movement of the tongue gave a flicker of hope.
Accustomed to dispensing care. The fingers were in action—
Massaging chest of the bird, helping him to breathe.
All the while lips whispered gentle comforting sounds.
Suddenly, the bird moved,
Raised the head and shook stupor off.
Flew past the hypnotic berries he had eaten earlier.
People in the crowded office stood on their feet,
Watching the entire scene through the glass window.
Someone boasted with glee: “That is my doctor.”
Lobby full of waiting patients clapped in approval!
—Amanullah Khan, MD, PhD
Dr. Khan (e-mail: aman1963@gmail.com) is an oncologist at Baylor Medical Center at McKinney. In addition to publishing over
100 research articles, he is an award-winning poet who has written poems in three languages.
April 2014
Bilateral diaphragmatic paralysis associated with the use of the tumor necrosis factor-alpha inhibitor adalimumab
115
Celiac artery disease and fatal rupture of a hepatic artery
aneurysm in the Ehlers-Danlos syndrome
Amritpal Nat, MD, Tanya George, MD, Gregory Mak, MPH, Amit Sharma, MD, MPH, Amitpal Nat, MD,
and Robert Lebel, MD
Isolated visceral arteriopathies of the celiac and hepatic artery are rare.
We present a case of a Caucasian man who presented with abdominal
pain and was found to have a spontaneous celiac artery dissection.
Genetic analysis revealed a mutation consistent with Ehlers-Danlos
syndrome type IV. The patient died 2 months later from a spontaneous
rupture of his hepatic artery.
CASE REPORT
A 31-year-old man with fragile, easily bruisable skin,
abnormal (atrophic) scarring, joint hypermobility, and
extensive varicosities of the legs presented with sudden
onset of left upper quadrant abdominal pain. His blood
pressure was 146/75 mm Hg and heart rate, 114 beats/
min. The epigastric region was tender and the left upper quadrant of his abdomen was soft. His joints were
hypermobile, his skin over the chest was translucent, and
severe varicose veins were present on his lower torso and
lower extremities. A complete blood count, basic metabolic
panel, liver function tests, activated partial thromboplastin
time, prothrombin time/international normalized ratio,
and amylase and lipase levels were within normal limits
(Table). An electrocardiogram showed only sinus tachycardia, and an echocardiogram was normal. Computed
tomography (CT) of the abdomen revealed high-density
fluid around the pancreas and spleen. A serologic workup
for a vasculitis was negative.
Due to a normal amylase and lipase level and persistent
abdominal pain, a CT angiogram of the thorax and abdomen was performed and revealed a celiac artery dissection
with associated thrombus extending into the splenic artery
(Figure). The spleen was infarcted. The patient was managed
with anticoagulation by continuous heparin infusion and
metoprolol. He responded well to conservative management
and was discharged home. There was a clinical suspicion of
Ehlers-Danlos syndrome (EDS) type IV. The patient’s paternal
grandmother also had extensive varicosities. Molecular studies
revealed a mutation in the COL3A1 gene, which is consistent
with the diagnosis of EDS type IV.
Approximately 2 months after hospital discharge, the patient
complained once again of sudden onset of severe abdominal
116
Table. Patient laboratory values
Test
Result
Sodium (mmol/L)
138
Potassium (mmol/L)
3.7
Chloride (mmol/L)
102
Bicarbonate (mmol/L)
28
Blood urea nitrogen (mg/dL)
11
Creatinine (mg/dL)
0.7
Glucose (mg/dL)
116
Alanine aminotransferase (U/L)
27
Aspartate aminotransferase (U/L)
21
Bilirubin total (mg/dL)
0.25
Lipase (U/L)
26
Amylase (U/L)
78
White blood cells (K/μL)
15.1
Hematocrit (%)
42.8
Hemoglobin (%)
15.2
Platelet (K/μL)
321
International normalized ratio
1.0
Partial thromboplastin time (seconds)
25
Antineutrophil cytoplasmic antibodies
Negative
Antinuclear antibody
Negative
pain. As he and his wife were on their way to the car to drive
to the emergency department, he collapsed and died. Autopsy
revealed a ruptured hepatic artery aneurysm with 2.5 to 3 L of
fresh blood in the peritoneal cavity. Their infant son did not
have the COL3A1 mutation.
From State University of New York Upstate Medical University, Syracuse,
New York.
Corresponding author: Amritpal Nat, MD, State University of New York
Upstate Medical University, 750 East Adams Street, Syracuse, NY 13210-2375
(e-mail: amritpal.nat@nih.gov).
Proc (Bayl Univ Med Cent) 2014;27(2):116–117
DISCUSSION
Edvard Ehlers (1863–1937) in Denmark and Henri-Alexandre Danlos (1844–1912) in France independently published
lucid descriptions of the condition that would later bear both
their names; Ehlers published in 1901 and Danlos in 1908 (1).
Now many types of EDS are recognized. All three patterns of
Mendelian inheritance are represented (autosomal dominant,
autosomal recessive, and X-linked recessive) (2). EDS type
IV, also known as the vascular type, is a rare connective tissue
disorder with autosomal dominant transmission (McKusick
catalog number 130050) caused by mutations in the COL3A1
gene. As a result, these patients have increased fragility of connective tissue with arterial, intestinal, and uterine ruptures.
The estimated prevalence for types of EDS varies between 1
in 10,000 and 1 in 25,000, with EDS type IV representing
approximately 5% to 10% of cases (3). The median age of
death is 50 years (3, 4).
Search of medical publications to 1959 revealed only
39 cases of isolated celiac artery dissections, making it the
least common visceral artery dissection reported. Treatment
options include surgery, endovascular repair, or medical management (3).
1.
2.
3.
Figure. CT angiogram of the abdomen (sagittal view) showing an isolated celiac
artery dissection.
April 2014
4.
Johns Hopkins Medicine. Online Mendelian Inheritance in Man. Available
at www.omim.org.
Genetests.org (for online information about genetic testing, and for brief
reviews)
Germain DP. Ehlers-Danlos syndrome type IV. Orphanet J Rare Dis
2007;2:32.
Ganesamoni R, Agarwal S, Stephen E, Narayan RL. Isolated celiac artery
dissection with splenic infarction: report of a case. Eur J Vasc Endovasc
Surg 2007;13(4):58–59.
Celiac artery disease and fatal rupture of a hepatic artery aneurysm in the Ehlers-Danlos syndrome
117
The most common cause of hemoptysis worldwide: a fluke?
Amritpal Nat, MD, Amitpal Nat, MD, Amit Sharma, MBBS, MPH, Ghanshyam Shastri, MD, and Michael C. Iannuzzi, MD, MBA
Global travel is associated with an increasing incidence of helminthic
infections in nonendemic regions. We describe a patient with recurrent
hemoptysis from a chronic infection not commonly found in the USA.
CASE PRESENTATION
A 20-year-old healthy female college swimmer was referred for evaluation of intermittent episodes of hemoptysis
for 1 year. She had one to two episodes every other week
of quarter-sized hemoptysis associated with dyspnea. Her
symptoms began after a dive 3 meters above the pool resulting in a “belly flop.” Her vital signs and complete blood
count with differential were within normal limits, and her
initial radiograph was normal. Computed tomography (CT)
showed two cystic lesions in the right lower lobe (Figure 1).
The patient denied alcohol, cigarette, or illicit drug use. She
had traveled to Costa Rica and the Bahamas 1 year earlier.
Bronchoscopy with bronchoalveolar lavage, brushings, and
CT-guided biopsy were unremarkable. Cultures from the
bronchial washings and the cytology were negative. Pulmonary function tests were normal. Workup for connective tissue disorders was negative. Further evaluation for pulmonary
tuberculosis, mycoplasma, histoplasmosis, and blastomycosis
was negative.
Subsequent CT scans showed interval resolution and redistribution of the cystic lesions (Figure 2). Paragonimus westermani
antibody titers were obtained 1 year after the initial presentation
and were elevated at 1:32. The diagnosis of chronic pulmonary
paragonimiasis was made, and the patient responded well to
praziquantel (1, 2).
DISCUSSION
The presentation of hemoptysis after diving with the
finding of cysts on chest CT led to a consideration of
traumatic pneumatocele. Given the relatively mild chest
injury at the time of the dive, the resolution and recurrence of the lung parenchymal cysts, and the recent travel
history, an infectious etiology was more likely. Although
stool, sputum, and bronchial washings for ova and parasites
118
Figure 1. CT thorax showing thin-walled cysts within the parenchyma of the right
lower lobe. This represents a late radiologic finding of pulmonary paragonimiasis.
were negative, Paragonimus westermani titers were elevated.
Serologic testing for anti-Paragonimus IgG has a sensitivity
of nearly 100% and a specificity of 91% to 100% (3).
Paragonimus westermani, also known as the lung fluke, is
acquired through the ingestion of raw/undercooked crabs or
crayfish. It is the most common cause of hemoptysis worldwide (4). Diagnosis can be challenging, and clinicians should
be alerted to the sensitivity and specificity of serologic testing. Treatment involves a 3-day course of praziquantel with a
response rate of 100% (5). This clinical vignette underscores
the importance of health care providers in the USA recognizing
common worldwide infections.
From State University of New York Upstate Medical University, Syracuse,
New York.
Corresponding author: Amritpal Nat, MD, State University of New York
Upstate Medical University, 750 East Adams Street, Syracuse, NY 13210-2375
(e-mail: NatA@upstate.edu).
Proc (Bayl Univ Med Cent) 2014;27(2):118–119
Figure 2. CT thorax 5 months later showing interval resolution of cysts within the lateral segment of the right lower lobe and the appearance of new thin-walled
cysts within the medial segments of the right lower and middle lobes. Additional, nonspecific patchy ground-glass and nodular opacities likely represent reactive
inflammation.
1.
2.
Johnson RJ, Jong EC, Dunning SB, Carberry WL, Minshew BH. Paragonimiasis: diagnosis and the use of praziquantel in treatment. Rev Infect
Dis 1985;7(2):200–206.
Nakamura-Uchiyama F, Onah DN, Nawa Y. Clinical features of paragonimiasis cases recently found in Japan: parasite-specific immunoglobulin
M and G antibody classes. Clin Infect Dis 2001;32(12):e151–e153.
April 2014
3.
4.
5.
Yong TS, Seo JH, Yeo IS. Serodiagnosis of human paragonimiasis by
ELISA-inhibition test using monoclonal antibodies. Korean J Parasitol
1993;31(2):141–147.
Davis GS, Marcy TW, Seward EA, eds. Medical Management of Pulmonary
Diseases. New York, NY: Marcel Dekker, 1999:345.
Nawa Y. Re-emergence of paragonimiasis. Intern Med 2000;39(5):353–354.
The most common cause of hemoptysis worldwide: a fluke?
119
Stress-induced (takotsubo) cardiomyopathy following thoracic
epidural steroid injection for postherpetic neuralgia
Nicholas P. McKernan, MD, Bryan J. Rondeau, MD, and Russell K. McAllister, MD
We present what may be the first documented case of takotsubo cardiomyopathy following a thoracic epidural steroid injection. The 77-year-old
patient had many risk factors predisposing her to takotsubo cardiomyopathy, including gender, postmenopausal status, and numerous recent
stressful events in her life. Although she presented to the emergency
department with symptoms of an acute myocardial infarction, her findings
on electrocardiography, echocardiography, coronary angiography, and
cardiac enzymes supported the diagnosis of takotsubo cardiomyopathy.
While takotsubo cardiomyopathy is rare, it is important for the clinician to
distinguish it from an acute myocardial infarction, as the two conditions
present similarly but may have distinctly different clinical outcomes.
akotsubo cardiomyopathy (TC), also known as stress-induced cardiomyopathy, is a transient systolic dysfunction
of the left ventricle typically triggered by an acute illness
or intense emotional or physical stress (1). Postherpetic
neuralgia (PHN) is pain persisting in a herpes zoster–affected
area >6 months after healing of the zoster eruptions (2). We
present a patient with significant psychosocial stressors who
underwent a thoracic epidural steroid injection for treatment
of PHN and then developed TC.
T
CASE REPORT
A 77-year-old woman with PHN returned to our anesthesia
pain clinic for a repeat thoracic epidural steroid injection. Prior
treatment with epidural steroid injections, propoxyphene, and
gabapentin had adequately managed her pain. Previously, she
had herpes zoster, multiple myeloma, stage III chronic kidney
disease, anemia, hypertension, hypothyroidism, a deep venous
thrombosis, and degenerative disk disease. A brother had recently died, and her husband had recently been admitted to a
nursing home for his declining health.
After reexamination, a T4-5 epidural steroid injection under
fluoroscopic guidance was planned. No sedation was administered.
The patient was positioned prone on the fluoroscopy table, and the
overlying tissue was anesthetized with 1% lidocaine. A 17-gauge
Tuohy needle was inserted via a left paramedian approach under
fluoroscopic guidance, and the loss of resistance technique was used
to identify the epidural space on the first pass. After negative aspiration of blood or cerebrospinal fluid, a solution containing 80 mg of
triamcinolone and 4 mL of 0.125% bupivacaine was injected.
120
The patient remained stable throughout the procedure. At
discharge, she had no new neurological deficits or complaints.
She attended an unrelated appointment and then returned
home to take a nap. Soon after, she developed a headache and
progressively worsening chest pain. She was taken to the emergency department (ED), where she reported substernal chest
pain radiating into her left neck, dyspnea, nausea, and an episode of vomiting.
While in the ED, she received nitroglycerin, fentanyl, heparin, and aspirin. An electrocardiogram showed mild ST-segment
elevation with Q waves in the precordial leads and widening
of the QRS complex. Her troponin was 0.09 ng/mL on arrival to the ED and 1.84 ng/mL 4 hours later. A transthoracic
echocardiogram demonstrated depression of the apex of the
left ventricle with apical ballooning, preserved wall motion of
the basal segments, and an estimated ejection fraction of 30%.
Cardiac catheterization revealed only mild narrowing of the left
main coronary artery. Her troponin level peaked at 2.7 ng/mL.
A repeat echocardiogram on hospital day 3 showed improvement of her ventricular function, and her troponin level had
dropped to 1.0 ng/mL. She was discharged home on hospital
day 4. A repeat echocardiogram 20 days later showed no regional wall motion abnormalities and an estimated ejection
fraction of 55%.
DISCUSSION
While there is an abundance of literature regarding the treatment of PHN, we know of no previously reported cases of TC
following an epidural steroid injection. TC derives its name
from the echocardiographic appearance of the heart, which
resembles a “takotsubo,” the Japanese word for an octopus trap.
The typical appearance is characterized by mid and apical segmental depression of the left ventricle with compensatory basal
wall hyperkinesis that results in ballooning of the left ventricular
apex during systole (3).
The condition is typically triggered by severe stress (e.g.,
severe illness, a catastrophic event, death in the family) and
From Baylor Scott & White Health and Texas A&M Health Science Center College
of Medicine, Temple, Texas.
Corresponding author: Russell K. McAllister, MD, Department of Anesthesiology,
Baylor Scott & White Health, 2401 South 31st Street, Temple, TX 76508 (e-mail:
rmcallister@sw.org).
Proc (Bayl Univ Med Cent) 2014;27(2):120–121
may mimic an acute myocardial infarction. The typical presentation is acute substernal chest pain accompanied by dyspnea,
syncope, or shock (1, 4). Electrocardiographic changes may
include initial ST segment elevation followed by T wave inversion with QT prolongation throughout the anterior leads
(5, 6). Patients also typically have cardiac enzyme elevation
and an absence of significant coronary artery disease on angiogram (1).
Unlike an acute myocardial infarction, TC appears most
commonly in postmenopausal women. It is theorized that decreased sex hormones (specifically estrogen) in such women
predispose them to the condition, although there is currently no
clear explanation (4). The prevalence of TC ranges from 0.7%
to 2.2% of patients (from Japan and the Western hemisphere)
who present with acute coronary syndrome. The prognosis is
excellent. In a review by Gianni et al, the condition was noted to
have a mortality of only 1.1%, and almost all surviving patients
fully recover, with a recurrence rate <3% (4, 5).
There is a strong correlation between emotional stress and
TC. Our patient’s recent family stressors and chronic PHN
pain likely predisposed her to TC, with the thoracic epidural
April 2014
injection likely acting as the final trigger for her ensuing cardiac
event.
1.
2.
3.
4.
5.
6.
Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa
M, Yoshiyama M, Miyazaki S, Haze K, Ogawa H, Honda T, Hase M,
Kai R, Morii I; Angina Pectoris-Myocardial Infarction Investigations in
Japan. Transient left ventricular apical ballooning without coronary artery
stenosis: a novel heart syndrome mimicking acute myocardial infarction.
J Am Coll Cardiol 2001;38(1):11–18.
Mahn F, Baron R. Postherpetic neuralgia [article in German]. Klin Monbl
Augenheilkd 2010;227(5):379–383.
Kurowski V, Kaiser A, von Hof K, Killermann DP, Mayer B, Hartmann
F, Schunkert H, Radke PW. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency,
mechanisms, and prognosis. Chest 2007;132(3):809–816.
Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical
ballooning syndrome or takotsubo cardiomyopathy: a systematic review.
Eur Heart J 2006;27(13):1523–1529.
Turley A, Graham R, Hall J. Takotsubo cardiomyopathy in two female
patients: two case reports. Cases J 2008;1(1):325.
Mitsuma W, Kodama M, Ito M, Tanaka K, Yanagawa T, Ikarashi N, Sugiura
K, Kimura S, Yagihara N, Kashimura T, Fuse K, Hirono S, Okura Y,
Aizawa Y. Serial electrocardiographic findings in women with takotsubo
cardiomyopathy. Am J Cardiol 2007;100(1):106–109.
Stress-induced (takotsubo) cardiomyopathy following thoracic epidural steroid injection for postherpetic neuralgia
121
Invited commentary
Takotsubo cardiomyopathy following epidural steroid injection: yet another
way to break the heart
n the relatively short period of time since takotsubo cardiomyopathy was described in Japan (1) or introduced to the
United States (2), there has been an explosion of publications regarding the ways the cardiomyopathy is triggered,
the patterns of the cardiomyopathy itself (typical and atypical), and potential mechanisms for the underlying pathology
(3–5). Dr. McAllister et al describe yet another way in which
patients with normal (or nearly normal) coronary arteries can
incur devastating yet transient damage to the heart during physiologic and emotional stress. The patient in this case had several
stressful issues occurring simultaneously, including the death
of a brother, the declining health of her husband, and the pain
of both her postherpetic neuralgia as well as the procedure to
treat that pain.
The features of this case, including the physical and emotional stress and the age and gender of the patient, have become
commonplace and well recognized. It is such a well-recognized
pattern that cardiology fellows see a ventriculogram of a left
anterior descending artery infarct and mistakenly assume that
it is another example of takotsubo cardiomyopathy rather than
the much more common ischemic cardiomyopathy.
While the triggers of the events seem to be a variety of
stresses, it is becoming clearer that the final common pathophysiology pathway may be coronary spasm, although the details
remain to be worked out (6). There are still many questions
to answer, including why takotsubo cardiomyopathy happens
infrequently, why there is an incredibly strong preponderance in
menopausal women, and why it is so uncommon for a patient
who had an initial event to experience it a second time.
I
122
A recent article by Tobis suggests that gathering and collating data from multiple centers may allow us to gain insights
into the cause of this fascinating and uncommon disease (7).
With additional cases and information, the mystery may yet
be solved.
—Jeffrey M. Schussler, MD
Division of Cardiology, Baylor University Medical Center
Texas A&M Health Science Center, College of Medicine
Dallas, Texas (e-mail: Jeffrey.Schussler@Baylorhealth.edu)
1.
2.
3.
4.
5.
6.
7.
Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning
due to simultaneous multivessel coronary spasms: a review of 5 cases
[article in Japanese]. J Cardiol 1991;21(2):203–214.
Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP,
Gerstenblith G, Wu KC, Rade JJ, Bivalacqua TJ, Champion HC. Neurohumoral features of myocardial stunning due to sudden emotional stress.
N Engl J Med 2005;352(6):539–548.
Mikail N, Hess S, Jesel L, El Ghannudi S, El Husseini Z, Trinh A,
Ohlmann P, Morel O, Imperiale A. Takotsubo and takotsubo-like syndrome: a common neurogenic myocardial stunning pathway? Int J Cardiol
2013;166(1):248–250.
Patankar GR, Choi JW, Schussler JM. Reverse takotsubo cardiomyopathy: two case reports and review of the literature. J Med Case Rep
2013;7(1):84.
Patankar GR, Donsky MS, Schussler JM. Delayed takotsubo cardiomyopathy
caused by excessive exogenous epinephrine administration after the treatment
of angioedema. Proc (Bayl Univ Med Cent) 2012;25(3):229–230.
Patel SM, Lerman A, Lennon RJ, Prasad A. Impaired coronary microvascular
reactivity in women with apical ballooning syndrome (takotsubo/stress
cardiomyopathy). Eur Heart J Acute Cardiovasc Care 2013;2(2):147–152.
Tobis J. Takotsubo syndrome: a call to action. Catheter Cardiovasc Interv
2013;82914.
Proc (Bayl Univ Med Cent) 2014;27(2):122
Irregular cardiac rhythm with wide QRS complexes
D. Luke Glancy, MD, and Manpreet Singh, MD
he patient is an 80-year-old woman
with a history of aortic valve replacement, chronic kidney disease, and a
left ventricular ejection fraction of
35%. The cardiac rhythm is atrial fibrillation,
which in her is permanent. A VVI pacemaker
senses and captures normally (Figure). The
pacemaker lead is in the right ventricle, and
consequently pacer-initiated QRS complexes
(the first QRS in the limb leads and the third
and fourth QRSs in the precordial leads) resemble left bundle branch block. The other
seven QRSs are the result of conduction down
the atrioventricular node and His bundle and
show left bundle branch block.
There is a difference between the QRSs
of the paced complexes and the QRSs of the
native complexes in addition to the presence
or absence of pacemaker spikes. In lead V1,
the paced QRS has a notch on its downstroke
making it slow, whereas the downstroke of the
native QRS has no notch and is quick. Kindwall et al described the differences between
lead V1 morphology in ventricular tachycardia
with a left bundle branch block-like morphology and in supraventricular tachycardia with
left bundle branch block aberration (1). With
ventricular tachycardia, V1 may show a wide
r wave and/or a notch on the downstroke of
Figure. Twelve-lead electrocardiogram in an 80-year-old woman with an electronic ventricular pacemaker.
the S wave, and from the beginning of the
QRS to the nadir of the S is > 0.06 s. In contrast, with left bundle branch block aberration, there is either
1. Kindwall KE, Brown J, Josephson ME. Electrocardiographic criteria for
a QS wave in lead V1 or the initial r wave is brief (≤0.02 s);
ventricular tachycardia in wide-complex left bundle-branch morphology
there is no notch on the quick downstroke of the S wave; and
tachycardia. Am J Cardiol 1988;61(15):1279–1283.
the time from the beginning of the QRS to the nadir is ≤0.06 s.
Although Kindwall et al described these differences in patients
with wide QRS tachycardias, they obviously would apply to
From the Sections of Cardiology, Departments of Medicine, Louisiana State
single premature complexes. As in our case, they also apply
University Health Sciences Center and the Interim LSU Hospital, New Orleans,
to right ventricular pacing which is not in a location that can
Louisiana.
replicate conduction that is normal except for left bundle branch
Corresponding author: D. Luke Glancy, MD, 7300 Lakeshore Drive, #30, New
Orleans, LA 70124 (e-mail: dglanc@lsuhsc.edu).
block.
T
Proc (Bayl Univ Med Cent) 2014;27(2):123
123
Inverted P waves, QRS complexes, and T waves in lead I in a
64-year-old woman
D. Luke Glancy, MD, and Davey L. Prout Jr., MD
he combination of inverted Ps,
QRSs, and Ts in lead I (Figure 1)
suggests two possibilities: arm-lead
reversal and situs inversus with
mirror-image dextrocardia. The standard
precordial leads usually settle the issue; they
are normal in arm-lead reversal and show
diminishing QRS voltage from V1 to V6,
usually with dominant S waves, in situs
inversus. This electrocardiogram (ECG),
however, fits neither description. The precordial leads show a reverse of the usual progression. Lead V1 resembles the usual lead
V6, V2 resembles the usual V5, and so forth,
with V6 resembling the usual V1. Thus, the
precordial leads also have been reversed.
When the arm leads are reversed, lead
I is an inversion of the true lead I; lead
II is the true lead III; lead III is the true
lead II; aVR is the true aVL; aVL is the
true aVR; and aVF is unchanged. With
these caveats and the reversed sequence
of V1 to V6 in mind, this ECG is normal.
An ECG recorded 12 days later (Figure 2)
indeed is normal and resembles all of the
ECGs recorded in this patient before the
one shown in Figure 1.
The bane of the electrocardiographer
is the misinformation provided by artifacts, lead misplacement, and labeling the
ECG with the wrong name (1). Most lead
misplacement is not intentional. When
it is intentional, such as recording the
chest leads on the right side looking for
evidence of right ventricular infarction in
a patient with an acute inferior infarct,
this should be stated clearly on the tracing.
T
1.
124
Figure 1. ECG in a 64-year-old woman.
Figure 2. ECG in the same woman 12 days later.
Surawicz B, Knilans TK. Misplacement of leads and electrocardiographic
artifacts. In Surawicz B, Knilans TK, eds. Chou’s Electrocardiography in
Clinical Practice: Adult and Pediatric, 5th ed. Philadelphia: WB Saunders,
2001:569–582.
From the Sections of Cardiology, Departments of Medicine, Louisiana State University
Health Sciences Center and the Interim LSU Hospital, New Orleans, Louisiana.
Corresponding author: D. Luke Glancy, MD, 7300 Lakeshore Drive, #30, New
Orleans, LA 70124 (e-mail: dglanc@lsuhsc.edu).
Proc (Bayl Univ Med Cent) 2014;27(2):124
Triple-hit lymphoma
Naresh Pemmaraju, MD, Javed Gill, MD, Saurabh Gupta, PhD, and John R. Krause, MD
We report a case of a triple-hit lymphoma in a 72-year-old man. This
lymphoma was diagnosed using morphology, flow cytometry, immunochemistry, and cytogenetics. Since many triple-hit lymphomas have not
been documented in the literature, it is important to bring attention to
this entity, as this lymphoma has different prognostic and therapeutic
implications than other diffuse large B-cell lymphomas, thus making a
correct and early diagnosis important.
hromosomal translocations are biologic and diagnostic
hallmarks of disease in many B-cell lymphomas. There is
a unique subset, the so-called “double-hit lymphomas,”
that are defined by a chromosomal breakpoint affecting
the MYC/8q24 locus in combination with another recurrent breakpoint, usually at (14;18)(q32;q21) involving BCL-2. This led to a
new category of lymphomas in the 2008 World Health Organization (WHO) classification: “B-cell lymphoma unclassifiable with
features intermediate between diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL).” Double-hit lymphomas are
associated with a poor prognosis. An even more uncommon entity
is the “triple-hit lymphoma.” The exact incidence is unknown, and
the WHO has not, as of yet, classified it specifically. Triple-hit lymphomas also have morphologic, phenotypic, and genetic features
intermediate between DLBCL and BL. However, the characteristic
cytogenetic abnormalities involve chromosomal rearrangements of
c-MYC, BCL-2, and BCL-6 genes. The clinical implication of correctly diagnosing this entity is significant, as triple-hit lymphomas
also have a much worse prognosis than either DLBCL or BL alone,
and therapeutic options are different. We report a case of a patient
presenting with fever, fatigue, night sweats, and an inguinal mass
that was biopsied to reveal a DLBCL of germinal center origin on
first impression. Because of a high proliferative index, cytogenetics were obtained, which showed chromosomal rearrangements
consistent with a diagnosis of triple-hit lymphoma.
C
CASE REPORT
A 72-year-old African American man with previous chronic
gout and hypertension was admitted to Baylor University Medical Center at Dallas due to weight loss of 25 pounds, fatigue,
and failure to thrive. He was found to have an enlarging inguinal mass on the left side measuring 7 cm, which had been
Proc (Bayl Univ Med Cent) 2014;27(2):125–127
Figure 1. Large cell lymphoma (hematoxylin and eosin, ×500).
present for 2 months. His lactate dehydrogenase was 882 U/L
(reference range, 100–190); beta-2-microglobulin, 5.56 ng/mL
(reference range, 0.60–2.29); ferritin, 926 ng/mL (reference
range, 22–322); hemoglobin, 8.5 g/dL; and hematocrit, 24.9%.
Radiographic imaging disclosed bilateral kidney masses, as well
as a mass in the left lobe of the liver. His hospital course was
complicated by acute renal failure and urinary tract infection
treated with antibiotics and intravenous fluids.
The inguinal mass was biopsied. Sections showed a diffuse
infiltrate consisting of sheets of discohesive medium and large
cells with large nuclei, irregular nuclear membranes, and prominent nucleoli with no architectural pattern (Figures 1 and 2).
Flow cytometry showed a 62% population of large clonal B
cells expressing CD10, CD19, CD20, CD45, and Kappa, but
not CD5. Immunochemistry showed CD45, BCL-2, BCL6, CD10, CD20, and CD79a positivity and CD30, MUM1,
EBER, and CD34 negativity. Ki-67 (proliferation index) was
very high (>90%) (Figure 2).
From the Department of Pathology, Baylor University Medical Center at Dallas.
Corresponding author: John R. Krause, MD, Section of Hematopathology,
Department of Pathology, Baylor University Medical Center at Dallas, 3500 Gaston
Avenue, Dallas, TX 75246 (e-mail: john.krause@BaylorHealth.edu).
125
Figure 2. CD20 immunostain indicating B-cell lymphoma (CD20 immunoperoxidase stain ×400).
The morphology, immunochemistry stains, and flow cytometry results supported a diagnosis of a lymphoma with features
intermediate between DLBCL and BL. Cytogenetic analysis was
performed with fluorescence in situ hybridization to reveal gene
rearrangements of BCL-2 (18q21), BCL-6 (3q27), and c-MYC
(8q24) genes (Figure 3). These features are consistent with a triplehit lymphoma. A bone marrow biopsy was negative. A positron
emission tomography scan revealed masses in the left inguinal
region, both kidneys, and the left lobe of the liver. The patient was
discharged to another facility in stable condition for treatment
and management options. On follow-up we were told that the
patient was treated with rituximab and hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone) alternately
with rituximab, methotrexate, and cytarabine. Apparently the
patient had an initial response but the tumor recurred, and he
died about 6 months following the initial diagnosis.
DISCUSSION
B-cell lymphomas commonly have chromosomal gene rearrangements (1). For example, rearrangement of the BCL-2 or
a
c-MYC gene with the immunoglobulin gene (IG) can result in
follicular lymphoma or BL, respectively. However, to have two
gene rearrangements (double-hit lymphomas) is uncommon
(2). Translocation of the BCL-2 gene on chromosome 18q21
results in constant inactivation of apoptosis (3). Translocation
of the c-MYC gene on chromosome 8q24 results in constant cell
proliferation (3). These double-hit lymphomas are associated
with an aggressive clinical course, with poor response to treatment, complex karyotypes, and pathologic features of DLBCL
and BL (4). These pathological features include a “starry sky”
appearance with a high MiB-1 (which is consistent with BL),
but with larger cells with irregular nuclei and more prominent
nucleoli (which is consistent with DLBCL). The incidence is
estimated to be approximately 2% of all B-cell lymphomas (5).
The median survival time is reported to be about 5 months,
significantly shorter than for either DLBCL or BL (6).
Triple-hit lymphomas have been infrequently reported, with
only a small number of case reports noted. These lymphomas
are rare and the exact incidence is unknown. The Mitelman
lymphoma database in 2009 reported only eight triple-hit
lymphomas out of 796 lymphomas containing a BCL-6 gene
rearrangement (7). Triple-hit lymphomas are defined similar to
double-hit lymphomas as having morphologic, biologic, and
cytogenetic properties similar to both DLBCL and BL, but
possessing three, instead of two, gene rearrangements: c-MYC,
BCL-2, and BCL-6 genes (7). They are also associated with
a more aggressive clinical course, as these lymphomas have a
propensity to spread to extranodal sites, including the bone
marrow and central nervous system (8). Because of the more
complicated clinical course and gene rearrangements, the standard chemotherapy used for DLBLC or BL is ineffective (8).
The survival rate for these lymphomas has been reported to be
about 4 months, shorter than for DLBCL, BL, and doublehit lymphoma (8). One of the challenges is how to recognize
these lymphomas and order the appropriate molecular studies
so that aggressive treatment may be started. We are routinely
ordering molecular studies to detect BCL-2, BCL-6, and c-MYC
rearrangements on any B-cell lymphoma with features intermediate between DLBCL and BL, any lymphoma with a Ki-67
proliferation index >90%, and any DLBCL that has recurred
and is refractory to therapy.
b
c
Figure 3. Fluorescence in situ hybridization showing (a) BCL-2, (b) BCL-6, and (c) c-MYC gene rearrangements as a break-apart probe with
two separate signals (red and green). A normal cell, for comparison, has the red and green signals connected.
126
Baylor University Medical Center Proceedings
Volume 27, Number 2
1.
2.
3.
4.
Carbone A, Gloghini A, Aiello A, Testi A, Cabras A. B-cell lymphomas
with features intermediate between distinct pathologic entities. From
pathogenesis to pathology. Hum Pathol 2010;41(5):621–631.
Aukema SM, Siebert R, Schuuring E, van Imhoff GW, Kluin-Nelemans
HC, Boerma EJ, Kluin PM. Double-hit B-cell lymphomas. Blood
2011;117(8):2319–2331.
Tomita N, Tokunaka M, Nakamura N, Takeuchi K, Koike J, Motomura
S, Miyamoto K, Kikuchi A, Hyo R, Yakushijin Y, Masaki Y, Fujii S,
Hayashi T, Ishigatsubo Y, Miura I. Clinicopathological features of lymphoma/leukemia patients carrying both BCL2 and MYC translocations.
Haematologica 2009;94(7):935–943.
Snuderl M, Kolman OK, Chen YB, Hsu JJ, Ackerman AM, Dal Cin P,
Ferry JA, Harris NL, Hasserjian RP, Zukerberg LR, Abramson JS, Hochberg EP, Lee H, Lee AI, Toomey CE, Sohani AR. B-cell lymphomas with
5.
6.
7.
8.
concurrent IGH-BCL2 and MYC rearrangements are aggressive neoplasms
with clinical and pathologic features distinct from Burkitt lymphoma and
diffuse large B-cell lymphoma. Am J Surg Pathol 2010;34(3):327–340.
de Jong D. Novel lymphoid neoplasms—the borderland between
diffuse large B-cell lymphoma and Burkitt’s lymphoma. Haematologica
2009;94(7):894–896.
Tomita N. BCL2 and MYC dual-hit lymphoma/leukemia. J Clin Exp
Hematop 2011;51(1):7–12.
Bacher U, Haferlach T, Alpermann T, Kern W, Schnittger S, Haferlach C.
Several lymphoma-specific genetic events in parallel can be found in mature B-cell neoplasms. Genes Chromosomes Cancer 2011;50(1):43–50.
Motlló C, Grau J, Juncà J, Ruiz N, Mate JL, Orna E, Navarro JT, Vives S,
Sancho JM, Esteban D, Granada I, Feliu E, Ribera JM, Millá F. Translocation (3;8)(q27;q24) in two cases of triple hit lymphoma. Cancer Genet
Cytogenet 2010;203(2):328–332.
Avocations
Photo © Amanullah Khan, MD, PhD. Dr. Khan (e-mail: aman1963@gmail.com) is an oncologist on the medical staff of Baylor Medical Center at McKinney.
April 2014
Triple-hit lymphoma
127
Small bowel intussusception causing a postoperative bowel
obstruction following laparoscopic low anterior resection in
an adult
Ahmad S. Hussain, MD, Rajalakshmi Warrier, MD, and Harry T. Papaconstantinou, MD
Adult intussusception usually presents with nonspecific symptoms
such as abdominal pain, bloating, nausea, vomiting, and a change
in bowel habits. Although postoperative intussusception has been
described in the pediatric population, there has been little description of it in the adult population. Postoperative intussusception has
unique challenges, as hydrostatic reduction may compromise bowel
anastomoses. Surgery is the universal treatment in these patients.
In adults, delay in diagnosis and definitive treatment may be a direct
result of common symptomatology between postoperative ileus and
intussusception. We present a case of an adult patient who underwent
laparoscopic low anterior resection for rectal cancer and developed a
small bowel intussusception causing obstruction requiring surgery. To
our knowledge, this is the first report of a small bowel intussusception masquerading as a postoperative ileus in an adult. While most
postoperative delayed bowel function is attributed to ileus, abscess
formation, or anastomotic leak, other uncommon etiologies, including intussusception, may occur and are important to include in the
differential diagnosis.
ntestinal intussusception is a relatively common abdominal
emergency in children; however, the incidence of intussusception in adults is rare and represents less than 5%
of all cases (1). In adults, transient asymptomatic enteric
intussusception is often noted on imaging and resolves spontaneously without any treatment (2). Complete and persistent
small bowel obstruction secondary to intussusception is less
common and is usually associated with a lead point lesion
(1). Adult intussusception usually presents with nonspecific
symptoms such as abdominal pain, bloating, nausea, vomiting, and a change in bowel habits. The abdominal exam is
often unremarkable, which contributes to an error or delay
in diagnosis. In children, initial attempts at reduction of the
intussusception with barium or air are often suggested, but
in adults surgery is the definitive treatment (3). Postoperative
intussusception has unique challenges, as hydrostatic reduction may compromise bowel anastomoses (4). In adults, delay
in diagnosis and definitive treatment may be a direct result
of common symptomatology between postoperative ileus
and intussusception. We present a case of an adult patient
I
128
who underwent laparoscopic low anterior resection for rectal
cancer and developed a small bowel intussusception causing
obstruction.
CASE REPORT
A 75-year-old man with chronic obstructive pulmonary
disease with bronchiectasis, coronary artery disease, and
hypertension underwent a single-incision laparoscopic low
anterior resection for recurrent rectal cancer. Nonsteroidal
antiinflammatory drugs were not utilized for pain control.
Postoperatively, he had persistent abdominal bloating, nausea, and emesis. Examination revealed a hypertympanic distended abdomen without signs of peritonitis. A computed
tomography (CT) scan of the abdomen and pelvis disclosed
a significantly dilated colon and small bowel with no signs of
obstruction. The bowel gas pattern was consistent with a postoperative ileus. The patient was initiated on total parenteral
nutrition. His condition thereafter progressively improved
with reduced abdominal distention. His bowel function eventually returned, an enteral diet was advanced as tolerated, and
he was sent home on postoperative day 20 on a regular diet.
Two days after discharge, the patient returned to the hospital
with obstipation, mild abdominal bloating, and emesis. CT
scan demonstrated an ileoileal intussusception causing a highgrade small bowel obstruction (Figure 1).
Nasogastric tube decompression and intravenous fluids
were initiated, and the patient continued to have signs of
bowel obstruction. At operation, he was found to have a
small bowel intussusception with fibrous bands holding
the telescoped bowel in place (Figure 2). He underwent
a small bowel resection and primary anastomosis without
From the Department of Surgery (Hussain, Warrier, Papaconstantinou), Section of
Colon and Rectal Surgery (Warrier), Scott & White Memorial Hospital and Clinic
and Texas A&M University System Health Science Center College of Medicine,
Temple, TX.
Corresponding author: Harry T. Papaconstantinou, MD, Associate Professor and
Interim Chairman, Department of Surgery, Scott & White Memorial Hospital and
Clinic, 2401 South 31st Street, Temple, TX 76508 (e-mail: hpapaconstantinou@
sw.org).
Proc (Bayl Univ Med Cent) 2014;27(2):128–130
DISCUSSION
Postoperative intussusception
in adults is an uncommon but
significant cause of small bowel
obstruction. Although it has been
previously described in the pediatric population (Table) (4–12),
to our knowledge this is the first
report of a small bowel intussusception masquerading as a postoperative ileus in an adult. Whereas
the time from surgery to diagnosis
appears to average about 1 week
c
d
for children, for our patient the
diagnosis was made 22 days after
surgery. This delay was likely due
to a lower index of suspicion in an
adult patient.
Diagnosis of postoperative
intussusception is difficult and is
often made by ultrasound, contrast
radiograph, or intraoperative findings in children (Table). In adults,
ileus is a far more common postopFigure 1 (a–d). CT scan at readmission showing a high-grade small bowel obstruction with a transition zone at a erative morbidity, presenting with
symptoms similar to obstruction,
region of ileoileal intussusception. Notice the telescoping of the small bowel (arrow) causing a bowel obstruction.
including nausea, vomiting, abdominal distention, and obstipadifficulty. Final pathology revealed benign mucosa with scattion (13). Further complicating the clinical picture in these
tered reactive lymphoid aggregates, vascular congestion,
patients is postoperative narcotics masking symptoms and
focal acute serositis, fibrous adhesions, and gross evidence
reliable physical exams (5) and the known negative effects
of small bowel telescoping. Postoperatively, total parenteral
of opiates on intestinal peristalsis (14). Postoperative ileus
nutrition was initiated to aid in nutrition, and his enteral
usually lasts on average 3 to 5 days, but can last much
diet was advanced. The patient regained normal bowel funclonger (15).
tion, and follow-up imaging showed no obstruction or other
In adults, CT scan is frequently used for postoperative evaluabnormality.
ation of patients with bowel obstruction and can be effective
in diagnosing postoperative ileus; however, given the transient
nature of intussusception, the CT scan must be obtained at
the time of discomfort, as spontaneous reduction may occur
between episodes. CT enteroclysis is a reliable diagnostic tool for
diagnosing small bowel intussusception (16) but has not been
documented as a reliable tool to reduce intussusception, with
recurrence of the intussusception described (17). CT evidence
of intussusception includes a target or sausage-shaped mass (18),
as shown in Figure 1. The transient nature of the pathology is
likely the reason we did not identify the intussusception earlier
in our patient.
Postoperative intussusception in children is frequently
treated by exploration and manual reduction (Table). We
chose to operate at the time of diagnosis and resect the intussuscepted bowel, as we were concerned about the etiology
and pathology of the lead point in this patient with a known
cancer. In adults, the lead point has a higher likelihood of
Figure 2. Intraoperative finding of the ileoileal intussusception. Notice the
being malignant. In our patient, the final pathology showed
proximal intussusceptum on the left telescoped circumferentially into the distal
intussuscipiens.
a benign lead point.
a
April 2014
b
Small bowel intussusception causing a postoperative bowel obstruction
129
Table. Literature review of postoperative intussusception
Author (reference)
Year
N
Age
Diagnostic modality
Time from surgery to diagnosis
Treatment
Ein et al (5)
1982
10
Children (2 m–15 y)
100% IO
8–39 days
70% MR
30% RR
West et al (6)
1988
36
Children (1 m–18 y)
86% XR
14% IO
Avg 8 days (1–24 days)
8% HR
81% MR
11% RR
Olcay et al (7)
1989
10
Children (3 m–10 y)
–
3–8 days
90% MR
10% RR
Velin et al (8)
1992
2
Children (6 m–12 m)
–
3–5 days
100% MR
Linke et al (4)
1998
5
Children
80% US
20% IO
5 days–3 months
100% MR
Kidd et al (9)
2000
5
Children
80% UGI SBFT
20% IO
Avg 7 days
100% MR
Niu et al (10)
2005
14
Children
7% US
93% IO
Avg 4 days (<10 days)
7% HR
86% MR
7% RR
Türkyilmaz et al (11)
2005
4
Children
–
Avg 2.5 days
100% MR
Bai et al (12)
2009
6
Children
83% US
17% IO
<7 days
100% MR
HR indicates hydrostatic reduction; IO, intraoperative; MR, manual reduction; RR, resection and reanastomosis; UGI SBFT, upper gastrointestinal study with small bowel follow-through;
US, ultrasound; XR, x-ray.
1.
2.
3.
4.
5.
6.
7.
8.
9.
130
Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G,
Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a
review. World J Gastroenterol 2009;15(4):407–411.
Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical
relevance. Radiol Clin North Am 2003;41(6):1137–1151.
Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, KohnehSharhi N, Lehur PA, Hamy A, Leborgne J, le Neel JC, Mirallie E. Clinical
spectrum and surgical approach of adult intussusceptions: a multicentric
study. Int J Colorectal Dis 2006;21(8):834–849.
Linke F, Eble F, Berger S. Postoperative intussusception in childhood.
Pediatr Surg Int 1998;14(3):175–177.
Ein SH, Ferguson JM. Intussusception—the forgotten postoperative obstruction. Arch Dis Child 1982;57(10):788–790.
West KW, Stephens B, Rescorla FJ, Vane DW, Grosfeld JL. Postoperative intussusception: experience with 36 cases in children. Surgery
1988;104(4):781–787.
Olcay I, Zorludemir U. Idiopathic postoperative intussusception. Z
Kinderchir 1989;44(2):86–87.
Velin P, Dupont D, Parizot P, Puig C, Grinda A. Postoperative intestinal
intussusception in children [article in French]. Ann Fr Anesth Reanim
1992;11(5):584–586.
Kidd J, Jackson R, Wagner CW, Smith SD. Intussusception following the
Ladd procedure. Arch Surg 2000;135(6):713–715.
10. Niu ZB, Hou Y, Wang CL. Postoperative intussusception in children: a
review of 14 cases. Chin Med Sci J 2005;20(4):265–267.
11. Türkyilmaz Z, Sönmez K, Demiroğullari B, Karabulut R, Ozen IO,
Moralioğlu S, Başaklar AC, Kale N. Postoperative intussusception in
children. Acta Chir Belg 2005;105(2):187–189.
12. Bai YZ, Chen H, Wang WL. A special type of postoperative intussusception: ileoileal intussusception after surgical reduction of ileocolic intussusception in infants and children. J Pediatr Surg 2009;44(4):755–758.
13. Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg 2013;17(5):962–972.
14. Pisano G, Manca A, Farris S, Tatti A, Atzeni J, Calò PG. Adult idiopathic intussusception: a case report and review of the literature. Chir
Ital 2009;61(2):223–229.
15. Carter S. The surgical team and outcomes management: focus on postoperative ileus. J Perianesth Nurs 2006;21(2A Suppl):S2–S6.
16. Moss A, Parrish FJ, Irving PM, Haines ML, Gibson PR. Quality, clinical
influence and tolerance of computed tomography enteroclysis in patients
with suspected small bowel disease. Intern Med J 2009;39(11):733–743.
17. Luckey P, Kemper J, Engelbrecht V, Mödder U. Idiopathic ileoileal intussusception in an adult with spontaneous reduction during enteroclysis: a
case report. Abdom Imaging 2000;25(1):48–50.
18. Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, Hertz M. Intussusception in adults: CT diagnosis. Clin Radiol 1998;53(1):53–57.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Fatal abdominal hemorrhage associated with gallbladder
perforation due to large gallstones
Luis R. Soto, MD, Harold R. Levine, MD, Scott A. Celinski, MD, and Joseph M. Guileyardo, MD
Gallbladder perforation is a relatively uncommon complication of acute
cholecystitis and may occur with or without gallstones. Prophylactic
cholecystectomy has been recommended for patients with very large
stones (>3 cm) due to an increased risk of gallbladder cancer. We present the case of a 68-year-old woman who died of hemorrhagic shock
following gallbladder perforation due to very large gallstones. This case
provides additional support for consideration of prophylactic cholecystectomy in patients with very large gallstones.
allbladder perforation (GP) is one of the most severe
complications of acute cholecystitis and is associated
with a mortality of up to 70% (1). It occurs in up
to 10% of patients with acute cholecystitis (2), but
GP in the absence of acute cholecystitis is rare. Nontraumatic
perforation results from ischemia and gangrene of the gallbladder wall and occurs most commonly in the fundus in cases
of acute cholecystitis (with or without stones). Such perforations are usually contained within the subhepatic space by the
omentum, duodenum, liver, or colon, and a localized abscess
may form. Less commonly, the gallbladder perforates into an
adjacent viscus, resulting in an enteric fistula and possible “gallstone ileus.” Rarely, the gallbladder perforates freely into the
peritoneal cavity, leading to generalized peritonitis (3). Hemorrhage associated with GP is even less common, but has been
reported with erosion into an adjacent artery (4). Although the
incidence of GP is similar in patients with stone-related versus
acalculous cholecystitis (5), the risk of GP due to very large
stones in the absence of acute cholecystitis is not known. Very
large gallstones have been associated with an increased risk of
gallbladder cancer, and we present the following case which
suggests that prevention of perforation may represent another
reason for consideration of prophylactic cholecystectomy in
patients with very large stones.
hours later it was 14.3 K/uL with 80% segmented neutrophils
and 12% band forms.
Her condition rapidly declined, and she required intubation
and red cell transfusions. Her admission aspartate aminotransferase was 7621 IU/L; alanine aminotransferase, 3475 IU/L;
direct bilirubin, 1.2 mg/dL; total bilirubin, 2.9 mg/dL; and
lactic acid, 5.8 mmol/L. Computed tomography (CT) revealed
a large calcified multilayered stone within a distended gallbladder in conjunction with a large complex fluid collection around
the gallbladder with extension into the liver and right paracolic
gutter (Figure 1). Radiologic interpretation included possible
liver mass versus abscess with GP.
On the day of admission, a cholecystostomy tube was
placed, and the hepatic artery was embolized with Gelfoam.
Subsequently, the patient’s hemoglobin stabilized, but she
developed hepatic failure with progressive jaundice and coagulopathy, followed by irreversible multisystem organ failure,
and died.
CASE STUDY
A 68-year-old woman was admitted to Baylor University
Medical Center at Dallas with right upper-quadrant abdominal
pain. Her admission hemoglobin fell from 11.3 to 6.1 g/dL
over several hours. Her initial white blood cell count was 17.4
K/uL with 93% segmented neutrophils (machine count), and
From the Departments of Pathology (Soto, Guileyardo), Radiology (Levine), and
Surgery (Celinski), Baylor University Medical Center at Dallas.
Corresponding author: Joseph M. Guileyardo, MD, Department of Pathology,
Baylor University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX
75246 (e-mail: guileyardo@sbcglobal.net).
G
Proc (Bayl Univ Med Cent) 2014;27(2):131–132
Figure 1. Coronal reformatted CT image demonstrates lamellated gallstone (red
arrow) and inflammatory changes in the gallbladder fossa with “biloma” versus
hemorrhage in the right hepatic lobe (blue circle).
131
Figure 2. Cross-section of the liver through the gallbladder wall and bed. A 0.5
cm transmural perforation extends as a necrotic fistula track into a large hematoma within the right lobe of the liver. Multifocal areas of yellow parenchymal
necrosis are also evident.
At necropsy the gallbladder contained a cholecystostomy
drain. The gallbladder was distended by two large gallstones,
each measuring 4.5 cm in diameter. The stones tightly conformed
to each other and completely filled the lumen, forming a single
mass measuring 8.0 cm in length. The gallbladder wall was
diffusely thin with an average thickness of 0.2 cm. There was a
0.5 × 1.5 cm transmural defect in the anterior wall of the gallbladder with a necrotic fistula track extending into a 10 cm hematoma in the right lobe of the liver (Figure 2), which weighed
1800 g. There were multifocal areas of necrosis throughout both
lobes. The intrahepatic hematoma was contiguous with subcapsular and extracapsular hematomas over the right lobe.
Microscopically, acute inflammatory cells were present near
the transmural disruption, but generalized acute cholecystitis
was absent. The common bile duct was not dilated or obstructed,
and it drained freely through the ampulla. Incidental necropsy
findings included a small renal cell carcinoma of the right kidney and moderate hypertensive and diabetic nephropathy. The
patient’s body mass index was 25.8 kg/m².
DISCUSSION
Although late operative intervention is associated with
increased morbidity, mortality, intensive care unit admissions,
and prolonged hospitalization, GP is rarely diagnosed pre-
132
operatively (1). There is significant clinical overlap between
acute cholecystitis with and without perforation, but findings
that suggest GP are a sudden decrease in pain intensity and
“toxic” signs in a rapidly declining patient (5, 6). Radiologic
evaluation for suspected GP often employs ultrasound initially
with subsequent CT, but no radiographic finding is absolutely pathognomonic of GP. The characteristic “hole-sign” is
rarely seen on ultrasound; however, findings of acute cholecystitis with indirect signs of complex free fluid, gallbladder
fossa hematoma, and intrahepatic hemorrhage should suggest perforation (7). Most patients with gallstones remain
asymptomatic; however, prophylactic cholecystectomy has
been recommended in patients with large gallstones due to an
increased risk for cancer (8). Lowenfels et al found the relative
risk of gallbladder cancer in patients with gallstones ≥3 cm
to be 9 times greater than in those with stones <1 cm (9). We
believe this case provides additional support for consideration
of prophylactic cholecystectomy in patients with very large
stones, since mechanical pressure by such stones probably led
to focal transmural necrosis and perforation of the gallbladder
wall in this patient.
1.
2.
3.
4.
5.
6.
7.
8.
9.
Stefanidis D, Sirinek KR, Bingener J. Gallbladder perforation: risk factors
and outcome. J Surg Res 2006;131(2):204–208.
Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol
2006;12(48):7832–7836.
Niemeier OW. Acute free perforation of the gallbladder. Ann Surg
1934;99(6): 922–924.
Ben-Ishay O, Farraj M, Shmulevsky P, Person B, Kluger YS. Gallbladder
ulcer erosion into the cystic artery: a rare cause of upper gastro-intestinal
bleeding: case report. World J Emerg Surg 2010;5:8.
Tsai MJ, Chen JD, Tiu CM, Chou YH, Hu SC, Chang CY. Can acute
cholecystitis with gallbladder perforation be detected preoperatively by
computed tomography in ED? Correlation with clinical data and computed tomography features. Am J Emerg Med 2009;27(5):574–581.
Chen JJ, Lin HH, Chiu CT, Lin DY. Gallbladder perforation with intrahepatic abscess formation. J Clin Ultrasound 1990;18(1):43–45.
Sood BP, Kalra N, Gupta S, Sidhu R, Gulati M, Khandelwal N, Suri S.
Role of sonography in the diagnosis of gallbladder perforation. J Clin
Ultrasound 2002;30(5):270–274.
Duncan CB, Riall TS. Evidence-based current surgical practice: calculous
gallbladder disease. J Gastrointest Surg 2012;16(11):2011–2025.
Lowenfels AB, Walker AM, Althaus DP, Townsend G, Domellöf L. Gallstone growth, size, and risk of gallbladder cancer: an interracial study. Int
J Epidemiol 1989;18(1):50–54.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Methemoglobinemia precipitated by benzocaine used during
intubation
Aasim Afzal, MD, Ruth Collazo, MD, Andrew Z. Fenves, MD, and John Schwartz, MD
Methemoglobinemia is a rare cause of tissue hypoxia that can quickly become fatal without immediate recognition and prompt treatment. It refers
to an increase in methemoglobin in the red blood cells, which can be due
to genetic deficiency of the enzymes responsible for reducing hemoglobin
or can develop after exposure to oxidizing agents or xenobiotics. Local
anesthetics, particularly benzocaine, have long been implicated in the
formation of methemoglobin. Benzocaine is used for teething pain as well
as before invasive procedures such as intubation and transesophageal
echocardiogram. In this case report, we describe a patient with acute
appendicitis who developed severe methemoglobinemia following use of
benzocaine during an emergent intubation. Our objective is to increase
awareness of this rare but potentially fatal complication associated with
the use of this anesthetic.
ethemoglobin is found in small quantities in red
blood cells (RBCs) in the normal physiologic state.
The reductive capacity of the RBCs can be compromised when exposed to overwhelming oxidative
stress. Typical symptoms of methemoglobinemia range from
confusion and dizziness to arrhythmias, coma, and death.
Methylene blue is the recommended treatment for severe cases
of methemoglobinemia. However, for this treatment to be effective, it must be given immediately, which requires prompt
recognition of the condition. We describe a patient who developed severe methemoglobinemia from benzocaine, which was
used during intubation in preparation for surgery. As of 2011,
the Food and Drug Administration had reported 319 cases of
methemoglobinemia related to benzocaine, including seven
cases of death and 32 cases categorized as life-threatening (1).
M
CASE DESCRIPTION
A 56-year-old white woman with known gluten and lactose
intolerance was admitted with severe right-sided abdominal pain,
nausea, vomiting, and fever. Appendicitis was diagnosed and an
uneventful laparoscopic appendectomy was performed. On the
second postoperative day, the patient became hypotensive and
tachypneic and developed bilateral pleural effusions followed
by profound respiratory failure requiring emergent intubation,
which was traumatic and caused significant damage to the oral
mucosa. Benzocaine was used during the intubation procedure.
Proc (Bayl Univ Med Cent) 2014;27(2):133–135
The patient developed significant cyanosis immediately after
intubation. Blood drawn for arterial blood gas (ABG) tests was
chocolate brown. Methemoglobinemia was diagnosed, and methylene blue was promptly administered. Prior to administration
of methylene blue, the methemoglobin concentration was 45%,
with an increased anion gap metabolic acidosis (Tables 1 and 2).
The cyanosis and methemoglobinemia resolved over 2.5 hours
following methylene blue administration. The patient was then
taken to the operating room for emergent exploratory laparotomy.
A small amount of murky fluid was collected in the abdomen
and sent for culture. No evidence of intestinal leak or bleeding
was found.
Her postoperative course was complicated by multiorgan
failure with respiratory and hepatic failure, lactic acidosis,
rhabdomyolysis, and hemodynamic instability requiring norepinephrine. Continued hypotension led to acute kidney injury
requiring continuous veno-venous hemodialysis. Her pulmonary function continued to worsen, and she was switched to
high-frequency oscillator ventilation to maintain oxygenation.
Chest tubes were also placed for bilateral pulmonary effusions. She developed sepsis and was placed on broad-spectrum
antibiotics. On hospital day 7, the patient was weaned from
Table 1. Arterial blood gas results after emergent intubation
Test
Result
pH
7.32
Partial pressure of carbon dioxide (mm Hg)
25
Partial pressure of oxygen (mm Hg)
116.7
Bicarbonate (mEq/L)
12.7
Carbon monoxide (%)
0
Methemoglobin (%)
44.9%
Oxygen (%)
54.6%
From the Department of Internal Medicine, Baylor University Medical Center
at Dallas (Afzal, Collazo, Schwartz); and the Massachusetts General Hospital,
Harvard Medical School, Boston Massachusetts (Fenves).
Corresponding author: Aasim Afzal, MD, 3600 Gaston Avenue, Suite 1155,
Dallas, TX 75246 (e-mail: Aasim.afzal1@baylorhealth.edu).
133
Table 2. Laboratory workup done at admission
Blood test
Results
White blood cells (K/μL)
13.8
Hemoglobin (g/dL)
14.9
Hematocrit (%)
40.9
Platelets (per μl)
48
Sodium (mEq/L)
138
Potassium (mEq/L)
4.4
Chloride (mEq/L)
98
Bicarbonate (mEq/L)
13
Blood urea nitrogen (mg/dL)
14
Creatinine (mg/dL)
1.4
Anion gap (mEq/L)
27
Glucose (mg/dL)
32
vasopressors, but she remained unresponsive and had severely
impaired neurologic function. An electroencephalogram confirmed anoxic brain injury, and the patient died.
DISCUSSION
Red blood cells are under constant oxidative stress by being
exposed to drugs and oxygen, as well as byproducts of intracellular metabolism. In a normal physiologic state, there is roughly
1% methemoglobin in the RBCs. This amount is kept in check
by reducing enzymes within the erythrocytes (2, 3).
The human body has three main mechanisms for reducing methemoglobin. The nicotinamide adenine dinucleotide
(NADH) pathway, catalyzed by cytochrome b5 reductase, is the
most important. It is responsible for reduction of up to 95% of the
methemoglobin (4). This mechanism efficiently reduces the ferric
atom in methemoglobin by transferring an additional electron
from NADH to methemoglobin. Another reductive mechanism
utilizes G6P dehydrogenase and its capability to produce nicotine
adenine dinucleotide phosphate (NADPH), which can lead to
the reduction of methemoglobin (3, 4) (Figure 1). A third minor
and nonenzymatic pathway that works to reduce methemoglobin
involves reduced glutathione, ascorbic acid, and cysteine.
Methemoglobin becomes clinically relevant when the oxidative burden overwhelms the cellular capability for reduction.
Patients usually become symptomatic when the level of methemoglobin exceeds 15%. Symptoms tend to positively correlate
with the methemoglobin level.
Causes of methemoglobinemia can be divided into inherited
defects of the oxidizing enzymes and acquired forms. The most
common inherited forms are autosomal recessive conditions.
Patients have decreased levels of NADH-cytochrome-b5 reductase. There is no reason to suspect that our patient had any
genetic susceptibility to develop this condition.
A myriad of oxidizing compounds have been identified that
can quickly overwhelm the reducing capabilities of the RBC.
The list includes industrial dyes, nitrates, chlorates, herbicides,
antibiotics such as dapsone and sulfonamides, as well as local
anesthetics, notably benzocaine and prilocaine (2).
The diagnosis of methemoglobinemia is based on clinical
symptoms and requires a high index of suspicion in patients
with a known exposure. Patients will present with cyanosis out
of proportion to the respiratory status, in the presence of normal
arterial oxygen content (partial pressure of oxygen > 60 mm
Hg) (2). No symptomatic improvement is seen with oxygen
administration. The arterial blood draw is chocolate brown due
to the oxidized hemoglobin. ABG will reveal an oxygen saturation gap (2). Methemoglobinemia should be suspected when
the oxygen saturation from the ABG is higher than the oxygen
saturation reported by pulse oximetry. A saturation gap of over
5% strongly suggests methemoglobinemia (5). The differential
diagnosis of a saturation gap includes carbon monoxide poisoning as well as sulfhemoglobinemia (2).
A pulse oximeter emits monochromatic light at wavelengths
of 660 (red) and 940 (infrared) nm. As light travels through the
tissues, the pulsation of the arteries converts this light into an
alternating pattern. This alternating light reaches a photodetector
and is amplified. When light travels through a nonpulsatile tissue
such as a vein, it is not changed to alternating and therefore not
amplified by the photodetector. This allows pulse oximeters to
detect only the hemoglobin in arteries (Figure 2).
Different hemoglobin species absorb light differently at
both wavelengths, and the ratio of red to infrared absorption
is calculated. When the two major hemoglobin molecules are
oxygenated hemoglobin (oxyhemoglobin) and nonoxygenated
hemoglobin (reduced hemoglobin), the ratio of absorbance
at these two wavelengths can be converted to oxygen saturation. Methemoglobin absorbs light equally at these two wavelengths and therefore always has a ratio of absorption of 1, which
Figure 1. The mechanism of methemoglobin reduction including the methylene blue rescue pathway.
134
Baylor University Medical Center Proceedings
Volume 27, Number 2
Figure 2. Hemoglobin extinction curves. Pulse oximetry uses the 660 and 940
nm wavelengths. As carboxyhemoglobin and oxyhemoglobin absorb equally at
660 nm, they both read the same oxygen saturation on a conventional pulse
oximeter. From Huford W, Kratz A (2). Copyright © 2004 Massachusetts Medical
Society. Reprinted with permission from Massachusetts Medical Society.
equates to an oxygen saturation of 85% (5). Therefore, the pulse
oximeter will display an oxygen saturation of approximately
85% regardless of the patient’s real oxygenation status.
Newer oximeters called co-oximeters measure absorption at
multiple wavelengths, which circumvents the issue seen with
traditional pulse oximeters. Co-oximeters will determine the
percentage of hemoglobin converted to methemoglobin and
carboxyhemoglobin and also will provide an accurate estimate
of the true oxygen saturation state of hemoglobin. However,
these co-oximeters are not widely used (5).
Most cases of methemoglobinemia will resolve within 24
to 36 hours. In severe cases, particularly when the methemoglobin blood level is above 30%, prompt treatment with methylene blue is advised. Methylene blue is quickly reduced by
NADPH methemoglobin reductase to leukomethylene blue,
which then reduces methemoglobin to hemoglobin. This is
called the methylene blue rescue pathway. This rescue pathway
relies on an intact glucose-6-phosphate dehydrogenase (G6PD)
system. In the rare event that the patient’s status worsens after
April 2014
methylene blue administration, G6PD deficiency should be
strongly suspected.
Benzocaine is still a widely used anesthetic. There are several
different formulations, the spray form being the most commonly used. Benzocaine sprays are marketed under different
brand names such as Hurricaine, Cetacaine, Exactacain, and
Topex (1). The benzocaine concentration in these formulations
ranges from 14% to 20%. The benzocaine dosage that can produce methemoglobinemia in adults has been estimated to be
approximately 300 mg, with initial onset of symptoms within
20 to 60 minutes.
The patient presented was exposed to benzocaine during
the second emergent intubation. It is unknown whether the
anesthetic utilized in the first intubation included benzocaine.
However, the benzocaine was administered to a mucosa that
was likely traumatized during the first intubation, potentially increasing its absorption and causing a greater oxidative
burden.
This patient likely had a gastrointestinal perforation from
her prior episode of acute appendicitis. After the second intubation, it was difficult to wean her off the ventilator. ABG analysis
showed her methemoglobin level rising to 45%. The methemoglobin level quickly declined over a period of 2.5 hours after
receiving methylene blue. Unfortunately, the patient developed
significant hemodynamic instability likely due to multiple factors, ultimately developed multiorgan failure and anoxic brain
injury, and subsequently died.
1.
2.
3.
4.
5.
US Food and Drug Administration. FDA continues to receive reports
of a rare, but serious and potentially fatal adverse effect with the use of
benzocaine sprays for medical procedures [Safety announcement, April 7,
2011]. Available at http://www.fda.gov/Drugs/DrugSafety/ucm250040.
htm.
Hurford WE, Kratz A. Case 23-2004. A 50-year-old woman with low
oxygen saturation. N Engl J Med 2004;351(4):380–387.
Chung NY, Batra R, Itzkevitch M, Boruchov D, Baldauf M. Severe methemoglobinemia linked to gel-type topical benzocaine use: a case report.
J Emerg Med 2010;38(5):601–606.
Janssen WJ, Dhaliwal G, Collard HR, Saint S. Clinical problem-solving.
Why “why” matters. N Engl J Med 2004;351(23):2429–2434.
El-Husseini A, Azarov N. Is threshold for treatment of methemoglobinemia the same for all? A case report and literature review. Am J Emerg Med
2010;28(6):748.e5–748.e10.
Methemoglobinemia precipitated by benzocaine used during intubation
135
Where is that hemodialysis catheter (superior vena cava
or aorta)? A case of intraarterial catheter placement
Valerie Tan, MD, and John C. Schwartz, MD
We present a case of a previously unrecognized intraarterial placement of
a central venous catheter (CVC)—in this case, a large-bore hemodialysis
catheter in an 82-year-old woman. CVC insertions have become a common practice in hospitals due to a variety of indications, and tunneled
CVCs still remain an important form of access in patients with end-stage
renal disease. Intraarterial puncture is a common complication during
CVC insertion, while intraarterial (mis)placement is fairly uncommon and
if unrecognized can lead to significant morbidity and mortality.
rterial puncture during central venous catheter (CVC)
insertion is one of the most common complications
related to CVC insertion, with an incidence varying
from 1% to 11%. Catheter misplacement outside of the
correct position (ideally a large central vein such as the superior
or inferior vena cava or the right atrium) has been described
with tips lying in aberrant sites in almost every possible anatomical position, including the arterial system, mediastinum,
pleura, and pericardium. CVC misplacement depends on several
factors such as site and technique of insertion, operator experience, number of needle passes, presence of unknown vascular
or anatomic abnormalities, and patient body habitus and positioning (1, 2).
A
CASE REPORT
An 82-year-old black woman with recently diagnosed
end-stage renal disease requiring hemodialysis was referred
for further evaluation of her kidney disease. Her past medical history was significant for hypertension, hypothyroidism, and pulmonary hypertension. She initially presented to
an outside hospital 1 month earlier for progressive edema,
nephrotic-range proteinuria, marked hypoalbuminemia, and
severe renal failure. Pertinent workup at the outside hospital
revealed urinary protein excretion of 10 g/day and a serum
albumin level of 0.9 g/dL. Routine serologies and urine and
serum protein electrophoreses were normal. The specific cause
of her end-stage renal disease was not known, as the patient
refused to undergo a kidney biopsy. Her renal function rapidly
deteriorated, and hemodialysis was started. She was placed on
prophylactic anticoagulation because of her severe nephrotic
syndrome.
136
Hemodialysis was performed using a central venous hemodialysis catheter. She was subsequently discharged to continue
maintenance hemodialysis at an outpatient hemodialysis unit.
Outpatient hemodialysis, however, was not tolerated due to
frequent episodes of intradialytic hypotension. She had several
catheter exchanges. The patient developed progressive anasarca
and dyspnea prompting transfer for management of renal disease and refractory volume overload.
Her admission vital signs included a heart rate of 86 beats
per minute; blood pressure, 103/57 mm Hg; respiratory rate,
18 breaths/min; and oxygen saturation, 96% on room air. She
was in no acute distress at rest. Neck veins were prominent.
Lung auscultation revealed decreased breath sounds at the bases.
Cardiovascular examination revealed a systolic murmur over the
right upper sternal border but no precordial heave. She had overt
anasarca with swelling to the level of the hips. A dual-lumen
dialysis catheter was located below the right clavicle.
Laboratory studies showed a hemoglobin of 12.5 g/dL;
hematocrit, 37.7%; white blood cell count, 9200/uL; platelets, 392,000/uL; sodium, 148 mEq/L; potassium, 5.2 mEq/L;
chloride, 111 mEq/L; bicarbonate, 27 mEq/L; blood urea nitrogen, 40 mg/dL; creatinine, 5.0 mg/dL; glucose, 106 mg/
dL; albumin, 1.2 g/dL; and calcium, 8.2 mg/dL. Coagulation
studies revealed a prothrombin time of 99.4 seconds with an
international normalized ratio of 10.6. Urinalysis was significant
for 3+ proteinuria, 2+ glucosuria, and 1+ blood with 15 to 30
red blood cells. A 24-hour urine collection revealed a creatinine
clearance of 4 mL/min and a urine protein excretion of 18 g/
day. A chest x-ray revealed small bilateral pleural effusions, and
the right internal jugular dialysis catheter tip was reported to be
in the superior vena cava (Figure 1). As part of the workup of
pulmonary hypertension, a CT scan with pulmonary embolus
protocol was done, which ruled out a pulmonary embolus. The
study, however, revealed the dialysis catheter to actually be in the
ascending aorta rather than the superior vena cava (Figure 2).
Because of the finding of arterial placement of the dialysis catheter, the vascular surgery service was consulted and
From the Division of Nephrology, Department of Internal Medicine, Baylor
University Medical Center at Dallas.
Corresponding author: Valerie Tan, MD, 3600 Gaston Avenue, Barnett Tower,
Suite 904, Dallas, TX 75246 (e-mail: Valerie.tan@baylorhealth.edu).
Proc (Bayl Univ Med Cent) 2014;27(2):136–138
Figure 1. A chest x-ray showing small bilateral pleural effusions. Based on this
image, the catheter tip was reported to be in the superior vena cava.
hemodialysis temporarily held. Blood was drawn from the
catheter and sent for blood gas analysis, which revealed pH
7.44, pCO2 38 mm Hg, and pO2 125 mm Hg, with an oxygen
saturation of 97%. This confirmed the intraarterial position
of the catheter. The patient’s coagulopathy was corrected. She
subsequently underwent surgical removal of the arterial dialysis
catheter with repair of the carotid artery at the catheter insertion site. A new tunneled dialysis catheter was placed in the left
internal jugular vein under ultrasound guidance with catheter
tip placement confirmed by fluoroscopy.
During the hospital course, a kidney biopsy was attempted
to determine the etiology of her nephrotic syndrome. The procedure was aborted due to technical difficulties. She was placed
empirically on steroids for treatment of suspected glomerulonephritis. Residual kidney function never recovered where
adequate volume management or solute clearance was possible.
Thrice weekly hemodialysis was resumed while she continued
steroids. Hemodialysis was initially tolerated with the help of
intradialytic albumin, but the patient did not tolerate it over the
succeeding sessions due to recurring hypotension. A right heart
catheterization was ultimately done to evaluate her pulmonary
hypertension. Results revealed mild pulmonary hypertension
and a very low cardiac output. A repeat 24-hour creatinine
clearance after 2 weeks of steroids revealed a clearance of 7 mL/
min. Due to her poor cardiac status, advanced age, and inability
to tolerate dialysis, the patient and family decided to pursue
comfort care and to stop dialysis.
Figure 2. A CT scan with pulmonary embolus protocol showing the dialysis
catheter to be in the ascending aorta.
DISCUSSION
Hemodialysis catheters are large-bore CVCs that have remained a frequent modality of both acute and chronic dialysis
vascular access in the United States. A large percentage (80%)
of patients initiating dialysis do so via a catheter, with some
continuing to chronically dialyze through it due to the inability
to obtain or unavailability of an adequate arteriovenous access.
Hemodialysis catheters are classified into two categories: acute
or nontunneled and chronic or tunneled catheters. Insertion of
these catheters follows the same principles of CVC insertion,
with the right internal jugular vein being the preferred insertion
site due to easier catheterization, a relatively straight path to the
superior vena cava and right atrium, high rates of cannulation
success, and low rates of central venous stenosis (3, 4).
As with CVC insertions, arterial puncture is a common
complication of hemodialysis catheters, and arterial puncture
can be recognized prior to insertion of the catheter by checking the color and pulsatility of the blood backflow. In certain
cases, however, such as shock, hypotension, or hypoxemia,
this check may be unreliable, and it may be difficult to distinguish between arterial and venous blood. In these cases, an
arterial blood gas or pressure transducer monitoring may be
used to detect misplacement (1). Use of ultrasound-guided
cannulation compared with the landmark (blind) method
has been proven to decrease the risk of procedural complications, including arterial puncture and misplacement, reduce
the number of multiple attempts, and reduce the number of
catheter placement failures (4–6).
April 2014
Where is that hemodialysis catheter (superior vena cava or aorta)? A case of intraarterial catheter placement
137
When choosing the internal jugular or subclavian veins for
CVCs, postprocedure films and fluoroscopy are useful in confirming catheter placement and tip location. These, however, are not
foolproof, as evidenced by this case, where admission chest x-ray
failed to recognize the arterial location of the catheter. In cases of
internal jugular vein CVCs, intraarterial misplacement may not be
apparent in routine x-rays when the CVC is in the ascending aorta
because of overlap of the superior vena cava and the aorta. Anatomic
vascular anomalies such as a right-sided aortic arch may also make
radiographic recognition difficult. Fluoroscopic confirmation after
a tunneled hemodialysis catheter insertion has the same limitation
unless contrast is used to see actual blood flow (1).
Upon recognition of an intraarterial placement of a CVC,
it should be left in place until further advice and management
from surgery or interventional radiology is obtained. Rare but
life-threatening complications include hematoma formation
enough to compromise airway, hemorrhage with or without
hemothorax, cerebrovascular accidents from thromboembolism,
Horner’s syndrome, pseudoaneurysm or arteriovenous fistula
formation, arterial occlusion, and even death (2, 3, 7). Removal
of large-bore hemodialysis catheters requires careful consideration and extensive operator experience. Treatment options vary
from extrinsic compression if the artery is accessible (although
this risks brain ischemia), to surgical removal of the catheter
with repair of the arterial defect, to endovascular repairs with or
without stent placement (1). Due to the associated significant
morbidity and mortality of CVC arterial puncture and catheter
misplacement, prevention is key, and the best preventive strategies are adequate patient and operator preparation and use of
real-time ultrasound-guided cannulation.
1.
2.
3.
4.
5.
6.
7.
Gibson F, Bodenham A. Misplaced central venous catheters: applied
anatomy and practical management. Br J Anaesth 2013;110(3):333–346.
Kusminsky RE. Complications of central venous catheterization. J Am
Coll Surg 2007;204(4):681–696.
Choi YS, Park JY, Kwak YL, Lee JW. Inadvertent arterial insertion of
a central venous catheter: delayed recognition with abrupt changes in
pressure waveform during surgery—a case report. Korean J Anesthesiol
2011;60(1):47–51.
Schwab SJ, Beathard G. The hemodialysis catheter conundrum: hate living
with them, but can’t live without them. Kidney Int 1999;56(1):1–17.
Vats HS. Complications of catheters: tunneled and nontunneled. Adv
Chronic Kidney Dis 2012;19(3):188–194.
Aydin Z, Gursu M, Uzun S, Karadag S, Tatli E, Sumnu A, Ozturk S,
Kazancioglu R. Placement of hemodialysis catheters with a technical, functional, and anatomical viewpoint. Int J Nephrol 2012;2012:302826.
Göksel OS, El H, Onalan A, Alpagut U. Successful removal of a malpositioned hemodialysis catheter into the aortic arch. J Vasc Access
2012;13(4):543.
Avocations
Spring flowers. Photos copyright © Rolando Solis, MD. Dr. Solis is an interventional cardiologist practicing at Baylor Medical Center at Garland and the Heart Hospital
Baylor Plano (e-mail: rmsolis@me.com).
138
Baylor University Medical Center Proceedings
Volume 27, Number 2
Renal failure due to Capnocytophaga canimorsus generalized
Shwartzman reaction from a dog bite (DF-2 nephropathy)
Valerie Tan, MD, and John C. Schwartz, MD
We report a case of a 54-year-old man who developed gram-negative
sepsis with multiorgan failure and generalized Shwartzman reaction after
sustaining a dog bite. The causative organism was the fastidious gramnegative rod Capnocytophaga canimorsus, which is a commensal organism found in the oral flora of dogs and cats. More than 30 years after it
was first described and despite technological advances in identification
techniques, proper identification of this organism remains a challenge. In
light of the increase in pet ownership as well as the increase in the different immunocompromised populations of the 21st century, we decided to
revisit the case and reignite awareness of physicians caring for patients
with recent dog or cat bites presenting with fulminant sepsis.
apnocytophaga canimorsus is a fastidious microaerophilic, non–spore-forming gram-negative rod that is
1 to 3 μm long, is oxidase and catalase positive, and is
capable of gliding motility under the microscope. The
first strain was received by the Centers for Disease Control and
Prevention (CDC) in 1961 and was assigned the name CDC
Group DF-2 (dysgonic fermenter-2). It first came to be recognized as a pathogen in 1976 when Bobo and Newton reported
a case of an unidentified gram-negative rod isolated in the blood
and cerebrospinal fluid of their patient with septicemia and
meningitis who sustained a dog bite. It was not until 1989
when Brenner et al studied 150 strains of the organism sent to
the CDC that the formal name of Capnocytophaga canimorsus
was proposed (1).
C
CASE REPORT
A 54-year-old white man with previously good health was
admitted with septic shock. A dog had bitten his left thumb
3 days earlier. The wound was cleaned and nothing unusual
happened over the next 2 days. Fever, chills, and myalgias then
appeared. He was admitted through the emergency room with
dyspnea and changes in skin color.
His temperature was 103.4°F; blood pressure, 70/45 mm
Hg; respiratory rate, 30 breaths/min; and heart rate, 120 beats/
min. He had diffuse dermal purpura with ecchymoses as well
as distal gangrene of the fingers, toes, ear tips, and nose. The
puncture site on the left thumb had some surrounding necrosis. He was emergently intubated and received vigorous fluids
Proc (Bayl Univ Med Cent) 2014;27(2):139–140
Table 1. Admitting laboratory results
Day 1
White blood cells (K/uL)
Neutrophils (%)
41
Bands (%)
43
Metamyelocytes (%)
3
Platelet count (K/uL)
115
Prothrombin time (seconds)
50
Partial thromboplastin time (seconds)
Day 2
3.9
15
>200
Blood urea nitrogen (mg/dL)
20
38
Creatinine (mg/dL)
1.5
4.3
Lactate dehydrogenase (IU/L)
14,000
and dopamine. He was started on ceftriaxone and tobramycin.
Penicillin was later added.
Admission laboratory data (Table 1) revealed leukopenia
with a left shift, worsening thrombocytopenia, prolonged coagulation times, worsening renal function tests, and a marked
elevation in lactate dehydrogenase level. Bacillary organisms
were seen on peripheral blood smear.
He rapidly developed multiorgan failure, including disseminated sepsis with shock, respiratory failure with acute respiratory
distress syndrome, disseminated intravascular coagulation, and
oligoanuric acute renal failure. He received anti–lipid A monoclonal antibody (Centoxin). Ampicillin-sulbactam was added
to his regimen. His hemodynamics stabilized, but he developed
worsening intradermal hemorrhage with diffuse distal blistering,
with toes and fingertips becoming necrotic.
Initial blood cultures and repeat blood cultures were negative at day 4, even though persistent bacteria were seen on
his peripheral blood smear. Blood cultures at day 8 revealed a
slow-growing gram-negative rod. The specimen was sent to the
State Laboratory of Hygiene for definitive identification. Blood
From the Division of Nephrology, Department of Internal Medicine, Baylor
University Medical Center at Dallas.
Corresponding author: Valerie Tan, MD, 3600 Gaston Avenue, Barnett Tower,
Suite 904, Dallas, TX 75246 (e-mail: Valerie.tan@baylorhealth.edu).
139
Table 2. Renal function tests over time
Day 4 Day 14 Day 44 Day 55 Day 79
Blood urea nitrogen (mg/dL)
96
129
50
52
28
Creatinine (mg/dL)
8.0
10.5
5.4
5.3
2.1
cultures, approximately a month following admission, were
confirmed as Capnocytophaga canimorsus (DF-2).
Hemodialysis was initiated on day 4. The patient remained
virtually anuric. Residual renal function by creatinine clearance
was zero. He underwent dialysis 4 times per week. He was extremely catabolic, with a urea nitrogen generation rate of 20 g
per day. He was treated with oral and parenteral nutrition to
achieve a protein intake of 120 g per day (1.8 g/kg per day). He
was extubated on day 6. His blood pressure was stable off dopamine at that time. Antibiotics were continued for 2 weeks.
A mercaptoacetyltriglycine (MAG3) scan on day 20 revealed
clear evidence of radionuclide uptake without renal excretion,
suggesting reversible renal disease. Hemodialysis was decreased to
3 times per week. He underwent amputation of all 10 toes on day
24, with split-thickness skin grafting to both arms and legs at the
same time. He underwent repeat skin grafting 1 week later.
Residual renal function measured by creatinine clearance
was 2 mL/min on day 31. At that time, his urine output was
rising. He underwent his last hemodialysis treatment on day
40 after 21 treatments. Residual renal function measured by
creatinine clearance on day 44 was 7 mL/min. The patient was
subsequently discharged on day 48. He experienced continued
improvement in his renal function in the outpatient setting over
the next month (Table 2). Dialysis was never again needed.
DISCUSSION
Capnocytophaga canimorsus (formerly CDC Group DF-2) has
been rarely but regularly isolated from dog or cat bite infections
since its discovery in 1976. It is a commensal organism of the
canine oral flora and can be isolated from mouths of healthy dogs
and cats (2, 3). Zoonotic infectious manifestations range from local
cellulitis to fulminant gram-negative sepsis with multiorgan failure,
disseminated intravascular coagulation, and peripheral gangrene.
The portal of entry is usually the skin after having been bitten by
a dog or cat, but there have also been reports of infection from
ordinary exposure, licks, and scratches (3–7). The organism spreads
hematogenously to the meninges, endocardium, and synovium,
causing infection in those sites. The reported mortality rate is 30%
to 36%, and implicated risk factors are a history of splenectomy,
alcohol abuse, lung disease, and an immunocompromised state.
Infection, however, is not limited to that population, with as many
as 40% of cases having no obvious risk factor (2, 4, 5).
Association of a generalized Shwartzman reaction after a dog
bite was first reported in 1970, when Capnocytophaga canimorsus
was still unrecognized as a significant pathogen in dog bites. The
generalized Shwartzman reaction has been well described in fulminant gram-negative septicemia in pregnancy and meningococcemia. It is characterized by thrombohemorrhagic skin necrosis and
140
disseminated intravascular coagulation from endotoxins causing
deposition of fibrin thrombi in small vessels (mainly renal glomerular capillaries and adrenals), which is considered the hallmark
of the disease. The deposition of fibrin thrombi usually results in
varying degrees of necrosis and hemorrhage, which accounts for the
renal failure from bilateral renal cortical necrosis and peripheral gangrene associated with the generalized Shwartzman reaction (8, 9).
Subsequent case reports of Capnocytophaga canimorsus infections,
including our case, made it clear, however, that infection with the
organism can be associated with renal failure apart from or as part
of the full spectrum of the generalized Shwartzman reaction (4–6,
10, 11). For this reason, we would like to coin the term DF-2
nephropathy to describe reversible or nonreversible oligoanuric
renal failure in Capnocytophaga canimorsus (DF-2) sepsis with or
without association with a generalized Shwartzman reaction.
Capnocytophaga canimorsus is susceptible to penicillins, imipenem, erythromycin, vancomycin, clindamycin, third-generation
cephalosporins, chloramphenicol, rifampicin, doxycycline, and
fluoroquinolones. It is resistant to aztreonam and aminoglycosides
and has variable resistance to trimethoprim-sulfamethoxazole. As
such, penicillin had long been the initial empiric drug of choice. A
recent report of a beta-lactamase–resistant strain has made a thirdgeneration cephalosporin or combination beta-lactam antibiotic/
beta-lactamase inhibitor better empiric coverage. The organism
can be identified by conventional microbiologic identification,
polymerase chain reaction, or DNA sequencing (1, 7, 12, 13).
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Brenner DJ, Hollis DG, Fanning GR, Weaver RE. Capnocytophaga canimorsus sp. nov. (formerly CDC group DF-2), a cause of septicemia following dog bite, and C. cynodegmi sp. nov., a cause of localized wound
infection following dog bite. J Clin Microbiol 1989;27(2):231–235.
Mally M, Shin H, Paroz C, Landmann R, Cornelis GR. Capnocytophaga
canimorsus: a human pathogen feeding at the surface of epithelial cells
and phagocytes. PLoS Pathog 2008;4(9):e1000164.
Carpenter PD, Heppner BT, Gnann JW Jr. DF-2 bacteremia following
cat bites. Report of two cases. Am J Med 1987;82(3 Spec No):621–623.
Butler T, Weaver RE, Ramani TK, Uyeda CT, Bobo RA, Ryu JS, Kohler
RB. Unidentified gram-negative rod infection. A new disease of man. Ann
Intern Med 1977;86(1):1–5.
Kalb R, Kaplan MH, Tenenbaum MJ, Joachim GR, Samuels S. Cutaneous
infection at dog bite wounds associated with fulminant DF-2 septicemia.
Am J Med 1985;78(4):687–690.
Zeier MG. A lick may be as bad as a bite: irreversible acute renal failure.
Nephrol Dial Transplant 2000;15(11):1883–1884.
Low SC, Greenwood JE. Capnocytophaga canimorsus: infection, septicaemia,
recovery and reconstruction. J Med Microbiol 2008;57(Pt 7):901–903.
Meyers BR, Hirschman SZ, Sloan W. Generalized Shwartzman reaction in
man after a dog bite. Consumption coagulopathy, symmetrical peripheral gangrene, and renal cortical necrosis. Ann Intern Med 1970;73(3):433–438.
Hjort P, Rapaport S. The Shwartzman reaction: pathogenetic mechanisms
and clinical manifestations. Annu Rev Med 1965;16:135–168.
Findling JW, Pohlmann GP, Rose HD. Fulminant gram-negative bacillemia (DF-2) following a dog bite in an asplenic woman. Am J Med
1980;68(1):154–156.
Hinrichs JH, Dunkelberg WE. DF-2 septicemia after splenectomy: epidemiology and immunologic response. South Med J 1980;73(12):1638–1640.
Velculescu V, Velji AM. Capnocytophaga canimorsus (DF-2) infection: a
continuing challenge for clinicians and microbiologists. Microb Ecol Health
Dis 1998;10(3–4):155–157.
Janda JM, Graves MH, Lindquist D, Probert WS. Diagnosing Capnocytophaga canimorsus infections. Emerg Infect Dis 2006;12(2):340–342.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Imaging manifestations of a dreaded obstetric complication
in the immediate postpartum period
Harold Levine, MD, Mehrzad Zarghouni, MD, and Walter Cannon, MD
HELLP (hemolysis, elevated liver enzymes, low platelet) syndrome is a
dreaded complication that may develop during pregnancy or in the immediate postpartum period. Rarely this syndrome manifests itself with
imaging findings. We report a case of HELLP syndrome in which the
diagnosis was reaffirmed via imaging findings.
ELLP syndrome is a descriptive acronym for a pregnancyinduced condition in which the patient presents with
hemolysis, elevated liver enzymes, and low platelets.
About 31% of the time, this syndrome manifests in the
immediate postpartum period (1). While HELLP syndrome
often occurs in the setting of preeclampsia or is thought of as a
variant of the preeclampsia/eclampsia spectrum (4%–12%), it
can occur independently, which can lead to a delay in diagnosis. While the clinical syndromes can overlap, risk factors for
HELLP syndrome and eclampsia differ in that multiparous
mothers and women older than 25 years old have an increased
risk for HELLP syndrome, while classically preeclampsia/eclampsia is associated with maternal age less than 20 or greater
than 45 and in the nulliparous.
Imaging abnormalities are rarely present in HELLP syndrome. However, when present, imaging and clinical presentations are characteristic and complementary in establishing the
correct diagnosis. Clinicians and radiologists should be aware
of the imaging manifestations, as prompt diagnosis and early
treatment are imperative. We describe a case in which the imaging and clinical presentations were characteristic.
H
CASE REPORT
A 22-year-old woman presented with abdominal pain postpartum. Her pregnancy course was complicated by severe preeclampsia, idiopathic thrombocytopenic purpura, and systemic
lupus erythematosus. Immediately in the postpartum period,
she developed progressive epigastric abdominal pain that radiated to her back. Her hematocrit level decreased from 36.8%
to 29.6%, while her aspartate aminotransferase level rose from
40 to 549 U/L and her alanine aminotransferase level rose from
30 to 321 U/L. During this time, her pain became severe, predominantly within the right upper quadrant. An initial hepatic
sonogram was unrevealing. However, further evaluation with
Proc (Bayl Univ Med Cent) 2014;27(2):141–142
contrast-enhanced computed tomography (CT) showed multiple areas of low attenuation within the liver parenchyma that
were nonenhancing compared with the rest of the liver (Figure).
These low-density areas were preferentially located within the
right hepatic lobe. There was no evidence of a subcapsular hematoma. The patient was treated supportively. Her symptoms
resolved and laboratory findings normalized. She was discharged
home in good condition.
DISCUSSION
Approximately 70% of patients who develop the HELLP
syndrome present in the antepartum period and about 30%
of patients present after delivery, as in our case. Typical onset
is within 48 hours of delivery, with symptoms varying from
simple generalized malaise to epigastric pain, nausea, vomiting, and headache. While it is less common to progress from
eclampsia and/or the HELLP syndrome to a hypovolemic state
and shock, clinicians must maintain a high index of suspicion
for hepatic hemorrhage and/or rupture in patients with perinatal
complicating disorders.
One study indicated that only 0.53% of 586 women with
perinatal HELLP syndrome or preeclampsia had positive imaging findings for hepatic rupture or hemorrhage. Hepatic hematomas were most commonly found in the right hepatic lobe,
believed to be secondary to its larger size and subsequent blood
flow in most patients; 75% of patients experienced right hepatic
lobe injury, while only about 10% had isolated left hepatic lobe
hematoma, and 14% had involvement of both hepatic lobes.
Imaging evaluation can be done with ultrasound or contrastenhanced CT for improved sensitivity and specificity.
Sonographic findings include irregularly shaped regions of
heterogeneous echoes, both regions of hyper- and hypoechogenicity within the hepatic parenchyma without intrinsic blood
flow. The regions are often wedge shaped, appearing similar to a
hepatic infarction. Often heterogeneous echoes are also seen in
the subcapsular regions compatible with associated subcapsular
hemorrhage and/or hematoma. Regions of abnormality can
From the Department of Radiology, Baylor University Medical Center at Dallas.
Corresponding author: Harold Levine, MD, Department of Radiology, Baylor
University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX 75246
(e-mail: haroldrlevine@gmail.com).
141
a
b
c
Figure. (a, b) Axial contrast-enhanced CT images show ill-defined hepatic hypodensities predominantly located within the right hepatic lobe (arrow). Notice the
appearance of a gallstone (arrowhead). (c) A coronal image shows ill-defined hepatic parenchyma hematomas predominantly within the right hepatic lobe (arrow).
be solitary or multiple and sometimes can be associated with
hepatic enlargement and edema.
Contrast-enhanced CT examination may be preferable in the
unstable patient if fast multislice technology can be employed,
given its rapidity and increased sensitivity and specificity. On
contrast-enhanced examination, hematoma and/or hemorrhage
will appear as single or multiple ill-defined or sometimes wedgeshaped regions of hypoattenuation. Hemorrhage tends to be
located near the portal triads, while hematomas can arise from
anywhere in the parenchyma. As in ultrasound, pericapsular
hemorrhage can occur and appears as a crescent-shaped fluid
density, usually hypoattenuating to adjacent normally perfused
hepatic parenchyma. An advantage of contrast-enhanced CT is
its ability to evaluate active extravasation of intravascular contrast, suggesting active hemorrhage. If contrast is seen outside a
vessel and appears the same density as the intravascular contrast,
142
the source of hemorrhage may be arterial in origin, and close
observation or potentially catheter-directed arterial embolization might be needed for treatment.
As the speed and accuracy of CT examination improves
with the employment of new low-dose techniques, clinicians are
becoming more inclined to employ CT imaging in the diagnosis
of patients with these perinatal complications. It is imperative
that radiologists be aware of the characteristics and potential
lethality of HELLP syndrome and other perinatal complications
to ensure correct and timely treatment.
1.
2.
Nunes JO, Turner MA, Fulcher AS. Abdominal imaging features of
HELLP syndrome: a 10-year retrospective review. AJR Am J Roentgenol
2005;185(5):1205–1210.
Padden MO. HELLP syndrome: recognition and perinatal management.
Am Fam Physician 1999;60(3):829–836, 839.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Fetal demise due to cord entanglement in the early second
trimester
Rahime Nida Ergin, MD, Murat Yayla, MD, and Ayse Seda Ergin, MD
In this report, we describe a rare cause of in utero fetal death, a complex
entanglement of the umbilical cord around the fetal neck. At the 16th
gestational week of pregnancy, routine fetal ultrasonography showed
no fetal heartbeat. Thereafter, the fetus was delivered vaginally in the
breech presentation. The neck was found to be encircled by multiple
tight loops of the umbilical cord. Other than a thin and elongated neck,
there were no dysmorphic features and no chromosomal abnormality
on cytogenetic analysis.
C
ord entanglement is a common finding in utero;
however, fetal demise resulting from nuchal cord
entanglement is rare (1–8). This report describes
such a case.
CASE PRESENTATION
The 37-year-old patient had no history of familial genetic
disease and no systemic disease. In her previous pregnancy, she
delivered a healthy baby girl vaginally at the age of 31 years. The
present pregnancy was conceived naturally. Screening completed
at the 12+3 gestational week, which included fetal nuchal translucency measurement, maternal serum pregnancy-associated
plasma protein A levels, and free beta-human chorionic gonadotropin levels, showed no increased risk for trisomies 21, 18, and
13. Doppler evaluation of maternal uterine arteries was within
normal limits. At the last routine visit at the 16th gestational
week, there was no fetal heartbeat. The fetus was delivered vaginally and was in the breech presentation. The fetus’s neck was
encircled by multiple tight loops of the umbilical cord and had a
reduced diameter (Figure). The umbilical cord was 35 cm long,
with a sectional diameter of 0.6 cm. There were no dysmorphic
features macroscopically and no congenital anomalies. Cytogenetic analysis showed 46, XY normal pattern.
DISCUSSION
The Table lists studies related to the incidence of nuchal
cord and two case reports with fetal demise due to nuchal cord
(1–8). The reported incidence of nuchal cord varies, with the
highest rates of 43% in the 13th to 16th gestational week and
8.3% in newborns (1, 6). The varying rates of incidence depend
mainly on the definition of cord entanglement. These studies
Proc (Bayl Univ Med Cent) 2014;27(2):143–144
Figure. A fetus with a thinned and elongated neck, encircled by multiple tight
loops of the umbilical cord.
From the Department of Gynecology and Obstetrics, Bahcesehir University,
Istanbul, Turkey (R. Ergin); the Department of Gynecology and Obstetrics,
International Hospital, Istanbul, Turkey (Yayla); and the Department of Radiology,
Istanbul University Cerrahpasa Medical Faculty, Istanbul, Turkey (A. Ergin).
Corresponding author: Rahime Nida Ergin, MD, Assistant Professor, Defne Apt
no:140 D:5 Feneryolu Kadıköy, Istanbul, Turkey (e-mail: drnidaergin@gmail.
com).
143
Table. Previously reported cases of nuchal cord entanglement
Reference
number
First
author
Year of
publication
Number of cases
Study design
Frequency
Study outcome
1
Lipitz S
1993
1016 newborns
Retrospective
+ prospective
8%
No effect on term birth weight
2
Larson JD
1995
326 newborns
Retrospective
4%
No effect on neonatal outcome. Increased risk of abnormal fetal
heart rate pattern, operative vaginal delivery
3
Larson JD
1997
4029 newborns
Retrospective
29%
4
Singh V
2003
1 intrauterine fetal
death (IUFD)
Prospective
5
Ghi T
2007
5 newborns
Prospective
3%
6
Tepper R
2009
64 fetuses
Prospective
43%
7
Gambhir PS
2011
3 cord entanglements
Case report
—
Died (3), one due to nuchal cord
8
Dodds M
2012
3 nuchal cord
entanglements
Case report
—
Died (1)
generally support that nuchal cord is a common finding in
fetal life, with decreasing rates in the newborn (1, 2, 5, 6).
However, rather than showing decreasing rates, one study
showed that nuchal cord rates increased linearly from 6% in
the 20th gestational week to 29% in the 42nd gestational week,
regardless of whether the entanglement involved a single loop
or multiple loops (3).
The presence of nuchal cord seems to have no effect on the
outcome of pregnancy in terms of birth weight, rate of stillbirth,
or rate of vaginal delivery after induction (1–3, 5). Compared to
no entanglement or only one cord entanglement, two or more
cord entanglements have been associated with an abnormal fetal
heart rate pattern, requiring more low or midforceps application with a lower 1-minute Apgar score and an umbilical artery
pH ≤ 7.10 without any adverse neonatal outcome (2). Umbilical cord abnormalities, mainly umbilical cord constriction and
coiling, have been shown to be related to 11% of intrauterine
fetal deaths within 16 gestational weeks (4). Fetal demise due
to nuchal cord entanglement has been reported to occur in the
first or second trimester in two case reports (7, 8).
A decreasing incidence of cord entanglement around the
neck seems to be a normal phenomenon during fetal uterine
development, but rare instances result in fetal demise. An autopsy study of 139 mostly second-trimester fetuses that died
due to umbilical cord stricture and overcoiling revealed the
absence of Wharton’s jelly as an intrinsic cord pathology (9).
Likewise, a not-yet-clarified intrinsic umbilical cord anomaly
associated with the physical compression of entanglement may
144
8%
No effect on stillbirth rate
Cord constriction, coiling, hemorrhage, thrombosis, amniotic
bands as frequent causes of IUFD
No effect on rate of vaginal delivery after induction
A 63% rate of any cord entanglement in early fetal life
explain why some rare cases of nuchal cord end in fetal demise.
To date, nuchal cords have been shown to have significantly
lower vascular coiling than ones without nuchal entanglement
(10). The relevance of this finding in terms of fetal demise is
not yet known.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Lipitz S, Seidman DS, Gale R, Stevenson DK, Alcalay M, Menczer J,
Barkai G. Is fetal growth affected by cord entanglement? J Perinatol
1993;13(5):385–388.
Larson JD, Rayburn WF, Crosby S, Thurnau GR. Multiple nuchal cord
entanglements and intrapartum complications. Am J Obstet Gynecol
1995;173(4):1228–1231.
Larson JD, Rayburn WF, Harlan VL. Nuchal cord entanglements and
gestational age. Am J Perinatol 1997;14(9):555–557.
Singh V, Khanum S, Singh M. Umbilical cord lesions in early intrauterine
fetal demise. Arch Pathol Lab Med 2003;127(7):850–853.
Ghi T, D’Emidio L, Morandi R, Casadio P, Pilu G, Pelusi G. Nuchal
cord entanglement and outcome of labour induction. J Prenat Med
2007;1(4):57–60.
Tepper R, Kidron D, Aviram R, Markovitch O, Hershkovitz R. High
incidence of cord entanglement during early pregnancy detected by
three-dimensional sonography. Am J Perinatol 2009;26(5):379–382.
Gambhir PS, Gupte S, Kamat AD, Patankar A, Kulkarni VD, Phadke MA.
Chronic umbilical cord entanglements causing intrauterine fetal demise
in the second trimester. Pediatr Dev Pathol 2011;14(3):252–254.
Dodds M, Windrim R, Kingdom J. Complex umbilical cord entanglement.
J Matern Fetal Neonatal Med 2012;25(9):1827–1829.
Peng HQ, Levitin-Smith M, Rochelson B, Kahn E. Umbilical cord
stricture and overcoiling are common causes of fetal demise. Pediatr
Dev Pathol 2006;9(1):14–19.
Strong TH Jr, Manriquez-Gilpin MP, Gilpin BG. Umbilical vascular coiling
and nuchal entanglement. J Matern Fetal Med 1996;5(6):359–361.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Ingrown toenails (unguis incarnatus): nail braces/bracing
treatment
Anca Chiriac, MD, PhD, Caius Solovan, MD, PhD, and Piotr Brzezinski, MD, PhD
Nail bracing is a safe, simple, and inexpensive treatment option that
avoids surgery, requires no anesthetic, requires no recovery period, allows wearing the existing shoes, offers immediate relief from pain, and
allows the practice of daily activities. Braces can be used for prolonged
periods of times. If recurrence occurs, reapplication of bracing is usually
required.
ngrown toenails are one of the most frequent nail disorders,
with great impact on daily activities, discomfort, and pain.
Its pathogenesis is simple: a wide, curved nail plate associated with lateral corners cuts obliquely, leaving a tiny spicule
(a small piece of nail) that digs into the lateral nail groove and
pierces the epidermis. The result is a foreign body reaction with
inflammatory cells, granulation tissue, and secondary infection
(1). Candida albicans is a frequent complicating factor in both
the causation of an ingrown nail as well as its management.
Precipitating factors are narrow pointed shoes, tight socks, hyperhidrosis, and diabetes mellitus (2). There are three stages of
an ingrown nail: 1) inflammation, swelling, and pain; 2) inflammation, pain, nonhealing wound and oozing, and granulation
tissue; and 3) abscess formation and chronic induration of the
lateral nailfold. The treatment is frustrating and difficult for the
patients and physicians and is associated with local complications and sometimes permanently distorted toes and nails.
Nail braces were created in 1872 by E. E. Stedman, but
their use began in Europe and Australia in 1960. Ingrown toenail bracing was developed in the 1980s by the Institute for
Orthonyxia in Erlangen, Germany. Nail bracing is a conservative method used for ingrown nails, applied even in children,
patients with diabetes mellitus, and cases of local infection (stage
3). The braces are made from steel wire or plastic bands; the
wire is applied over the dorsal surface of the nail and curved
under its lateral edges (Figure) (3). A loop bridges the levers
and draws them together. The wires are then trimmed and the
edges covered with an artificial nail mass to protect footwear.
The braces are applied after measuring the nail of the individual,
and the pressure is modified monthly based on the presence of
symptoms. The administration of antibiotics is controversial,
and most favor simple hygienic measures. Braces are removed
when all symptoms vanish.
I
Proc (Bayl Univ Med Cent) 2014;27(2):145
Figure. Nail brace treatment for an ingrown nail in an active athlete.
1.
2.
3.
Brzezinski P. Assessment of the effectiveness of application antiseptics in
prevention of foot skin inflammation. N Dermatol Online 2011;2(1):21–
24.
Brzezinski P. Skin disorders of the foot during military exercise and their
impact on soldier’s performance. Lek Wojsk 2009;87(2):80–83.
Talwar A, Puri N. A study on the surgical treatment of ingrowing toe nail
with nail excision with chemical matricectomy versus nail excision alone.
Our Dermatol Online 2013;4(1):32–34.
From the Department of Dermatology, Nicolina Medical Center, Iasi, Romania
(Chiriac); Department of Dermatology, Victor Babes University of Medicine,
Timisoara, Romania (Solovan); and Department of Dermatology, 6th Military
Support Unit, Ustka, Poland (Brzezinski).
Corresponding author: Piotr Brzezinski, MD, PhD, Department of
Dermatology, 6th Military Support Unit, os. Ledowo 1N, 76-270 Ustka, Poland
(e-mail: brzezoo77@yahoo.com).
145
Baylor news
■ The Heart Hospital Baylor Denton opens
On January 6, 2014, The Heart Hospital
Baylor Denton began treating cardiovascular
patients at its newly remodeled location, 2801
South Mayhill Road, Denton. Part of Baylor Scott
& White Health, the 68,580-square-foot, 16-inpatient bed specialty hospital offers comprehensive cardiac and vascular services. According to
the hospital’s administrators, all Denton cardiac
surgeons are members of the facility’s medical
staff, and more than 90% of the area’s cardiologists have joined the medical staff of The Heart
Hospital Baylor Denton.
“Expanding our brand of five-star services
further into North Texas has been a goal of
ours,” said Mark A. Valentine, president, The
Heart Hospital Baylor Plano. “We’re pleased to
be welcomed by Denton cardiovascular physicians.” Valentine also serves as president of the
new Denton facility.
Services at The Heart Hospital Baylor Denton
include a cardiac catheterization lab; an electrophysiology lab; cardiovascular operating suites
(with a hybrid operating suite used for minimally
invasive procedures, which can be converted to
open surgery); and advanced imaging, including a
256-slice computed tomography scanner, threedimensional and two-dimensional ultrasound,
fluoroscopy, and 1.5T magnetic resonance imaging. A 16-bed inpatient nursing unit will be
expanded to 22 beds in May 2014. In addition,
there is a 12-bed outpatient ambulatory surgery unit and outpatient cardiovascular services
through the Center for Advanced Cardiovascular
Care. A Comprehensive Wound Center offers hyperbaric oxygen therapy; the emergency department has been expanded from 2 to 5 beds; and
the full-service hospital laboratory offers 24/7
services, including transfusions.
Baylor acquired the facility in May 2013 and
quickly began a two-stage renovation project
that is scheduled to be completed in May 2014.
The second phase of construction will add six
more intensive care unit suites and an additional cardiovascular operating room. Ascension
Architects Inc., CBRE, and MEDCO Construction
comprise the renovation team.
■ Baylor Emergency Medical Center at
Murphy opens
The new Baylor Emergency Medical Center
at Murphy opened as the first center of its kind
from Baylor in Collin County when it began
146
seeing patients at 511 FM 544, Suite 100, on
February 3, 2014. Baylor Emergency Medical
Center at Murphy offers emergency medical and
inpatient care that is “patient-centric” in its innovative approach. From the moment the patient
enters the facility, the experienced medical staff,
systems, and technology will be ready to meet
the patient’s needs in a way that is convenient,
accessible, efficient, and compassionate. Unlike
urgent care centers, which are designed to handle non–life-threatening medical complaints, or
freestanding emergency departments, Baylor
Emergency Medical Center at Murphy will be a
licensed hospital, providing clinical quality and
efficient operations.
At Baylor Emergency Medical Center at
Murphy, patients have convenient access to an
emergency physician, whom they can usually
see within minutes, with an average door-todoc time of less than 10 minutes; hospital-level
amenities, including a dedicated inpatient wing;
an in-house laboratory for prompt results; and
on-site imaging, including x-ray, computed tomography scanning, and ultrasound. An added
benefit to this community hospital is the inpatient beds it offers. If a patient requires an overnight stay, Baylor Emergency Medical Center at
Murphy offers comfortable inpatient beds and
around-the-clock care.
Baylor opened its first emergency medical
center in Aubrey, and other emergency medical
centers are planned for other areas.
■ Baylor research uses stem cells to
heal the heart
As scientists investigate the medical potential
for adult stem cells, new research from Baylor’s
Soltero Cardiovascular Research Center (SCRC)
seeks to provide deeper insight on the topic. Led
by Cara East, MD, medical director of the SCRC,
the center is involved in a set of two clinical trials
studying the use of autologous adult stem cells in
various heart and vascular conditions. The team
has researched stem cells in particular for more
than 8 years because of the cells’ special ability
to “mend.” Autologous stem cells come from
the patient’s own body.
“Adult stem cells are actually ‘super repair
cells,’” Dr. East said. “We know—from recent,
basic research—that adult stem cells do not
transform into new cells. Rather, they stimulate
removal of scar tissue, which then causes healthy
cells to grow and replenish. After the healthy cells
do their work, the adult stem cells die; they may
only live 2 weeks to 3 months. This ensures that
the repair cycle does not continue indefinitely,
which could result in tissue overgrowth.”
Each clinical trial has its own criteria, objectives,
and parameters, but they share a similar goal: to
explore (and possibly harness) the human body’s
restorative power through its own cells. The first trial
studies patients with critical limb ischemia, to determine if the injection of bone marrow into damaged
tissues improves blood flow. The ixCELL study is for
patients with congestive heart failure. Through this
research, investigators will determine if catheterbased injection of ixmyelocel-T (compared with placebos) is effective, safe, and tolerated for certain
heart failure patients. Ixmyelocel-T is developed
by culturing the patient’s own bone marrow. The
resulting cell treatment is then injected into the
patient’s heart muscles to encourage growth of
new tissue and improve inflammation.
“Our dream is to develop therapies that are
less invasive and can help patients who cannot
currently be helped with available therapies,” Dr.
East said. “Plus, we hope this research leads
us to treatments that work even better than our
current therapies.”
■ Baylor prescribes FollowMyHealth,
new patient portal
Baylor Health Care System (BHCS) patients
are beginning to use FollowMyHealth™ to
manage their personal health records. Baylor’s
FollowMyHealth is a patient portal that provides
a convenient and secure way for patients to
manage their personal health record from any
computer or mobile device with Internet access.
Patient portals are an effective tool for patient
engagement, where patients are partners in
their own medical care, supporting Baylor’s
patient-centered focus. Patient portals are also
one of the objectives of the federal government’s
Health Information Technology for Economic and
Clinical Health (HITECH) Act. The meaningful use
provision requires that patient portals be made
available and used by patients.
Patients receive automatic email invitations
to create accounts after discharge. If they
choose not to connect by email, they can go to
the Baylor consumer portal, BaylorHealth.com/
FollowMyHealth, to fill out and return a request
form to the health information management department of the hospital where they were most
recently a patient.
Proc (Bayl Univ Med Cent) 2014;27(2):146–148
RECENT GRANTS
• JC virus and human colorectal
neoplasia
Principal investigator: C. Richard Boland,
MD
Sponsor: National Institutes of Health
Funding: $240,637
Award period: 2/1/14–1/31/15
• Patient engagement
Principal investigator: Andrew Masica, MD
Sponsor: Dartmouth College/Department
of Health and Human Services/Centers
for Medicare and Medicaid Services
Funding: $374,872
Award period: 7/1/13–6/30/14
• Ubiquitin-mediated regulation of Tak1
and tumor-associated inflammation
Principal investigator: Venuprasad
Poojary, PhD
Sponsor: American Cancer Society
Funding: $180,000
Award period: 11/13/13–6/30/16
• Targeting plasmacytoid dendritic cells
to treat human myeloma
Principal investigator: Yong-Jun Liu, PhD,
MD
Sponsor: Cleveland Clinic/National Institutes
of Health
Funding: $96,002
Award period: 9/13/13–1/31/14
• Altered T follicular helper cell subsets
in active pediatric SLE
Principal investigator: Hideki Ueno, MD,
PhD
Sponsor: Alliance for Lupus Research
Funding: $169,932
Award period: 2/1/14–1/31/15
• Glycemia reduction approaches in
diabetes: a comparative effectiveness
study
Principal investigator: Priscilla Hollander,
MD
Sponsor: George Washington University/
National Institutes of Health
Funding: $432,322
Award period: 8/1/13–7/31/14
• Baylor core clinical center for the
Cardiothoracic Surgical Network
Principal investigator: Michael Mack,
MD
Sponsor: National Institutes of Health
Funding: $349,316
Award period: 2/1/14–1/31/15
FollowMyHealth provides access to a portion of the medical record, including reports on
laboratory studies and other test results, and
clinical information such as allergies, immunizations, and discharge medications. Not all
clinical data is available in FollowMyHealth. For
example, physician documentation and certain
sensitive results such as hepatitis, HIV, STD, and
genetic testing results are not available at this
time. For the complete medical record, patients
will continue to contact the health information
department at the Baylor facility where they
were most recently a patient.
list of “100 Hospitals With Great Women’s Health
Programs,” as well as its list of “100 Hospitals
With Great Orthopedic Programs.” Becker’s
Hospital Review, a widely read and highly respected health care industry trade publication,
selected BUMC for these elite lists based on a
variety of criteria. “To be included on these lists
alongside some of the other most highly respected hospitals in the country is a tremendous
tribute to our staff in both Women and Children’s
Services and Orthopedics, as well as all those
who support them,” said John McWhorter, DSc,
MHA, BUMC president.
Advanced Palliative Care. The hospital is the second Baylor facility to earn this distinction. BUMC
was the first program in Texas—and one of the
first 10 in the nation—to receive this certification
from the Joint Commission in September 2013.
■ Baylor Irving earns coveted Magnet®
■ Fort Worth is second Baylor facility to
designation for nursing excellence
Baylor Medical Center at Irving has received
Magnet designation for excellence in nursing
services from the Magnet Recognition Program
of the American Nurses Credentialing Center.
Magnet designation is one of the highest levels
of recognition a hospital can achieve. For patients, this designation means that their care
is provided by a nursing staff that ranks in the
top 7% of hospitals in the country. According
to the American Nurses Credentialing Center,
Magnet designation is the gold standard of patient care.
earn Palliative Care Certification
The Joint Commission recently certified
Baylor All Saints Medical Center at Fort Worth for
■ Becker’s recognizes BUMC’s women’s
health, orthopedics among top 100
Becker’s Hospital Review has named Baylor
University Medical Center at Dallas (BUMC) to its
April 2014
■ The Heart Hospital Baylor Plano
receives three-star rating
The Heart Hospital Baylor Plano (THHBP)
earned a high honor from the Society of Thoracic
Surgeons (STS): a three-star rating for aortic
valve replacement surgery, coronary bypass
surgery, as well as doing both procedures
simultaneously. Only a small percentage
of hospitals qualify to receive the prestigious
three-star rating for all three procedures, based
on the STS’s quality methodology. “This is a
testament to the expertise of our health care
UPCOMING CME PROGRAMS
The A. Webb Roberts Center for Continuing Education of Baylor Health Care System is
offering the following programs:
Cardiac Innovations, May 8, 2014, at The Heart Hospital Baylor Plano
Fifth Annual Latest Advances in Ischemic and Hemorrhagic Stroke Therapy, May
17, 2014, at Westin Galleria Dallas
41st Annual Williamsburg Conference on Heart Disease, December 7–9, 2014, in
Williamsburg, Virginia
For more information, call 214.820.2317 or visit www.cmebaylor.org.
Baylor news
147
PHILANTHROPY NOTES
■ A heart for the Dallas community
BHCS Foundation is pleased to announce that
long-time supporters Gayle and Paul Stoffel have
recently contributed $500,000 to establish an
endowment fund in support of BHCS cardiology
initiatives. The fund will be known as the Gayle
and Paul Stoffel Endowed Fund in Cardiovascular
Research and Education. It will provide essential
funding for cardiovascular leadership, innovative
research, patient-centered programs, capital investments, and education.
“Gifts like these validate Baylor’s advanced
cardiology research and education programs.
We are now seeing a return on our investments
in the development of new and innovative therapies that are improving the lives of our patients
and the health of the community,” said Kevin
Wheelan, MD, chief of staff, Baylor Jack and
Jane Hamilton Heart and Vascular Hospital.
■ $1 million corporate grant supports
enhanced memory center at Baylor
Thanks to a $1 million grant from a large
Dallas-based corporation, Baylor is poised to
create a world-class center of excellence in the
diagnosis and treatment of Alzheimer’s disease
and dementia. Through the enhanced Memory
Center, patients and families navigating a diagnosis of dementia or Alzheimer’s disease will
have expanded treatment options and greater
social and emotional support. The Memory
Center will be located on the northwest corner
of Park Lane and Central Expressway, across
the street from NorthPark Center.
team,” said Mark Valentine, THHBP president.
“With this latest STS quality ranking, The Heart
Hospital Baylor Plano is one of only 14 programs
in the United States to hold a three-star ranking
in all three categories.”
■ Ballard book on STEEEP care
receives prestigious Shingo Award
Achieving STEEEP Health Care, the story
of Baylor Health Care System’s journey of improving quality, received the Shingo Research
and Professional Publication Award. David J.
148
The $1 million corporate grant, combined
with an additional $1 million from BHCS
Foundation, officially launches an ambitious
effort to bring much-needed resources and
staffing to the Memory Center. Initially, these
resources will allow Baylor to double the number
of patients cared for annually. Additionally, these
funds will allow the Memory Center to greatly
reduce the diagnosis and treatment wait times.
Generous donor support will also enable a care
coordinator from the Alzheimer’s Association
to be located at the Memory Center to help
connect patients, families, and caregivers with
important social, financial, legal, residential, and
educational support. Long-term objectives of
the Memory Center include expanded research
and clinical trial programs.
“We are incredibly grateful for the extraordinary support and interest the Memory Center
has received to date. Through continued interest and support of the Memory Center,
donors will directly impact families struggling
with diagnoses of dementia,” said Rowland
K. Robinson, president of BHCS Foundation.
“We’re excited about the opportunity not
only to care for additional patients, but also
to provide an additional scope of services to
help navigate a lifelong journey with these
diseases.”
■ Pathology’s 10-person microscope
provides multiple benefits to Baylor
patients
Peter A. Dysert II, MD, chief of pathology and director of the pathology residency
Ballard, MD, MSPH, PhD, FACP, CMM, chief
quality officer for Baylor Scott & White Health
and president of the STEEEP Global Institute, is
the book’s editor.
In his book, Ballard offers strategies and
lessons in the areas of people, culture, and
processes that have contributed to the improvements in patient and operational outcomes at
Baylor. STEEEP is an acronym trademarked by
Baylor to communicate the six “aims” for improvement set forth by the Institute of Medicine
based on the core need for health care to be
Baylor University Medical Center Proceedings
program at BUMC, said he is certain of one
thing: the study of disease is too vast a
knowledge set for any single person to master. With the addition of a new 10-headed
microscope, funded by BHCS Foundation,
pathologists and pathology residents have
a new educational and diagnostic tool that
will further enhance training and patient
outcomes at BHCS.
The 10-headed scope is primarily used
for a daily case review conference that allows pathologists to review slides on challenging cases as a group. The microscope
also serves as a valuable teaching tool.
Pathology residents are not only able to sit
in on discussions between pathologists as
they review cases, but are able to simultaneously view the slide images in real time on a
60-inch, flat screen monitor, providing virtually the same effect of sitting at the scope
themselves.
“It is huge to bring together the experiences of 10 to 15 pathology experts at
one time—with a collective experience of
several hundred years—to provide more
accurate diagnoses for Baylor patients,
especially involving complex cases,” said
Dr. Dysert. “This 10-headed microscope is
the single biggest improvement, from my
vantage point, that has been made in our
practice of surgical pathology in the last 10
years.”
For information on how you can support
these or other initiatives at Baylor, please contact the Foundation at 214.820.3136.
safe, timely, effective, efficient, equitable, and
patient centered.
“Achieving STEEEP Health Care is a compelling and comprehensive book on improving
quality,” said Troyen A. Brennan, MD, executive
vice president and chief medical officer at CVS
Caremark. “Baylor Health Care System’s commitment to better health care is unmatched,
and in David Ballard they found a person who
can not only lead change, but also capture and
characterize the key insights that will help the
rest of us get on the path to superb care.”
Volume 27, Number 2
In memoriam
GEORGE KENNEDY (“KEN”) HEMPEL JR., MD
Department of Surgery, Baylor University Medical Center
at Dallas
Dr. Ken Hempel, a prominent surgeon at Baylor University
Medical Center (BUMC), died on December 26, 2013. Proceedings published an interview with him in 2007 (20:369–380),
and the text below was taken from the introduction to that
interview by Dr. William C. Roberts.
Ken Hempel lived virtually his entire life in Dallas, Texas.
He was born on October 25, 1934. He graduated from public
schools, including Highland Park High School, where he was
a star athlete. He married Ruth Barrett, his sweetheart from
the eighth grade, as a senior in high school. Ken attended
Southern Methodist University and after 3 years there entered
the University of Texas (UT) Southwestern Medical School,
where he obtained his medical degree in 1959. He did a rotating internship at BUMC and then entered the general surgery
program of Parkland Hospital after a brief stint in Iowa City.
After completing his residency in 1965, he spent 1 year in
Houston at Methodist Hospital doing a cardiovascular fellowship under Dr. Michael E. DeBakey and his colleagues.
In 1966, he entered the US Army Medical Corps, where he
remained for 2 years before returning to Dallas and beginning
a private practice of both vascular and general surgery. Within
a few years, he became a major player at BUMC, where he
practiced for over 40 years. He and Ruth were the proud
parents of three children.
GEORGE J. RACE, MD, PHD
Department of Pathology, Baylor University Medical Center
at Dallas
Dr. George Race, the founding editor of BUMC Proceedings, who also served as chief of pathology, dean of continuing
education, and chairman of the Baylor Research Foundation,
died on December 17, 2013. He was interviewed in Proceedings (2001;14:264–285), and the introduction to his interview
by Dr. Roberts appears below. Tributes to Dr. Race appear on
p. 150 of this issue.
George Race was born in Everman, Texas, on March 2,
1926. He grew up in a 2-room house with running water but
without plumbing and usually without a father. He graduated
from high school in 1942. After a year at Texas Wesleyan College
and a second year at Baylor University, he had acquired enough
premedical credits to enter medical school at UT Southwestern
Medical School, where he graduated in June 1947 at age 21.
Proc (Bayl Univ Med Cent) 2014;27(2):149
He was allowed to complete medical school in 36 consecutive
months because the USA wanted to avoid a physician shortage
during the war. He interned in pathology at Duke University
and in surgery at the Boston City Hospital. On July 1, 1949, he
entered the US Air Force at Alamogordo, New Mexico, becoming a flight surgeon and spending time in Korea. After nearly
3 years in the armed services, he returned to Duke University,
completing his pathology residency in 1953. He then moved
to Harvard Medical School and Peter Bent Brigham Hospital
in Boston, where he was a faculty member for a year. In 1954,
he went to St. Petersburg, Florida, as chief of the pathology
department at St. Anthony’s Hospital; he stayed for a year before
returning to Dallas and Southwestern Medical School, where
he was appointed to the pathology faculty in 1955. In 1959,
he became chief of pathology at BUMC, a position he held
until 1986.
George Race was responsible for building the splendid
laboratories at BUMC. He published extensively. His book,
Laboratory Medicine (written at Baylor), a 4-volume loose-leaf
publication, was updated regularly through 13 revisions. He
published 165 articles in peer-reviewed journals and nearly as
many abstracts. He was instrumental in starting the A. Webb
Roberts Center for Continuing Education and was its first dean.
He was also chairman of the Baylor Research Foundation from
1986 to 1989 and during that period founded BUMC Proceedings and received the Distinguished Achievement Award from
Baylor University. Along the way, George Race studied anthropology at Southern Methodist University and, for 1 year, law
at the evening law school of the same university.
George and his lovely wife, Anne, also a physician, traveled
extensively. His interest in animals led him to acquire many species on his ranch in Lampasas. He and Anne were the parents
of four living children, all of whom are physicians. Through the
years, Dr. Race received many awards and honors, including
the presidencies of the North Texas Society of Pathologists, UT
Southwestern Medical School Alumni, the Dallas Academy of
Pathology, the Texas Society of Pathologists, the American Cancer Society of Dallas County, the Texas Division of the American
Cancer Society, the Dallas Southern Clinical Society, and the
Society of Medical College Directors of Continuing Medical
Education. He served as chairman of the Explorers Club, Texas
Chapter, and vice president for chapters and a board member of
the Explorers Club, New York. His many hobbies, wide travels,
keen insights, and incredible memory made him a fascinating
man from whom we can all learn.
149
Tributes to George J. Race, MD, PhD
W. L. JACK EDWARDS, MD
I first met George Race in 1945 at the Phi Chi medical
fraternity house, where he served as house manager in return
for reduced cost of room and board. He was a sophomore and
I was a freshman at the University of Texas (UT) Southwestern
Medical School. After graduation, George had an internship
in pathology at Duke under Dr. Forbus. Then he tried an
internship in surgery at Boston City Hospital. That year I had
an internship in pathology at Peter Bent Brigham Hospital.
A college roommate of mine had found a small apartment
on Newbury Street for Patsy and me, but it was adjacent
to four railroad tracks. There was no air-conditioning so the
windows were open. When we heard a train coming, it was a
race to shut the windows before the smoke came billowing in.
Patsy contacted Anne Race to look for another place to live.
They found a two bedroom, one bath apartment facing the
Charles River, and we decided to share it to cut expenses. Our
first child, Tricia, came in January. George never complained
about a crying child. In general, he was very accepting and
not critical of people.
Then George went to the Air Force for training as a flight
surgeon, winding up at Nagoya, Japan. I had a year at Mass
Memorial in medicine and 4 months of a medical residency at
Parkland before being called to active duty in the Navy and was
assigned to the Army when the Korean War broke out. I wound
up as the pathologist and lab officer at the hepatitis center hospital at Kyoto, Japan. Courtesy of a kind commanding officer, I
was able to visit George in Nagoya, which was bombed heavily
in World War II since it was Japan’s major air center. We drove
around the city, seeing only block after block of vacant land
cleared of rubble 5 years after the war. Years later, George had
his own plane, and he flew into his early 80s.
After finishing his training at Duke and Peter Bent Brigham,
George got his first job as the pathologist for a hospital in
Tampa, Florida. That year I had a National Institutes of Health
traineeship in cardiology in Birmingham with Dr. Harrison. So
we packed up our three children and visited the Races. George
liked his job but wanted to return to Dallas. It was not long
before he became an assistant professor in pathology at UT
Southwestern. The medical school was nice, but low pay led to
his taking a job with Dr. Terrell, who did much of the pathology
and lab services for Fort Worth and West Texas.
150
When Baylor University Medical Center (BUMC) was
looking for a new chief of pathology, Jesse Thompson and I,
among others, campaigned for George to take the job. He was
chosen and made a very good contract to provide pathology and
laboratory services for the hospital. George has trained many
pathology residents, and all of them have passed the pathology
boards. He found good people to run the Baylor laboratories.
He exhibited good organizational skills.
In 1955, Patsy, Anne, Alice McCarley, and Margaret Clayton decided to form a gourmet club, rotating in turn the chore
of fixing a multicourse fancy dinner monthly. It was a bonanza
for George, Ben McCarley, John Clayton, and me! The group
did meet monthly into the 1990s!
In 1960, I told George that I wanted to buy some land using a loan from the new Texas Veterans Land Board. This precipitated George’s first raw land purchase near Murphy, Texas,
and started his lifelong pursuit of real estate. Anne and George
have invited us to their ranch near Lampasas and to their South
Padre beach house. George preferred air-conditioning over salt
water, so he stayed in the house and watched three television
sets simultaneously.
I have been on three different deer leases with George. He
liked the camaraderie with the other hunters but not learning
the finer points of deer hunting. He frequently took a stack
of medical journals into a blind, flipped pages to advertise his
presence to deer, and then wondered why he saw no deer that
day. He would often arrive late at night after a day’s work at the
hospital wearing a suit, in which he hunted the next day. On
another occasion, he brought slides and movies from a recent
trip to Africa. That evening, he projected both slides and movies
simultaneously on the wall of the cabin. His only commentary
was a repeated “Africa is lousy with animals.”
George had the ability to concentrate and the drive to finish
a job promptly. When he began his tenure at Baylor, there were
about 100 unfinished autopsy reports. He worked night and
day for 2 months until all reports were current.
George believed in education. While a resident at Duke,
he obtained a master’s degree from a nearby college. While at
Baylor, he finished his PhD at Southern Methodist University
(SMU). He also took one course in contract law from the SMU
law school to help with his real estate investments. George was
instrumental in starting and editing the BUMC Proceedings, a
Proc (Bayl Univ Med Cent) 2014;27(2):150–152
good place for Baylor residents and researchers to place their
papers, as well as a good advertising vehicle among physicians
and health professionals. All four of his children became physicians, perhaps a tribute to his love of medicine.
Although he was dedicated to pathology, he had many other
interests and abilities. He was an upholsterer, having worked in
a furniture factory during high school. He was also a plumber,
electrician, and auto mechanic. He directed the continuing
education department at the medical school.
George was a good pathologist, a good teacher, a good organizer, a man blessed with a near-perfect memory, a forward
thinker, a good father, and a good husband. Most of all to me,
he was a good friend.
JOSEPH W. FAY, MD
Dr. George Race was instrumental in the early success of the
Baylor Research Institute and the Charles A. Sammons Cancer Institute. His dedication to laboratory discovery, clinical
pathological correlation in malignant disease, and translation
to the clinical practice of medicine was unsurpassed at Baylor.
His ability to understand and help direct investigator-initiated
research was evident in the early interaction with me during the
establishment of the hematopoietic cell transplantation program
at the Sammons Cancer Institute and Baylor Research Institute.
This was evident by his support and encouragement to me and
others in establishing new approaches to the treatment of cancer
with cellular therapy initially using hematopoietic stem cells
and, through his legacy, blood cells used to immunize patients
to treat cancer in clinical trials involving dendritic cells alone
and in combination.
Dr. Race made it possible for the establishment of the North
American Blood and Marrow Transplantation Program, one of
the first cooperative transplant programs in the United States,
whose members convened from several academic transplant
centers for meetings in Dallas. As a result, several important
developments were made in the field of clinical hematopoietic
cell transplantation. These discoveries tested in clinical trials
included new pretransplant conditioning regimens, cytokines
to enhance marrow and immune recovery posttransplant, and
methods to prevent graft-versus-host disease and opportunistic
infections. These efforts resulted in several publications as well
as Dallas community and peer-reviewed grant support.
Indeed, such early efforts with the support of Drs. John
Fordtran and Marvin Stone led to the successful launching
of studies in human immunology in our own laboratories
in collaboration with several investigators led by Dr. Jacques
Banchereau at the Baylor Institute for Immunology Research
(BIIR). Such work resulted in a decade of successful funding by
the National Cancer Institute in collaboration with Dr. Ralph
Steinman, Nobel Laureate and discoverer of the dendritic cell.
Indeed, the blood and marrow transplant research in some way
played an important part in establishment of BIIR. Dr. Race
with others provided the scientific and clinical catalyst for the
BIIR, which has evolved into a major immunology institution
with seminal work in autoimmunity, cancer immunotherapy,
transplantation immunology, and infectious disease.
April 2014
Dr. Race directly and indirectly is recognized as one of the
most important members of the Baylor Research Institute’s success. His attitude, work ethic, and interests continue to flourish.
Dr. Race will be missed by many.
MICHAEL RAMSAY, MD
George Justice Race, MD, PhD, was a giant of a man and
physician. His contributions to medicine and to BUMC have
been outstanding. George’s counseling and mentoring for me,
during my career at Baylor, will never be forgotten.
George Race became chief of pathology at BUMC in 1959,
but he also became a physician leader at Baylor. He planned
and built the first “state-of-the-art” pathology laboratories.
This experience caused him to write the leading textbook on
this topic at the time, Laboratory Medicine. This continued on
through 13 editions.
George’s large interest in medical education and research
resulted in him being a powerful force in the creation of both
the A. Webb Roberts Center for Continuing Education and
the Baylor Research Foundation, soon to become the Baylor
Research Institute (BRI). George Race was a leader in both these
entities. He was dean of the former and chairman of the latter.
He also started BUMC Proceedings in 1988. This was planned
as a medical journal that would publish the clinical reports of
the Baylor residents. It was modeled from other hospital journals, such as those of the Mayo Clinic, Cleveland Clinic, Johns
Hopkins, and Henry Ford Hospital.
The legacy that George Race leaves is that of outstanding
accomplishments. The BUMC Proceedings is now in its 27th
year, is indexed by PubMed, and receives 2 million hits a year
on the website. BRI is now a $60 million a year operation with
over 900 active research projects underway, an National Institutes of Health Center of Excellence for lupus research, and
federal grants exceeding $20 million a year. The intellectual
property portfolio is large, many patents have been licensed
by industry, and academic and industry collaborations flourish. The institutional review board was the first independent
board to receive full accreditation from the Association for the
Accreditation of Human Research Programs, a fine accolade
for the high standard of performance. The pathology department continues as a major foundation of the institution and
has now partnered in a major innovative laboratory company,
Medfusion.
George was not a politician. He always said what he thought
and did not pull any punches. He continued on the BRI board
until his death and was always a source of good counsel. We are
also very grateful for his and Anne’s support of BRI financially.
The George and Anne Race Immunology Research Laboratory
is providing internationally recognized results.
Boone Powell Sr. recruited George Race to Baylor, and they
became close friends. The vision of Boone Powell was matched
by the vision and innovation of George Race. Baylor was the
beneficiary and is still reaping the rewards by becoming a worldrecognized medical center.
George Race was a truly a giant among physicians, a man
who could see the vision and accomplish it. With a warm and
Tributes to George J. Race, MD, PhD
151
generous heart behind a challenging exterior, he accomplished
much during his lifetime, for which we shall all be grateful.
ALBERT D. ROBERTS JR., MD
George Race was a peripatetic polymath. His energies and
curiosity seemed inexhaustible. He authored many books on
pathology. There was also his collection of old cars and, for a
while, his beloved B25 bomber, such as the one he flew in the
South Pacific and later in the Korean War. Also, he was busy at
his ranch and with a tremendous amount of travel. He was a
member of the New York Explorers Club. He was soft spoken,
always accessible, and a fine pathologist and administrator, an
unobtrusive presence in many venues.
Dr. Race and I were friends and colleagues from the 1960s,
when he was chief of pathology at Baylor and I was practicing
there. Later on, in the 1970s and 1980s, we were colleagues
in academic administration at UT Southwestern; he, associate
dean for continuing education, and I, associate dean for clinical
affairs. I also cherished a friendship with his talented wife, the
late Dr. Anne Race. I miss them both very much.
MARVIN J. STONE, MD
George Race was a multifaceted person: physician, educator, mentor, administrator, scientist, innovator, rancher, aviator, photographer, and explorer. A native Texan, George was
one of the early students at UT Southwestern Medical School,
graduating in 1947 at age 21. He received postgraduate training
at Duke and in Boston and served on the faculty of Harvard
Medical School at the Peter Bent Brigham Hospital.
George returned to Dallas in 1955 and joined the faculty at
Southwestern. He moved to BUMC in 1959, becoming chief of
pathology, a position he held until his retirement in 1986.
With the support of Boone Powell Sr., George built an
expanded, excellent pathology department at Baylor. Longtime
members included Bill Kingsley, Sol Haberman, Weldon Tillery, Norman Helgeson, Allen Marengo-Rowe, Charles Rietz,
Joe Newman, and several women including Gwendolyn Crass,
Freida Carson, Marie Shaw, and Doris Vendrell. George also
served as director of the pathology residency program during
his entire tenure as chief at Baylor. Many practicing pathologists in Texas and surrounding states are graduates of the Baylor
program.
In addition to building pathology at Baylor, George made
three unique contributions to the institution. A gift from Mr.
A. Webb Roberts in 1972 established the Center for Continuing Education, and George became its first dean. Initially, this
was a joint venture with UT Southwestern Medical School,
152
and George directed both programs. In 2012 some 250 CME
activities with 45,000 participants (over 50% physicians) were
sponsored by the A. Webb Roberts Center for Continuing
Education.
Second, George was instrumental in forming the Baylor
Research Institute in 1986. He served as its first chairman with
the assistance of J. Lester Matthews. BRI remains the scientific
research arm of the health care system and currently oversees
more than $20 million in research grants as well as the institutional review board.
Third, in 1988 George established the BUMC Proceedings
and was its first editor-in-chief. In the inaugural issue, he
stated that the journal “is intended to serve as a forum for
scientific communication and education and will include clinical, technical, and research articles; grand rounds; case reports;
and articles related to available medical services throughout
the Baylor Health Care System.” The first article was written
by Ralph Tompsett entitled, “Reminiscing About Penicillin.”
Rose Kraft played a major role in editing the Proceedings and
other publications. BUMC Proceedings has grown in size and
reputation under the leadership of Dr. Bill Roberts. Today
each issue is sent to over 7000 health care professionals free
of charge.
George was a consistently strong advocate of the cancer
program at Baylor and one of the key medical staff members
whose support led to the formation of the Sammons Cancer
Center. When I came to Baylor in 1976 as director of the new
Sammons Cancer Center and chief of oncology, George asked
me to become director of immunology in his department, a
position I held for 35 years. George was active in the American Cancer Society and, together with Dr. Billie Aronoff, gave
Baylor a national presence in cancer care.
George was involved in a number of scholarly activities
as investigator and author. He published over 150 articles in
peer-reviewed journals and was the chief editor of Laboratory
Medicine, a four-volume compendium of clinical pathology that
went through 13 revisions. He also earned a PhD in anatomy
and microbiology and attended law school for a year.
George Race left a huge imprint on BUMC. He often likened its potential to the Harvard hospitals and believed that
Baylor could evolve from “a sleeping giant” into a recognized
major academic center.
George and his lovely wife, Anne, a respected physician in
her own right, were married for 61 years. Not only did they
have distinguished medical careers themselves, but all four of
their living children have become physicians. I know of no other
contemporary family with such a legacy.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Cardiologist in the shadow of Angkor Wat: a medical mission
to Cambodia
John Davis Cantwell, MD
In a medical mission to Cambodia, our team of doctors, dentists, and
nurses saw over 1000 patients during 4 days of clinics. The most common cardiovascular problems were hypertension (11%) and heart murmurs (3%). Obesity and a history of diabetes were very rare. Unlike the
cardiac patients I typically see in my Atlanta office, the Cambodians were
trim and muscular from their predominantly farming and, less often,
construction jobs. They are a gentle, seemingly happy people, appreciative of whatever limited medical help we could offer. Tuberculosis was
the most prevalent serious illness noted.
y knowledge of Cambodia was mainly limited to the
1970s atrocities I had read about: Pol Pot, the Khmer
Rouge, “Killing Fields,” and land mines causing legless children. I had heard of Angkor Wat, felt by some
to be the eighth wonder of the old world. When I heard about
the Flying Doctors of America’s medical mission to Cambodia,
my wife and I signed on, I as a cardiologist and Marilyn as an
aide in the distribution of medications. The team was headed
by Allen Hord, MD, an anesthesiologist and pain specialist,
assisted by Dave Rayburn, EMT. The team included two other
physicians, nurses, dentists, and a chiropractor.
M
CAMBODIA
I tried to learn as much as I could about the country before
we arrived. Twenty hours of flying time (Atlanta to Seoul to
Siem Reap) provided ample opportunity for reading.
About 1000 years ago, the Khmer Empire ruled most of
Southeast Asia between the 9th and 15th centuries. The capital, Angkor, sprawls over 138 square miles and features innumerable temples distributed over 77 square miles, the most
famous of which (besides Angkor Wat) include Angkor Thom,
Ta Prohm (Figure 1), and Banteay Srei. Angkor Thom alone
is spread over 10 square miles and was built by Jayavarman
VII, the greatest Khmer king in the 13th century who converted from Hinduism to Buddhism, a faith followed today by
90% of the people. When a Chinese diplomat visited in 1296
ad, there were at least 700,000 inhabitants of Angkor Thom
(when the populations of Paris and London were <100,000).
Today, the temple, Ta Prohm, brings to mind scenes from the
movie Tomb Raiders, starring Angelina Jolie (who has a special
Proc (Bayl Univ Med Cent) 2014;27(2):153–155
Figure 1. Ta Prohm Temple, used in the Tomb Raiders movie.
interest in landmine removal and even adopted a Cambodian
child).
Cambodia today is a multiparty democracy under a constitutional monarch, King Norodom Sihamoni. The prime minister (for the past 28 years) is Hun Sen, a former member of the
notorious Khmer Rouge.
Cambodia is about the size of Oklahoma, with a population
of 15 million, 75% of whom are farmers. It is a poor country,
with a per capita income of only $2470 (1). Over a third live
in poverty. An estimated 1 of 275 people have been maimed by
landmines. Under the 4-year rule (1975–1979) of Khmer Rouge
and notorious leader Pol Pot, up to 2 million Cambodians died
of starvation, overwork, and execution.
From Piedmont Heart Institute, Atlanta, Georgia.
Corresponding author: John Davis Cantwell, MD, MACP, Piedmont Heart
Institute, 275 Collier Road, NW, Suite 500, Atlanta, GA 30309 (e-mail: john.
cantwell@piedmont.org).
153
Figure 2. Patients awaiting our arrival at an area clinic.
Figure 4. Scars from the application of heated cups, to self-treat pain in the
head, chest, and abdomen.
The fall of the Khmer Empire in the early 1400s was due
likely to invasions, floods, droughts, and a lack of access to
emerging shipping trades (2). Cambodia was remote to the
outside world until the arrival of explorers, including French
naturalist Henri Mouhot, who discovered Angkor and published accounts of his findings in 1868 (3).
POLITICAL CONCERNS TODAY
To compete with factories in China, foreign companies have
been heading to Cambodia. Between 2011 and 2012, foreign
direct investments increased by 70%. National elections on July
28, 2013, produced claims of widespread cheating and threats
of mass protests, owing to thousands of temporary “identification cards” that voters required. Forests are being chopped
down and burned to make charcoal. Large sugar plantations
are confiscating individual homes at subpar prices and selling
their products largely to Europeans, who enjoy duty-free access.
Cambodian and Thai troops have clashed in recent years over
ownership of land and temples along the border, an area near
where one of our clinics was held.
MEDICAL PREPARATION
Each of us was given a large shopping bag full of medications and supplies we took with us and assembled at the hotel
in Siem Reap. We were advised to get typhoid shots, to take
atovaquone-proguanil (Malarone) for malaria protection, to
spray our clothing with Permethrin, and to apply DEET to
exposed skin areas to help protect against dengue fever. It was
not very reassuring that a current guidebook advised us to “get
a blood test if you suspect you have dengue fever, as there is a
fatal variety that does not need to be treated” (1). We also took
ciprofloxacin and metronidazole in case we got traveler’s diarrhea and used standard precautions since HIV/AIDS and tuberculosis were common. Upon our return, we added mebendazole
to protect against worm infestations.
THE MEDICAL MISSION
Our medical team was busy, seeing a total of over 1000
patients in 4 days of clinics, with about 20% of the cases being
dental. We visited four different sites (Sre Nouye, Chanleasdai,
Svay Chek, and Srogne). Patients were waiting for
us upon our arrival (Figure 2). Our facilities were
adequate (Figure 3), except for the lack of sinks and
running water.
Medical histories were hard to obtain, even
with fairly good translators. Important aspects of
chest pain, such as precipitating cause, duration,
etc., were vague at best. Only 1% of patients I saw
had histories consistent with angina pectoris. Eleven
percent were hypertensive. Heart murmurs were
heard in 3%. One of the latter, a diffuse grade 3/6
murmur, was likely due to mitral regurgitation, as
the carotid upstroke was normal and the murmur
did not change on the beat after an ectopic beat.
Another was most likely a bicuspid aortic valve with
aortic stenosis and aortic regurgitation. A 14-yearold girl had clubbing of the fingers and toes and
a diffuse grade 3 systolic ejection murmur spillFigure 3. (a) My medical office and (b) my wife, Marilyn, who helped in medication packaging ing over in diastole; she likely had a bidirectional
shunt with Eisenmenger physiology and possibly
and distribution.
154
Baylor University Medical Center Proceedings
Volume 27, Number 2
6 years ago and has 5 full-time medical doctors and 7 part-time ones to
care for up to 30 patients. I met with
Dr. Kamol Prinyanusom, a general
medical doctor and head of marketing. He indicated that they average
about one myocardial infarction per
month. They lack an on-site cardiologist but consult via the Internet
with cardiologists in Bangkok and
administer streptokinase when appropriate. Critically ill cardiac patients are transported 40 minutes by
plane or helicopter to Bangkok, and
they recalled three such transports
in the past year. They have an automatic external defibrillator, but lack
electrocardiography, treadmill, and
bicycle testing and do not provide
Figure 5. Dr. Uy Chanthol, the only “adult heart doctor” in Figure 6. Defused mines at the Landmine Museum.
cardiac rehabilitation.
Siem Reap, Cambodia, with his echocardiogram machine.
The hospital was immaculate
and seemingly catered to the more
tetralogy of Fallot. A handheld echocardiogram would have
affluent Cambodians and tourists. It was about to open an “antibeen useful.
aging” facility in conjunction with a center based in San Diego,
The internist asked my opinion about a 53-year-old lady
California, which will utilize chelation, cleansing enemas, and
with a cough and bibasilar rales. Her neck veins were a little
other alternative health measures.
distended and her apical impulse was displaced and diffuse. I
felt she did have mild heart failure, most likely due to a carTHE LANDMINE MUSEUM AND DEPARTURE
diomyopathy, as she lacked a murmur. Obesity was seen in
We did visit the Landmine Museum early in our extra time
<1%, as most patients were hardworking farmers and a few
and saw the thousands of defused mines that had been detected
were construction workers, subsisting on a largely rice-based
(Figure 6). A school accompanies the museum and initially
diet. Application of heated cups (Figure 4) was fairly common
focused on children who were missing appendages because of
to treat various pains in the head, chest, or abdomen. Goiters
landmines, but it now has mainly polio victims and other diswere rare, as was a history of diabetes.
advantaged individuals. An estimated 820,000 antipersonnel
Back in Siem Reap, I met with Uy Chanthol, MD (Figure 5),
mines, 20,000 antitank mines, and 1.7 million unexploded
the only “heart doctor” for a metropolitan area well over
ordinances were removed between 1992 and 2008. A local hero,
125,000. Dr. Chanthol is 41, trained primarily as a psychiaAki Ra, initially removed thousands of mines, using just a stick
trist. Because many of his psychiatric patients had symptoms
and a pair of pliers.
seemingly cardiac in origin, he recently took a 6-month intenWe celebrated the end of our enjoyable medical and dental
sive cardiology training course in Seoul, learning electrocardimission in the Elephant Bar of the famous Raffles Grand Hotel,
ography and echocardiography. He spends mornings overseeing
anxious to fly home before the arrival of typhoon Haiyan. On
the intensive care unit at the Siem Reap Provincial Hospital,
the plane, we met several members of the Johns Hopkins Carwith 5 to 7 patients at present, and afternoons in his small office,
diac Surgical Mission to the Jayavarman VII Children’s Hospital
seeing up to 10 patients. He states that he has a defibrillator in
in Siem Reap. Their team included pediatric cardiologist Bill
the intensive care unit and is “learning to use it.”
Rauckes, MD, and surgeon Luca Vricella, MD, who had repaired
I tried to ask older patients what their lives were like under
13 congenital cardiac maladies in the prior week.
the Khmer Rouge period. Many had had parents, siblings, and
1. Vater T. Angkor Wat. Berkeley, CA: Moon Handbooks, 2013.
spouses killed for no good reason.
2. Stone R. Divining Angkor. National Geographic 2009;220:27–55.
The last day I visited the Royal Angkor International Hospi3. Ray N, Bloom G. Cambodia. Oakland, CA: Lonely Planet, 2012.
tal, part of the Bangkok Hospital network. The hospital opened
April 2014
Cardiologist in the shadow of Angkor Wat: a medical mission to Cambodia
155
A tale of Congress, continuing medical education, and the
history of medicine
Clyde Partin, MD, Howard I. Kushner, PhD, and Mary E. Kollmer Horton, MPH, MA
Well-intentioned attempts by the Senate Finance Committee to improve
the content and quality of continuing medical education (CME) offerings
had the unanticipated consequence of decimating academically oriented
history of medicine conferences. New guidelines intended to keep CME
courses free of commercial bias from the pharmaceutical industry were
worded in a fashion that caused CME officials at academic institutions
to be reluctant to offer CME credit for history of medicine gatherings. At
the 2013 annual conference of the American Association for the History
of Medicine, we offered a novel solution for determining CME credit in
line with current guidelines. We asked attendees to provide narrative
critiques for each presentation for which they desired CME credit. In this
essay, we evaluate the efficacy of this approach.
In 1957, Guthrie spoke of the history of medicine as
a means, perhaps the only means, of reuniting a profession
now so fragmented by many specialties, a means of reviving
the wide outlook of former times. . . . Never before, in the long
evolution of medicine, has there been a time when there was
greater need for retrospection—for looking back, in order that
we may be better qualified to look forward (1, 2).
Physicians and academic historians of the history of medicine
meet and discuss their research, but well-intentioned attempts
by the Senate Finance Committee to improve the content and
quality of continuing medical education (CME) offerings have
had the unanticipated consequence of decimating academically
oriented history of medicine conferences. This article outlines
efforts to allow CME credit at those meetings following the
changes in CME guidelines.
CME IN HISTORICAL CONTEXT
The genesis of CME in the United States is largely the result
of the efforts of the Mayo brothers, Charles and William. Visiting surgeons, anxious to incorporate novel surgical techniques,
traveled to the Mayo Clinic in Rochester, Minnesota, to learn
about surgical progress. Eventually these itinerant surgeons
created a Surgeons Club, which “partook in vigorous daily discourse regarding new techniques being advanced” (3). In 1927,
the Clinical Week, “the prototype of the modern CME course,”
began, which evolved into today’s popular clinical reviews at
156
the Mayo Clinic (3). Other medical schools and eventually
specialty societies embraced the CME torch. The American Urological Association initiated the first mandatory CME program
in 1934. By 1957, the American Medical Association (AMA)
had published the first set of CME guidelines. However, in the
1970s, “the political predominance of the AMA in continuing
education was questioned by other professional associations”
(4). As a result, in 1981, a successor to the AMA’s Liaison Committee on CME—the Accreditation Council for Continuing
Medical Education (ACCME)—was formed.
This council, with guidance from various educational and
professional groups, was a step forward in the professionalism and quality of CME. From this vantage point, the rather
constitutional-sounding declaration is found: “The ACCME
accreditation process is of, by, and for the profession of medicine” (5). Standards to assess accreditation requirements ensued, such as the Seven Essentials in 1982. By 1998, the revised
System98 “encouraged accredited providers to focus on CME
that linked educational needs with desired results, and to evaluate the effectiveness of their CME activities in meeting those
educational needs.” By the early 21st century the ACCME
positioned itself “to support US health care quality improvement efforts and to align with emerging continuing professional development systems to support US health care quality
improvement efforts” (5).
CME system challenged
This seemingly bucolic and utopian situation for CME and
the American medical education system was eventually challenged by the US Congress. In a 2007 letter from Senator Max
Baucus, chairman of the Committee on Finance, and ranking
committee member Senator Charles Grassley, addressed to Dr.
Murray Kopelow, chief executive for the ACCME, the senators
noted that “the pharmaceutical industry spends more than a
billion dollars a year to fund CME programs that are accredited
by the ACCME” (6). The letter harshly criticized the ACCME
for poor oversight of CME activities and failure to adequately
From Emory University, Atlanta, Georgia.
Corresponding author: Clyde Partin, MD, Associate Professor of Medicine,
Emory University School of Medicine, Emory Clinic, 1365 Clifton Road, First Floor,
Atlanta, GA 30322 (e-mail: clyde.partin@emoryhealthcare.org).
Proc (Bayl Univ Med Cent) 2014;27(2):156–160
limit bias in big pharmaceutical companies’ CME activities and
indicated that the ACCME focused on the
documentation surrounding the process for funding and creating CME activities, as opposed to the substance of the activities themselves. For example, it does not appear that ACCME
review involves analyzing the contents the educational activities
created for accuracy, to determine whether the activities include
a fair and balanced discussion of competing therapeutic options, or whether the activities favor products manufactured
by the commercial sponsor (6).
By extension, one can see the implications: the integrity of
clinical trials, biased and tainted dissemination of knowledge,
and the degradation of the very fabric of trust between physician, patient, and society. From this perspective, the notion that
the abyss-like pockets of the pharmaceutical industry are funding CME at fine restaurants, ski resorts, and cruises is unsavory
to contemplate. More troubling is the conflict of interest that
is inevitable in presentations of industry-sponsored research of
principal investigators whose research is often also funded by the
National Institutes of Health (NIH). Such potential conflicts of
interest fueled the skepticism of the Senate Finance Committee
about the role and independence of the CME enterprise.
In the spirit of engaging this congressional criticism, the
ACCME developed the descriptions and guidelines that appear
in the box below (7). Unfortunately, CME offices across the
country, faced with increasing scrutiny and threats of probation
Continuing medical education consists of educational activities which serve
to maintain, develop, or increase the knowledge, skills, and professional
performance and relationships that a physician uses to provide services for
patients, the public, or the profession. The content of CME is that body of
knowledge and skills generally recognized and accepted by the profession
as within the basic medical sciences, the discipline of clinical medicine, and
the provision of health care to the public.
ACCME Note:
The definition below describes the content that the ACCME considers
acceptable for activities developed within an accredited provider’s
CME program. The ACCME definition of CME is broad, to encompass
continuing educational activities that assist physicians in carrying out their
professional responsibilities more effectively and efficiently. Examples of
topics that are included in the ACCME definition of CME content include:
• Management, for physicians responsible for managing a health care
facility
• Educational methodology, for physicians teaching in a medical school
• Practice management, for physicians interested in providing better
service to patients
• Coding and reimbursement in a medical practice
When physicians participate in continuing education activities that are
not directly related to their professional work, these do not fall within
the ACCME definition of CME content. Although they may be worthwhile
for physicians, continuing education activities related to a physician's
nonprofessional educational needs or interests, such as personal financial
planning or appreciation of literature or music, are not considered CME
content by the ACCME.
Figure. CME content: definition and examples. Source: ACCME (7).
April 2014
for inappropriately awarded CME credit, began refusing to offer
CME for history of medicine seminars. This contrary action by
institutional CME boards continues despite the language outlined by the ACCME, which provides support for the history
of medicine as an avenue for legitimate intellectual inquiry and
study serving to benefit the practice of medicine.
THE CHALLENGE OF CME FOR MEDICAL HISTORIANS
What are physician historians of medicine to do? Caught
in the cross-hairs of a skirmish involving the pharmaceutical
industry, well-intended congressional members, and the formal
CME enterprise, physician historians of medicine have become
victims of unintended collateral damage. What is at stake?
Dollar-wise, not much. Money spent on academic history of
medicine conferences is a mere pittance compared to the cascade
of dollars involved in NIH grants and pharmaceutical funding
for drug research and development and drug trials. Most history
of medicine conferences receive no pharmaceutical industry
funding. Depending on the particular conference, a variable mix
of PhD graduate students, history professors, lawyers, librarians,
physicians, and a slowly increasing breed, an MD with a PhD in
history, attend these gatherings. A drug company representative
is hard to find under these circumstances, although rare book
dealers often set up shop on the environs.
What is at stake is the long and fruitful intercourse between
physicians and historians of medicine, and the resulting benefit
to patients and society. Note the opening paragraph of a recent
article in the New England Journal of Medicine:
Over the past half-century, historians have used episodes of
epidemic disease to investigate scientific, social, and cultural
change. Underlying this approach is the recognition that disease, and especially responses to epidemics, offers fundamental
insights into scientific and medical practices, as well as social
and cultural values. As historian Charles Rosenberg wrote,
“disease necessarily reflects and lays bare every aspect of the
culture in which it occurs” (8).
In the swirling winds of discontent and the increasingly politicized milieu in which medicine is practiced today, the profession
of medicine would do well to understand its roots and its role in
society and to account for how we have arrived at the current state
of affairs. As Harvard historian Peter Bol sagely observed:
How do I know the historian’s mind-set when I see it? I know
it because it’s somebody interested in how things change over
time, but not just that. They’re also interested in the problem of
how things change over time. And how to account for change
over time (9).
CME AT THE AAHM 2013 ANNUAL MEETING: TOWARD A
NEW PARADIGM
Confronted with this disconnect between CME and history of medicine scholarship, a group of scholars, including
these authors, hosting the 86th annual meeting of the American
Association for the History of Medicine (AAHM) in May 2013
offered a novel solution to the predicament. As it seemed almost
A tale of Congress, continuing medical education, and the history of medicine
157
an ethical conflict at worst and difficult at best to declare, seemingly arbitrarily, ahead of time whether a presentation may or
may not meet the criteria for awarding CME credit, the authors
of this paper shifted that burden to the physician seeking CME
credit. We asked the attendee: “Describe how this presentation addressed your current practice-based needs: How will you
use the information presented to 1) change/impact how you
care for your patients; or 2) improve your medical administrative skills; or 3) enhance your research skills.” In other words,
credit would be based on physician response.
With open-minded and close collaboration among the host
university CME office, the national office of the AAHM, and
the ACCME, an agreement was forged to pursue this approach.
Through the support and collaboration of the chair of the institution’s CME committee, we reached a suitable mechanism
for providing CME for physicians attending the AAHM meeting. Members of the local arrangements committee of the host
institution also reviewed the process and supported it. While an
online submission process for physician attendees seeking CME
credit was preferred, time and finances led in this case to a paper
submission process. The revised rules of the national ACCME had
been the barrier preventing participants in history of medicine
meetings from obtaining legitimate credit. Once approved by the
national offices of the AAHM and the ACCME, this hurdle had
become surmountable, and the work became logistical.
It is beyond the scope of this article to persuade the reader
of the value of studying the history of medicine. Rather, the
article focuses on the quandary of awarding CME at history of
medicine conferences. Others have written eloquently of this
struggle. Prior to the 2010 AAHM annual meeting in Rochester,
Minnesota, Bruce Fye, former president of the American College of Cardiology, wrote in a letter in support of CME:
History teaches many valuable lessons that can be incorporated
into medical practice. The history of medicine serves several
useful functions today, when doctors live and work in an environment of escalating expectations, eroding autonomy, and
decreasing discretionary time. Understandably, many doctors
are concerned about the future of medicine as they watch so
many powerful political, economic, and social forces transform
medical practice, research, and education (10).
Jacalyn Duffin, a physician, author, and passionate supporter of
the history of medicine, chronicled the CME quest, observing:
Not only does it illustrate how current standards came into
existence; its pursuit is a mirror of clinical practice. History is
predicated on the idea that things change. It proclaims the importance of life-long learning; its method—question, evidence
and interpretation—reflects diagnostic reasoning (11).
Her book, Clio in the Clinic: History in Medical Practice,
brings a pragmatic realism to the history of medicine in the
form of applied medicine (12). Physicians particularly enjoy
case-based approaches. History of medicine can be taught that
way, a method epidemiologists and public health officials use to
good effect. For example, Kushner’s work on Kawasaki’s disease,
which involved reapplying an updated case definition, allowed
158
clinicians to recognize late effects of the disease that had been
missed (13). That is applied history and a reason to keep teaching history of medicine for CME credit. This is not your father’s
history of medicine paradigm.
Numerical results
To the authors’ knowledge, this is the first large-scale effort
implementing this type of CME approach. Since there are no
prior data, we elected to examine our acquired information to
see what we could discover, as quantification may shed light on
a subject when least expected. Einstein has noted in a quote inconclusively attributed to him, “Everything that can be counted
does not necessarily count. Everything that counts cannot necessarily be counted.” On the other hand, “Academics always want
to show we’re serious these days by talking numbers. And two
problems arise when we do that. We get the numbers wrong, and
we forget that numbers can’t tell us everything” (14). Regardless,
numerical data can be an instructive and informative start.
The conference was attended by 351 registrants, of whom
26 (7%) were MDs. Of the physician registrants, all submitted
requests for CME credit. Credit was based on a narrative summary of each presentation for which credit was requested. A
total of 370 narrative statements were submitted and studied by
a physician from the host university in charge of CME for this
annual meeting, as designated by the AAHM. From this review
of individual presentation requests, 56% were accepted and
44% were rejected. The average was 14.2 requests per physician,
with a range of 3 requests (2 people) to 28 requests (1 person).
Eight physicians submitted 21 or more requests. The highest
acceptance rate was 100% (3 of 3). The lowest acceptance rate
was 0% (0 of 12 and 0 of 3).
The primary reason for CME rejection was failure to follow
the instructions: “Describe how this presentation addressed your
current practice-based needs. How will you use the information
presented to 1) change/impact how you care for your patients;
or 2) improve your medical administrative skills; or 3) enhance
your research skills.” The specific failure was documenting how
the talk could be utilized to enhance skills in the three categories
above. Most rejections resulted from the applicants limiting their
remarks to a simple summary of the presentation. There were
two rejections for illegibility. Of the submissions approved, 45%
were approved for patient care, 27% for medical administration,
and 21% for research. A handful, 7%, were approved in multiple
categories. The Table provides samples of the responses.
Approximately 130 talks were delivered in the academic sessions. The lunch sessions, the Fielding Garrison Lecture, and the
plenary session featuring two internationally prominent public
health physicians were not included. This was an administrative
oversight, as the forms were not provided in those locations. The
academic sessions lasted 90 minutes and typically featured three
speakers and sometimes two or four. The maximum number
of talks one could attend was about 36. Thus, the maximum
possible number of awarded CME hours was 18 hours at the
rate of 0.5 CME hours per presentation. For this meeting, the
maximum number of CME hours actually awarded to a participant was 10 hours. That person submitted 23 requests, of
Baylor University Medical Center Proceedings
Volume 27, Number 2
Table. Examples of narrative critiques and the associated CME outcome
Category
Quotes
Offered no substantive reasoning
as to why the presentation was
useful; rejected for CME credit
• Beautiful preamble on the history of vaccines—very related to my interests.
• Very interesting epidemiologic data on clothing and infectious disease.
• Helpful presentation for clinician-historians.
Provided substantive reasoning;
received CME credit
• Wow! A beautiful example of how a good observer who questions assumptions can discover something entirely new.
Teaches me to look past assumptions.
• I am a physician and historian; understanding the origins and controversies regarding disciplinary boundaries’ history
is crucial for my teaching and for my knowing how to bridge disciplinary boundaries in my medical school teaching—
where I will be teaching about the non-“science” factors in the development of medical specialties—as well as in
practice in collaborating in care with other specialties.
• Reinforces clinical inclination to have a great skepticism about surgical referral unless one has positive knowledge of a
surgeon’s skill and judgment.
• Use to consider timing of medications.
• Increased perspective on duty-hour limitations and stresses on medical trainees.
• Thoughtful analysis of the epidemiology of CHD [coronary heart disease] this past century. Helps me to think about
changing risk factor profiles in my patients over those decades.
• Great paper! Raises issues of celebrity endorsements of public health initiatives and potential personalities to distort the
real agenda through pseudo-scientific arguments.
• Contemplate play as a therapeutic intervention. Contemplate human reflex to mock disability embedded in children’s games.
• An important discussion about malaria, health, control and treatment. It brought out the need to explore humanism in
the care and treatment of this disease for the overall public health. Should help me understand and incorporate humanism into the care of patients. This is also important to medical administration skills and expands my understanding of
public health research. Also illustrated the importance of cost and value in health.
• Raised issues about the real health aspects of obesity on medical care and health in general that will help me address
obese patients in practice and the true impact of their weight on their health.
• Henle-Koch causal rules—it was nice to put a name to this idea. I am often disabusing patients of causal relationships
based on their faulty connections between two events with only a temporal relationship which does prove causality. I
frequently review causality with my patients. I can do so more confidently now. I also give talks that rely on data from
observational epidemiology—where causality is typically controversial.
• Narcotic prescription writing is often a distasteful and unpleasant problem in my office. I am reminded to maintain a skepticism
of complaints, seek objective evidence to support my diagnosis behind the pain and be alert, as always, for diversion.
Substantive comments on
socially and politically charged
topics showing the clinically
empowering information imparted; received CME credit
• Evolution of patient-centered choice in sperm selection—interesting case study for any patient-centered approach—
social forces of women’s health movement and gay-lesbian movement.
• Fascinating discussion of drug and pharmaceutical policy. Makes one reconsider the impact of racism on drugs of choice.
• This session was informative for my medical school teaching in the medical humanities, particularly the medicalization
of social problems, the stigmatizing of poverty and “otherness” and the ways medical interventions have been used
(disproportionately to certain groups in the population) punitively. It will inform my practice especially regarding the differential tendency to medicalize (or dismiss) particular conditions differently in different populations (health disparities).
• The interaction of the drug industry and the tobacco industry on recommendations to quit smoking for all patients will
help me counsel my own patients concerning tobacco use.
• The stress for women over the years in assessing appropriate pregnancy options—including abortion—continues into the
present. Helping my female patients cope with present and past trauma related to this will be helped by understanding the
political climate concurrent with their traumas.
which 20 (87%) were approved. The average number of CME
hours awarded was 3.98 hours. Had all 370 CME requests been
granted, the average would have been 14.23 hours per physician
requestor. Fourteen talks did not elicit a request for CME.
Follow-up
In retrospect, we realized that one category was noticeably absent from the form: teaching. We believe that should physicians
learn something or discover information that does not clearly fit
April 2014
into the above categories but enhances their ability to teach medical
students, residents, or colleagues, they should be awarded CME
credit. Informally, the reviewers noted 13 critiques that could have
stood on their own merit as enhancing teaching. When we later
included teaching as an option for CME compliance at the Annual
J. Willis Hurst Symposium, held at Emory University School of
Medicine in September 2013, the results were similar to those at
the earlier AAHM conference. At the Hurst Symposium, 41 of 59
attendees (69%) submitted 179 critiques, of which 91 (51%) were
A tale of Congress, continuing medical education, and the history of medicine
159
approved. An average of 1.11 CME credit hours (range 0-3) was
awarded. Despite a brief PowerPoint display explaining the new
criteria and procedures, failure to follow directions was again the
primary reason for denial of CME credit.
Lessons learned
One downside to this CME approach is the labor involved
in reviewing the critiques. Yet for one arbitrator, who soldiered
through 370 handwritten reviews of widely varying but mostly
poor penmanship quality, the experience was heartwarming and
informative. A common positive theme among the responses,
especially for politically charged and socially complex topics
such as abortion, gender issues, sexual orientation, and drug
abuse issues, was the implication that the physician, possessed
of this historical background knowledge, felt more empowered,
confident, and informed when talking with patients personally
struggling in these areas.
needs. The ACCME accreditation process is of, by, and for the
profession of medicine (5).
We will also be happy to hear from the US Senate regarding
our progress.
Acknowledgments
The authors wish to acknowledge the support and advice of
Arnold Berry, MD, Emory’s director of CME, and Ms. Melissa
Boone, Emory University CME manager, who were willing to
explore and support this novel CME adventure.
1.
2.
3.
4.
DISCUSSION
In our view, this CME experimental protocol with a premier
national history of medicine conference, retested at a focused
medical history symposium, was a success. Greater attention to
following the rules for submitting CME requests would have
led to enhanced success at both meetings. We hope the AAHM
continues to use and refine this method and that other history of
medicine gatherings adopt similar tactics. One future improvement will involve transitioning to an online submission format.
However this process evolves, we feel we have made a significant
and positive impact on validating the CME process for history
of medicine gatherings. In doing so we think we have complied
with the laudable and stated aims of the ACCME as follows:
The ACCME’s purpose is to oversee a voluntary, self-regulatory process for the accreditation of institutions that provide
continuing medical education (CME) and develop rigorous
standards to ensure that CME activities across the country are
independent, free from commercial bias, based on valid content, and effective in meeting physicians’ learning and practice
160
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
Guthrie D. Whither medical history. Med Hist 1957;1(4):307–317.
Burnham JC. A brief history of medical practitioners and professional historians as writers of medical history. Health & History 1999;1:250–273.
Feely MA. The Mayo brothers and the history of continuing medical education at the Mayo Clinic—in pursuit of lifelong learning. In Abstracts: 40th
Annual Meeting of the American Osler Society, April 26–29, 2010, p. 27.
Josseran L, Chaperon J. History of continuing medical education in the
United States. Presse Med 2001;30(10):493–497.
ACCME. Our history. Available at http://www.accme.org/about-us/ourhistory.
Baucus M, Grassley C, US Senate Committee on Finance. Letter to Murray
Kopelow, chief executive, Accreditation Council for Continuing Medical
Education: April 25, 2007. Available at http://www.finance.senate.gov/
newsroom/ranking/release/?id=637bd77c-508f-489d-84fd-133c94e6ea3b.
ACCME. CME content: definition and examples. Available at http://www.
accme.org/requirements/accreditation-requirements-cme-providers/policies-and-definitions/cme-content-definition-and-examples.
Brandt AM. How AIDS invented global health. N Engl J Med
2013;368(23):2149–2152.
Heller N. Laptop U. The New Yorker 2013;89(14):80–91.
Fye WB. Mayo CPD category 1 credit application. Copy provided by the
author, 2009.
Duffin J. Lament for the humanities in continuing medical education.
CMAJ 2011;183(12):1452.
Duffin J. Clio in the Clinic: History in Medical Practice. Toronto: University
of Toronto Press, 2005.
Kushner HI. History as a medical tool. Lancet 2008;371(9612):552–
553.
Grafton AT, Grossman J. The humanities in dubious battle. Chronicle of
Higher Education 2013(July 5):25–26.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Mentoring: a tale of two poems, filling graveyards, and
learning the art of medicine
Clyde Partin, MD
Polar approaches to mentoring are reflected in this pair of poems, which
on first inspection appear to be unrelated. Mentoring comes in different
forms, and combining medicine, mentoring, and poetry in one essay is an
opportunity to explore the vital role mentoring plays in medical education.
A nod toward the humanistic side of medicine is also illuminated by the
selected poetry and associated discussion.
his essay reflects on two poems that initially seem unrelated and unconnected, but upon further scrutiny
demonstrate complementary ideas about teaching and
mentoring in medicine. The first poem, “The Surgeon” by
Alicia Suskin Ostriker (1), tells the story of a surgeon reminiscing about his internship and a red-headed young woman who
unexpectedly died in the midst of surgery. The second poem,
“The Ropes” by Kimberly Manning (2), renders a more personal
teaching experience. The first poem is from the viewpoint of the
mentored, and the second, from that of the mentor.
Ostriker’s poem arrests our attention with an evocative
metaphor as the surgeon, feeling raw and vulnerable at the
unanticipated demise of his patient, recalls that he
T
Shook
Like a car with a broken axle.
Seeking solace from the head surgeon, he is advised:
You got to fill a graveyard
Before you know this business
And you just did row one, plot one.
I once heard Emory University poet Kevin Young mention
a lesson given to him by the Irish poet Seamus Heaney. To end
a poem, “tuck it in,” Heaney taught. Only in a cemetery could
one find an ending tucked in any tighter than Ostriker’s. In the
past, when I have read this poem to others, their facial expression dissolved into an inaudible gasp more seen than heard the
moment I finished reading the poem.
“The Surgeon” was also published in the journal Academic
Medicine (3) accompanied by a rumination on the poem by a
family medicine residency director, Dean Gianakos (4), whose
insight and curiosity about the poem mirrored my own. Who
was this surgeon? Where did Ostriker encounter him? Was he
Proc (Bayl Univ Med Cent) 2014;27(2):161–162
an uncle or avuncular friend of the family reminiscing one
night while sharing a table and some wine with Ostriker? This
reviewer and I both noticed the frosty pronoun that is the genesis of the following line, as if dehumanizing the red-headed
woman could put some emotional distance between him and
her death, “its” death.
It was a young red-headed woman.
The past tense is all too poignant here, as his patient will
never have the chance to be old, or gray-headed. A medical
student with whom I was reviewing this poem wondered aloud
if “it” could be synonymous with death: Death was a young
red-headed woman.
The medical sociologist Joe Lella argued that “in a discussion of poetic endings, the effect of this one and the shock it
might have produced in the intern led to a consideration of
the ways and means of imparting ‘lessons’ on how to deal with
the life and death situations of doctoring. Whether saying you
just began filling your physician’s graveyard was a good way of
doing it as the mentoring surgeon did in the poem will prompt
varied opinions from readers” (personal communication, April
7, 2013, annual meeting of the American Osler Society).
Some background helps put this poem in perspective. It
comes from the 70-page-long The Book of Seventy (1), written
by a poet entering “the territory of seventy and beyond.” Accordingly, poems remarking on “death’s certainty” enliven the
collection. Ostriker reported that she wrote about “the body in
sickness and health” (5). Described as a Jewish feminist revolutionary and a “most fiercely honest poet,” Ostriker attacked her
70s the same way she tackled her life, with fervor, energy, and
without reticence regarding her waning time. Other poems in
this first section of the book include “Insomnia,” “Lymphoma,”
and “Neurologist.” The poet Ingrid Wendt observed that these
poems are focused “on health and illness, the diminishments
and degradations of aging, the many things that can and do go
wrong with our earthly bodies” (6). Consider Ostriker’s poem
From the Department of Medicine, Emory University School of Medicine, Atlanta,
Georgia.
Corresponding author: Clyde Partin, MD, Emory Clinic, 1365 Clifton Road NE,
First Floor, Atlanta, GA 30322 (e-mail: clyde.partin@emoryhealthcare.org).
161
“Almanac” (1) about a dancer absorbing a biopsy report gone
wrong:
How can this be
Happening to me
I did everything right.
No doubt this is self-insight on Ostriker’s own publicly acknowledged skirmish with breast cancer, which is further addressed in
her essay “Scenes from a Mastectomy” (7) and the collection “The
Mastectomy Poems,” a section in a larger work called The Crack in
Everything (8). These mastectomy poems emanate powerful images
and compelling feelings and remind us of the indelible link between
the human spirit, art, and medicine. One cannot help but empathize
with Ostriker’s emotions shared in the following poetic excerpts:
And you have already become a statistic,
Citizen of a country where the air,
Water, your estrogen, have just saluted
Their target cells, planted their Judas kiss,
Inside the Jerusalem of the breast (“The Bridge,” p. 85 [8]).
What my husband sucked on
For decades, so that I thought
Myself safe, I thought love
Protected the breast (“What Was Lost,” p. 90 [8]).
Today I’m half a boy,
Flat as something innocent, a clean
Plate, just needing a story (“Wintering,” p. 93 [8]).
These poems and their message mentor us.
The poem we next untie is “The Ropes” by Kimberly Manning, a physician educator at Atlanta’s Grady Memorial Hospital. The synergy between the two poems and their authors
gradually became evident to me as I considered how conclusively
Manning tucked in her ending. Dr. Manning, herself only a bit
beyond halfway to 70, is a popular and vibrant professor in our
medical school. In her poem, she proposed to teach by showing
her students the ropes. She got in her own zinger of a metaphor
when she conquered a diagnostic challenge:
Listen as I share with you stories of ropes I’ve seen
The impossible ones that I unraveled
When no one else could.
Earlier in the poem she demonstrated appreciation for both
patient and student of medicine:
suddenly I freeze
Realizing that
I am the ropes.
As a metaphor for learning, ropes are tied to history. In the
nautical world, a sailor had to master many knots and understand which rope controlled what sail. Learning the ropes was
crucial to survival on the high seas. So to learn the ropes of
medicine, to teach the ropes of medicine, and to be the ropes
is a connection all encompassing for this poet. She envisioned
herself as “the ropes” in the same way she saw herself in her advisees and recognized the need to make sure they learn medicine
in the best fashion possible.
Ostriker had her own thoughts on her role as an educator:
“Teaching is extremely important to me; my students are important. I try my best to awaken them to the delight of using their
minds” (5). In the same manner that Ostriker is characterized as
a “most fiercely honest” poet, while listening to Manning lecture
at grand rounds I see that same spirit. I marvel at her delivery
as she revels in her womanness, her motherness, her AfricanAmericanness, her medicalness, her sense of selfness. She wears
all this this-ness on her white coat like an autobiography sewn
on her sleeve, a sartorial accoutrement for all to witness and for
her students to emulate. This is poetry at its best by kindred
poets, using their verse to teach and mentor.
Acknowledgment
The author thanks Dean Dianakos, MD, Karen A. Stolley, PhD, Michael Lubin, MD, and Stacia Brown, PhD, who
reviewed this manuscript.
1.
Hands pressing into carefully exposed flesh
Mine first, then yours
Both of us smiling at the person
To whom what is being palpated belongs
Appreciative for this teachable moment
Whilst remembering who provided it.
2.
3.
4.
5.
6.
There is a pleasing possessive complexity engendered by
Manning’s description of the anatomy being palpated. For just
that teachable moment, it is as if the patient bestows to the student
joint ownership of the palpated part for all to appreciate.
162
The author shared with me this sentiment regarding “The
Ropes”: “I wrote this poem after reflecting on how powerful role
modeling is in medical education. The more I think about it,
the more I recognize that the best thing I can do as an educator
is to be intentional as a role model and a responsible steward
of my influence. I ‘see myself ’ in my advisees all the time. This
is both terrifying and gratifying” (personal communication,
March 4, 2013).
Above all this poem is about mentoring—though mentoring of a kinder and gentler nature than the blunt mentoring of
“The Surgeon.” Manning is simultaneously learning the ropes
and teaching the ropes, functioning exquisitely as her own automentor. Let her say it in an ending that “tucks it in” tighter than
any knot any sailor ever tied:
7.
8.
Ostriker AS. The surgeon. In The Book of Seventy. Pittsburgh, PA: University
of Pittsburgh Press, 2009.
Manning KD. The ropes. Ann Intern Med 2012;156(5):398.
Ostriker AS. The surgeon. Acad Med 2011;86(6):724.
Gianakos D. Commentary. Acad Med 2011;86(6):725.
Poetry Foundation. Alicia Ostriker. Available at http://www.poetryfoundation.
org/bio/alicia-ostriker.
Wendt I. Alicia Ostriker and Marilyn Krysl: Review. Valparaiso Poetry
Review 2011;12(2). Available at http://www.valpo.edu/vpr/v12n2/v12n2prose/wendtreviewostrikerkrysl.php.
Ostriker A. Scenes from a mastectomy. Acad Med 2007;82(12):1196–1197.
Ostriker A. The mastectomy poems. In The Crack in Everything. Pittsburgh, PA: University of Pittsburgh Press, 1996:83–99.
Baylor University Medical Center Proceedings
Volume 27, Number 2
HIPAA: a flawed piece of legislation
Allen B. Weisse, MD
physician who always insisted that, as a sign of respect, his
office staff address patients by their surnames arrives one
morning to find that, to conceal identities, someone like
“Mr. or Mrs. so-and so” is now being greeted as “Harry”
or “Mary” or, worse, “Grandpa” and “Granny.”
A physician well known to the local pharmacy writes a prescription for his wife, who drops it off on her way to work. Shortly
thereafter, the pharmacy calls about a problem concerning it. The
physician, who is home alone at the time of the call, offers to resolve
the problem. Despite the fact that he had written the prescription, he
is informed that the pharmacy will speak to no one but his wife.
A neurologist arrives on a medical ward to perform a consultation. All the charts on the chart rack are turned facing the wall
so that no names are visible on viewing it. He must then remove
each one individually until he finds the name of the patient on
the proper chart.
A physician has brought his pet dog to the local veterinary
hospital to have certain blood work performed. The next day he
calls to determine the results of this testing, but they will not be
revealed to him unless he appears at the hospital with proof that
he is, indeed, owner of the “patient.”
In collecting these bizarre vignettes occurring after the 1996
passing of Public Law 104-191, better known as the Health
Insurance Portability and Accountability Act (HIPAA), and
then complaining about it, I thought that the least I should do
was to read it. And, even more importantly, since I planned to
comment upon its outsized successor, the Omnibus Final Rule
of 2013, a similar chore would be required. The original HIPAA,
as suggested by its title, was concerned mainly with insurance
matters, although in its preamble it promised a lot more:
A
To amend the Internal Revenue Code of 1986 to improve
portability and continuity of health insurance coverage in the
group and individual markets, to combat waste, fraud and
abuse in health insurance and health care delivery [italics added],
to promote the use of medical savings accounts, to improve
access to long-term care services and coverage, to simplify the
administration of health insurance, and for other purposes [italics added].
Much of the 167 pages of legislative gobbledygook about
health insurance was pretty much unintelligible to one without the proper background in these matters, but despite such
Proc (Bayl Univ Med Cent) 2014;27(2):163–165
shortcomings, the general impression received was that some
positive measures were in the offing regarding the workings of
the medical insurance system and related issues. As for patients’
privacy rights, only about a single page in toto was included
and, in this respect, the content of the message was crystal clear.
Under the subtitle concerning data collection, the secretary of
the Department of Health and Human Services (HHS) would
include procedures to ensure the privacy of individuals receiving
health care services. And under the section regarding “wrongful
disclosure of individually identifiable health information,” any
person knowingly violating the law using a unique health identifier might be liable for fines up to $50,000 and 1 year in prison
or both. If the offense was committed under false pretenses, the
fine might be as high as $100,000 with up to 5 years in prison.
If such an offense was committed for some commercial advantage, personal gain, or malicious harm, the penalties could rise
to $250,000 with 10 years in prison or both. What constituted
an illegal breach of confidential information was simply what
the secretary of HHS said it was. Given the vagueness of this
criterion and such potentially draconian punishments for any
breach in confidentiality, it is no wonder that many health care
providers were driven by paranoia to the kinds of absurdities in
behavior described above.
Between 1996 and 2013, supplementary regulations broadening and attempting to explain the law have been issued.
Prominent among them was one defining the role of the Office of Civil Rights in assuming responsibility for the privacy
provisions under HIPAA. A record of the number of possible
breaches reported between 2004 and 2012 can be obtained over
the Internet (1). The totals have nearly doubled during this time
period. There were 4799 in 2004; 5683 in 2005; 8363 in 2011;
and 9411 in 2012. Although these numbers may not seem
excessively high for the entire country, each breach can involve
many individuals. The 9411 number registered in 2012 actually
represents the involvement of 6.7 million individuals.
What of the Omnibus Final Rule of 2013? To further educate
myself on the subject, I sought assistance from governmental
From the Department of Medicine (retired), Rutgers–New Jersey Medical School,
Newark, NJ.
Corresponding author: Allen B. Weisse, MD, 164 Hillside Avenue, Springfield,
NJ 07081 (e-mail: allenweisse@gmail.com).
163
sources. The Congressional Research Service (CRS) is an independent part of the Library of Congress. It provides excellent
reports on a variety of questions received from congressmen and
their offices. Ordinarily, this service is not available to the public.
However, as an academician engaged in a scholarly endeavor, I
wrote to the director of the CRS asking for an exemption. My
request was never answered. Similarly, a letter to the director of
the Office of Civil Rights at HHS received no reply. Fortunately,
I was able to obtain a number of useful CRS reports through
a friendly connection to Congress. Another individual I knew
to be professionally involved with the system gave me further
access to important information. A copy of the new rule was
obtainable over the Internet (2).
In a preamble to the rule that went into effect in March
2013, the stated aims of this new version of HIPAA include,
among others, making business associates of covered doctors
and other entities such as medical practices and hospitals directly liable for compliance with HIPAA rules and regulations;
strengthening limitations on the use of protected patient information; expanding individuals’ rights to access of electronic
information; requiring changes and redistribution of notices
of privacy practices by physicians and hospitals; implementing more objective standards defining “harms” when privacy
is breached; and prohibiting most hospital plans from using
genetic information for underwriting purposes. No priority was
given to means of improving cooperation and understanding
between patients and their physicians.
Confronting the Omnibus Final Rule of 2013 was daunting, and not only because of its 563-page length. The routine
use of impenetrable legalistic jargon jarred the mind. Adding
to the bulk of material to be reviewed was the practice of printing an initially proposed version of a provision of the rule; this
was followed by public commenters’ input, often a response to
the commenters’ suggestions or objections, and then the final
version of the rule.
Since the new law incorporates portions of previous laws
still in effect, reference to these pepper the pages. These include the Health Information Technology for Economic and
Clinical Health Act of 2009, the Social Security Act, the Patient
Safety and Quality Improvement Act of 2005, and the Genetic
Information Non-Discrimination Act of 2008, among others. At every point I wished to examine and enlighten myself,
I found references to previous acts that were in effect, some
identified only by number and sections. An example on page
35: 164.504(c)(4)(ic)(B). I began to feel the same way I did
when I examined my first matryoshka doll, opening it up to
reveal its essence only to find a smaller but otherwise identical doll, containing a still smaller one, and so on, all smiling
inscrutably in colorful lacquered dress. If I was really to make
a legitimate study of the law, I would be compelled to open up
all the previously referred to laws now included in the 2013
document. This would no doubt take many months rather than
the several weeks I planned to devote to the project, and I seriously doubted whether, given the character of such legislative
documents—assuming I could acquire them—I would emerge
any better informed. I therefore settled on limiting the project
164
to extracting whatever few pieces of information I could that
might prove to be of some value to physicians and other socalled “entities” reading the law.
What about privacy? The ability of individuals to completely
control access to their personal medical records is the Holy Grail
of privacy rights advocates. The possibility of actually achieving
this is as much a myth as the Holy Grail itself. Were it seriously
attempted, the whole machinery of medical care administration
would come to a screeching halt. Insurance companies and billing services require such information to process charges. Institutions such as Medicare and Medicaid need this information to
audit their operations and plan for the future. Certain diseases
are classified as “reportable” in the interests of public health.
Immunization records are often required by school districts to
ensure protection of the children attending their schools. Such
requirements are actually recognized by the new law. Perhaps
the only type of care that may effectively adhere to the ideal of
personal privacy is psychiatric treatment, since this is so often
paid out of pocket directly to the psychologist or psychiatrist.
What about genetic information? This is a major component
within the 2013 rule, taking up almost 100 pages, about a fifth
of the document. With the recent advances in the field, this is a
highly charged, newly recognized element of medical care now
being given its proper due. Mercifully, this section contains
much writing that actually could past muster in English 101.
The rule prohibits “using or disclosing protected health information that is genetic information for underwriting purposes in all
plans covered in the HIPAA privacy rule.” It also distinguishes
between “manifest disease” (symptoms and physical findings
characteristic of a particular genetically based disease) and the
finding of a genetic component that may or may not coexist
(a genetic abnormality). This section would make worthwhile
reading for anyone practicing medicine where genetics is emerging as a primary factor.
What about decedent information? Knowledge about cause
of death and its relationship to various patient characteristics
has been critical in advancing the quality of medical care. The
new rule sets 50 years after demise as an appropriate period of
protection before postmortem information might be obtained
without permission from survivors of the deceased. While some
medical historians might find this satisfactory, with new diagnostic modalities and treatments occurring at a rapidly advancing rate and the need for their evaluation urgent, practitioners
and medical researchers might find this rule overly restrictive.
Those empowered to make disclosures about decedents are defined as those with first to fourth degrees of familial relationship. The marital bond appears to be given equal recognition.
No mention is made of civil unions, gay or lesbian, but those
primarily responsible for the decedent’s health concerns prior
to death appear to be given some consideration. Issues such as
removal from artificial life support systems, organ donation,
and permission for autopsy are not covered.
How much will the activation and continued support of
these new regulations cost? The estimate for the first year of
operation was $114 to $225 million, with an estimate of $14.5
million annually thereafter.
Baylor University Medical Center Proceedings
Volume 27, Number 2
What are the penalties involved for breaking the law? Four
categories are defined reflecting the increased severity of any
malfeasance: 1) violations in which the covered entity did not
know and, with reasonable diligence, would not have known
a violation had occurred; 2) violations due to reasonable cause
and not to willful neglect; 3) violations due to willful neglect but
corrected in a timely manner; and 4) violations due to willful
neglect and not corrected in a timely manner. At the low end,
each violation can be met with a fine of $100 to $50,000, with
$1.5 million for identical violations within a calendar year. For
the most severe category, a minimal penalty of $50,000 can
be levied with an annual maximum of $1.5 million for repeat
offenses. The severity of the penalty will be determined by the
nature of the violation and the resulting harm caused. Compared to 1996, the potential financial penalties are appreciably
higher, but prison time is no longer mentioned.
Presumably the income generated by violations will meet the
costs of conducting the program. Such penalties, even before
the 2013 law went into effect, have been considerable. Brach/
Eichler, a New Jersey legal firm that is involved in such matters,
keeps a tab on such penalties and includes many physicians on
their mailing list. Before the new law took effect, they noted a
$1.2 million penalty against Affinity Health Plans and a settlement with WellPoint, Inc. for $1.7 million as examples of recent
actions by the government.
In the end, this legislative voyage of discovery was pretty
disappointing. I was left pondering another Russian-related
metaphor, that uttered by Winston Churchill regarding his view
of the Soviets: “a riddle wrapped in a mystery inside an enigma.”
Most laws passed by Congress are flawed to some extent but,
once passed, they seem to develop a life of their own, persisting
within the body politic. Of course there are some really bad
ones, such as that ushering in prohibition, which was passed in
1919 and repealed in 1933. However, for most laws passed by
April 2014
Congress during the last couple of hundred years, repeal will not
happen. There is always some small but powerful constituency
that benefits even from a bad law, and congressional inertia can
be counted upon to keep it on the books.
James Madison, the father of the Constitution, warned us,
“It will be of little avail to the people that the laws are made
by men of their own choice if the laws be so voluminous that
they cannot be read or so incoherent that they cannot be understood.” Despite his concern at the beginning of the Republic,
we continue to witness legislative behemoths like HIPAA and
its reincarnations bearing down upon us with little hope for
revision or repeal.
Despite the worthy portions of these laws, their emphasis
on punishment for breaches only serves to inhibit the flow of
information necessary for efficient medical management and
erode the bonds of trust so essential to a proper doctor-patient
relationship. Stuart Graves, in writing about confidentiality
and the effect of electronic health records upon it, commented,
“Physicians seem to live interminably hassled lives” (3). How
true.
Acknowledgment
Jerilyn Goodman and Kevin Littlefield assisted in the preparation of this paper.
1.
2.
3.
US Department of Health and Human Services. Health information
privacy: Enforcement results by year. Available at http://www.hhs.gov/ocr/
privacy/hipaa/enforcement/data/historicalnumbers.html#tenth.
US Department of Health and Human Services. Modifications to the
HIPAA Privacy, Security, Enforcement, and Breach Notification Rules under
the Health Information Technology for Economic and Clinical Health Act and
the Genetic Information Nondiscrimination Act; Other Modifications to the
HIPAA Rules. Available at https://s3.amazonaws.com/public-inspection.
federalregister.gov/2013-01073.pdf
Graves S. Confidentiality, electronic health records, and the clinician.
Perspect Biol Med 2013;56(1):105–125.
HIPAA: a flawed piece of legislation
165
Book Review
Selected Roberts Papers from
Seven Generations by Charles
Stewart Roberts, MD
Spartanburg, SC: The Reprint
Company, 2013.
Hardback, $42.95; Paperback,
$32.95; 528 pp.
Reviewed by F. David Winter Jr., MD
his treatise is an ambitious endeavor to
report on seven consecutive generations
of accomplished men in the
Roberts family. Th e last of
the lineage, who authored
the book, began the project with “my two sons in mind.”
There are seven chapters, one from each of the seven generations of the family. There is much to write about among the
Roberts men:
T
No man lived a life free of difficulty and even tragedy; some
experienced poverty, loss of fortune or favor, lives cut short, . . .
deaths, divorce, . . . goals unachieved, and promises unfulfilled. . . .
[The book is] balanced, however, by a respectable record of
accomplishment and fortitude.
Chapter 1 discusses John Roberts Sr., born in 1764 in
the state of Virginia on a farm previously occupied by the
Cherokee Indians. His ancestors were thought to have come
from Kent, England. He would later reside in South Carolina, Georgia, and Mississippi. Mr. Roberts Sr. served in the
war of 1781 but not for long and was denied a pension due to
the brevity of his service. He and his wife were of the Baptist
denomination, but he was once cited for nonattendance,
a feat worthy of publication in those days. Nonetheless, a
later genealogist would label him “the keystone American
ancestor.”
Chapter 2 chronicles James Roberts, son of the aforementioned John Roberts Sr., who rose to become a judge in Georgia.
He was not formally schooled in the law but earned his title after
serving 16 years in the courtroom. James had 12 children. He
himself was a staunch unionist, though five of his sons served
in the Confederate army. His youngest would later adopt his
father’s ideals and switch to the loyalist forces.
George Washington Roberts, named after America’s first
president, is discussed in chapter 3. He was the first son of
James Roberts. Educated in the legal profession and admitted
to the bar at age 22, he expired at age 35 of “consumption.”
166
During his abbreviated adult life as a slave owner, he was a vocal secessionist. In a resolution of his county in Mississippi, he
wrote that the election of Abraham Lincoln “is a violation of the
constitution in spirit . . . and therefore we are resolved to resist
Lincoln.” In the great American spirit, criticism of presidents
continues to this day.
James William Roberts, the topic of chapter 4 and son of
George Washington Roberts, had a longer and more noteworthy life. Left fatherless at age 10, the young man supported his
mother and two younger siblings by selling apples. A Georgian
businessman would take a shine to him and foster his education
at Emory College. This Roberts would graduate first in his class
and go on to become a Methodist minister described as “intelligent and literary” yet “forceful and controversial.” Later in
his career he became president of Wesleyan College in Macon.
He was known for championing several controversial issues of
the day:
• “A nation cannot exist without a conscience, and that it
can have no conscience without recognized standards of
morality and religion.”
• “Man is a religious being, and the religious element within
him must and will have either religion or anarchy.”
• “Foreign immigration, on the whole, introduces demoralizing agencies among us. . . . Anarchists, nihilists, all sorts—
they come. . . . It seems to me that in this matter the time
has come for restriction and selection.”
• “Liquor . . . enslaves, corrupts and damns the whole
man.”
• “I am opposed to woman’s suffrage.” If women “will confine
themselves to their divinely appointed sphere, their children
will be better trained and their homes will be happier.”
His tombstone carries the inscription, “Preacher, Teacher,
Man.”
Stewart R. Roberts was the son of the aforementioned
preacher-teacher-man, an internist and the first heart specialist
in Georgia. He was a well-respected academician and served as
president of the Southern Medical Association and the American Heart Association. He was said to have “cured” an ailing
pastor with the following instructions:
1. Eat less bread, no butter, no gravy, no rice, no desserts,
except fruit.
2. Have all the right fun that you can. Go fishing. Go walking
in the woods, go on picnics with your wife. Quit trying to
keep up. Assert what you already have in your mind. You
know more than St. Peter did.
3. The rest of the year do just as little reading and mental work
as you can. Take more to rides, laughing, and walks.
4. See how much you can get out of pastoral visiting.
5. Rest about one hour after lunch.
Proc (Bayl Univ Med Cent) 2014;27(2):166–167
6. Cold bath on waking in the morning; and another after
getting up in the afternoon.
Dr. Stewart Roberts began in the private practice of medicine and later became professor of clinical medicine at Emory
Medical School. He was active in many medical societies, had
a literary interest, and was a prolific author. It was written that
“his papers . . . were masterpieces of learning and style.” His
essay, “The Doctor,” serves as an example: “Born of science and
suffering, he lives amid the sadness of death and the gladness of
birth. Pain is his problem and his pursuit, death his constant
enemy, and the exactness of science is his strong right arm.” In
total, the book contains 120 pages of his writings.
William Clifford Roberts was one of three children of
Dr. Stewart R. Roberts. He studied to become an internist
like his father but was subsequently attracted to the field of
pathology and focused mainly on research of heart disease.
After a distinguished 28-year career as the chief pathologist
at the National Institutes of Health, he began a second career at the Heart and Vascular Institute at Baylor University
Medical Center at Dallas. He has reached 20 years in this,
his current role.
He also inherited his father’s “writing bug” and authored
or coauthored >1600 scientific publications on cardiovascular
disease. For more than 30 years, he has served, and continues
to serve, as the editor in chief of The American Journal of Cardiology and in a similar role for nearly 20 years now as editor
of Baylor University Medical Center Proceedings. In his role as
editor, he has reviewed >60,000 manuscripts and as a lecturer
he has visited >2200 cities. In addition to heart-related topics,
his writings and lectures cover the importance of the physical
examination, the relevance of autopsies, advice to young physi-
April 2014
cians, and preventive lifestyles. Dr. Bill Roberts is widely quoted
with memorable sayings, such as:
• “Hospitals are the most expensive hotels in the world.”
• “The only absolute, unequivocal, independent atherosclerotic risk factor is an elevated LDL cholesterol.”
• “The more we weigh, the sooner we die.”
• “You should limit the flesh you eat to fish.”
• “You kill the cow, you eat the cow, and the cow kills you.”
• “Statin drugs are to atherosclerosis what penicillin was to
infectious disease.”
The author of the book, Charles Stewart Roberts, is the
second of the four children of Dr. William Clifford Roberts and
followed in his father’s and grandfather’s footsteps into medicine yet strayed to become a heart surgeon. The love of writing
persisted in the gene pool; he has authored or coauthored 50
medical publications, 35 other writings, and also 27 poems
to date. The habits, recommendations, and accomplishments
of medical luminaries are of particular interest to Dr. Charles
Roberts. Many vignettes of such are included in the book.
The writings of Dr. Stewart Roberts, Dr. William Clifford
Roberts, and Dr. Charles Stewart Roberts (chapters 5, 6, and 7)
in this book read as essays or short stories. Many are instructive,
and all are quite interesting for those who enjoy biographical
lessons and the history of medicine. Reflecting back to the goal
mentioned in the introduction, I am sure that the two sons of
the author will be quite proud of this compilation of their ancestors. I suspect the author’s two daughters will also be pleased.
The reviewer, F. David Winter Jr., MD, is an internist on the medical staff of
Baylor University Medical Center and chief clinical officer and chairman of the
board of HealthTexas Provider Network.
Book review
167
From the Editor
Facts and ideas from anywhere
DEVELOPMENT OF INTERNAL
MEDICINE
In 2003, Dr. H. Lawrence
Wilsey gave me the book Grand
Rounds: One Hundred Years of Internal Medicine edited by Russell
C. Maulitz and Diana E. Long (1).
The book was published in 1988
and includes chapters on general
internal medicine and many of its
William C. Roberts, MD.
subspecialties (infectious diseases,
gastroenterology, rheumatology,
nephrology, and cardiology). This book would appeal to any
internist. The chapter that intrigued me the most was entitled
“The Inner History of Internal Medicine” by Paul Beeson and
Russell C. Maulitz. Paul Beeson is a favorite of mine, and
maybe that is one reason I enjoyed so much his 40-page chapter. Beeson has many similarities to William Osler. Both were
Canadians, both were chairmen of departments of medicine at
prominent institutions (Osler: University of Pennsylvania and
Johns Hopkins University; Beeson: Emory University and Yale
University), both were Regius professors at Oxford University,
United Kingdom, and both had biographies of them written
by a neurosurgeon.
Beeson and Maulitz asked initially “What is internal medicine? And who is the internist?” The terms have been misunderstood by many in the public. American internists trace their
ancestry back to the tiny Royal College elites granted monopoly
rights by royal warrant beginning in the 16th century. The
American College of Physicians professes a filial relationship
with the Royal College of Physicians of London (now of England), empowered by Henry VIII in 1518. From there, Beeson
and Maulitz developed the internist’s world from the scientific,
clinical, personal, and professional perspectives.
The process of demarcating new medical specialties first
in Germany and soon after in the other industrial nations was
fueled by two powerful engines: new technology (primarily
diagnostic but also therapeutic) and an increased professional
competition. Specialized fields like ophthalmology and otolaryngology found professional niches. Slightly later, old fields
like surgery gained in professional power as they created their
edifices on foundations of science.
168
The designation “internal medicine” seems to have originated around 1880 in Germany with the use of the modifying word
innere. The term was employed to indicate a field of practice in
which concepts were based on an emerging understanding of
physiology, biochemistry, bacteriology, and pathology and in
which surgical methods were not employed. The expression was
intended to connote special knowledge and training rather than
dogma, empty hypotheses, and mere observation of outward
manifestations of disease. At that time, North America took
most of its medical cues from Germany. Over a few decades,
thousands of physicians and medical students flocked to the
laboratories of polyclinics of Strasbourg, Berlin, and Vienna.
Consequently, the expression “internal medicine” reflecting
German institutional arrangements was adopted quickly in
America. William Osler, incidentally, disputed its status as an
incipient specialty but favored the good old name “physician”
in contradiction to general practitioners, surgeons, and obstetricians and gynecologists. Osler tended to deemphasize the
“specialized” aspect of the field and chose to stress its role as a
gateway to other more limited specialties—domains of scientific
knowledge or technical expertise now conventionally thought of
as subspecialties. Most American internists preferred the phrase
“internists” to Osler’s “physician.”
The chapter goes on to describe contributions made by
American physicians and important events in the specialty: the
development of the Association of American Physicians, the
publication of the first edition of Osler’s textbook, Principles
and Practice of Medicine (1892), the founding of the Johns Hopkins Medical School (1893), the Flexner report on American
medical education (1910), the development of the Rockefeller
Institution, the making of clinical investigation scientific, the
development of the full-time system, the explosion of medical
research just before and after World War II, the changes in
patient mix seen by internists over the decades, the changes in
therapeutics in internal medicine, and the development of the
various subspecialties in internal medicine.
KIDNEY TRANSPLANTS
According to Gary S. Becker and Julio J. Elias, writing in
The Wall Street Journal, in 2012, 95,000 American men, women,
and children were on the waiting list for a new kidney, the
most commonly transplanted organ (2). Yet, only about 16,500
Proc (Bayl Univ Med Cent) 2014;27(2):168–178
kidney transplant operations were performed that year. Taking
into account the number of people who die while waiting for
a transplant, this figure implies an average wait of 4.5 years for
a kidney transplant in the USA. This situation surprisingly is
far worse than it was just 10 years ago, when nearly 54,000
people were on the waiting list, with an average wait of 2.9
years. Finding a way to increase the supply of organs would of
course reduce wait times and deaths, and it would greatly ease
the suffering that many sick individuals now endure while they
hope for a transplant. The most effective change, these authors
believe, would be to provide compensation to people who give
their organs.
The first kidney transplant and indeed the first successful
organ transplant was in 1954 at the Brigham and Women’s
Hospital in Boston. Kidney transplantation did not really take
off, however, until the 1970s with the development of immunosuppressive drugs that could prevent the rejection of transplanted organs. Since then, the number of kidney and other
organ transplants, of course, has grown rapidly, but not nearly
as rapidly as the growth in the number of people with defective
organs who need transplants. Many of those waiting for kidneys
are on dialysis, and life expectancy while on dialysis is not long.
People, for example, aged 45 to 49 on average live an additional
8 years if they remain on dialysis, but they live an additional
23 years if they get a kidney transplant. Almost 4500 people
died in 2012 while waiting for a kidney transplant, and most
died because they were unable to replace their defective kidneys
quickly enough. Most of those on dialysis cannot work, and
the annual cost of dialysis averages about $80,000. The total
cost over the average 4.5-year waiting period before receiving
a kidney transplant is about $350,000, which is much larger
than the $150,000 cost of the transplant itself.
Individuals can live a normal life with only one kidney, so
about 35% of all kidneys used in transplants come from live
donors. Most kidney transplants come from parents, children,
siblings, and other relatives of those who need transplants. The
rest come from individuals who want to help those in need of
transplants.
Exhortations and other efforts to encourage more organ
donations have failed to significantly close the large gap between
supply and demand. Some countries use an implied consent
approach, in which organs from cadavers are assumed to be
available for transplant unless, before death, individuals indicate that they don’t want their organs to be used. The US
continues to use informed consent, requiring people to make
an active declaration of their wish to donate. Switching to implied consent would unlikely lead to a large enough effect to
eliminate the sizeable shortfall in the supply of organs in the
US. That shortfall, however, is not just an American problem.
It exists in most other countries as well, even when they use
different methods to procure organs and have different cultures
and traditions.
Paying donors for their organs would, in the authors’ opinions, eliminate the supply-demand gap. In particular, sufficient
payment to kidney donors would increase the supply of kidneys
by a large percentage, without greatly increasing the total cost
April 2014
of kidney transplantation. The authors opine that a very large
number of both live and cadaveric kidney donations would
be available by paying about $15,000 for each kidney. Few
countries, however, have ever allowed the open purchase and
sale of organs. Iran permits the sale of kidneys by living donors.
The price there appears to be about $4000 per kidney, and the
waiting time to get kidneys has been largely eliminated. (Iran’s
per capita income is one quarter that of the USA.) Since the
number of kidneys available at a reasonable price would be far
more than needed to close the gap between the demand and
supply of kidneys, there would no longer be any significant
waiting time to get a kidney transplant. The number of people
on dialysis would decline dramatically, and deaths due to long
waits for a transplant would essentially disappear. The system
proposed by the authors would include payment to individuals who agree that their organs can be used after they die. This
is important because transplantation for hearts and lungs and
most livers only uses organs from the deceased. Under a new
system, individuals would sell their organs “forward” (that is, for
future use), with payment going to their heirs after their organs
are harvested. Relatives sometimes refuse to have organs used
even when a deceased family member has explicitly requested it,
and they would be more inclined to honor such wishes if they
received substantial compensation for their assent.
Whether paying donors is immoral because it involves the
sale of organs is a much more subjective matter, but the two
authors question this assertion given the very serious problems
with the present system. Any claim about the supposed immorality of organ sales should be weighed against the morality
of preventing thousands of deaths each year and improving
the quality of life of those waiting for organs. How can paying
for organs to increase their supply be more immoral than the
justice of the present system?
Researchers in space have learned that stem cells grow super
fast in that area (3). A CEO of a stem cell upstart (Zero Gravity
Solutions) has indicated that a kidney can grow in space in 30
to 35 days. The organ shortage might be improved by space
laboratories.
TRANSPLANTED WOMBS
Nine women in Sweden have successfully received transplanted wombs donated from relatives (4). The women with
their new wombs will soon try to become pregnant. The nine
women were born without a uterus or had it removed because
of cervical cancer. Most are in their 30s. (In most European
countries, including Sweden, using a surrogate to carry a pregnancy is not allowed.) There have been two previous attempts
to transplant a womb—in Turkey and in Saudi Arabia—but
both failed to produce babies. Some have raised concerns about
whether it is ethical to use live donors for an experimental procedure that does not save lives. The womb transplants began in
September 2012, and the nine womb recipients are all doing
well. Many already had periods 6 weeks after the transplants,
an early sign that the wombs are healthy and functioning. The
transplant operations did not connect the women’s uteruses to
the Fallopian tubes, so they are unable to get pregnant naturally.
Facts and ideas from anywhere
169
But all who received the womb have their own ovaries and can
make eggs. Before the operation they had some eggs removed
to create embryos through in vitro fertilization. The embryos
were then frozen, and physicians plan to transfer them into the
new wombs, allowing the women to carry their own biologic
children.
WOMAN TO BIRTH GRANDCHILD
A 58-year-old Utah woman is set to give birth very soon to
her first grandchild (5). She is serving as a gestational surrogate
for her daughter and son-in-law after the couple struggled with
fertility problems. The 32-year-old daughter has had about a
dozen miscarriages, with the longest pregnancy lasting only 10
weeks. After she looked unsuccessfully for a surrogate, her mother volunteered. The baby girl was due in February 2014. This is
not the first such incident. In 2012, a 53-year-old Iowa woman
gave birth to her twin granddaughters, and in the same year a
49-year-old woman in Maine gave birth to her grandson.
INSOMNIA AIDS
According to a piece by Jennifer Alsever in The Wall Street
Journal, Americans spent just over $32 billion in 2012 on sleeprelated aids (6). According to an August 2013 study by The
Centers for Disease Control and Prevention, 8.6 million people
in the US reported taking medications before going to sleep.
Falling asleep and staying asleep through the night is a constant
struggle for many. Alsever described using an iPhone sleep app
and a CD set based on audio brain research. There was also an
MP3 download.
The Brainwave Music System was a 6-CD set created by
Jeffrey Thompson, director of the Center for Neuroacoustic
Research in Carlsbad, California. The CDs use music embedded with tones to make sleep come faster. The music apparently sounded somewhat dreamlike with low humming and
piano melodies. Alsever tried two 30-minute sleep tracks and a
30-minute relaxation track. She played the relaxation track in
the background while she performed regular activities before
bedtime such as brushing her teeth, and she played the sleep
CD at bedtime. She indicated that she fell asleep quickly and
felt refreshed in the morning.
She also hired a relaxation coach who had taught corporate
workshops and yoga and meditation classes. The bedtime packet
cost $50 and included a custom recording of relaxing music with
voice relaxation instructions and help with the development of
a “sleep ritual.” The American Institute of Stress in Fort Worth,
Texas, offers referrals to stress-management professionals who
can offer advice on how to wind down. The relaxation coach
inquired about nightly habits, such as TV viewing and worry
level at bedtime, and also preferences on relaxation sounds, such
as wind chimes, Tibetan singing bowls, or seashore sounds. She
advised to stop cleaning the house or working on the computer
at night. The coach suggested creating a bedtime routine that
brings down the level of activity, such as gentle stretching and
a nighttime bath. The 27-minute relaxation track includes the
relaxation coach’s soft steady voice over the sound of Tibetan
singing bowl music. The coach advised squeezing and relaxing
170
muscles, moving up from one’s legs to one’s eyes. Alsever indicated that she fell asleep 10 minutes into the track.
She also tried the SleepEasily MP3 package, a program by
a Denver behavioral consultant. The five tracks didn’t work
well for Alsever. The download came with a 38-page PDF of
instructions including how to use the ear plugs. On the sleep
track the instructor advised thinking about calming your jaw
muscles and opening your throat for an inner sleep breathe.
In the 21-minute track, the instructors’ words got slower and
slower when talking about imagining sounds of seashells and
lullabies.
Alsever also tested an iPhone and iPad app called “ABCs
of Better Sleep” created by a British hypnotherapist. The app
included tips on better sleep and a 23-minute hypnosis session
for deep sleep. In a 12-minute practice session, the hypnotist
explained what the ABCs of the program are: “A” stands for “Are
my eyelids so relaxed that I couldn’t open them if I tried?”; “B”
stands for “breath” instructions—to take a deep breath, hold
it, and then release it using every muscle; and “C” stands for
“the sea,” in which one imagines floating underwater. The app
included a 23-minute audio clip with the main hypnosis session
played in bed. Alsever fell asleep at the end of it and felt great
the next day. The hypnotist indicated that once it was used for
a week, the hypnosis session would no longer be needed.
OBESITY RATE
In the US the obesity rate appears to be leveling off, according to the National Center for Health Statistics (7). The
percentage of adults in the USA who were obese (body mass
index ≥30 kg/m²) in 2008 through 2012 was about 35%. In
1960, it was 13% and in 1980, 15%. Thus presently in the US,
about 80 million adults are overweight by at least 35 pounds
(BMI ≥30). The prevalence of obesity increased dramatically in
the 1980s and 1990s.
DECREASING CALORIES BY FOOD COMPANIES
Sixteen companies, including General Mills, Campbell’s
Soup, ConAgra Foods, Kraft Foods, Kellogg, Coca-Cola, PepsiCo, and Hershey, pledged to cut 1 trillion calories by 2012
and 1.5 trillion calories by 2015 in their products (8). A study
sponsored by The Robert Wood Johnson Foundation evaluated
the progress toward that goal and found that between 2007
and 2012, the companies had reduced their products’ calories
by the equivalent of 78 calories per person per day. The Robert Wood Johnson Foundation, which works to improve the
nation’s health, hired researchers at the University of North
Carolina at Chapel Hill to count the calories in almost every
packaged item in the grocery store. To do that, the researchers
used the store-based scanner data of hundreds of thousands of
foods, commercial databases, and nutritional-facts panels to
calculate the calories the companies were selling. The investigators indicated that the companies have exceeded their own
goals by a wide margin. As a consequence, many products now
come in lower-calorie versions, are baked instead of fried, or are
sold in miniature as well as larger versions. Smaller servings—
100-calorie packs of popular snacks, for example—and smaller
Baylor University Medical Center Proceedings
Volume 27, Number 2
cans of sugary drinks may have contributed to the reduction
in calories.
LATIN AMERICA’S FIGHT AGAINST JUNK FOOD
Since 2012, Peru, Uruguay, and Costa Rica have banned
junk food from public schools (9). Ecuador recently mandated
a nutritional label system that warns against high salt, sugar,
and fat. Industrial food makers in Ecuador also will be banned
from using images of animal characters, cartoon personalities,
or celebrities to promote products high in salt, sugar, or fat. In
2013, Mexico passed a special tax of 8% on packaged foods like
potato chips, and a per liter tax (about 8 US cents) on sugary
beverages. (Mexico is Coca-Cola Company’s second-biggest
market in the world by volume sales.) Columbia is also considering a beverage tax. In contrast, in more developed countries,
proposed soda taxes have failed.
Obesity has become a major problem in Latin America, and
the trend coincides with Latin America’s becoming an important
growth region for multinational food and beverage corporations.
(PepsiCo Inc.’s Latin American food volume sales soared 11%
while contracting 1% in North America.) Mexicans presently
allot 45% of their household food expenditures to packaged
foods. Chileans are on par with Americans, spending 63% of
their food budget on packaged products. In both Chile and
Mexico, roughly 7 of 10 adults and nearly a third of children
are overweight, and diabetes mellitus threatens to overwhelm
the country’s health system. Serious health problems correlate
with high consumption of snacks, soda, and other industrialized
foods. Good for Latin America!
SMOKING DECREASE
The war on smoking, now 5 decades old, is one of the nation’s greatest public health success stories (10). In 1964, four in
10 adults in the US smoked; today, fewer than 2 in 10 smoke.
In 1964, the number of cigarettes smoked in the US annually
by adults was 4,195 and by 2011, the number had dropped by
70%. The first surgeon general’s report on smoking and health
appeared on January 11, 1964. Its statement that smoking is
a cause of lung cancer and other disease was major news then.
The report led to cigarette warning labels, a ban on TV ads, and
eventually an antismoking movement that shifted the nation’s
attitude on smoking. Then, smokers were cool; today, many are
outcasts (banished from restaurants, bars, public buildings, and
their workplaces). The formula for success is no longer unclear:
adopt tough warning labels, air public health ads, fund smoking
cessation programs, impose smoke-free laws, and raise taxes on
cigarettes. Few people start smoking after age 19!
High taxes kill smoking as surely as cigarettes kill smokers.
The evidence that taxing decreases smoking is overwhelming.
The 10 US states with the lowest adult smoking rates have an
average tax of $2.42 on every pack, 3 times the average tax in the
states with the highest smoking rates. New York has the highest
cigarette tax in the country at $4.35 per pack, and just 12% of
teens smoke in the state—far below the national average of 18%.
In Kentucky, in contrast, the taxes are low (60¢ per pack), smoking restrictions are weak, and the teen smoking rate is double
April 2014
New York’s. Other low-tax states have similar dismal records.
The effect of the cigarette taxes is amplified when the revenue is
used to fund initiatives that help smokers quit or persuade teens
not to smoke. The antismoking forces in the US in the last 50
years have helped to prevent 8 million premature deaths. But,
as long as 3000 adolescents and teens take up smoking each
day, the war against cigarettes is not over.
HOME HEALTH TESTING
Already tests are available at home to determine whether
women are ovulating, to measure blood alcohol levels, to test
for the presence of illegal drugs, to determine cholesterol and
glucose values, and to find out whether one has HIV or hepatitis C (11).
MEDICAL SCHOOL APPLICATIONS
A record number of students applied to and enrolled in US
medical schools in 2013 (12). The total number of applicants
grew by 6.1% to 48,014, up from 45,266 in 2012, surpassing
the previous record set in 1996 by 1049 students. The number
of students enrolling in medical schools increased by 3% over
last year at 20,055, exceeding 20,000 for the first time. The
number of first-time applicants, an important indicator of interest in medicine, went up by 5.5% to 35,727. Overall, this
surge in applicants continues a decade-long rise from a low of
33,624 in 2002. Since then, the number of applicants has risen
each year to this new all-time high. Even though medical school
enrollment is rising, unless Congress lifts the 16-year-old cap
on federal support for residency training, there will be serious
shortages of physicians across the board, geographically and
across specialties. In 2013, four new medical schools welcomed
their charter classes, accounting for about half of the enrollment
increase. In addition, 14 medical schools increased their class
sizes by more than 10%.
THE MAYO CLINIC AT 150 YEARS
On January 27, 1864, Dr. William Worrall Mayo (“Dr. W.
W.”) (1819–1911) announced in the area newspapers that he
was opening a private medical practice in Rochester, Minnesota.
He had been directed to Rochester 9 months earlier as the result
of a short-lived appointment from President Abraham Lincoln
to serve as an examining surgeon for the Union Army during
the Civil War. From these beginnings, his independent private
practice thrived and later experienced exponential growth when
his sons, Dr. William James Mayo (“Dr. Will”) (1861–1939)
and Dr. Charles Horace Mayo (“Dr. Charlie”) (1865–1939),
joined after graduating from medical school in 1883 and 1888,
respectively, to form a group practice that would later become
Mayo Clinic (13). From these family origins, the small private
practice on the remote prairie of southeastern Minnesota has
evolved into an internationally recognized medical center.
The success of Mayo Clinic can be attributed to an organizational culture, begun by its founders, that provides cohesive
values while inspiring innovation. This Mayo Clinic model of
care has enabled Mayo Clinic to develop attributes and make
discoveries that benefit people far beyond its patient base; it
Facts and ideas from anywhere
171
also positions the clinic to continue to lead well into the 21st
century.
The mid-19th century educational background of Dr. W. W.
was unique in that although not from a privileged background,
he studied Latin and Greek, was a student of the physicist and
chemist John Dalton (an early contributor to atomic theory and
the medical description of color-blindness), attended college,
and achieved two medical degrees. A strong advocate for lifetime
learning, he was, as his eldest son, Dr. Will, eulogized him, “a
man of hope and forward-looking mind.” Among the oldest
patient records is a ledger that Dr. W. W. used. His handwritten
entry on January 8, 1866, “Left open for further thought and
research,” shows how he continually sought out new medical
advances and was never satisfied with the status quo.
Dr. W. W.’s partnership with his two sons grew to become
the first—and today, the largest—integrated, not-for-profit,
private, multispecialty medical practice in the world. The values
of Mayo Clinic are particularly informed by Rochester Franciscans, a Catholic order founded by Maria Alfred Moes (“Mother
Alfred,” 1828–1899) in Rochester, whose magnificent motherhouse, Assisi Heights, is slightly more than a mile from Mayo
Clinic facilities. The Franciscans and the Mayos became partners
in healing in response to a tornado that devastated Rochester
in 1883. From this collaboration, Mother Alfred proposed that
the sisters would fund construction of a hospital and serve as
nurses if Dr. W. W. and his sons would provide surgical and
medical care. As a result, St. Marys Hospital opened in 1889
and was an early adopter of Listerian aseptic and antiseptic
principles. In addition to the Catholic values of the Franciscans
and the scientific-humanistic values of the Protestant Mayo
family, many cultures and traditions have contributed to the
ethos of Mayo Clinic.
How has the Mayo Clinic become so successful? The core or
primary value of Mayo Clinic is that “the needs of the patient
come first.” Generations of practitioners at Mayo Clinic have
upheld this value. Strict adherence to this ethic affords daily
purpose and meaning to the organization and its contributors. Such an environment, built over 150 years and focused
on the welfare of the patient, has led to an ingrained commitment to excellence and ongoing continuous improvement
for all activities that constitute the Mayo Clinic’s approach to
medical care. The unwavering commitment to the patient also
is complemented by the discovery of new information and the
translation and adaption of those discoveries to advance clinical care (Table). Innovations in education also help inform all
appropriate parties of new information, again with a focus on
improving clinical care. The triple shield logo of Mayo Clinic—
clinical care, education, and research—that is liberally displayed
around Mayo Clinic campuses and other venues is an ongoing
reminder of the philosophy and focus of the institution.
In 1919, the Mayo brothers and their wives signed a deed
of gift donating most of their life savings and all of their assets
in the Rochester medical practice (including land, buildings,
and equipment) to an entity, the Mayo Properties Association,
which would ensure the perpetuation of Mayo Clinic beyond
the lifetimes of its founders. This gift from the Mayos, the
172
Table. Highlights of Mayo Clinic’s many contributions to medicine∗
• Intraoperative diagnosis using frozen sections of tissue specimens
• The world’s first program in postgraduate medical education
• Reliable laboratory procedures for determining basal metabolic rate
• Broders index for tumor staging
• Goeckerman treatment for psoriasis
• The nation’s first hospital-based blood bank
• Introduction of the postanesthesia recovery room to civilian hospitals
• Advocacy for the nutritional enrichment of flour
• The high-altitude oxygen mask and G-suit
• The pioneering use of streptomycin to treat tuberculosis
• The discovery and clinical application of cortisone (for which the
investigators won the 1950 Nobel Prize in Physiology or Medicine)
• The first successful series of open heart surgical procedures using the
heart-lung bypass machine
• Early development of the intensive care unit
• Early development of the radial nursing unit
• The Rochester/Olmsted County Epidemiology Project
• The first Food and Drug Administration–approved artificial hip joint replacement
• Introduction of computed tomography to North America
• Test for rapid diagnosis of anthrax poisoning following the September 11,
2001, terrorist attacks
∗Reprinted
with permission from Olsen KD, Dacy MD, 2014 (13).
equivalent of more than $100 million today, was accompanied
by a statement that the ultimate success of Mayo Clinic, “past,
present and future, must be measured largely by its contributions to the general good of humanity.”
Teamwork has been a major emphasis since the beginning of
the Mayo Clinic. Dr. W. W. stated, “No man is big enough to be
independent of others.” The Mayo brothers always spoke of their
accomplishments in terms of “My brother and I.” They encouraged medical subspecialization, and Mayo Clinic contributed to
the establishment of many disciplines, including orthopedics,
neurology, dermatology, thoracic surgery, anesthesiology, and
pediatrics, yet the integrated team-oriented practice was always
essential to Mayo Clinic’s success.
Quality has been at the forefront of the Mayo Clinic. The
first sentence in the Mayo Clinic model of care mentions high
quality. A closed medical staff with fully integrated hospital
care and outpatient clinics and a common medical record in an
all-electronic environment are important factors that enhance
safety and quality. Continuous professional training in quality and safety is mandatory for all staff. Five safety workplace
behaviors are regularly discussed and incorporated: paying attention to detail, communicating clearly, having a questioning
and receptive attitude, handing off effectively, and supporting
each other. Mayo Clinic is proud to be at the top of all the main
published quality indices and continues to set and define new
standards of quality and safety.
Baylor University Medical Center Proceedings
Volume 27, Number 2
Compensation of the physician staff focuses on quality, not
quantity. All physicians at Mayo Clinic are salaried. Their salary
range is approximately at the 70th percentile of market level
with no productivity bonuses. It is the Mayo Clinic perspective
that patients are not served well if physicians compete with each
other. The highly productive work of the staff is maintained
through careful staff selection for special expertise, proven excellence in patient care, and a strong work ethic. There are no
employment contracts or tenured periods for physicians. The
environment also promotes staff loyalty and stability, with low
attrition. In recent years, only 2.4% of physicians and 4% of
nurses left the institution after appointment to the staff.
And cost must be appropriate. Dr. Will described the neverending number of patients who would seek out care at the
Mayo Clinic if the clinic provided the best possible diagnostic
and treatment outcomes at low cost, a concept now recognized
as the value equation in health care. Mayo Clinic has taken a
strong stance nationally that medical reimbursement should
pay for value, not volume. Assessing and improving value is
taken seriously and is defined by outcomes, quality, safety, and
service divided by cost. Data from the Dartmouth Atlas of Health
Care looking at total cost for patients in the last 2 years of life
found that costs at Mayo Clinic were far less than at other
major medical centers for similar patients. Factors contributing
to these findings may include salaried physicians, efficiency of
testing and procedures, ready access to a team of physicians, fast
diagnoses, short hospitalizations and episodes of care, and fewer
evaluations, tests, and consultations. Physicians at Mayo Clinic
typically do not know the insurance status of their patients.
Behind the practice structure at the clinic is a highly involved
logistics system aimed at improving quality of care and reducing costs for all patients. This system is built on three goals:
shortening the time for tests to be performed and results to be
available, reducing the non–patient-related work for physicians,
and optimizing the time that physicians spend with patients.
Comprehensive care has been a hallmark of the clinic. One
provision of the Mayo Clinic model of care is the performance of
a comprehensive evaluation. This is not necessary in all patients
but remains a hallmark of the Mayo Clinic experience. Thorough evaluation includes attention to each patient’s physical,
emotional, psychological, and spiritual needs.
Scholarship and continuous improvement is a hallmark of the
clinic. As an academic medical center, Mayo Clinic is committed
to education and research, with a distinction being that these
endeavors are ultimately focused on strengthening the standard
of patient care. As such, at Mayo Clinic, all faculty participants,
whether working primarily in clinical care, education, or research, are cognizant that they are part of a team effort focused
on improving patient care, not just contributing to academic
activity for its own sake.
The rate of change in medical care, medical education, and
medical research is accelerating. In only the past 30 years, the
institution has been transformed by Mayo Clinic’s integration
with St. Marys Hospital and Rochester Methodist Hospital in
1986; expansion of the Mayo model of care to group practices in
Florida and Arizona in 1986 and 1987, respectively; creation of
April 2014
the Mayo Clinic Health System in 1992; and the development
of wide-ranging business endeavors to generate funds for the
not-for-profit mission. Mayo Clinic now employees 4100 physicians/scientists and 53,600 allied health practitioners. Patients
come to the Mayo Clinic from all 50 states and from many foreign countries. More than 1 million patients are seen each year,
and more than 500 operations are performed daily. Revenue
exceeds $8.8 billion per year. Mayo Clinic is not standing still. It
continues to expand, discover, and create new knowledge, promote health, and deliver health care in new ways to patients and
the public. Major initiatives include individualized medicine,
regenerative medicine, and the science of health care delivery.
A major area of research is individualized medicine with direct
patient care impact from pharmacogenomics, gene therapy,
proteinomics, metabolomics, and biomarker applications to
predict and enhance therapeutics for cancer and other diseases.
Mayo Clinic’s leaders have announced the goal of touching
200 million lives annually by 2020. This will be undertaken by
sharing and applying Mayo Clinic medical knowledge through
print publications, websites, social media, and a variety of other
products and services.
For patient care, Mayo Clinic tops the list.
ZONES ON PLANET EARTH WHERE PEOPLE COMMONLY LIVE
100 YEARS
Dan Buettner has written
a book entitled The Blue Zones:
Lessons for Living Longer from the
People Who’ve Lived the Longest
(14). The Blue Zones are areas of
the world with concentrations of
some of the world’s longest-lived
people. When the author first set
out to investigate human longevity, he recruited demographers
and scientists at the National
Institute on Aging to identify
pockets around the world where
people reached age 100 at rates
significantly higher, and on average, lived longer, healthier lives
than Americans do. The Blue Zones, the world’s confirmed
longevity hot spots, include Sardinia in Italy, Okinawa in Japan,
Loma Linda in California, and the Nicoya Peninsula in Costa
Rica. The author with his team traveled to these four Blue
Zones where people have a 3 times better chance of living 100
years than does the average American and then described each
of these places and the differing cultures that allowed longevity.
Some studies have shown that about 25% of how long we live
is dictated by genes and the other 75% by lifestyles and the
everyday choices we make. This book provides a great deal of
evidence that the way the people in the Blue Zones eat, interact
with each other, shed stress, heal themselves, avoid disease, and
view the world yields them many good years of life.
The Sardinian Blue Zone. The people of Sardinia have remained genetically distinct from the people in the rest of Europe.
The Sardinians’ lifestyle in the Blue Zone has not changed much
Facts and ideas from anywhere
173
since the time of Christ. The people there maintain not only their
genetic features, but also their economic isolation and traditional
social values, such as respect for elders, the importance of family, and the presence of unwritten laws. Genetic and cultural
isolation appear to go hand in hand. Most male Sardinians are
farmers or shepherds, and they can burn up to nearly 500 calories an hour. In the USA, only about 1 male in 20,000 reaches
age 100. The chance of two centenarians in the same family is
astronomically unlikely. In Sardinia, seeing more than one family
member aged 100 or more is not an uncommon occurrence. The
author found in the Sardinia Blue Zone 47 men and 44 women
who lived past their 100th birthday in a population of just under
18,000, a rate of centenarians that exceeds that in the US by a
factor of 30. More men than women lived to 100.
The diet of the shepherds and peasants in Sardinia is simple.
Bread is by far the main food. Peasants leave early in the morning with a kilogram of bread in their saddlebag. At noon their
meal consists only of bread with some cheese, occasionally an
onion, a little fennel, or a bunch of radanelli. At dinner, the
reunited family meal consists of vegetable soup (minestrone)
with or without some pasta. Families eat meat about once a
week, on Sunday. Fish does not figure prominently in their
diet. The shepherds drink wine daily, usually only at the evening
meal and no more than one quarter of the bottle. The wine is
usually made from Cannonau grapes, resulting in a red wine
with 2 to 3 times the level of flavonoids found in other wines.
Goat’s milk and mastic oil are other common foods.
In 1960, almost no one in Sardinia’s Blue Zone was overweight; now 15% of adolescents are. Most unique longevity factors have disappeared or are disappearing quickly from residents’
everyday life. The Sardinian wives are more sedentary than their
husbands. Women tend to stay home caring for children, doing
home repairs, and managing household finances. The Sardinian
diet was largely lean and plant based with an emphasis on beans,
whole wheat, and garden vegetables usually washed down by
Cannonau wine. Goat’s milk and mastic oil is far less common
today in their diet than in the past.
The Blue Zone in Okinawa. This is in essence a Japanese
Hawaii, an exotic laid-back group of islands with a warm temperate climate, palm trees, and white sandy beaches. For nearly
a millennium, this Pacific archipelago, nearly 1000 miles from
Tokyo, has maintained a reputation for extreme longevity. These
islands for a long time were referred to as “the land of the immortals.” Despite enduring years of Chinese and then Japanese
domination, a devastating world war, famines, and typhoons,
Okinawa can still claim to be the home of some of the world’s
longest-lived people. The Okinawan people enjoy what is probably the highest life expectancy on earth (in 2000 figures that
was 78 years for men and 86 for women), the most years of
healthy life (the Japanese have the greatest number of disabilityfree years at 72 for men and 78 for women), and one of the
highest centenarian ratios (about 5 per 10,000). They suffer
from diseases that kill Americans, but at much lower rates: a fifth
the rate of cardiovascular disease, a fourth the rate of breast and
prostate cancer, and a third the rate of dementia. In the USA
or Europe, only about 15% of centenarians are independent in
174
their activities of daily living. Of 32 centenarians interviewed in
Okinawa, all but four were functionally independent. According to governmental records, there are 700 centenarians among
Okinawa’s 1.3 million people.
The Okinawans grow vegetables in their gardens all year
long. A family pig is butchered on certain holidays and cooked
for a long time, the fat is skimmed off, and the rest of the animal is used in a stew-like dish. The Okinawan people historically have eaten meat only during ceremonial occasions. Before
World War II, sweet potatoes were eaten for breakfast, lunch,
and dinner. In 1900, Okinawans got 80% of their calories from
sweet potatoes. Peasants tended to scrape out a living by cultivating millet, rice, and barley. The half dozen annual typhoons
often wipe out or destroy their crops. The idea of retirement
never occurred to the Okinawan peasants. To this day, there is
not a word for retirement in their language. They eat vegetables,
daikon, bitter melon, garlic, onion, peppers, and tomatoes, as
well as some fish and tofu. They drink green tea. Before each
meal, they say “hara hachi bu,” meaning “Eat until you are
80% full.” Okinawans may be the only human population that
purposefully restricts how many calories they eat, and they do
it by reminding themselves to eat only until they are 80% full.
(It takes about 20 minutes for the stomach to tell the brain it is
full.) Okinawans tend to have a positive outlook, are kind, and
smile a lot. They avoid candy, cookies, and other sweets.
The notion of moai, which roughly means “meeting for a common purpose,” originated as the village’s financial support system.
If a village member died or was depressed, neighbors visited. They
create a safety net. The Okinawans tend to have close friends and
watch after them. (In contrast, the average American adult has only
two close friends he or she can count on, recently down from three.)
Processed food is avoided. They eat a lot of mugwort, which tends
to grow everywhere in Okinawa. Their food has a very low caloric
density yet is very nutritious. The typical Okinawan meal—a tofu
stir fry, miso soup, and some greens—has 3 or 4 times as much
volume and more nutrients than the typical hamburger eaten in
the USA, which has twice as many calories.
Okinawa’s longevity lessons include embracing an Ikigai
(having a purpose-imbued life that provides clear roles of responsibility and a feeling of being needed); relying on a plantbased diet (stir-fry vegetables, sweet potatoes, tofu, goya);
gardening (almost all Okinawan centenarians grow or once
grew a garden, a source of daily physical activity); eating more
soy (tofu and miso); maintaining moai (secure social networks);
enjoying the sunshine; staying active; planting a medicinal garden (mugwort, ginger, and turmeric); and having an attitude
(an affable smugness).
Unfortunately, the Okinawan culture of longevity is beginning to disappear with the encroaching American food culture.
Kentucky Fried Chicken and McDonalds were the last calamity
to befall Okinawa; the fast-food invasion has threatened many
of the positive behaviors that led to Okinawan longevity. Men
under 55 in Okinawa are now among the most obese and do
not live much longer than the Japanese average.
An American Blue Zone (Loma Linda, California). Loma
Linda, which is Spanish for “lovely hill,” is located about 60
Baylor University Medical Center Proceedings
Volume 27, Number 2
miles east of Los Angeles and is the home of the Seventh-Day
Adventists. Some of the most conservative Adventists do not
believe in going to the theater or movies or indulging in any
other form of popular culture. The Loma Linda University first
embarked on a study of the dietary habits of 25,000 Adventists
in California about 50 years ago. One key discovery of the
Adventists health study was that approximately half of the Adventists were vegetarians or rarely ate meat. The Adventists who
consumed nuts at least 5 times a week had about half the risk
of heart disease of those who did not. This was true of men and
women, vegetarians and nonvegetarians. Since that finding was
published in 1992, at least four major studies have confirmed
that eating nuts serves as a cardiovascular disease preventive.
The study also found that consuming fruits, vegetables, and
whole grains also was protective for a wide variety of cancers.
They found, for example, that the Adventists who ate meat had
a 65% increased risk of colon cancer compared with the vegetarian Adventists. Adventists who ate more legumes, like peas and
beans, had a 30% to 40% reduction in colon cancer. Pancreatic,
ovarian, and lung cancer frequencies were much lower in the
vegetarian Adventists than in the flesh-eating Adventists. Being
vegetarian, eating nuts, not smoking, being physically active,
and having a normal body weight added as much as a decade
to the lives of Adventists.
Being healthy has always been a fundamental part of the
Adventists’ message. One doesn’t have to be an Adventist to
admire how they have generated a Blue Zone out of whole cloth
by sticking together and reinforcing the right behaviors for longevity. These include finding a sanctuary in time (the weekly 24hour Sabbath, which provides a time to focus on family, God,
camaraderie, and nature); staying lean; getting regular moderate
exercise; spending time with like-minded friends; snacking on
nuts; giving something back (helping others); eating meat in
moderation; eating an early, light dinner (“eat breakfast like a
king, lunch like a prince, and dinner like a pauper”); eating more
fruits and vegetables; and drinking plenty of water.
Costa Rica’s Blue Zone. In 2002, Louis Rosero-Bixby, a demographer working with Costa Rican population data, noticed
that men living there seemed to be living longer than men
in more developed countries around the world. This fact had
gone unnoticed because in developing countries and in Central
America—a part of the world notorious for malaria, dengue
fever, and revolutions—most mortality studies did not even ask
if anyone lived past age 80, which was considered well beyond
the life expectancy of the area. Moreover, organizations like the
United Nations had assumed that many Costa Ricans exaggerated their ages so that any finding would be considered invalid.
Nevertheless, Louis Rosero-Bixby, the director of the Central
American Population Center in San Jose, took a sampling of
births recorded between 1890 and 1900 and then found the
death records. From that he calculated the average age of death
(life expectancy) and the chance of dying at any given age (mortality rate). Comparing these findings with data from developed
countries, he figured that a Costa Rican man at age 60 had
about twice the chance of reaching age 90 as did a man living
in the US, France, or even Japan. He also found that if a man
April 2014
reached 90, he could expect an average of another 4.4 years of
life—again a life expectancy higher that than in most developed
countries. Costa Rica spends only 15% of what America does
on health care, yet its people live longer, seemingly healthier
lives than people in other countries.
Rosero-Bixby identified a group of villages around the Nicoya
Peninsula in Costa Rica where the proportion of the oldest people was significantly higher than in the rest of the country. The
Nicoya Peninsula, until very recently, was one of the most isolated parts of Costa Rica. Buettner and his colleagues learned that
Nicoya, like all of Costa Rica, has the best public health system
in Central America—with good sewage systems, immunization
programs, and clinics in almost every village. The investigators
learned that Nicoyans had lived in relative isolation for the last
4 centuries, so their culture developed differently from that of the
rest of Costa Rica, although they are not genetically different. They
have the country’s lowest rates of cancer. The authors’ colleagues
interviewed about 20 of the oldest Nicoyans, asking them about
diet and hours of sleep, taking their blood pressure and heart rate,
and putting them through short physical tests. After considerable investigation and facts learned from the 1958 book entitled
Nicoya: A Cultural Geography by Phillip Wagner, the investigators
concluded that Nicoyans ate the emblematic low-caloric, low-fat,
plant-based diet rich in legumes. But, unlike in other Blue Zones,
the Nicoyan diet featured portions of corn tortillas at almost every
meal and huge quantities of tropical fruit. The water that Nicoyans
drank had calcium and magnesium contents higher than anywhere
else in Costa Rica. The investigators calculated that if the average
Nicoyan consumed (through drinking, cooking, or making coffee) 6 liters of water daily, he or she would ingest a gram a day of
calcium. (The World Health Organization had previously found
that populations drinking hard water had 25% fewer deaths from
heart disease than populations drinking soft water.) Thus, Costa
Rica’s longevity secrets include having a plan de vita (a strong sense
of purpose); drinking hard water (with a high calcium content);
keeping a focus on family; eating a light dinner; maintaining social
networks; keeping hard at work; getting some sensible sunlight;
and embracing a common history (modern Nicoyans’ roots to
the indigenous Chorotega and their traditions have enabled them
to remain relatively free of stress). Their traditional diet of fortified maize and beans may be the best nutritional combination for
longevity the world has ever known.
Previous areas of the world believed to be similar to the Blue
Zones described by Buettner, including the longevity claims
made decades ago about populations in Georgia in the Soviet
Union, in Pakistan’s Hunza Valley, and in Ecuador’s Vilcabamba
Valley, all turned out to be overstated and based on faulty data,
according to Buettner.
For those of us living in non–Blue Zone areas, Buettner recommends the following: natural movement (be active without
having to think about it); hara hachi bu (painlessly cut calories
by 20%); plant slant (avoid meat and processed food); purpose
now (take time to see the big picture); downshift (take time to
relieve stress); belong (participate in a spiritual community);
loved ones first (make family a priority); and right tribe (be
surrounded by those who share Blue Zone values).
Facts and ideas from anywhere
175
MUSINGS ON MORTALITY
Victor Brombert, a 90-yearold emeritus professor of literature at Yale and Princeton,
who escaped Hitler and fought
as a young American soldier on
Omaha Beach, has written Musings on Mortality: From Tolstoy to
Primo Levi, which examines how
eight major 20th-century authors
wrote about death (15). Since physicians face the end of life rather
frequently with their patients and
themselves, the book may be of
interest. It includes the thoughts
regarding this topic of Leo Tolstoy
(The Death of Ivan Ilych); Thomas Mann (Death in Venice, The
Magic Mountain, Mario and the Magician); Franz Kafka (The
Death Journey in the Everlasting Present); Virginia Woolf (To the
Lighthouse, Between the Acts, Jacob’s Room, Mrs. Dalloway, The
Waves, The Years, The Common Reader, A Room of One’s Own,
Orlando, Elegy); Albert Camus (The Stranger, The Plague, The
First Man, A Happy Death, Nuptials, The Myth of Sisyphus, The
Wind of Djémila, The Fall, The Exile and the Kingdom); Giorgio
Basani (The Garden of the Finzi-Continis, The Gold-Rimmed Spectacles, Five Stories of Ferrara, The Heron, “The Cardplayers”); J. M.
Coetzee (Waiting for the Barbarians, Boyhood, Elizabeth Costello,
Dusklands, In the Heart of the Country, Slow Man, The Good Soldier, Foe, Youth, Age of Iron, Disgrace, The Master of Petersburg);
and Primo Levi (The Search for Roots, The Wrench, The Periodic
Table, The Sixth Day, The Drowned and the Saved, Lager, Survival
in Auschwitz, If Not Now, When?, The Truce, If This Is a Man).
In the epilogue, Brombert emphasizes that Musings on
Mortality is not to be mistaken for meditations on death or
obsessions with it. Confronting mortality implies being alive,
questioning how to live, or raising moral issues. He affirms
that the need to live fully is “prompted by the recurrent sense
of the transitory and the perishable.” Thus, he stresses that we
should savor whatever hours we are granted, for soon enough
the eternal barman will announce with finality the last call.
THE PASSENGER PIGEON
Joel Greenberg has written
A Feathered River Across the Sky
about the disappearance of the
passenger pigeon (16). Two hundred years ago, the passenger pigeon was one of North America’s
greatest natural wonders. One
hundred years later it was gone, as
lost as the dinosaurs. Greenberg’s
book tells the sad story of how
this singular species, once the
most numerous bird on the planet, became extinct. The passenger
pigeon, a relative of the common
176
city pigeon, but larger and more brightly colored with a long
tail, once flew in America’s skies in flocks of astonishing size.
Around 1860, an English naturalist visiting the US wrote:
Early in the morning . . . I was perfectly amazed to behold
the air filled, the sun obscured by millions of pigeons . . . in a
vast mass a mile or more in breadth, and stretching before and
behind as far as the eye could reach. . . . It was late afternoon
before any decrease in the mass was perceptible. . . . The column
(allowing a probable velocity of sixty miles an hour) could not
have been less than 300 miles in length. That suggests there
were more than 3.7 billion birds in that flock—only a portion
of the entire continental population.
This report was not an outlier. Such distinguished ornithologists
as Alexander Wilson and John James Audubon reported similar
sightings, as did many others.
But, on September 1, 1914, Martha, a denizen of the Cincinnati Zoo, was found dead in her cage. She was the last of her
kind. Stuffed and mounted, she is in the Smithsonian, although
not currently on display. What could have driven a bird so
abundant as to blot out the sun into extinction in only half a
century? Joel Greenberg makes clear it was the combination of
three factors: the species’ peculiar nesting habits, the Industrial
Revolution, and human ignorance.
The passenger pigeon was a child of the once vast eastern
North American forest, a forest that stretched unbroken from
the Atlantic to well past the Mississippi River. The nut trees of
this forest, such as oak and beech, produced mast in prodigious
quantities, which animals like the passenger pigeon would feed
on, but mast is produced irregularly. One year in one area there
is a bumper crop; the next year that area will likely produce
next to none. So passenger pigeons not only migrated in mass
numbers, they also nestled that way, flocking to an area where
lots of mast had been produced the previous fall. These nesting
areas could themselves be almost unimaginably huge. One in
Wisconsin in 1872 covered 850 square miles of forest. A single
tree might contain a hundred nesting pairs or more. Some observers reported trees with as many as 600 nests.
In the morning, the males would leave the nesting area to
forage, returning at midday, when the females would leave.
About 2 weeks after the eggs hatched, the adults abandoned the
well-fed, indeed roly-poly squabs, who would flutter down to
the ground and begin feeding for themselves. After a few days
they would be strong enough to fly away.
Mass nesting in unpredictable locations was an effective reproductive strategy for the passenger pigeon as a species. Predators
who happened to be nearby would have a field day, but with so
many pigeons and squabs, they could hardly make a dent in the
total numbers. Even in the early days of European settlement,
when settlers armed with shotguns discovered they could bring
down a dozen or more pigeons with a single blast, human hunters
weren’t numerous enough to be a threat to the birds.
But in the 19th century, the burgeoning population of the
US surged westward, and the forest was increasingly turned to
farmland. The big eastern cities, growing in size, needed inexpensive food, and nothing was more plentiful and inexpensive
Baylor University Medical Center Proceedings
Volume 27, Number 2
than the pigeon, which could be cooked like chicken, then a
semi-luxury dish. But it was the railroad and telegraph, which
began to spread across the landscape in the 1830s and 1840s,
that proved lethal to the species.
Previously, hunters’ inability to predict where passenger pigeons would nest in a given year protected the creatures. With
the telegraph, however, the news of a major nesting could move
at the speed of light. With the railroad, market hunters could
converge in a few days and then send the slaughtered pigeons
to market. And slaughtered they were. Greenberg quotes one
pigeoner at the great Wisconsin nesting of 1872 attacking the
departing males in the morning.
Hundreds, yes thousands, dropped in the open fields below.
. . . The slaughter was terrible beyond any description. Our
guns became so hot by rapid discharges we were afraid to load
them. . . . Below the scene was truly pitiable. Not less than
2,500 birds covered the ground.
Having killed as many of the males as they could, the hunters moved in on the females and the squabs, who, unable to fly
yet, were easy pickings. Greenberg reported one estimate that
at least a hundred barrels, each holding 300 birds, were shipped
daily during the 40 days that the hunt lasted. That doesn’t count
the birds shipped alive, consumed locally, or just left to rot. Nor
does it count the myriad squabs that starved to death in the
nests because their parents had been killed.
Besides guns, nets were used. Designed like vast mouse traps,
they would be baited with corn and other grains and with tame
birds to lure the wild ones. (This was the origin of the term “stool
pigeon” because the birds were tethered to a small platform
called a stool.) When enough birds had gathered, the trap would
be sprung and snapped over the victims. The catch would be
enormous. One spring of a trap in Wisconsin yielded 35,000
birds. A three-man team in 1878 netted more than 50,000 birds
during the hunting season.
With this sort of predation, the number of passenger pigeons
declined rapidly. As it did so, the market hunters converged on
the remaining flocks, and the population crashed. By the 1890s,
the flocks were too scattered and too few to be worth pursuing
anymore. By that time it was too late. The last definite specimen
to be shot in the wild died in 1898. The last birds seen in the
wild were observed about a decade later. By 1912, only a few
birds, all captive, remained. Will humans survive our increasing population proliferation, nuclear weapons, and our rapidly
changing environment?
WAR ON POVERTY
January 2014 was the 50th anniversary of President Lyndon
B. Johnson’s declaration of the war on poverty. As Thomas G.
Donlan writes in Barron’s, “From it came Medicare, Medicaid,
Head Start, Community Action, and many other antipoverty
programs,” numbering at least 126 (17). “The poverty rate,” as
Donlan continues, “in 1964 was 19% and in 2013, 16%.” At
that rate, Donlan calculated that the poor will still be poor in
2264. The federal and state governments’ spending amounted
to more than $16 trillion (adjusted for inflation) over 50 years.
April 2014
Did all that money improve the economic potential of the
people who live in poverty? Donlan answers “yes.” Antipoverty
spending, now about $600 billion a year in our $3.4 trillion
federal budget and another $230 billion in antipoverty spending by the states, makes life in poverty less painful than in
1964, especially for the sick, aged, and children. That money,
however, has not brought meaningful education, positive attitudes, or better employment. The amount of money that
the US has spent on fighting poverty is close to the size of the
national debt.
The amount of money spent in 2013 on fighting poverty in
the US would have been enough to send every poor person a
check for $11,000, which is the annual US measure of poverty
for an individual. Many of the 46 million people in poverty were
pushed there by sickness, so more than half of the money spent
on fighting poverty goes through the Medicaid program. Thus,
poor people in ill health would still be needy if they received an
annual check for $11,000.
Donlan indicates that the 16% poverty rate is an annual
summation, but most people become poor temporarily and
then recover. The Census Bureau indicates that nearly 32% of
the nation’s households were in poverty for at least 2 months
from 2009 through 2011. It also indicates that only 3.5% of
households were in poverty for the whole 3 years.
Surprisingly, the standard government data on the income
of people in poverty does not include the value of povertyfighting benefits, the largest of which include the food people
buy with food stamps and other food subsidies, home-heating
subsidies, the earned income tax credit, the premium for private
health insurance that would substitute for Medicaid, free and
reduced-priced school lunches, and public housing and housing subsidies.
The Census Bureau’s statisticians of poverty developed
an alternative poverty rate a few years ago that accounts for
government programs as income. It also estimates expenses
for out-of-pocket health care, work-related expenses, and
child care expenses. For 2012, the overall poverty rate was
slightly higher, 16% for the supplemental poverty measure
vs. 15.1% with the official poverty measure in 2012. The
supplemental poverty measure shows that if there were no
government programs, the US would have a poverty rate of
nearly 30%.
DEFINING “PUBLIC SERVANTS”
Peggy Noonan, who usually has a piece in Saturday editions
of The Wall Street Journal, recently had a piece on selfishness in
our political life (18). I was struck by the following paragraph:
There’s an increasing sense in our political life that in both parties politicians call themselves public servants but act like bosses
who think the voters work for them. Physicians who routinely
help the needy and the uninsured do not call themselves servants. They get to be the 1%. Politicians who jerk around doctors, nurses and health systems call themselves servants, when
of course they look more like little kings and queens instructing
the grudging peasants in how to arrange their affairs.
Facts and ideas from anywhere
177
OPPORTUNITY ON MARS
On January 24, 2004, the rover Opportunity landed on the
Martian surface, and 10 years later it is still going strong (19).
Opportunity has finally spotted a place where the conditions
were once hospitable to living organisms. The first such site,
a complex of lake beds and streams, was revealed by NASA’s
Curiosity rover that landed on Mars in mid 2012. It is just
unbelievable to me that this rover is still roving 10 years after
it started on Mars. These kinds of accomplishments humble
medicine.
5.
6.
7.
8.
9.
10.
11.
12.
13.
1.
2.
3.
4.
William Clifford Roberts, MD
10 February 2014
14.
Beeson PB, Maulitz RC. The inner history of internal medicine. In Maulitz
RC, Long DE, eds. Grand Rounds: One Hundred Years of Internal Medicine.
Philadelphia: University of Pennsylvania Press, 1988:15–54.
Becker GS, Elias JJ. Cash for kidneys. Wall Street Journal, January 18–19,
2014.
Vance A. It’s faster to grow a kidney up here than down there. Bloomberg,
December 2–8, 2013.
Associated Press. Nine receive transplanted wombs. Dallas Morning News,
January 14, 2014.
15.
16.
17.
18.
19.
Associated Press. Woman, 58, to give birth to grandchild. Dallas Morning
News, January 9, 2014.
Alsever J. Trouble falling asleep? Ways to wind down faster. Wall Street
Journal, January 14, 2014.
Hellmich N. Obesity rate in USA levels off. USA Today, October 18,
2013.
Jalonick MC. Favorite foods are getting less fattening. Dallas Morning
News, January 2, 2014.
Guthrie A. Latin America’s public enemy #1: junk food. Wall Street Journal,
December 28–29, 2013.
50 years later, war against smoking aims at teens. USA Today, January 9,
2014.
Chretien K. Lessons from 23andMe home tests: self-testing is the future.
USA Today, January 9, 2014.
Mann S. Record number of students apply, enroll in medical school in
2013. AAMC Reporter, November 2013.
Olsen KD, Dacy MD. Mayo Clinic—150 years of serving humanity
through hope and healing. Mayo Clin Proc 2014;89(1):8–15.
Buettner D. The Blue Zones: Lessons for Living Longer from the People Who’ve
Lived the Longest. Washington, DC: National Geographic Society, 2008
(277 pp.).
Brombert V. Musings on Mortality: From Tolstoy to Primo Levi. Chicago:
University of Chicago Press, 2013 (188 pp.).
Greenberg J. A Feathered River Across the Sky: The Passenger Pigeon’s Flight
to Extinction. New York: Bloomsbury, 2014 (304 pp.).
Donlan TG. Poverty and measurement. Barron’s, January 13, 2014.
Noonan P. Our selfish ‘public servants.’ Wall Street Journal, January 18–19,
2014.
Watson T. Opportunity still rocking and roving on Red Planet. USA
Today, January 24, 2014.
Reader comments
Dear Dr. Roberts,
Just a quick note to say I always enjoy the Proceedings, but
especially so for the January 2014 issue. I liked the inclusion of
the tribute to Marvin and Bob Mennel’s words, and also your
good interview with Sabrina Dean Phillips—her remarks about
Baylor dovetailed nicely with the tribute. I’m going to send on
your interview and the White Coat Lecture to my grandson,
who’s considering medicine as a career, and I thought your
“Facts and Ideas from Anywhere” column especially relevant,
having just returned from 2 weeks in Antarctica!
Dear Dr. Roberts,
Thank you for publishing Dr. Donald Knowlan’s White
Coat Lecture at Georgetown University Medical School in the
Proceedings. It really is an inspiring piece, and we never would
have seen it had you not published it. I am making sure that
many of the Georgetown people I know have the chance to
read it.
—Jim Ronan, MD
Washington, DC
—Joe VanderVeer, MD
Devon, PA
178
Baylor University Medical Center Proceedings
Volume 27, Number 2
Selected published abstracts of Baylor researchers
AMERICAN JOURNAL OF CARDIOLOGY
Morphologic features of cardiac sarcoidosis in native hearts of
patients having cardiac transplantation
Roberts WC, Chung MS, Ko JM, Capehart JE, Hall SA
Am J Cardiol 2013 Nov 23 [Epub ahead of print]. Reprinted with
permission from Elsevier.
Described herein are 10 patients who underwent cardiac transplantation (CT) for severe chronic systolic heart failure resulting from
cardiac sarcoidosis. None had the diagnosis of sarcoidosis established
before CT except for the 3 patients who earlier had had a portion of
left ventricular wall excised for insertion of a left ventricular assist
device and non-caseating granulomas were present in the removed
myocardium. Although none of the 10 patients had significant narrowing of any of the epicardial coronary arteries, all had focal scarring
of the walls of the left and right ventricles and ventricular septum and
all had dilated ventricular cavities. The patients with the most ventricular wall scarring tended to have the fewest sarcoid granulomas in
the ventricular walls. Two patients had no sarcoid granulomas in the
excised heart although one did have typical sarcoid granulomas in the
portion of left ventricular wall excised to insert a left ventricular assist
device. Patients with cardiac sarcoidosis severe enough to warrant CT
had characteristic cardiac ventricular morphologic findings, and no
dysfunction of other non-cardiac organs, making clinical diagnosis of
cardiac sarcoidosis rather difficult.
BRITISH JOURNAL OF CANCER
Efficacy and safety of sunitinib in elderly patients with
metastatic renal cell carcinoma
Hutson TE, Bukowski RM, Rini BI, Gore ME, Larkin JM, Figlin RA,
Barrios CH, Escudier B, Lin X, Fly K, Martell B, Matczak E, Motzer RJ
Br J Cancer 2014 Jan 16 [Epub ahead of print]. Reprinted with permission from Nature Publishing Group.
Background: We retrospectively analyzed sunitinib outcome as a function of age in metastatic renal cell carcinoma (mRCC) patients.
Methods: Data were pooled from 1059 patients in six trials. KaplanMeier estimates of progression-free survival (PFS) and overall survival
(OS) were compared by log-rank test between patients aged <70 (n =
857; 81%) and ≥70 (n = 202; 19%) years.
Results: In first-line patients, median PFS was comparable in younger
and older patients, 9.9 vs 11.0 months, respectively (HR, 0.89; 95%
CI: 0.73–1.09; P = 0.2629), as was median OS, 23.6 vs 25.6 months
(HR, 0.93; 95% CI: 0.74–1.18; P = 0.5442). Similarly, in cytokinerefractory patients, median PFS was 8.1 vs 8.4 months (HR, 0.79; 95%
CI: 0.49–1.28; P = 0.3350), while median OS was 20.2 vs 15.8 months
(HR, 1.14; 95% CI: 0.73–1.79; P = 0.5657). Some treatment-emergent
adverse events were significantly less common in younger vs older patients,
including fatigue (60% vs 69%), cough (20% vs 29%), peripheral edema
(17% vs 27%), anemia (18% vs 25%), decreased appetite (13% vs 29%),
and thrombocytopenia (16% vs 25%; all P < 0.05). Hand-foot syndrome
was more common in younger patients (32% vs 24%).
Proc (Bayl Univ Med Cent) 2014;27(2):179–181
Conclusions: Advanced age should not be a deterrent to sunitinib
therapy and elderly patients may achieve additional clinical benefit.
HEALTH SERVICES RESEARCH
The impact of electronic health records on workflow and
financial measures in primary care practices
Fleming NS, Becker ER, Culler SD, Cheng D, McCorkle R, Graca BD, Ballard DJ
Health Serv Res 2014;49(1 Pt 2):405–420. Reprinted with permission
from John Wiley & Sons.
Objective: To estimate a commercially available ambulatory electronic
health record’s (EHR’s) impact on workflow and financial measures.
Data sources/study setting: Administrative, payroll, and billing data were
collected for 26 primary care practices in a fee-for-service network that
rolled out an EHR on a staggered schedule from June 2006 through
December 2008.
Study design: An interrupted time series design was used. Staffing, visit
intensity, productivity, volume, practice expense, payments received,
and net income data were collected monthly for 2004–2009. Changes
were evaluated 1–6, 7–12, and >12 months postimplementation.
Data collection/extraction methods: Data were accessed through a SQL
server database, transformed into SAS®, and aggregated by practice.
Practice-level data were divided by full-time physician equivalents for
comparisons across practices by month.
Principal findings: Staffing and practice expenses increased following EHR
implementation (3 and 6 percent after 12 months). Productivity, volume,
and net income decreased initially but recovered to/close to preimplementation levels after 12 months. Visit intensity did not change significantly,
and a secular trend offset the decrease in payments received.
Conclusions: Expenses increased and productivity decreased following
EHR implementation, but not as much or as persistently as might be
expected. Longer term effects still need to be examined.
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Anomalous cord from the raphe of a congenitally bicuspid aortic valve
to the aortic wall producing either acute or chronic aortic regurgitation
Vowels TJ, Gonzalez-Stawinski GV, Ko JM, Trachiotis GD, Roberts BJ,
Roberts CS, Roberts WC
J Am Coll Cardiol 2014;63(2):153–157. Reprinted with permission
from Elsevier.
Objectives: This report calls attention to an unappreciated cause of
both acute and chronic aortic regurgitation (AR).
Background: Although stenosis develops in most patients with a congenitally bicuspid aortic valve (BAV), in others with this anomaly,
pure AR (no element of stenosis) develops, some in the absence of
infection or other clear etiology.
Methods: We describe 5 men who underwent aortic valve replacement
for pure AR associated with a BAV containing an anomalous cord
attaching the raphe of the conjoined cusp near its free margin to the
wall of the ascending aorta cephalad to the sinotubular junction.
179
Results: Three of these 5 patients had a history of progressive dyspnea,
and the anomalous cord, which was intact at operation, appeared to
cause chronic AR by preventing proper coaptation of the 2 aortic valve
cusps. The other 2 patients heard a “pop” during physical exertion and
immediately became dyspneic, and at operation, the anomalous cord
was found to have ruptured. Prolapse of the conjoined aortic valve cusp
toward the left ventricular cavity resulted in severe acute AR.
Conclusions: This variant of the purely regurgitant BAV may cause
either chronic AR (when the anomalous cord does not rupture) or
acute severe AR (when the cord ruptures).
JOURNAL OF HEPATOLOGY
Role of magnetic resonance elastography in compensated and
decompensated liver disease
Asrani SK, Talwalkar JA, Kamath PS, Shah VH, Saracino G, Jennings
L, Gross JB, Venkatesh S, Ehman RL
J Hepatol 2013 Dec 19 [Epub ahead of print]. Reprinted with permission from Elsevier.
Background and aims: Non-invasive predictors identifying subjects
with compensated liver disease at highest risk for transitioning to a
decompensated state are lacking. We hypothesized that liver shear stiffness as measured by magnetic resonance elastography is an important
non-invasive predictor of hepatic decompensation.
Methods: Among patients with advanced fibrosis undergoing magnetic
resonance elastography (2007–11), a baseline cohort and follow up
cohort (compensated liver disease) were established. Cause specific
Cox proportional hazards analysis adjusting for competing risks was
utilized to determine the association between elevated liver shear stiffness and development of decompensation (hepatic encephalopathy,
ascites, variceal bleeding).
Results: In the baseline cohort (n = 430), subjects with decompensated liver
disease had a significantly higher mean liver shear stiffness (6.8 kPa, IQR
4.9–8.5) as compared to subjects with compensated liver disease (5.2 kPa,
IQR 4.1–6.8). After adjustment for Model for End Stage Liver Disease
score, hepatitis C, age, gender, albumin, and platelet count, the mean
liver shear stiffness (OR = 1.13, 95% CI 1.03–1.27) was independently
associated with decompensated cirrhosis at baseline. Over a median follow
up of 27 months (n = 167), 7.2% of subjects with compensated disease
experienced hepatic decompensation. In the follow up cohort, the hazard
of hepatic decompensation was 1.42 (95% CI 1.16–1.75) per unit increase
in liver shear stiffness over time. The hazard of hepatic decompensation
was 4.96 (95% CI 1.4–17.0, P = 0.019) for a subject with compensated
disease and mean LSS value ≥ 5.8 kPa as compared to an individual with
compensated disease and lower mean LSS values.
Conclusion: Baseline liver shear stiffness assessed by magnetic resonance elastography is independently associated with decompensated
liver disease.
LIVER TRANSPLANTATION
Antibody-mediated rejection as a contributor to previously
unexplained early liver allograft loss
O’Leary JG, Kaneku H, Demetris AJ, Marr JD, Shiller SM, Susskind
BM, Tillery GW, Terasaki PI, Klintmalm GB
Liver Transpl 2013 Nov 6 [Epub ahead of print]. Reprinted with permission from Wiley/American Association for the Study of Liver Diseases.
180
We analyzed 60 patients with idiopathic early allograft loss (defined
as death or retransplantation at <90 days) to determine the relative
contribution of preformed donor-specific human leukocyte antigen alloantibodies (DSAs) to this endpoint, and we defined strict criteria for
the diagnosis of antibody-mediated rejection (AMR) in liver allografts.
The inclusion criteria encompassed the availability of a pretransplant
serum sample and both postreperfusion and follow-up tissue specimens
for a blinded, retrospective re-review of histology and complement
component 4d (C4d) staining. AMR was diagnosed on the basis of
the presence of all 4 of the following strict criteria: (1) DSAs in serum, (2) histopathological evidence of diffuse microvascular injury/
microvasculitis consistent with antibody-mediated injury, (3) diffuse
C4d staining in the portal microvasculature with or without staining
in the sinusoids or central veins in at least 1 sample, and (4) the exclusion of other causes of a similar type of injury. Patients thought to
be experiencing definite AMR on the basis of routine histopathology
alone showed the highest levels of DSA sensitization. Forty percent
of patients with pretransplant DSAs with a pattern of bead saturation
after serial dilutions developed AMR. Another multiparous female
developed what appeared to be a strong recall response, which resulted in combined AMR and acute cellular rejection (ACR) causing
graft failure. A contribution of DSAs to allograft failure could not
be excluded for 3 additional patients who received marginal grafts.
In conclusion, liver allograft recipients with preformed DSAs with a
high mean fluorescence intensity despite dilution seem to be at risk for
clinically significant allograft injury and possibly for loss from AMR,
often in combination with ACR.
MOLECULAR GENETICS AND METABOLISM
Quantitative neuroimaging in mucolipidosis type IV
Schiffmann R, Mayfield J, Swift C, Nestrasil I
Mol Genet Metab 2013 Nov 21 [Epub ahead of print]. Reprinted with
permission from Elsevier.
Mucolipidosis type IV (MLIV) is an autosomal recessive disorder
resulting from mutations in the MCOLN1 gene. This gene encodes
the endosomal/lysosomal transient receptor potential channel protein mucolipin-1 (TRPML1). Affected patients suffer from neurodevelopmental abnormalities and progressive retinal dystrophy.
In a prospective natural history study we hypothesized the presence
of an additional slow cerebral neurodegenerative process. We have
recruited 5 patients, tested their neurodevelopmental status, and
measured cerebral regional volumes and white matter integrity using
MRI yearly. Over a period of up to 3 years, MLIV patients remained
neurologically stable. There was a trend for increased cortical and
subcortical gray matter volumes and increased ventricular size, while
white matter and cerebellar volumes decreased. Mean diffusivity
(MD) was increased and fractional anisotropy (FA) values were below
normal in all analyzed brain regions. There was a positive correlation
between motor scores of the Vineland Scale and the FA values in
the corticospinal tract (corr coef 0.39), and a negative correlation
with the MD values (corr coef –0.50) in the same brain region. We
conclude from these initial findings that deficiency in mucolipin-1
affects the entire brain but that there might be a selective regional
cerebral neurodegenerative process in MLIV. In addition, these data
suggest that diffusion-weighted imaging might be a good biomarker
for following patients with MLIV. Therefore, our findings may be
helpful for designing future clinical trials.
Baylor University Medical Center Proceedings
Volume 27, Number 2
SPINE JOURNAL
Analysis of the direct cost of surgery for four diagnostic
categories of adult spinal deformity
McCarthy IM, Hostin RA, O’Brien MF, Fleming NS, Ogola G, Kudyakov R,
Richter KM, Saigal R, Berven SH, Ames CP; International Spine Study
Group
Spine J 2013;13(12):1843–1848. Reprinted with permission from
Elsevier.
Background context: Existing literature on adult spinal deformity (ASD)
offers little guidance regarding an evidence-based approach to care. To
optimize the value of medical treatment, a thorough understanding
of the cost of surgical treatment for ASD is required.
Purpose: To evaluate four clinically and radiographically distinct groups
of ASD and identify and compare the cost of surgical treatment among
the groups.
Study design/setting: Multicenter retrospective study of consecutive
surgeries for ASD.
Background: The treatment of steroid-resistant rejection (SRR) is associated with severe recurrent hepatitis C virus (HCV) infection after
liver transplantation (LTx). After OKT3 was recently withdrawn from
the market, thymoglobulin (TG) became the principal treatment for
SRR.
Methods: A retrospective analysis of 32 HCV patients who were treated
for SRR with OKT3 (n = 15) or TG (n = 17) using yearly protocol
liver biopsies. Mean follow-up was 4.3 years (OKT3) and 3.2 years
(TG). We compared both groups for patient survival, graft loss, and
severity of HCV recurrence, manifested as the mean stage of fibrosis
(MSF).
Results: Patient survival at 1, 2, and 5 years after LTx was 80%, 73%,
and 67% in the OKT3 group and 82%, 77%, and 64% in the TG
group, respectively. At 2 years after LTx, the graft losses were 3 versus
4 in the OKT3 and TG groups, respectively. At years 1 and 2, the
MSF in the OKT3 group was 1.9 and 2.3 versus 2.4 and 2.8 in the
TG group, respectively. None of the differences between both groups
was statistically significant.
Patient sample: Three hundred twenty-five consecutive ASD patients
treated between 2008 and 2010.
Conclusion: There was no significant difference in patient survival,
graft loss, or severity of recurrent HCV, measured as MSF, between
both groups.
Outcome measures: Cost data were collected from hospital administrative records on the direct costs (DCs) incurred for the episode of
surgical care, excluding overhead.
West Nile virus infection in kidney and pancreas transplant recipients
in the Dallas-Fort Worth metroplex during the 2012 Texas epidemic
Methods: Based on preoperative radiographs and history, patients were
categorized into one of four diagnostic categories of deformity: primary idiopathic scoliosis (PIS), primary degenerative scoliosis (PDS),
primary sagittal plane deformity (PSPD), and revision (R). Analysis of
variance and generalized linear model regressions were used to analyze
the DCs of surgery and to assess differences in costs across the four
diagnostic categories considered.
Results: Significant differences were observed in DC of surgery for
different categories of ASD, with surgical treatment for PDS the most
expensive followed in decreasing order by PSPD, PIS, and R (P < .01).
Results further revealed a significant positive relationship between age
and DC (P < .01) and a significant positive relationship between length
of stay and DC (P < .01). Among PIS patients, for every incremental
increase in levels fused, the expected DC increased by $3,997 (P =
.00). Fusion to pelvis also significantly increased the DC of surgery
for patients aged 18 to 29 years (P < .01) and 30 to 59 years (P < .01)
but not for 60 years or more (P = .86).
Conclusions: There is an increasing DC of surgery with increasing age,
length of hospital stay, length of fusion, and fusions to the pelvis. Revision surgery is the least expensive surgery on average and should therefore not preclude its consideration from a pure cost perspective.
TRANSPLANTATION
A comparison of outcomes between OKT3 and antithymocyte
globulin for treatment of steroid-resistant rejection in hepatitis C
liver transplant recipients
Benjamin MM, Dasher KJ, Trotter JF
Transplantation 2013 Oct 17 [Epub ahead of print]. Reprinted with
permission from Wolters Kluwer Health.
April 2014
Yango AF, Fischbach BV, Levy M, Chandrakantan A, Tan V, Spak C,
Melton L, Rice K, Barri Y, Rajagopal A, Klintmalm G
Transplantation 2014 Jan 8 [Epub ahead of print]. Reprinted with
permission from Wolters Kluwer Health.
Background: In 2012, the United States experienced one of its worst
West Nile virus (WNV) epidemics, reporting 5,387 human cases and
final death toll of 243. Texas was at the epicenter of the outbreak,
with 1,875 reported cases and 89 deaths that year. The Texas outbreak
centered mainly in the Dallas–Fort Worth area where 30 deaths were
reported. We report three cases of severe WNV infection complicated
by meningoencephalitis in our organ transplant population.
Methods: Clinical data were collected from chart review. Therapy and
outcomes on three identified patients were reviewed and compared
with previously reported cases of WNV infection in kidney/pancreas
transplant recipients and the general population.
Results: Two recipients of kidney and one recipient of a combined kidney and pancreas transplant were treated at our center for WNV infection. All three patients presented with a rapid decline in mental status
within 24 hours of admission consistent with meningoencephalitis.
Diagnosis was made based on detection of WNV IgM in the serum.
All patients received intravenous immunoglobulin (IVIG) therapy at
400 mg/kg × 3 to 4 doses. As a result, two patients had a full recovery,
and one patient died.
Conclusion: Transplant recipients have a higher risk of neurologic complications from WNV infection. In areas where WNV is endemic,
clinicians must have a high index of suspicion when treating patients
presenting with fever, headache, and confusion. Full recovery in two of
three patients suggests a potential role of IVIG therapy in controlling
active WNV infection, particularly in immunosuppressed patients.
Selected published abstracts of Baylor researchers
181
2013
publications of the
Baylor Health Care System
medical and scientific staff
ANESTHESIOLOGY AND PAIN MANAGEMENT
1. Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE,
Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson
BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y,
Jaeschke R; American College of Critical Care Medicine. Clinical practice
guidelines for the management of pain, agitation, and delirium in adult
patients in the intensive care unit. Crit Care Med 2013;41(1):263–306.
2. Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE,
Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson
BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y,
Jaeschke R; American College of Critical Care Medicine. Clinical practice
guidelines for the management of pain, agitation, and delirium in adult
patients in the Intensive Care Unit: executive summary. Am J Health Syst
Pharm 2013;70(1):53–58.
3. Lagow EE, Leeper B, Jennings LW, Ramsay MAE. Incidence and severity
of respiratory insufficiency detected by transcutaneous carbon dioxide
monitoring after cardiac surgery and intensive care unit discharge. Proc
(Bayl Univ Med Cent) 2013;26(4):373–375.
4. Needleman SM. Safety of rapid intravenous infusion of acetaminophen.
Proc (Bayl Univ Med Cent) 2013;26(3):235–238.
5. Ramsay M. Advances in transplantation 1940–2014. Anesthesiol Clin
2013;31(4):645–658.
6. Ramsay M. Anesthesia for patients with liver disease. In Butterworth JF,
Mackey DC, Wasnick JD, eds. Morgan and Mikhail’s Clinical Anesthesiology,
5th ed. New York: McGraw-Hill/Lange, 2013.
7. Ramsay M. Biological cost of the depression of consciousness. Anestezjologia
I Ratownictwo 2013;7:94–100.
8. Ramsay MA. The chronic inflammation of obesity and its effects on surgery
and anesthesia. Int Anesthesiol Clin 2013;51(3):1–12.
9. Ramsay M. Hepatic physiology and anesthesia. In Butterworth JF, Mackey
DC, Wasnick JD, eds. Morgan and Mikhail’s Clinical Anesthesiology, 5th
ed. New York: McGraw-Hill/Lange, 2013.
10. Ramsay M. Justification for routine intensive care after liver transplantation.
Liver Transpl 2013;19(Suppl 2):S1–S5.
11. Ramsay M. Monitoring respiratory rate. In Ehrenfeld JM, Cannesson M, eds.
Monitoring Technologies in Acute Care Environments. A Comprehensive Guide to
Patient Monitoring Technology. New York: Springer, 2013:207–216.
12. Ramsay M. Role of microdialysis catheters in clinical decision making:
bench to bedside? Liver Transpl 2013;19(3):243–245.
13. Ramsay MA, Usman M, Lagow E, Mendoza M, Untalan E, De Vol E.
The accuracy, precision and reliability of measuring ventilatory rate and
detecting ventilatory pause by rainbow acoustic monitoring and capnometry.
Anesth Analg 2013;117(1):69–75.
14. Sessler CN, Riker RR, Ramsay MA. Evaluating and monitoring
sedation, arousal, and agitation in the ICU. Semin Respir Crit Care Med
2013;34(2):169–178.
CARDIOLOGY/CARDIAC, VASCULAR, AND THORACIC SURGERY
15. Adams J, Berbarie RF. High-intensity cardiac rehabilitation training of a
police officer for his return to work and sports after coronary artery bypass
grafting. Proc (Bayl Univ Med Cent) 2013;26(1):39–41.
16. Adams J, Cheng D, Berbarie RF. High-intensity, occupation-specific training in a series of firefighters during phase II cardiac rehabilitation. Proc (Bayl
Univ Med Cent) 2013;26(2):106–108; discussion, 26(4):429–431.
182
17. Adams J, Jordan S, Spencer K, Belanger J, Cheng D, Shock T, Karcher J.
Energy expenditure in US automotive technicians and occupation-specific
cardiac rehabilitation. Occup Med (Lond) 2013;63(2):103–108.
18. Afilalo J, Alexander KP, Mack MJ, Maurer MS, Green P, Allen LA, Popma
JJ, Ferrucci L, Forman DE. Frailty assessment in the cardiovascular care of
older adults. J Am Coll Cardiol 2013 Nov 18 [Epub ahead of print].
19. Arnold SV, Spertus JA, Lei Y, Green P, Kirtane AJ, Kapadia S, Thourani
VH, Herrmann HC, Beohar N, Zajarias A, Mack MJ, Leon MB, Cohen
DJ. How to define a poor outcome after transcatheter aortic valve
replacement: conceptual framework and empirical observations from the
placement of aortic transcatheter valve (PARTNER) trial. Circ Cardiovasc
Qual Outcomes 2013;6(5):591–597.
20. Askar M, Hsich E, Reville P, Nowacki AS, Baldwin W, Bakdash S,
Daghstani J, Zhang A, Klingman L, Smedira N, Moazami N, Taylor DO,
Starling RC, Gonzalez-Stawinski G. HLA and MICA allosensitization
patterns among patients supported by ventricular assist devices. J Heart
Lung Transplant 2013;32(12):1241–1248.
21. Benjamin MM, Fazel P, Filardo G, Choi JW, Stoler RC. Prevalence of and
risk factors of renal artery stenosis in patients with resistant hypertension.
Am J Cardiol 2013 Nov 23 [Epub ahead of print].
22. Benjamin MM, Filardo G, Donsky MS, Schussler JM. A pilot study of
prasugrel followed by post-procedural maintenance with clopidogrel in
patients receiving percutaneous coronary intervention. J Interv Cardiol
2013;26(1):38–42.
23. Benjamin MM, Roberts WC. Facts and principles learned at the 39th
Annual Williamsburg Conference on Heart Disease. Proc (Bayl Univ Med
Cent) 2013;26(2):124–136.
24. Brown CR, Shafii AE, Farver CF, Murthy SC, Pettersson GB, Mason DP.
Pathologic correlates of heparin-free donation after cardiac death in lung
transplantation. J Thorac Cardiovasc Surg 2013;145(5):e49–50.
25. Chamogeorgakis T, Lima B, Shafii AE, Nagpal D, Pokersnik JA, Navia
JL, Mason D, Gonzalez-Stawinski GV. Outcomes of axillary artery side
graft cannulation for extracorporeal membrane oxygenation. J Thorac
Cardiovasc Surg 2013;145(4):1088–1092.
26. Chamogeorgakis T, Rafael A, Shafii AE, Nagpal D, Pokersnik JA, GonzalezStawinski GV. Which is better: a miniaturized percutaneous ventricular
assist device or extracorporeal membrane oxygenation for patients with
cardiogenic shock? ASAIO J 2013;59(6):607–611.
27. Chen S, Shimoda M, Chen J, Grayburn PA. Stimulation of adult
resident cardiac progenitor cells by durable myocardial expression of
thymosin beta 4 with ultrasound-targeted microbubble delivery. Gene
Ther 2013;20(2):225–233.
28. Chung MS, Ko JM, Chamogeorgakis T, Hall SA, Roberts WC. The myth of
the Bernheim syndrome. Proc (Bayl Univ Med Cent) 2013;26(4):401–404.
29. Cianci C, Kowal RC, Feghali G, Hohmann S, Stoler RC, Choi JW.
Critical lower limb ischemia from an embolized Angio-Seal closure
device. Proc (Bayl Univ Med Cent) 2013;26(4):398–400.
30. da Graca B, Filardo G, Nicewander D. Consequences for healthcare
quality and research of the exclusion of records from the Death Master
File. Circ Cardiovasc Qual Outcomes 2013;6(1):124–128.
31. Davis M, Brennan JM, Vish N, Adams J, Muldoon M, Renbarger T,
Garner J. Lessons learned from study of depression in cardiovascular
patients in an acute-care heart and vascular hospital. Proc (Bayl Univ Med
Cent) 2013;26(1):6–9.
Proc (Bayl Univ Med Cent) 2014;27(2):182–196
32. Dewey TM, Bowers B, Thourani VH, Babaliaros V, Smith CR, Leon MB,
Svensson LG, Tuzcu EM, Miller DC, Teirstein PS, Tyner J, Brown DL,
Fontana GP, Makkar RR, Williams MR, George I, Kirtane AJ, Bavaria
JE, Mack MJ. Transapical aortic valve replacement for severe aortic
stenosis: results from the nonrandomized continued access cohort of the
PARTNER trial. Ann Thorac Surg 2013;96(6):2083–2089.
33. Dunagan J, Adams J, Cheng D, Barton S, Bigej-Cerqua J, Mims L,
Molden J, Anderson V. Development and evaluation of a treadmill-based
exercise tolerance test in cardiac rehabilitation. Proc (Bayl Univ Med Cent)
2013;26(3):247–251.
34. Edgerton J, Filardo G, Ryan WH, Brinkman WT, Smith RL, Hebeler
RF Jr, Hamman B, Sass DM, Harbor JP, Mack MJ. Risk of not being
discharged home after isolated coronary artery bypass graft operations.
Ann Thorac Surg 2013;96(4):1287–1292.
35. Edgerton JR, Herbert MA, Mahoney C, Armstrong D, Dewey TM,
Holper E, Roper K, Mack MJ. Long-term fate of patients discharged
to extended care facilities after cardiovascular surgery. Ann Thorac Surg
2013;96(3):871–877.
36. Eikelboom JW, Connolly SJ, Brueckmann M, Granger CB, Kappetein
AP, Mack MJ, Blatchford J, Devenny K, Friedman J, Guiver K, Harper R,
Khder Y, Lobmeyer MT, Maas H, Voigt JU, Simoons ML, Van de Werf
F; RE-ALIGN Investigators. Dabigatran versus warfarin in patients with
mechanical heart valves. N Engl J Med 2013;369(13):1206–1214.
37. Falcone AM, Choi JW, East C, Stoler RC, Fenves A, Laible E, Moshayedi
P, Dunkerley J, Waters K. Renal denervation for resistant hypertension.
Proc (Bayl Univ Med Cent) 2013;26(3):320–321.
38. Falcone AM, Matter GJ, Schussler JM. Right atrial appendage thrombus
found in a patient in normal sinus rhythm with normal right ventricular
systolic function. Echocardiography 2013;30(3):E70–E71.
39. Fazel P, Vallabhan RC, Roberts WC. Massive bloody pericardial effusion
as an initial manifestation of chronic kidney disease. Proc (Bayl Univ Med
Cent) 2013;26(1):33–34.
40. Foster E, Kwan D, Feldman T, Weissman NJ, Grayburn PA, Schwartz
A, Rogers JH, Kar S, Rinaldi MJ, Fail PS, Hermiller J, Whitlow PL,
Herrmann HC, Lim DS, Glower DD; EVEREST Investigators. Percutaneous mitral valve repair in the initial EVEREST cohort: evidence of reverse left ventricular remodeling. Circ Cardiovasc Imaging
2013;6(4):522–530.
41. Friedewald VE, Hayes SN, Pepine CJ, Roberts WC, Wenger NK. The
editor’s roundtable: the 10Q Report—advancing women’s heart health
through improved research, diagnosis, and treatment. Am J Cardiol
2013;112(10):1676–1687.
42. George BA, dePrisco G, Trotter JF, Henry AC III, Stoler RC. Ascites with
elevated protein content as the presenting sign of constrictive pericardial
disease. Proc (Bayl Univ Med Cent) 2013;26(2):168–170.
43. George BA, O’Hayre TA, Schussler JM. Association between congenitally
quadricuspid aortic valve and mitral valve prolapse. Proc (Bayl Univ Med
Cent) 2013;26(3):272–274.
44. Gierman JL, Shutze WP Sr., Pearl GJ, Foreman ML, Hohmann SE, Shutze
WP Jr. Thermoregulatory catheter–associated inferior vena cava thrombus.
Proc (Bayl Univ Med Cent) 2013;26(2):100–102.
45. Golba K, Mokrzycki K, Drozdz J, Cherniavsky A, Wrobel K, Roberts BJ,
Haddad H, Maurer G, Yii M, Asch FM, Handschumacher MD, Holly
TA, Przybylski R, Kron I, Schaff H, Aston S, Horton J, Lee KL, Velazquez
EJ, Grayburn PA; STICH TEE Substudy Investigators. Mechanisms of
functional mitral regurgitation in ischemic cardiomyopathy determined
by transesophageal echocardiography (from the Surgical Treatment for
Ischemic Heart Failure Trial). Am J Cardiol 2013;112(11):1812–1818.
46. Gopal A, Aranson N, Woo K, Clavijo L, Shavelle DM. Recalcitrant
peroneal artery pseudoaneurysm in a patient with hemophilia B. Cardiovasc
Revasc Med 2013;14(6):359–362.
47. Grayburn PA. New concepts in functional mitral regurgitation: it is not just
a disease of the left ventricle. J Am Coll Cardiol 2013;61(17):1817–1819.
48. Grayburn PA, Foster E, Sangli C, Weissman NJ, Massaro J, Glower DG,
Feldman T, Mauri L. Relationship between the magnitude of reduction
in mitral regurgitation severity and left ventricular and left atrial reverse
remodeling after MitraClip therapy. Circulation 2013;128(15):1667–1674.
April 2014
49. Green P, Cohen DJ, Généreux P, McAndrew T, Arnold SV, Alu M, Beohar
N, Rihal CS, Mack MJ, Kapadia S, Dvir D, Maurer MS, Williams MR,
Kodali S, Leon MB, Kirtane AJ. Relation between six-minute walk test
performance and outcomes after transcatheter aortic valve implantation
(from the PARTNER trial). Am J Cardiol 2013;112(5):700–706.
50. Grover FL, Mack MJ. The current role of coronary artery bypass in diabetics
with multivessel coronary disease. EuroIntervention 2013;9(2):183–186.
51. Harskamp RE, Alexander JH, Schulte PJ, Jones WS, Williams JB, Mack
MJ, Peterson ED, Gibson CM, Califf RM, Kouchoukos NT, Ferguson
TB, de Winter RJ, Lopes RD. Impact of extracardiac vascular disease on
vein graft failure and outcomes after coronary artery bypass surgery. Ann
Thorac Surg 2013 Dec 19 [Epub ahead of print].
52. Holper EM, Kim RJ, Mack M, Brown D, Brinkman W, Herbert M,
Stewart W, Vance K, Bowers B, Dewey T. Randomized trial of surgical
cutdown versus percutaneous access in transfemoral TAVR. Catheter
Cardiovasc Interv 2013 May 22 [Epub ahead of print].
53. Horton RP, Di Biase L, Hume A, Edgerton JR, Sanchéz JE, Natale AA. The
combined surgical/endocardial ablation procedure for atrial fibrillation. In
Al-Ahmad A, Callans D, Hsia HH, Natale A, Oseroff O, Wang PJ, eds.
Hands-On Ablation: The Expert’s Approach. Minneapolis, MN: Cardiotext
Publishing, 2013.
54. Hundae AY, Hebert CA, Schussler JM. Fibromuscular dysplasia of the
renal artery as a cause of secondary hypertension. Proc (Bayl Univ Med
Cent) 2013;26(4):405–406.
55. Kerwin KB, Pearl GJ, Molina CD, Coker PJ. Pineiro LA, Urschel HC Jr.,
East CA. Avoidance of lower-limb amputation by surgical implantation of
autologous stem cells. Proc (Bayl Univ Med Cent) 2013;26(3):285–287.
56. Keshava HB, Farver CF, Brown CR, Shafii AE, Murthy SC, Yun JJ,
Vakil N, Pettersson GB, Mason DP. Timing of heparin and thrombus
formation in donor lungs after cardiac death. Thorac Cardiovasc Surg
2013;61(3):246–250.
57. Khani-Hanjani A, Loor G, Chamogeorgakis T, Shafii A, Mountis M,
Hanna M, Soltesz E, Gonzalez-Stawinski GV. Case series using the
ROTAFLOW system as a temporary right ventricular assist device after
HeartMate II implantation. ASAIO J 2013;59(4):456–460.
58. Khvilivitzky K, Gonzalez-Stawinski GV. Bioprosthetic aortic valve changes
late after insertion of a left ventricular assist device. Proc (Bayl Univ Med
Cent) 2013;26(1):45–46.
59. Kim M, Muntner P, Sharma S, Choi JW, Stoler RC, Woodward M, Mann
DM, Farkouh ME. Assessing patient-reported outcomes and preferences
for same-day discharge after percutaneous coronary intervention: results
from a pilot randomized, controlled trial. Circ Cardiovasc Qual Outcomes
2013;6(2):186–192.
60. Kirtane AJ, Leon MB, Ball MW, Bajwa HS, Sketch MH Jr, Coleman PS,
Stoler RC, Papadakos S, Cutlip DE, Mauri L, Kandzari DE; ENDEAVOR
IV Investigators. The “final” 5-year follow-up from the ENDEAVOR IV
trial comparing a zotarolimus-eluting stent with a paclitaxel-eluting stent.
JACC Cardiovasc Interv 2013;6(4):325–333.
61. Lim DS, Reynolds MR, Feldman T, Kar S, Herrmann HC, Wang A, Whitlow
PL, Gray WA, Grayburn P, Mack MJ, Glower D. Improved functional status
and quality of life in prohibitive surgical risk patients with degenerative mitral
regurgitation following transcatheter mitral valve repair with the MitraClip®
System. J Am Coll Cardiol 2013 Oct 24 [Epub ahead of print].
62. Mack MJ, Brennan JM, Brindis R, Carroll J, Edwards F, Grover F, Shahian
D, Tuzcu EM, Peterson ED, Rumsfeld JS, Hewitt K, Shewan C, Michaels
J, Christensen B, Christian A, O’Brien S, Holmes D; STS/ACC TVT
Registry. Outcomes following transcatheter aortic valve replacement in
the United States. JAMA 2013;310(19):2069–2077.
63. Mack MJ, Head SJ, Holmes DR Jr, Ståhle E, Feldman TE, Colombo
A, Morice MC, Unger F, Erglis A, Stoler R, Dawkins KD, Serruys PW,
Mohr FW, Kappetein AP. Analysis of stroke occurring in the SYNTAX
trial comparing coronary artery bypass surgery and percutaneous coronary
intervention in the treatment of complex coronary artery disease. JACC
Cardiovasc Interv 2013;6(4):344–354.
64. Mack MJ, Holmes DR, Webb J, Cribier A, Kodali SK, Williams MR,
Leon MB. Patient selection for transcatheter aortic valve replacement.
J Am Coll Cardiol 2013;62(17 Suppl):S1–S10.
2013 publications of the Baylor Health Care System medical and scientific staff
183
65. Magee MJ, Herbert MA, Roper KL, Holper E, Dewey TM, Snelus T,
Mack MJ. Pulmonary function tests overestimate chronic pulmonary disease in patients with severe aortic stenosis. Ann Thorac Surg
2013;96(4):1329–1335.
66. Main ML, Grayburn PA, Lang RM, Goldman JH, Gibson CM, Sherwin P,
DeMaria AN. Effect of Optison on pulmonary artery systolic pressure and
pulmonary vascular resistance. Am J Cardiol 2013;112(10):1657–1661.
67. Mauri L, Foster E, Glower DD, Apruzzese P, Massaro JM, Herrmann
HC, Hermiller J, Gray W, Wang A, Pedersen WR, Bajwa T, Lasala J, Low
R, Grayburn P, Feldman T; EVEREST II Investigators. 4-year results of
a randomized controlled trial of percutaneous repair versus surgery for
mitral regurgitation. J Am Coll Cardiol 2013;62(4):317–328.
68. McMaster KS, Blanc JMB, Hamman BL, Rosenthal RL. Abnormal origin
of the left internal thoracic artery detected only by computed tomography.
Proc (Bayl Univ Med Cent) 2013;26(3):283–284.
69. Moussa ID, Klein LW, Shah B, Mehran R, Mack MJ, Brilakis ES, Reilly
JP, Zoghbi G, Holper E, Stone GW. Consideration of a new definition of
clinically relevant myocardial infarction after coronary revascularization: an
expert consensus document from the Society for Cardiovascular Angiography
and Interventions (SCAI). J Am Coll Cardiol 2013;62(17):1563–1570.
70. Nagpal AD, Chamogeorgakis T, Shafii AE, Hanna M, Miller CM, Fung
J, Gonzalez-Stawinski GV. Combined heart and liver transplantation: the
Cleveland Clinic experience. Ann Thorac Surg 2013;95(1):179–182.
71. Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra
PG, Dubuc M, Reddy V, Nelson L, Holcomb RG, Lehmann JW, Ruskin
JN; STOP AF Cryoablation Investigators. Reply: CryoBalloon ablation:
first results of North American STOP AF pivotal trial. J Am Coll Cardiol
2013;62(14):1307–1308.
72. Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG,
Dubuc M, Reddy V, Nelson L, Holcomb RG, Lehmann JW, Ruskin
JN; STOP AF Cryoablation Investigators. Cryoballoon ablation of
pulmonary veins for paroxysmal atrial fibrillation: first results of the
North American Arctic Front (STOP AF) pivotal trial. J Am Coll Cardiol
2013;61(16):1713–1723.
73. Parker JM, Weller MW, Feinstein LM, Adams RJ, Main ML, Grayburn
PA, Cosgrove DO, Goldberg BA, Darge K, Nihoyannopoulos P, Wilson S,
Monaghan M, Piscaglia F, Fowlkes B, Mathias W, Moriyasu F, Chammas
MC, Greenbaum L, Feinstein SB. Safety of ultrasound contrast agents
in patients with known or suspected cardiac shunts. Am J Cardiol
2013;112(7):1039–1045.
74. Patankar GR, Choi JW, Schussler JM. Reverse takotsubo cardiomyopathy: two case reports and review of the literature. J Med Case Rep
2013;7(1):84.
75. Pearl GJ. ATOS in the competitive athlete. In Illig KA, Thompson RW,
Freischlag JA, Donahue DM, Jordan SE, Edgelow PI, eds. Thoracic Outlet
Syndrome. London: Springer, 2013:565–571.
76. Pearl GJ. Brachiocephalic reconstruction. In Cameron JL, Cameron AM, eds.
Current Surgical Therapy, 11th ed. Philadelphia: Elsevier, 2013:836–843.
77. Pearl GJ. NTOS in the competitive athlete. In Illig KA, Thompson RW,
Freischlag JA, Donahue DM, Jordan SE, Edgelow PI, eds. Thoracic Outlet
Syndrome. London: Springer, 2013:81–85.
78. Pearl GJ. Outcomes after treatment of ATOS. In Illig KA, Thompson
RW, Freischlag JA, Donahue DM, Jordan SE, Edgelow PI, eds. Thoracic
Outlet Syndrome. London: Springer, 2013:615–619.
79. Pinard EA, Fazal S, Schussler JM. Catastrophic paradoxical embolus after
hemodialysis access thrombectomy in a patient with a patent foramen
ovale. Int Urol Nephrol 2013;45(4):1215–1217.
80. Podduturi V, Armstrong DR, Hitchcock MA, Roberts WC, Guileyardo
JM. Isolated atrial amyloidosis: the importance of molecular classification.
Proc (Bayl Univ Med Cent) 2013;26(4):387–389.
81. Prasad A, Zareh M, Doherty R, Gopal A, Vora H, Somma K, Mehra A,
Clavijo LC, Matthews RV, Shavelle DM. Use of regadenoson for measurement of fractional flow reserve. Catheter Cardiovasc Interv 2013 Jun 13
[Epub ahead of print].
82. Rankin JS, He X, O’Brien SM, Jacobs JP, Welke KF, Filardo G, Shahian
DM. The Society of Thoracic Surgeons risk model for operative mortality
after multiple valve surgery. Ann Thorac Surg 2013;95(4):1484–1490.
184
83. Roberts WC, Filardo G, Ko JM, Siegel RJ, Dollar AL, Ross EM, Shirani
J. Comparison of total 12-lead QRS voltage in a variety of cardiac conditions and its usefulness in predicting increased cardiac mass. Am J Cardiol
2013;112(6):904–909.
84. Roberts WC, Roberts CC, Ko JM, Grayburn PA, Tandon A, Kuiper JJ,
Capehart JE, Hall SA. Dramatically different phenotypic expressions of
hypertrophic cardiomyopathy in male cousins undergoing cardiac transplantation with identical disease-causing gene mutation. Am J Cardiol
2013;111(12):1818–1822.
85. Roberts WC, Stoler RC, Grayburn PA, Hebeler RF Jr, Ko JM, Brown DL,
Brinkman WT, Mack MJ, Guileyardo JM. Necropsy findings early after
transcatheter aortic valve implantation for aortic stenosis. Am J Cardiol
2013;111(3):448–452.
86. Roberts WC, Vowels TJ, Filardo G, Ko JM, Mathur RP, Shirani J. Natural
history of unoperated aortic stenosis during a 50-year period of cardiac
valve replacement. Am J Cardiol 2013;112(4):541–553.
87. Roberts WC, Vowels TJ, Ko JM, Hebeler RF Jr. Gross and histologic
features of excised portions of posterior mitral leaflet in patients having
operative repair of mitral valve prolapse and comments on the concept
of missing (=ruptured) chordae tendineae. J Am Coll Cardiol 2013 Nov
30 [Epub ahead of print].
88. Roberts WC, Zafar S, Ko JM. Morphological features of temporal arteritis.
Proc (Bayl Univ Med Cent) 2013;26(2):109–115.
89. Roberts WC, Zafar S, Ko JM, Carry MM, Hebeler RF. Combined congenitally bicuspid aortic valve and mitral valve prolapse causing pure
regurgitation. Proc (Bayl Univ Med Cent) 2013;26(1):30–32.
90. Saxon RR, Chervu A, Jones PA, Bajwa TK, Gable DR, Soukas PA, Begg
RJ, Adams JG, Ansel GM, Schneider DB, Eichler CM, Rush MJ. Heparin-bonded, expanded polytetrafluoroethylene-lined stent graft in the
treatment of femoropopliteal artery disease: 1-year results of the VIPER
(Viabahn Endoprosthesis with Heparin Bioactive Surface in the Treatment
of Superficial Femoral Artery Obstructive Disease) trial. J Vasc Interv Radiol
2013;24(2):165–173.
91. Schussler JM. Trends and advances in transradial access. Diagnostic and
Interventional Cardiology, May 20, 2013. Available at http://www.dicardiology.
com/article/trends-and-advances-transradial-access.
92. Shahian DM, He X, Jacobs JP, Rankin JS, Peterson ED, Welke KF, Filardo
G, Shewan CM, O’Brien SM. Issues in quality measurement: target population, risk adjustment, and ratings. Ann Thorac Surg 2013;96(2):718–726.
93. Shutze W, Gierman J, McQuade K, Pearl G, Smith B. Treatment of
proximal vertebral artery disease. Vascular 2013 Mar 21 [Epub ahead
of print].
94. Svensson LG, Adams DH, Bonow RO, Kouchoukos NT, Miller DC,
O’Gara PT, Shahian DM, Schaff HV, Akins CW, Bavaria JE, Blackstone
EH, David TE, Desai ND, Dewey TM, D’Agostino RS, Gleason TG,
Harrington KB, Kodali S, Kapadia S, Leon MB, Lima B, Lytle BW, Mack
MJ, Reardon M, Reece TB, Reiss GR, Roselli EE, Smith CR, Thourani VH, Tuzcu EM, Webb J, Williams MR. Aortic valve and ascending
aorta: guidelines for management and quality measures. Ann Thorac Surg
2013;95(6 Suppl):S1–S66.
95. Tandon A, Grayburn PA. Imaging of low-gradient severe aortic stenosis.
JACC Cardiovasc Imaging 2013;6(2):184–195.
96. Thompson RW, Pearl GJ. Neurovascular injuries in the throwing shoulder.
In Dines JS, Altchek DW, Andrews J, ElAttrache NS, Wilk K, Yocum
L, eds. Sports Medicine of Baseball. Philadelphia: Lippincott Williams &
Wilkins, 2013:180–193.
97. van Diepen S, Brennan JM, Hafley GE, Reyes EM, Allen KB, Ferguson
TB, Peterson ED, Williams JB, Gibson CM, Mack MJ, Kouchoukos
NT, Alexander JH, Lopes RD. Endoscopic harvesting device type and
outcomes in patients undergoing coronary artery bypass surgery. Ann Surg
2013 Dec 23 [Epub ahead of print].
98. Wenger NK, Hayes SN, Pepine CJ, Roberts WC. Cardiovascular care for
women: the 10-Q Report and beyond. Am J Cardiol 2013;112(4):S2.
99. Zafar S, Roberts WC. Congenitally bicuspid aortic valve in brothers:
coarctation of the aorta with a normally functioning aortic valve in one
and no coarctation but severe aortic stenosis in the other. Proc (Bayl Univ
Med Cent) 2013;26(2):171–173.
Baylor University Medical Center Proceedings
Volume 27, Number 2
DERMATOLOGY
100. Abramovits W. Autoinflammatory diseases and syndromes in dermatology.
Preface. Dermatol Clin 2013;31(3):xi.
101. Abramovits W, Oquendo M. Introduction to autoinflammatory syndromes
and diseases. Dermatol Clin 2013;31(3):363–385.
102. Abramovits W, Oquendo M, Vincent KD, Gupta AK. PICATO (ingenol
mebutate 0.015% and 0.05% gels): a novel treatment for actinic keratosis.
Skinmed 2013;11(2):111–115.
103. Abramovits W, Rivas Bejarano JJ, Valdecantos WC. Role of interleukin
1 in atopic dermatitis. Dermatol Clin 2013;31(3):437–444.
104. Augustin M, Blome C, Costanzo A, Dauden E, Ferrandiz C, Girolomoni
G, Gniadecki R, Iversen L, Menter A, Michaelis-Wittern K, Morita A,
Nakagawa H, Reich K. Nail Assessment in Psoriasis and Psoriatic Arthritis
(NAPPA): Development and validation of a tool for assessment of nail
psoriasis outcomes. Br J Dermatol 2013 Oct 11 [Epub ahead of print].
105. Boehncke WH, Menter A. Burden of disease: psoriasis and psoriatic
arthritis. Am J Clin Dermatol 2013;14(5):377–388.
106. Duncan FJ, Silva KA, Johnson CJ, King BL, Szatkiewicz JP, Kamdar SP,
Ong DE, Napoli JL, Wang J, King LE Jr, Whiting DA, McElwee KJ,
Sundberg JP, Everts HB. Endogenous retinoids in the pathogenesis of
alopecia areata. J Invest Dermatol 2013;133(2):334–343.
107. Gottlieb AB, Matheson RT, Menter A, Leonardi CL, Day RM, Hu C,
Schafer PH, Krueger JG. Efficacy, tolerability, and pharmacodynamics
of apremilast in recalcitrant plaque psoriasis: a phase II open-label study.
J Drugs Dermatol 2013;12(8):888–897.
108. Gupta AK, Paquet M, Abramovits W. ONMEL (itraconazole) 200-mg
tablet. Skinmed 2013;11(2):105–107.
109. Gupta AK, Simpson FC, Abramovits W. Efinaconazole 10% nail solution.
Skinmed 2013;11(4):239–241.
110. Horner ME, Alikhan A, Tintle S, Tortorelli S, Davis DM, Hand JL.
Cutaneous porphyrias part I: epidemiology, pathogenesis, presentation,
diagnosis, and histopathology. Int J Dermatol 2013;52(12):1464–1480.
111. Kimball AB, Pariser D, Yamauchi PS, Menter A, Teller CF, Shi Y, Yong M,
Creamer K, Hooper M, Aras G, Kricorian G, Gelfand JM. OBSERVE-5
interim analysis: an observational postmarketing safety registry of etanercept
for the treatment of psoriasis. J Am Acad Dermatol 2013;68(5):756–764.
112. Kivelevitch DN, Hebeler KR, Patel M, Menter A. Emerging topical
treatments for psoriasis. Expert Opin Emerg Drugs 2013;18(4):523–532.
113. Kragballe K, Menter A, Lebwohl M, Tebbey PW, van de Kerkhof PC;
International Psoriasis Council. Long-term management of scalp psoriasis:
perspectives from the International Psoriasis Council. J Dermatolog Treat
2013;24(3):188–192.
114. Lebwohl MG, Del Rosso JQ, Abramovits W, Berman B, Cohen
DE, Guttman E, Mancini AJ, Schachner LA. Pathways to managing
atopic dermatitis: consensus from the experts. J Clin Aesthet Dermatol
2013;6(7 Suppl):S2–S18.
115. Mamolo C, Harness J, Tan H, Menter A. Tofacitinib (CP-690,550),
an oral Janus kinase inhibitor, improves patient-reported outcomes in a
phase 2b, randomized, double-blind, placebo-controlled study in patients
with moderate-to-severe psoriasis. J Eur Acad Dermatol Venereol 2013
Jan 7 [Epub ahead of print].
116. Mansouri B, Patel M, Menter A. Biological therapies for psoriasis. Expert
Opin Biol Ther 2013;13(12):1715–1730.
117. Mansouri B, Patel M, Menter A. Tumour necrosis factor-α inhibitor
use in patients with psoriasis with organ transplantation. Br J Dermatol
2013;169(2):481–483.
118. Menter A, Gold LS, Bukhalo M, Grekin S, Kempers S, Boyce BM, Ganslandt
C, Villumsen J, Lebwohl M. Calcipotriene plus betamethasone dipropionate
topical suspension for the treatment of mild to moderate psoriasis vulgaris
on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs
Dermatol 2013;12(1):92–98.
119. Mercy K, Kwasny M, Cordoro KM, Menter A, Tom WL, Korman N,
Belazarian L, Armstrong AW, Levy ML, Paller AS. Clinical manifestations
of pediatric psoriasis: results of a multicenter study in the United States.
Pediatr Dermatol 2013;30(4):424–428.
120. Mitsui H, Suárez-Fariñas M, Gulati N, Shah KR, Cannizzaro MV,
Coats I, Felsen D, Krueger JG, Carucci JA. Gene expression profiling
April 2014
121.
122.
123.
124.
125.
126.
127.
of the leading edge of cutaneous squamous cell carcinoma: IL-24-driven
MMP-7. J Invest Dermatol 2013 Nov 22 [Epub ahead of print].
Paller AS, Mercy K, Kwasny MJ, Choon SE, Cordoro KM, Girolomoni
G, Menter A, Tom WL, Mahoney AM, Oostveen AM, Seyger MM.
Association of pediatric psoriasis severity with excess and central
adiposity: an international cross-sectional study. JAMA Dermatol
2013;149(2):166–176.
Papp K, Menter A, Poulin Y, Gu Y, Sasso EH. Long-term outcomes of
interruption and retreatment vs. continuous therapy with adalimumab
for psoriasis: subanalysis of REVEAL and the open-label extension study.
J Eur Acad Dermatol Venereol 2013;27(5):634–642.
Ryan C, Shaw RE, Cockerell CJ, Hand S, Ghali FE. Novel sodium hypochlorite cleanser shows clinical response and excellent acceptability in the treatment of atopic dermatitis. Pediatr Dermatol
2013;30(3):308–315.
Shah KR, Boland CR, Patel M, Thrash B, Menter A. Cutaneous
manifestations of gastrointestinal disease: part I. J Am Acad Dermatol
2013;68(2):189.e1–e21.
Strober B, Buonanno M, Clark JD, Kawabata T, Tan H, Wolk R, Valdez
H, Langley RG, Harness J, Menter A, Papp K. Effect of tofacitinib, a
Janus kinase inhibitor, on haematological parameters during 12 weeks
of psoriasis treatment. Br J Dermatol 2013;169(5):992–999.
Thrash B, Patel M, Shah KR, Boland CR, Menter A. Cutaneous
manifestations of gastrointestinal disease: part II. J Am Acad Dermatol
2013;68(2):211.e1–e33.
Warren RB, Menter A. Dermatology: future therapeutic perspectives.
Dermatol Ther (Heidelb) 2013;3(2):115–116.
EMERGENCY MEDICINE
Note: See also Trauma.
128. Brown BJ. Valproate related hyperammonemic encephalopathy. Michigan
College of Emergency Physicians News & Views, Jan/Feb 2013.
129. Kline JA, Hernandez J, Garrett JS, Jones AE. Pilot study of a protocol to
administer inhaled nitric oxide to treat severe acute submassive pulmonary
embolism. Emerg Med J 2013 Apr 13 [Epub ahead of print].
ENDOCRINOLOGY
Note: See also Transplantation for articles on islet cell transplantation.
130. Bode BW, Buse JB, Fisher M, Garg SK, Marre M, Merker L, Renard
E, Russell-Jones DL, Hansen CT, Rana A, Heller SR; BEGIN® BasalBolus Type 1 trial investigators. Insulin degludec improves glycaemic
control with lower nocturnal hypoglycaemia risk than insulin glargine
in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes
(BEGIN(®) Basal-Bolus Type 1): 2-year results of a randomized clinical
trial. Diabet Med 2013;30(11):1293–1297.
131. Hollander P, Gupta AK, Plodkowski R, Greenway F, Bays H, Burns C,
Klassen P, Fujioka K; COR-Diabetes Study Group. Effects of naltrexone
sustained-release/bupropion sustained-release combination therapy on
body weight and glycemic parameters in overweight and obese patients
with type 2 diabetes. Diabetes Care 2013;36(12):4022–4099.
132. Hollander P, Lasko B, Barnett AH, Bengus M, Kanitra L, Pi-Sunyer FX,
Balena R. Effects of taspoglutide on glycemic control and body weight in
obese patients with type 2 diabetes (T-Emerge 7 study). Obesity (Silver
Spring) 2013;21(2):238–247.
133. Mathieu C, Hollander P, Miranda-Palma B, Cooper J, Franek E, RussellJones D, Larsen J, Tamer SC, Bain SC; NN1250-3770 (BEGIN: Flex T1)
Trial Investigators. Efficacy and safety of insulin degludec in a flexible dosing
regimen vs insulin glargine in patients with type 1 diabetes (BEGIN: Flex
T1): a 26-week randomized, treat-to-target trial with a 26-week extension.
J Clin Endocrinol Metab 2013;98(3):1154–1162.
134. Meneghini L, Kesavadev J, Demissie M, Nazeri A, Hollander P. Once-daily
initiation of basal insulin as add-on to metformin: a 26-week, randomized,
treat-to-target trial comparing insulin detemir with insulin glargine in
patients with type 2 diabetes. Diabetes Obes Metab 2013;15(8):729–736.
135. Nathan DM, Bayless M, Cleary P, Genuth S, Gubitosi-Klug R, Lachin
JM, Lorenzi G, Zinman B; DCCT/EDIC Research Group. Diabetes
control and complications trial/epidemiology of diabetes interventions
2013 publications of the Baylor Health Care System medical and scientific staff
185
136.
137.
138.
139.
140.
141.
142.
and complications study at 30 years: advances and contributions. Diabetes
2013;62(12):3976–3986.
Niswender K, Piletic M, Andersen H, Hiort LC, Hollander P. Weight
change upon once-daily initiation of insulin detemir with or without
dietary intervention in overweight or obese insulin-naïve individuals
with type 2 diabetes: results from the DIET trial. Diabetes Obes Metab
2013 Oct 1 [Epub ahead of print].
Renthal N, Roe ED, Adams-Huet B, Raskin P. A novel glucose-insulin
infusion maintains perioperative glycamic control through multiple
transitions of care. J Perioperative Practice 2013;23(10):222–227.
Rodbard HW, Cariou B, Zinman B, Handelsman Y, Philis-Tsimikas A,
Skjøth TV, Rana A, Mathieu C; BEGIN Once Long trial investigators.
Comparison of insulin degludec with insulin glargine in insulin-naive
subjects with type 2 diabetes: a 2-year randomized, treat-to-target trial.
Diabet Med 2013;30(11):1298–1304.
Roe ED, Pon NC, Hollander P, Raskin P. The ‘collateral benefits’ of noninsulin
therapies for type 2 diabetes. Diabetes Manage 2013;3(2):145–160.
Vora J, Bain SC, Damci T, Dzida G, Hollander P, Meneghini LF,
Ross SA. Incretin-based therapy in combination with basal insulin: a
promising tactic for the treatment of type 2 diabetes. Diabetes Metab
2013;39(1):6–15.
Wadden TA, Hollander P, Klein S, Niswender K, Woo V, Hale PM,
Aronne L; NN8022-1923 Investigators. Weight maintenance and
additional weight loss with liraglutide after low-calorie-diet-induced
weight loss: the SCALE Maintenance randomized study. Int J Obes (Lond)
2013;37(11):1443–1451.
Wilding JP, Charpentier G, Hollander P, González-Gálvez G, Mathieu
C, Vercruysse F, Usiskin K, Law G, Black S, Canovatchel W, Meininger
G. Efficacy and safety of canagliflozin in patients with type 2 diabetes
mellitus inadequately controlled with metformin and sulphonylurea: a
randomised trial. Int J Clin Pract 2013;67(12):1267–1282.
GASTROENTEROLOGY
Note: See also Oncology for research on colon cancer.
143. Fordtran JS, Goyal RK, Feldman M, Soll AH, Trier JS, Ockner RK,
Larusso NF, Podolsky DK, Brenner DA, Rustgi AK, Omary MB.
Gastroenterology’s editors-in-chief: historical and personal perspectives
of their editorships. Gastroenterology 2013;145(1):16–31.
144. Kathiria AS, Butcher MA, Hansen JM, Theiss AL. Nrf2 is not required
for epithelial prohibitin-dependent attenuation of experimental colitis.
Am J Physiol Gastrointest Liver Physiol 2013;304(10):G885–G896.
145. Theiss AL. Sphingosine-1-phosphate: Driver of NFκB and STAT3 persistent activation in chronic intestinal inflammation and colitis-associated
cancer. JAKSTAT 2013;2(3):e24150.
146. Thompson CC, Chand B, Chen YK, Demarco DC, Miller L, Schweitzer
M, Rothstein RI, Lautz DB, Slattery J, Ryan MB, Brethauer S, Schauer
P, Mitchell MC, Starpoli A, Haber GB, Catalano MF, Edmundowicz S,
Fagnant AM, Kaplan LM, Roslin MS. Endoscopic suturing for transoral
outlet reduction increases weight loss after Roux-en-Y gastric bypass
surgery. Gastroenterology 2013;145(1):129–137.e3.
147. Van Dinter TG Jr, John L, Guileyardo JM, Fordtran JS. Intestinal perforation caused by insertion of a nasogastric tube late after gastric bypass. Proc
(Bayl Univ Med Cent) 2013;26(1):11–15.
HEALTH CARE RESEARCH AND IMPROVEMENT
Note: This section represents primarily the publications of the IHCRI staff, although
some of those publications are included under other areas.
148. Bayley KB, Belnap T, Savitz L, Masica AL, Shah N, Fleming NS.
Challenges in using electronic health record data for CER: experience of 4 learning organizations and solutions applied. Med Care
2013;51(8 Suppl 3):S80–S86.
149. Carter JL, Trungale KR, Barnes SA. From bedside to graveside: increased
stress among healthcare chaplains. J Pastoral Care Counsel 2013;67(4):1–8.
150. Collinsworth AW, Vulimiri M, Schmidt KL, Snead CA. Effectiveness
of a community health worker-led diabetes self-management education
program and implications for CHW involvement in care coordination
strategies. Diabetes Educ 2013;39(6):792–799.
186
151. da Graca B, Filardo G, Nicewander D. Consequences for healthcare
quality and research of the exclusion of records from the death master
file. Circ Cardiovasc Qual Outcomes 2013;6(1):124–128.
152. Filardo G, Lederle FA, Ballard DJ, Hamilton C, da Graca B, Herrin J,
Harbor J, Vanbuskirk JB, Johnson GR, Powell JT. Immediate open repair
vs surveillance in patients with small abdominal aortic aneurysms: survival
differences by aneurysm size. Mayo Clin Proc 2013;88(9):910–919.
153. Fleming NS, Becker ER, Culler SD, Cheng D, McCorkle R, Graca
BD, Ballard DJ. The impact of electronic health records on workflow
and financial measures in primary care practices. Health Serv Res 2013
Dec 21 [Epub ahead of print].
154. Goz V, Weinreb JJ, McCarthy I, Schwab F, Lafage V, Errico T. Perioperative
complications and mortality after spinal fusions; analysis of trends and risk
factors. Spine (Phila Pa 1976) 2013;38(22):1970–1976.
155. Hart R, McCarthy I, O’Brien M, Bess S, Line B, Adjei OB, Burton D,
Gupta M, Ames C, Deviren V, Khaled Kebaish, Shaffrey C, Wood K,
Hostin R; International Spine Study Group Denver, CO. Identification
of decision criteria for revision surgery among patients with proximal
junctional failure following surgical treatment for spinal deformity. Spine
(Phila Pa 1976) 2013 Jun 17 [Epub ahead of print].
156. Holter V, Crenshaw JT, Gilder R. Content analysis of continuing education
for cervical cytology. Int J Evid Based Healthc 2013;11(4):291–298.
157. Hostin R, O’Brien M, McCarthy I, Bess S, Gupta M, Klineberg E;
International Spine Study Group, Denver, CO. Retrospective study of
anterior interbody fusion rates and patient outcomes of using mineralized
collagen and bone marrow aspirate in multilevel adult spinal deformity
surgery. J Spinal Disord Tech 2013 Nov 6 [Epub ahead of print].
158. Jacobs JP, He X, O’Brien SM, Welke KF, Filardo G, Han JM, Ferraris
VA, Prager RL, Shahian DM. Variation in ventilation time after coronary
artery bypass grafting: an analysis from the Society of Thoracic Surgeons
adult cardiac surgery database. Ann Thorac Surg 2013;96(3):757–762.
159. Kennerly DA, Saldaña M, Kudyakov R, da Graca B, Nicewander D,
Compton J. Description and evaluation of adaptations to the global
trigger tool to enhance value to adverse event reduction efforts. J Patient
Saf 2013 Jan 17 [Epub ahead of print].
160. Klineberg E, Gupta M, McCarthy I, Hostin R. Detection of pseudarthrosis in adult spinal deformity: the use of health-related quality-of-life
outcomes to predict pseudarthrosis. J Spinal Disord Tech 2013 Dec 11
[Epub ahead of print].
161. Masica AL, Ewen E, Daoud YA, Cheng D, Franceschini N, Kudyakov
RE, Bowen JR, Brouwer ES, Wallace D, Fleming NS, West SL. Comparative effectiveness research using electronic health records: impacts
of oral antidiabetic drugs on the development of chronic kidney disease.
Pharmacoepidemiol Drug Saf 2013;22(4):413–422.
162. McCarthy I, Hostin R, O’Brien M, Fleming N, Ogola G, Kudyakov R,
Richter K, Berven S, Saigal R, Ames C, International Spine Study Group.
Analysis of direct cost of surgery for four diagnostic categories of adult
spinal deformity. Spine J 2013;13(12):1843–1848.
163. McCarthy I, Hostin R, O’Brien M, Fleming N, Ogola G, Kudyakov R,
Richter K, Saigal R, Berven S, Deviren V, Ames C, International Spine
Study Group. Cost-effectiveness of surgical treatment for adult spinal
deformity: a comparison of dollars per quality of life improvement across
health domains. Spine Deformity 2013;1(4):293–298.
164. McCarthy I, Hostin R, O’Brien M, Saigal R, Ames CP. Health economic analysis of adult deformity surgery. Neurosurg Clin N Am 2013;24(2):293–304.
165. Newgard CD, Fildes JJ, Wu L, Hemmila MR, Burd RS, Neal M, Mann
NC, Shafi S, Clark DE, Goble S, Nathens AB. Methodology and analytic
rationale for the American College of Surgeons Trauma Quality Improvement
Program. J Am Coll Surg 2013;216(1):147–157.
166. Nuss TD, Bryant L, Edwards M. Patient privacy in an open-access
environment. Compliance Today 2013 (April);66–73.
167. Probst CA, Shaffer VA, Chan YR. The effect of defaults in an electronic
health record on laboratory test ordering practices for pediatric patients.
Health Psychol 2013;32(9):995–1002.
168. Shaffer VA, Probst CA, Merkle EC, Arkes HR, Medow MA. Why do
patients derogate physicians who use a computer-based diagnostic support
system? Med Decis Making 2013;33(1):108–118.
Baylor University Medical Center Proceedings
Volume 27, Number 2
169. Sobrino J, Barnes SA, Dahr N, Kudyakov R, Berryman C, Nathens
AB, Hemmila MR, Neal M, Shafi S. Frequency of adoption of practice
management guidelines at trauma centers. Proc (Bayl Univ Med Cent)
2013;26(3):256–261.
170. Sobrino J, Shafi S. Timing and causes of death after injuries. Proc (Bayl
Univ Med Cent) 2013;26(2):120–123.
171. Staggers N, Xiao Y, Chapman L. Debunking health IT usability myths.
Appl Clin Inform 2013;4(2):241–250.
188.
189.
190.
HEPATOLOGY
Note: See also Transplantation.
172. Asrani SK, Kamath PS. Natural history of cirrhosis. Curr Gastroenterol
Rep 2013;15(2):308.
173. Asrani SK, Larson JJ, Yawn B, Therneau TM, Kim WR. Underestimation of liver-related mortality in the United States. Gastroenterology
2013;145(2):375–382.e1–2.
174. Asrani SK, Talwalkar JA, Kamath PS, Shah VH, Saracino G, Jennings L,
Gross JB, Venkatesh S, Ehman RL. Role of magnetic resonance elastography in compensated and decompensated liver disease. J Hepatol 2013
Dec 19 [Epub ahead of print].
175. Asrani SK, Warnes CA, Kamath PS. Hepatocellular carcinoma after the
Fontan procedure. N Engl J Med 2013;368(18):1756–1757.
176. Gonzalez SA. Acute Liver Failure: Diagnosis and Management (BMJ Point
of Care Monograph), 4th ed. London: BMJ Group, 2013. Available at
https://online.epocrates.com/home.
177. Gonzalez SA. Future directions in hepatitis C therapy. In Emerging
Therapeutic Options for Hepatitis C. London: Future Science Group,
2013:98–111.
178. Rahimi RS, Elliott AC, Rockey DC. Altered mental status in cirrhosis:
etiologies and outcomes. J Investig Med 2013;61(4):695–700.
179. Rahimi RS, Landaverde C. Nonalcoholic fatty liver disease and the
metabolic syndrome: clinical implications and treatment. Nutr Clin
Pract 2013;28(1):40–51.
180. Rahimi RS, Rockey DC. End-stage liver disease complications. Curr
Opin Gastroenterol 2013;29(3):257–263.
181. Singal AG, Rahimi RS, Clark C, Ma Y, Cuthbert JA, Rockey DC,
Amarasingham R. An automated model using electronic medical record
data identifies patients with cirrhosis at high risk for readmission. Clin
Gastroenterol Hepatol 2013;11(10):1335–1341.e1.
182. Singh S, Fujii LL, Murad MH, Wang Z, Asrani SK, Ehman RL,
Kamath PS, Talwalkar JA. Liver stiffness is associated with risk of
decompensation, liver cancer, and death in patients with chronic liver
diseases: a systematic review and meta-analysis. Clin Gastroenterol
Hepatol 2013;11(12):1573–1584.e1–2.
IMMUNOLOGY/BASIC SCIENCES
Note: Some publications of the BRI/BIIR staff are listed under Neurology,
Dermatology, and Transplantation.
183. Aghaeepour N, Finak G; FlowCAP Consortium; DREAM Consortium,
Hoos H, Mosmann TR, Brinkman R, Gottardo R, Scheuermann RH.
Critical assessment of automated flow cytometry data analysis techniques.
Nat Methods 2013;10(3):228–238.
184. Banchereau R, Cepika AM, Pascual V. Systems approaches to human
autoimmune diseases. Curr Opin Immunol 2013;25(5):598–605.
185. Bao M, Liu YJ. Regulation of TLR7/9 signaling in plasmacytoid dendritic
cells. Protein Cell 2013;4(1):40–52.
186. Bentebibel SE, Lopez S, Obermoser G, Schmitt N, Mueller C, Harrod
C, Flano E, Mejias A, Albrecht RA, Blankenship D, Xu H, Pascual V,
Banchereau J, Garcia-Sastre A, Palucka AK, Ramilo O, Ueno H. Induction
of ICOS+CXCR3+CXCR5+ TH cells correlates with antibody responses to
influenza vaccination. Sci Transl Med 2013;5(176):176ra32.
187. Bloom CI, Graham CM, Berry MP, Rozakeas F, Redford PS, Wang
Y, Xu Z, Wilkinson KA, Wilkinson RJ, Kendrick Y, Devouassoux G,
Ferry T, Miyara M, Bouvry D, Valeyre D, Gorochov G, Blankenship
D, Saadatian M, Vanhems P, Beynon H, Vancheeswaran R,
Wickremasinghe M, Chaussabel D, Banchereau J, Pascual V, Ho LP,
Lipman M, O’Garra A. Transcriptional blood signatures distinguish
April 2014
191.
192.
193.
194.
195.
196.
197.
198.
199.
200.
201.
202.
203.
204.
205.
206.
207.
208.
pulmonary tuberculosis, pulmonary sarcoidosis, pneumonias and
lung cancers. PLoS One 2013;8(8):e70630.
Chujo D, Foucat E, Nguyen TS, Chaussabel D, Banchereau J, Ueno
H. ZnT8-specific CD4+ T cells display distinct cytokine expression
profiles between type 1 diabetes patients and healthy adults. PLoS One
2013;8(2):e55595.
Coffman RL. Converging discoveries: the first reports of IL-4. J Immunol
2013;190(3):847–848.
Coussens LM, Zitvogel L, Palucka AK. Neutralizing tumor-promoting
chronic inflammation: a magic bullet? Science 2013;339(6117):286–291.
Ding Q, Cao X, Lu J, Huang B, Liu YJ, Kato N, Shu HB, Zhong J.
Hepatitis C virus NS4B blocks the interaction of STING and TBK1 to
evade host innate immunity. J Hepatol 2013;59(1):52–58.
Disis ML, Palucka K. Evaluation of cancer immunity in mice. Cold Spring
Harb Protoc 2013 Sep 30 [Epub ahead of print].
Duluc D, Gannevat J, Anguiano E, Zurawski S, Carley M, Boreham
M, Stecher J, Dullaers M, Banchereau J, Oh S. Functional diversity
of human vaginal APC subsets in directing T-cell responses. Mucosal
Immunol 2013;6(3):626–638.
Duluc D, Gannevat J, Joo H, Ni L, Upchurch K, Boreham M, Carley
M, Stecher J, Zurawski G, Oh S. Dendritic cells and vaccine design for
sexually-transmitted diseases. Microb Pathog 2013;58:35–44.
Flamar AL, Xue Y, Zurawski SM, Montes M, King B, Sloan L, Oh S,
Banchereau J, Levy Y, Zurawski G. Targeting concatenated HIV antigens
to human CD40 expands a broad repertoire of multifunctional CD4+
and CD8+ T cells. AIDS 2013;27(13):2041–2051.
Klechevsky E, Banchereau J. Human dendritic cells subsets as targets and
vectors for therapy. Ann N Y Acad Sci 2013;1284:24–30.
Lee S, Cantarel B, Henrissat B, Gevers D, Birren BW, Huttenhower C,
Ko G. Gene-targeted metagenomic analysis of glucan-branching enzyme
gene profiles among human and animal fecal microbiota. ISME J 2013
Oct 10 [Epub ahead of print].
Lin YC, Murre C. Nuclear location and the control of developmental
progression. Curr Opin Genet Dev 2013;23(2):104–108.
Margine I, Hai R, Albrecht RA, Obermoser G, Harrod AC, Banchereau
J, Palucka K, García-Sastre A, Palese P, Treanor JJ, Krammer F. H3N2
influenza virus infection induces broadly reactive hemagglutinin stalk
antibodies in humans and mice. J Virol 2013;87(8):4728–4737.
Martirosyan A, Ohne Y, Degos C, Gorvel L, Moriyón I, Oh S, Gorvel
JP. Lipopolysaccharides with acylation defects potentiate TLR4 signaling
and shape T cell responses. PLoS One 2013;8(2):e55117.
Mejias A, Dimo B, Suarez NM, Garcia C, Suarez-Arrabal MC, Jartti
T, Blankenship D, Jordan-Villegas A, Ardura MI, Xu Z, Banchereau J,
Chaussabel D, Ramilo O. Whole blood gene expression profiles to assess
pathogenesis and disease severity in infants with respiratory syncytial
virus infection. PLoS Med 2013;10(11):e1001549.
Mitoma H, Hanabuchi S, Kim T, Bao M, Zhang Z, Sugimoto N, Liu
YJ. The DHX33 RNA helicase senses cytosolic RNA and activates the
NLRP3 inflammasome. Immunity 2013;39(1):123–135.
Obermoser G, Presnell S, Domico K, Xu H, Wang Y, Anguiano E,
Thompson-Snipes L, Ranganathan R, Zeitner B, Bjork A, Anderson
D, Speake C, Ruchaud E, Skinner J, Alsina L, Sharma M, Dutartre H,
Cepika A, Israelsson E, Nguyen P, Nguyen QA, Harrod AC, Zurawski
SM, Pascual V, Ueno H, Nepom GT, Quinn C, Blankenship D, Palucka
K, Banchereau J, Chaussabel D. Systems scale interactive exploration
reveals quantitative and qualitative differences in response to influenza
and pneumococcal vaccines. Immunity 2013;38(4):831–844.
Palucka K. Q&A: Evidence presenter. Interview by Marian Turner. Nature
2013;504(7480):S9.
Palucka K, Banchereau J. Dendritic-cell-based therapeutic cancer
vaccines. Immunity 2013;39(1):38–48.
Palucka K, Banchereau J. Human dendritic cell subsets in vaccination.
Curr Opin Immunol 2013;25(3):396–402.
Palucka K, Coussens LM, O’Shaughnessy J. Dendritic cells, inflammation,
and breast cancer. Cancer J 2013;19(6):511–516.
Palucka AK, Pulendran B. Linking genome and immunity. Curr Opin
Immunol 2013;25(5):549–550.
2013 publications of the Baylor Health Care System medical and scientific staff
187
209. Park J, Munagala I, Xu H, Blankenship D, Maffucci P, Chaussabel D,
Banchereau J, Pascual V, Cunningham-Rundles C. Interferon signature
in the blood in inflammatory common variable immune deficiency. PLoS
One 2013;8(9):e74893.
210. Schmitt N, Bustamante J, Bourdery L, Bentebibel SE, Boisson-Dupuis S,
Hamlin F, Tran MV, Blankenship D, Pascual V, Savino DA, Banchereau J,
Casanova JL, Ueno H. IL-12 receptor β1 deficiency alters in vivo T follicular
helper cell response in humans. Blood 2013;121(17):3375–3385.
211. Schmitt N, Ueno H. Blood Tfh cells come with colors. Immunity
2013;39(4):629–630.
212. Schmitt N, Ueno H. Human T follicular helper cells: development and
subsets. Adv Exp Med Biol 2013;785:87–94.
213. Voo KS, Bover L, Harline ML, Vien LT, Facchinetti V, Arima K, Kwak
LW, Liu YJ. Antibodies targeting human OX40 expand effector T cells
and block inducible and natural regulatory T cell function. J Immunol
2013;191(7):3641–3650.
214. Yu CI, Becker C, Wang Y, Marches F, Helft J, Leboeuf M, Anguiano
E, Pourpe S, Goller K, Pascual V, Banchereau J, Merad M, Palucka
K. Human CD1c+ dendritic cells drive the differentiation of CD103+
CD8+ mucosal effector T cells via the cytokine TGF-β. Immunity
2013;38(4):818–830.
215. Zhang Z, Bao M, Lu N, Weng L, Yuan B, Liu YJ. The E3 ubiquitin ligase
TRIM21 negatively regulates the innate immune response to intracellular
double-stranded DNA. Nat Immunol 2013;14(2):172–178.
INTERNAL MEDICINE AND FAMILY MEDICINE
Note: Most family medicine and internal medicine articles are subclassified by
specialty, even if generalists were first authors or coauthors.
216. Abdul-Karim R, Ryan C, Rangel C, Emmett M. Levamisole-induced
vasculitis. Proc (Bayl Univ Med Cent) 2013;26(2):163–165.
217. Arroyo M, Fenves AZ, Emmett M. The calcium-alkali syndrome. Proc
(Bayl Univ Med Cent) 2013;26(2):179–181.
218. Benjamin MM, Gummelt KL, Zaki R, Afzal A, Sloan L, Shamim S.
Herpes simplex virus meningitis complicated by ascending paralysis.
Proc (Bayl Univ Med Cent) 2013;26(3):265–267.
219. George J, Graves R, Meador R Jr. Inguinal lymphadenopathy as the initial
presentation of sarcoidosis. Proc (Bayl Univ Med Cent) 2013;26(2):161–162.
220. Ha KY, Tyring SK. Vibrio vulnificus necrotizing fasciitis preceding herpes
zoster. Proc (Bayl Univ Med Cent) 2013;26(1):55–57.
221. Mantas AM, Wells J, Trotter J. Kayser-Fleischer rings of acute Wilson’s
disease. Proc (Bayl Univ Med Cent) 2013;26(2):166–167.
222. Patel T, Tietze D, Mehta AN. Amlodipine overdose. Proc (Bayl Univ Med
Cent) 2013;26(4):410–411.
223. Robinson SD, Cooper B, Leday TV. Copper deficiency (hypocupremia)
and pancytopenia late after gastric bypass surgery. Proc (Bayl Univ Med
Cent) 2013;26(4):382–386.
METABOLIC DISEASES
224. Bottiglieri T. Folate, vitamin B12, and S-adenosylmethionine. Psychiatr
Clin North Am 2013;36(1):1–13.
225. Butler LM, Arning E, Wang R, Bottiglieri T, Govindarajan S, Gao YT,
Yuan JM. Prediagnostic levels of serum one-carbon metabolites and
risk of hepatocellular carcinoma. Cancer Epidemiol Biomarkers Prev
2013;22(10):1884–1893.
226. Christensen KE, Deng L, Leung KY, Arning E, Bottiglieri T, Malysheva
OV, Caudill MA, Krupenko NI, Greene ND, Jerome-Majewska L,
MacKenzie RE, Rozen R. A novel mouse model for genetic variation in
10-formyltetrahydrofolate synthetase exhibits disturbed purine synthesis
with impacts on pregnancy and embryonic development. Hum Mol Genet
2013;22(18):3705–3719.
227. Dainese L, Monin ML, Demeret S, Brochier G, Froissart R, Spraul
A, Schiffmann R, Seilhean D, Mochel F. Abnormal glycogen in
astrocytes is sufficient to cause adult polyglucosan body disease. Gene
2013;515(2):376–379.
228. Fonseca VA, Lavery LA, Thethi TK, Daoud Y, DeSouza C, Ovalle F, Denham
DS, Bottiglieri T, Sheehan P, Rosenstock J. Metanx in type 2 diabetes with
peripheral neuropathy: a randomized trial. Am J Med 2013;126(2):141–149.
188
229. Forni S, Pearl PL, Gibson KM, Yu Y, Sweetman L. Quantitation of
gamma-hydroxybutyric acid in dried blood spots: feasibility assessment
for newborn screening of succinic semialdehyde dehydrogenase (SSADH)
deficiency. Mol Genet Metab 2013;109(3):255–259.
230. Forni S, Pearl PL, Gibson KM, Yu Y, Sweetman L. Response to Stove
and colleagues concerning newborn screening of succinic semialdehyde
dehydrogenase (SSADH) deficiency in dried blood spots. Mol Genet
Metab 2013;110(1–2):196.
231. Gauthier N, Wu JW, Wang SP, Allard P, Mamer OA, Sweetman L, Moser
AB, Kratz L, Alvarez F, Robitaille Y, Lépine F, Mitchell GA. A liver-specific
defect of Acyl-CoA degradation produces hyperammonemia, hypoglycemia
and a distinct hepatic Acyl-CoA pattern. PLoS One 2013;8(7):e60581.
232. Glier MB, Ngai YF, Sulistyoningrum DC, Aleliunas RE, Bottiglieri T,
Devlin AM. Tissue-specific relationship of S-adenosylhomocysteine
with allele-specific H19/Igf2 methylation and imprinting in mice with
hyperhomocysteinemia. Epigenetics 2013;8(1):44–53.
233. Inoue-Choi M, Nelson HH, Robien K, Arning E, Bottiglieri T, Koh WP,
Yuan JM. Plasma S-adenosylmethionine, DNMT polymorphisms, and
peripheral blood LINE-1 methylation among healthy Chinese adults in
Singapore. BMC Cancer 2013;13(1):389.
234. Lai SC, Nakayama Y, Sequeira JM, Wlodarczyk BJ, Cabrera RM, Finnell
RH, Bottiglieri T, Quadros EV. The transcobalamin receptor knockout
mouse: a model for vitamin B12 deficiency in the central nervous system.
FASEB J 2013;27(6):2468–2475.
235. Meng XL, Eto Y, Schiffmann R, Shen JS. HIV tat domain improves crosscorrection of human galactocerebrosidase in a gene- and flanking sequencedependent manner. Mol Ther Nucleic Acids 2013 Oct 22;2:e130.
236. Schiffmann R, Ries M, Blankenship D, Nicholls K, Mehta A, Clarke
JT, Steiner RD, Beck M, Barshop BA, Rhead W, West M, Martin R,
Amato D, Nair N, Huertas P. Changes in plasma and urine globotriaosylceramide levels do not predict Fabry disease progression over 1 year
of agalsidase alfa. Genet Med 2013;15(12):983–989.
237. Simons C, Wolf NI, McNeil N, Caldovic L, Devaney JM, Takanohashi
A, Crawford J, Ru K, Grimmond SM, Miller D, Tonduti D, Schmidt
JL, Chudnow RS, van Coster R, Lagae L, Kisler J, Sperner J, van der
Knaap MS, Schiffmann R, Taft RJ, Vanderver A. A de novo mutation
in the β-tubulin gene TUBB4A results in the leukoencephalopathy
hypomyelination with atrophy of the basal ganglia and cerebellum. Am
J Hum Genet 2013;92(5):767–773.
238. Skvorak KJ, Dorko K, Marongiu F, Tahan V, Hansel MC, Gramignoli
R, Arning E, Bottiglieri T, Gibson KM, Strom SC. Improved amino
acid, bioenergetic metabolite and neurotransmitter profiles following
human amnion epithelial cell transplant in intermediate maple syrup
urine disease mice. Mol Genet Metab 2013;109(2):132–138.
239. Totonchy MB, Tamura D, Pantell MS, Zalewski C, Bradford PT, Merchant
SN, Nadol J, Khan SG, Schiffmann R, Pierson TM, Wiggs E, Griffith AJ,
DiGiovanna JJ, Kraemer KH, Brewer CC. Auditory analysis of xeroderma
pigmentosum 1971-2012: hearing function, sun sensitivity and DNA repair
predict neurological degeneration. Brain 2013;136(Pt 1):194–208.
240. Vanderver A, Tonduti D, Bernard G, Lai J, Rossi C, Carosso G, Quezado
M, Wong K, Schiffmann R. More than hypomyelination in Pol-III
disorder. J Neuropathol Exp Neurol 2013;72(1):67–75.
241. Vogel KR, Arning E, Wasek BL, Bottiglieri T, Gibson KM. Characterization of 2-(methylamino)alkanoic acid capacity to restrict blood-brain
phenylalanine transport in Pah enu2 mice: preliminary findings. Mol
Genet Metab 2013;110(Suppl):S71–S78.
242. Vogel KR, Arning E, Wasek BL, Bottiglieri T, Gibson KM. Nonphysiological amino acid (NPAA) therapy targeting brain phenylalanine reduction: pilot studies in PAHENU2 mice. J Inherit Metab Dis
2013;36(3):513–523.
NEUROLOGY/NEUROSURGERY
Note: See also Health Care Research and Improvement for articles related to spine surgery.
243. Chad DA, Rowland LP, Armon C, Bedlack R, Durham H, FactorLitvak P, Heiman-Patterson T, Heitzman D, Lacomis D, Ludolph A,
Maragakis N, Miller R, Pattee G, Shoesmith C, Sorenson E, Turner
MR. Peer recommendations on how to improve clinical research, and
Baylor University Medical Center Proceedings
Volume 27, Number 2
244.
245.
246.
247.
248.
249.
250.
251.
252.
253.
254.
255.
256.
257.
conference wrap-up. Amyotroph Lateral Scler Frontotemporal Degener
2013;14(Suppl 1):67–73.
Cudkowicz ME, van den Berg LH, Shefner JM, Mitsumoto H, Mora
JS, Ludolph A, Hardiman O, Bozik ME, Ingersoll EW, Archibald D,
Meyers AL, Dong Y, Farwell WR, Kerr DA; EMPOWER Investigators.
Dexpramipexole versus placebo for patients with amyotrophic lateral
sclerosis (EMPOWER): a randomized, double-blind, phase 3 trial. Lancet
Neurology 2013;12(11):1059–1067.
Freitag F. Managing and treating tension-type headache. Med Clin North
Am 2013;97(2):281–292.
Freitag FG. Why do migraines often decrease as we age? Curr Pain
Headache Rep 2013;17(10):366.
Freitag FG, Lyss H, Nissan GR. Migraine disability, healthcare utilization,
and expenditures following treatment in a tertiary headache center. Proc
(Bayl Univ Med Cent) 2013;26(4):363–367.
Garrett JS, Zarghouni M, Layton KF, Graybeal D, Daoud YA. Validation
of clinical prediction scores in patients with primary intracerebral
hemorrhage. Neurocrit Care 2013;19(3):329–335.
Heitzman D, Sharma M, Pascual P, Phillips JT. Whole blood transcriptional profiling of sporadic amyotrophic lateral sclerosis patients identifies
a sub-population with an inflammatory component (P02-175). Neurology
2013;80:P02–175.
Hutchinson M, Fox RJ, Miller DH, Phillips JT, Kita M, Havrdova E,
O’Gorman J, Zhang R, Novas M, Viglietta V, Dawson KT. Clinical
efficacy of BG-12 (dimethyl fumarate) in patients with relapsingremitting multiple sclerosis: subgroup analyses of the CONFIRM study.
J Neurol 2013;260(9):2286–2296.
Khoury C. Chiari malformations. In UpToDate, last updated June 20,
2013.
Khoury C. Pathogenesis and types of occult spinal dysraphism. In
UpToDate, last updated October 31, 2013.
Kirk K, D’Aurelio M, Tadesse S, Hupf J, Hirano M, Mitsumoto H,
Manfriedi G, Study Group ALS COSMOS. Mitochondrial metabolic
markers in ALS fibroblasts. Amyotroph Lateral Scler Frontotemporal
Degener 2013;14(Suppl 2):26.
Mitsumoto H, Factor-Litvak P., Andrews H, Goetz RR, Andrews L,
Rabkin J, McElhiney M, Nieves J, Santella RM, Nagy PL, Murphy
J, Hupf J, Singleton J, Merle D, Kilty M, Heitzman D, Sedlack R,
Katz J, Forshew DA, Barohn RJ, McVey A, Dimachkie M, Sorenson
EJ, Oskarsson B, Fernandes Filho Jam, Kasarski E, Lomen-Hoerth C,
Mozaffar T, Rollins, YD, Nations SP, Swenson A J, Shefner JM, Andrews
JA, Koczon J, ALS COSMOS Study Group. ALS Multicenter Cohort
Study of Oxidative Stress (ALS COSMOS): the study of methodology, recruitment, and baseline demographics and disease characteristics.
Amyotroph Lateral Scler Frontotemporal Degener 2013;14(Suppl 2):24.
O’Connor JK, Bidiwala S. Effectiveness and safety of Gamma Knife
radiosurgery for glossopharyngeal neuralgia. Proc (Bayl Univ Med Cent)
2013;26(3):262–264.
Phillips JT, Fox RJ. BG-12 in multiple sclerosis. Semin Neurol
2013;33(1):56–65.
Rothrock JF, Freitag FG, Farr SJ, Smith EF 3rd. A review of needlefree sumatriptan injection for rapid control of migraine. Headache
2013;53(Suppl 2):21–33.
NURSING/ALLIED HEALTH
258. Cormier JE. Asthma exacerbations. Texas EMS Magazine July/August
2013, 34–39.
259. Gordon C, Schmelzer M. Care of the patient in excited delirium. J Emerg
Nurs 2013;39(2):190–196.
260. Gray LR, Shirey MR. Nurse manager engagement: what it means to nurse
managers and staff nurses. Nurs Adm Q 2013;37(4):337–345.
261. Hasse JM. Developing the “write” skills for publishing. Nutr Clin Pract
2013;28(2):153–157.
262. Hasse JM. Nutrition and liver disease: complex connections. Nutr Clin
Pract 2013;28(1):12–14.
263. Newland L, L’huillier MW, Petrey B. Implementation of cue-based
feeding in a level III NICU. Neonatal Netw 2013;32(2):132–137.
April 2014
264. Pilcher J. Learning preferences among neonatal and maternal child
nurses. Neonatal Netw 2013;32(2):117–119.
265. Pilcher J. NICU nurse educators: what evidence supports your teaching
strategies? Neonatal Netw 2013;32(4):281–284.
266. Pilcher J, Bradley DA. Best practices for learning with technology.
J Nurses Prof Dev 2013;29(3):133–137.
267. Pilcher J, Stone L, Reynolds R. Contact hours, skills fairs, and competency
assessment. Neonatal Netw 2013;32(5):359–364.
268. Roberts SR. Improving patient outcomes through registered dietitian
order writing. Nutr Clin Pract 2013;28(5):556–565.
269. Saracino G, Jennings LW, Hasse JM. Basic statistical concepts in nutrition
research. Nutr Clin Pract 2013;28(2):182–193.
270. Sturdivant C. A collaborative approach to defining neonatal therapy.
Newborn and Infant Nursing Reviews 2013;13(1):23–26.
271. Vaughn E, Hamann A, Koo C. Management of pulmonary vein
thrombosis following recent hemorrhagic stroke: a case report. Texas
Society of Health-System Pharmacists Journal 2013;14(2):15–18.
OBSTETRICS/GYNECOLOGY/FETAL MEDICINE
272. Nugent AW, Kowal RC, Juraszek AL, Ikemba C, Magee K. Model
of magnetically guided fetal cardiac intervention: potential to avoid
direct cardiac puncture. J Matern Fetal Neonatal Med 2013;26(18):
1778–1781.
ONCOLOGY/HEMATOLOGY/SURGICAL ONCOLOGY/BONE MARROW
TRANSPLANTATION
273. Armand P, Nagler A, Weller EA, Devine SM, Avigan DE, Chen YB,
Kaminski MS, Holland HK, Winter JN, Mason JR, Fay JW, Rizzieri
DA, Hosing CM, Ball ED, Uberti JP, Lazarus HM, Mapara MY, Gregory
SA, Timmerman JM, Andorsky D, Or R, Waller EK, Rotem-Yehudar
R, Gordon LI. Disabling immune tolerance by programmed death-1
blockade with pidilizumab after autologous hematopoietic stemcell transplantation for diffuse large B-cell lymphoma: results of an
international phase II trial. J Clin Oncol 2013;31(33):4199–4206.
274. Ashktorab H, Rahi H, Wansley D, Varma S, Shokrani B, Lee E,
Daremipouran M, Laiyemo A, Goel A, Carethers JM, Brim H. Toward a
comprehensive and systematic methylome signature in colorectal cancers.
Epigenetics 2013;8(8):807–815.
275. Bachanova V, Marks DI, Zhang MJ, Wang H, de Lima M, Aljurf MD,
Arellano M, Artz AS, Bacher U, Cahn JY, Chen YB, Copelan EA, Drobyski
WR, Gale RP, Greer JP, Gupta V, Hale GA, Kebriaei P, Lazarus HM, Lewis
ID, Lewis VA, Liesveld JL, Litzow MR, Loren AW, Miller AM, Norkin
M, Oran B, Pidala J, Rowe JM, Savani BN, Saber W, Vij R, Waller EK,
Wiernik PH, Weisdorf DJ. Ph+ ALL patients in first complete remission
have similar survival after reduced intensity and myeloablative allogeneic
transplantation: impact of tyrosine kinase inhibitor and minimal residual
disease. Leukemia 2013 Aug 30 [Epub ahead of print].
276. Barakat A, Barnes SA, Casanova MA, Stone MJ, Shuey KM, Miller AM.
Advance care planning knowledge and documentation in a hospitalized
cancer population. Proc (Bayl Univ Med Cent) 2013;26(4):368–372.
277. Becerra CR, Hanna N, McCollum AD, Becharm N, Timmerman RD,
DiMaio M, Kesler KA, Yu M, Yan T, Choy H. A phase II study with
cetuximab and radiation therapy for patients with surgically resectable
esophageal and GE junction carcinomas: Hoosier Oncology Group
G05-92. J Thorac Oncol 2013;8(11):1425–1429.
278. Boland CR, Jung B, Carethers JM. Cancer of the colon and gastrointestinal tract. In Rimoin DL, Pyeritz RE, Korf BR, eds. Emery and Rimoin’s
Principles and Practice of Medical Genetics, 6th ed. Boston: Elsevier/
Academic Press, 2013:1–31.
279. Boland CR, Lynch HT. The history of Lynch syndrome. Fam Cancer
2013;12(2):145–157.
280. Boland CR. The mystery of mismatch repair deficiency: Lynch or
Lynch-like? Gastroenterology 2013;144(5):868–870.
281. Boland CR. The stories behind the science: seminal CRC research was
a family affair. AGA Perspectives Oct/Nov 2013.
282. Boostrom SY, Dozois EJ. Recurrent pelvic surgery. Surg Clin North Am
2013;93(1):199–215.
2013 publications of the Baylor Health Care System medical and scientific staff
189
283. Boostrom SY, Mathis KL, Pendlimari R, Cima RR, Larson DW, Dozois
EJ. Risk of neoplastic change in ileal pouches in familial adenomatous
polyposis. J Gastrointest Surg 2013;17(10):1804–1808.
284. Boostrom SY, Nelson H. Current treatment of rectal cancer: the
watch and wait method. Are we there yet? Sem Colon Rectal Surg
2013;24(3):147–150.
285. Bredeson C, Lerademacher J, Kato K, Dipersio JF, Agura E, Devine
SM, Appelbaum FR, Tomblyn MR, Laport GG, Zhu X, McCarthy
PL, Ho VT, Cooke KR, Armstrong E, Smith A, Rizzo JD, Burkart JM,
Pasquini MC. Prospective cohort study comparing intravenous busulfan
to total body irradiation in hematopoietic cell transplantation. Blood
2013;122(24):3871–3878.
286. Burch M, Schneider R, Barakat A, Abushahin L, Cao Y, Ewing J, Stone
MJ. Results of an educational program to promote the use of pooled
instead of single-donor platelet transfusions. Proc (Bayl Univ Med Cent)
2013;26(1):3–5.
287. Cairncross G, Wang M, Shaw E, Jenkins R, Brachman D, Buckner J,
Fink K, Souhami L, Laperriere N, Curran W, Mehta M. Phase III trial of
chemoradiotherapy for anaplastic oligodendroglioma: long-term results
of RTOG 9402. J Clin Oncol 2013;31(3):337–343.
288. Chamogeorgakis T, Bhora F, Toumpoulis I, Nabong A, Connery C. Effect
of postoperative course on midterm outcome after esophageal resection
for cancer. Proc (Bayl Univ Med Cent) 2013;26(3):239–242.
289. Chen JL, Appelbaum DE, Kocherginsky M, Cowey CL, Kimryn
Rathmell W, McDermott DF, Stadler WM. FDG-PET as a predictive
biomarker for therapy with everolimus in metastatic renal cell cancer.
Cancer Med 2013;2(4):545–552.
290. Cheng YS, Jordan L, Rees T, Chen HS, Oxford L, Brinkmann O, Wong
D. Levels of potential oral cancer salivary mRNA biomarkers in oral
cancer patients in remission and oral lichen planus patients. Clin Oral
Investig 2013 Jul 28 [Epub ahead of print].
291. Choudhury S, Almendro V, Merino VF, Wu Z, Maruyama R, Su Y,
Martins FC, Fackler MJ, Bessarabova M, Kowalczyk A, Conway T,
Beresford-Smith B, Macintyre G, Cheng YK, Lopez-Bujanda Z, Kaspi
A, Hu R, Robens J, Nikolskaya T, Haakensen VD, Schnitt SJ, Argani P,
Ethington G, Panos L, Grant M, Clark J, Herlihy W, Lin SJ, Chew G,
Thompson EW, Greene-Colozzi A, Richardson AL, Rosson GD, Pike M,
Garber JE, Nikolsky Y, Blum JL, Au A, Hwang ES, Tamimi RM, Michor
F, Haviv I, Liu XS, Sukumar S, Polyak K. Molecular profiling of human
mammary gland links breast cancer risk to a p27+ cell population with
progenitor characteristics. Cell Stem Cell 2013;13(1):117–130.
292. Choueiri TK, Fay AP, Gagnon R, Lin Y, Bahamon B, Brown V, Rosenberg
JE, Hutson TE, Baker-Neblett KL, Carpenter C, Liu Y, Pandite L, Signoretti
S. The role of aberrant VHL/HIF pathway elements in predicting clinical
outcome to pazopanib therapy in patients with metastatic clear-cell renal cell
carcinoma. Clin Cancer Res 2013;19(18):5218–5226.
293. Cowey CL. Profile of tivozanib and its potential for the treatment of
advanced renal cell carcinoma. Drug Des Devel Ther 2013;7:519–527.
294. Cowey CL. Targeted therapy for advanced basal-cell carcinoma: vismodegib
and beyond. Dermatol Ther (Heidelb) 2013;3(1):17–31.
295. Coyle YM, Miller AM, Paulson RS. Model for the cost-efficient delivery of
continuous quality cancer care: a hospital and private-practice collaboration.
Proc (Bayl Univ Med Cent) 2013;26(2):95–99.
296. Craig DW, O’Shaughnessy JA, Kiefer JA, Aldrich J, Sinari S, Moses TM,
Wong S, Dinh J, Christoforides A, Blum JL, Aitelli CL, Osborne CR,
Izatt T, Kurdoglu A, Baker A, Koeman J, Barbacioru C, Sakarya O, De La
Vega FM, Siddiqui A, Hoang L, Billings PR, Salhia B, Tolcher AW, Trent
JM, Mousses S, Von Hoff D, Carpten JD. Genome and transcriptome
sequencing in prospective metastatic triple-negative breast cancer uncovers
therapeutic vulnerabilities. Mol Cancer Ther 2013;12(1):104–116.
297. Forero-Torres A, Infante JR, Waterhouse D, Wong L, Vickers S, Arrowsmith
E, He AR, Hart L, Trent D, Wade J, Jin X, Wang Q, Austin T, Rosen M,
Beckman R, von Roemeling R, Greenberg J, Saleh M. Phase 2, multicenter,
open-label study of tigatuzumab (CS-1008), a humanized monoclonal
antibody targeting death receptor 5, in combination with gemcitabine in
chemotherapy-naive patients with unresectable or metastatic pancreatic
cancer. Cancer Med 2013;2(6):925–932.
190
298. Galsky MD, Hahn NM, Powles T, Hellerstedt BA, Lerner SP, Gardner
TA, Yu M, O’Rourke M, Vogelzang NJ, Kocs D, McKenney SA, Melnyk
AM Jr, Hutson TE, Rauch M, Wang Y, Asmar L, Sonpavde G. Gemcitabine, Cisplatin, and sunitinib for metastatic urothelial carcinoma and as
preoperative therapy for muscle-invasive bladder cancer. Clin Genitourin
Cancer 2013;11(2):175–181.
299. Glück S, Russell C, O’Shaughnessy J, McKenna EF, Hu S, Odom D,
Blum JL. Treatment effect of capecitabine and docetaxel or docetaxel alone
by oestrogen receptor status in patients with metastatic breast cancer: results
of an exploratory analysis. Breast 2013;22(6):1087–1093.
300. Goss PE, Smith IE, O’Shaughnessy J, Ejlertsen B, Kaufmann M, Boyle
F, Buzdar AU, Fumoleau P, Gradishar W, Martin M, Moy B, PiccartGebhart M, Pritchard KI, Lindquist D, Chavarri-Guerra Y, Aktan G,
Rappold E, Williams LS, Finkelstein DM; on behalf of the TEACH
investigators. Adjuvant lapatinib for women with early-stage HER2positive breast cancer: a randomised, controlled, phase 3 trial. Lancet
Oncol 2013;14(1):88–96.
301. Graham RL, Cooper B, Krause JR. T-cell prolymphocytic leukemia. Proc
(Bayl Univ Med Cent) 2013;26(1):19–21.
302. Han TH, Chen R, Advani R, Berryman RB, Smith SE, Forero-Torres A,
Rosenblatt JD, Smith MR, Zain J, Hunder NN, Engert A. Brentuximab
vedotin does not cause clinically relevant QTc interval prolongation in
patients with CD30-positive hematologic malignancies. Cancer Chemother
Pharmacol 2013;72(1):241–249.
303. Harmon CS, Deprimo SE, Figlin RA, Hudes GR, Hutson TE, Michaelson
MD, Négrier S, Kim ST, Huang X, Williams JA, Eisen T, Motzer RJ.
Circulating proteins as potential biomarkers of sunitinib and interferon-α
efficacy in treatment-naïve patients with metastatic renal cell carcinoma.
Cancer Chemother Pharmacol 2013 Nov 13 [Epub ahead of print].
304. Heithaus RE Jr., Hitchcock MA, Guileyardo JM. Pulmonary tumor
embolism syndrome from occult colonic adenocarcinoma. Proc (Bayl
Univ Med Cent) 2013;26(3):290–292.
305. Heyninck K, Haegeman G, Goel A. Cancer chemoprevention by dietary
polyphenols: role for epigenetics and inflammation. In Preedy V, Zibadi
S, Watson R, eds. Polyphenols in Health and Disease. Waltham, MA:
Elsevier/Academic Press, 2013.
306. Holmes FA, Espina V, Liotta LA, Nagarwala YM, Danso M, McIntyre
KJ, Osborne CR, Anderson T, Krekow L, Blum JL, Pippen J, Florance
A, Mahoney J, O’Shaughnessy JA. Pathologic complete response after
preoperative anti-HER2 therapy correlates with alterations in PTEN,
FOXO, phosphorylated Stat5, and autophagy protein signaling. BMC
Res Notes 2013;6(1):507.
307. Hur K, Cejas P, Feliu J, Moreno-Rubio J, Burgos E, Boland CR, Goel A.
Hypomethylation of long interspersed nuclear element-1 (LINE-1) leads
to activation of proto-oncogenes in human colorectal cancer metastasis.
Gut 2013 May 23 [Epub ahead of print].
308. Hur K, Toiyama Y, Takahashi M, Balaguer F, Nagasaka T, Koike J,
Hemmi H, Koi M, Boland CR, Goel A. MicroRNA-200c modulates
epithelial-to-mesenchymal transition (EMT) in human colorectal cancer
metastasis. Gut 2013;62(9):1315–1326.
309. Hutson TE, Escudier B, Esteban E, Bjarnason GA, Lim HY, Pittman KB,
Senico P, Niethammer A, Lu DR, Hariharan S, Motzer RJ. Randomized
phase III trial of temsirolimus versus sorafenib as second-line therapy
after sunitinib in patients with metastatic renal cell carcinoma. J Clin
Oncol 2013 Dec 2 [Epub ahead of print].
310. Hutson TE, Lesovoy V, Al-Shukri S, Stus VP, Lipatov ON, Bair AH,
Rosbrook B, Chen C, Kim S, Vogelzang NJ. Axitinib versus sorafenib as firstline therapy in patients with metastatic renal-cell carcinoma: a randomised
open-label phase 3 trial. Lancet Oncol 2013;14(13):1287–1294.
311. Jones G, Arthurs B, Kaya H, Macdonald K, Qin R, Fairbanks RK,
Lamoreaux WT, Jawed I, Tward JD, Martincic D, Shivnani AT, Lee
CM. Overall survival analysis of adjuvant radiation versus observation in
stage I testicular seminoma: a surveillance, epidemiology, and end results
(SEER) analysis. Am J Clin Oncol 2013;36(5):500–504.
312. Jones SE, Collea R, Paul D, Sedlacek S, Favret AM, Gore I Jr, Lindquist DL,
Holmes FA, Allison MA, Brooks BD, Portillo RM, Vukelja SJ, Steinberg
MS, Stokoe C, Crockett MW, Wang Y, Asmar L, Robert NJ, O’Shaughnessy
Baylor University Medical Center Proceedings
Volume 27, Number 2
313.
314.
315.
316.
317.
318.
319.
320.
321.
322.
323.
324.
325.
326.
327.
328.
J. Adjuvant docetaxel and cyclophosphamide plus trastuzumab in patients
with HER2-amplified early stage breast cancer: a single-group, open-label,
phase 2 study. Lancet Oncol 2013;14(11):1121–1128.
Komarova NL, Boland CR. Cancer: calculated treatment. Nature
2013;499(7458):291–292.
Krause JR, Drinkard LC, Keglovits LC. Hodgkin lymphoma transformation of chronic lymphocytic leukemia/small lymphocytic lymphoma.
Proc (Bayl Univ Med Cent) 2013;26(1):16–18.
Krause JR. Signet ring lymphoma: a potential diagnostic mishap. Proc
(Bayl Univ Med Cent) 2013;26(3):293–294.
Kroeker TR, O’Brien JC. Outcomes of combined oncologic resection
and carotid endarterectomy in patients with head and neck cancer.
Head Neck 2013;35(5):E167–E170.
Kwak EL, Shapiro GI, Cohen SM, Becerra CR, Lenz HJ, Cheng WF,
Su WC, Robohn M, Le Maulf F, Lobmeyer MT, Chand VK, Iafrate AJ.
Phase 2 trial of afatinib, an ErbB family blocker, in solid tumors genetically screened for target activation. Cancer 2013;119(16):3043–3051.
Landry CS, Lin HY, Phan A, Charnsangavej C, Abdalla EK, Aloia
T, Nicolas Vauthey J, Katz MH, Yao JC, Fleming JB. Resection of
at-risk mesenteric lymph nodes is associated with improved survival
in patients with small bowel neuroendocrine tumors. World J Surg
2013;37(7):1695–1700.
Larkin J, Fishman M, Wood L, Negrier S, Olivier K, Pyle L, Gorbunova V,
Jonasch E, Andrews L, Staehler M. Axitinib for the treatment of metastatic
renal cell carcinoma: recommendations for therapy management to optimize
outcomes. Am J Clin Oncol. 2013 Jan 24 [Epub ahead of print].
Lee SJ, Storer B, Wang H, Lazarus HM, Waller EK, Isola LM, Klumpp
TR, Umejiego JB, Savani BN, Loren AW, Cairo MS, Camitta BM,
Cutler CS, George B, Jean Khoury H, Marks DI, Rizzieri DA, Copelan
EA, Gupta V, Liesveld JL, Litzow MR, Miller AM, Schouten HC, Gale
RP, Cahn JY, Weisdorf DJ. Providing personalized prognostic information for adult leukemia survivors. Biol Blood Marrow Transplant
2013;19(11):1600–1607.
Lin PJ, Concannon TW, Greenberg D, Cohen JT, Rossi G, Hille J,
Auerbach HR, Fang CH, Nadler ES, Neumann PJ. Does framing of cancer
survival affect perceived value of care? A willingness-to-pay survey of US
residents. Expert Rev Pharmacoecon Outcomes Res 2013;13(4):513–522.
Link A, Balaguer F, Shen Y, Lozano JJ, Leung HC, Boland CR, Goel A.
Curcumin modulates DNA methylation in colorectal cancer cells. PLoS
One 2013;8(2):e57709.
Lu KH, Skates S, Hernandez MA, Bedi D, Bevers T, Leeds L, Moore R,
Granai C, Harris S, Newland W, Adeyinka O, Geffen J, Deavers MT,
Sun CC, Horick N, Fritsche H, Bast RC Jr. A 2-stage ovarian cancer
screening strategy using the Risk of Ovarian Cancer Algorithm (ROCA)
identifies early-stage incident cancers and demonstrates high positive
predictive value. Cancer 2013;119(19):3454–3461.
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM, Brundage TM, Robertson AT, Godkin S, Momméja-Marin H,
Boeckh M; CMX001-201 Clinical Study Group. CMX001 to prevent
cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J
Med 2013;369(13):1227–1236.
Mathis KL, Boostrom SY, Pemberton JH. New developments in colorectal surgery. Curr Opin Gastroenterol 2013;29(1):72–78.
Miles DW, Diéras V, Cortés J, Duenne AA, Yi J, O’Shaughnessy J.
First-line bevacizumab in combination with chemotherapy for HER2negative metastatic breast cancer: pooled and subgroup analyses of data
from 2447 patients. Ann Oncol 2013;24(11):2773–2780.
Modi S, Saura C, Henderson C, Lin NU, Mahtani R, Goddard J,
Rodenas E, Hudis C, O’Shaughnessy J, Baselga J. A multicenter trial
evaluating retaspimycin HCL (IPI-504) plus trastuzumab in patients
with advanced or metastatic HER2-positive breast cancer. Breast Cancer
Res Treat 2013;139(1):107–113.
Molina AM, Hutson TE, Larkin J, Gold AM, Wood K, Carter D, Motzer
R, Michaelson MD. A phase 1b clinical trial of the multi-targeted tyrosine
kinase inhibitor lenvatinib (E7080) in combination with everolimus for
treatment of metastatic renal cell carcinoma (RCC). Cancer Chemother
Pharmacol 2013 Nov 5 [Epub ahead of print].
April 2014
329. Motzer RJ, Escudier B, Bukowski R, Rini BI, Hutson TE, Barrios CH,
Lin X, Fly K, Matczak E, Gore ME. Prognostic factors for survival in
1059 patients treated with sunitinib for metastatic renal cell carcinoma.
Br J Cancer 2013;108(12):2470–2477.
330. Motzer RJ, Escudier B, Tomczak P, Hutson TE, Michaelson MD, Negrier
S, Oudard S, Gore ME, Tarazi J, Hariharan S, Chen C, Rosbrook B, Kim
S, Rini BI. Axitinib versus sorafenib as second-line treatment for advanced
renal cell carcinoma: overall survival analysis and updated results from a
randomised phase 3 trial. Lancet Oncol 2013;14(6):552–562.
331. Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, Nathan
P, Staehler M, de Souza P, Merchan JR, Boleti E, Fife K, Jin J, Jones R,
Uemura H, De Giorgi U, Harmenberg U, Wang J, Sternberg CN, Deen
K, McCann L, Hackshaw MD, Crescenzo R, Pandite LN, Choueiri TK.
Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J
Med 2013;369(8):722–731.
332. Motzer RJ, Nosov D, Eisen T, Bondarenko I, Lesovoy V, Lipatov O,
Tomczak P, Lyulko O, Alyasova A, Harza M, Kogan M, Alekseev BY,
Sternberg CN, Szczylik C, Cella D, Ivanescu C, Krivoshik A, Strahs A,
Esteves B, Berkenblit A, Hutson TE. Tivozanib versus sorafenib as initial
targeted therapy for patients with metastatic renal cell carcinoma: results
from a phase III trial. J Clin Oncol 2013;31(30):3791–3799.
333. Nishida N, Kudo M, Nishimura T, Arizumi T, Takita M, Kitai S, Yada
N, Hagiwara S, Inoue T, Minami Y, Ueshima K, Sakurai T, Yokomichi
N, Nagasaka T, Goel A. Unique association between global DNA
hypomethylation and chromosomal alterations in human hepatocellular
carcinoma. PLoS One 2013;8(9):e72312.
334. O’Shaughnessy J, Gradishar WJ, Bhar P, Iglesias J. Nab-paclitaxel for
first-line treatment of patients with metastatic breast cancer and poor
prognostic factors: a retrospective analysis. Breast Cancer Res Treat
2013;138(3):829–837.
335. Owen RG, Kyle RA, Stone MJ, Rawstron AC, Leblond V, Merlini G,
Garcia-Sanz R, Ocio EM, Morra E, Morel P, Anderson KC, Patterson CJ,
Munshi NC, Tedeschi A, Joshua DE, Kastritis E, Terpos E, Ghobrial IM,
Leleu X, Gertz MA, Ansell SM, Morice WG, Kimby E, Treon SP. Response
assessment in Waldenström macroglobulinaemia: update from the VIth
International Workshop. Br J Haematol 2013;160(2):171–176.
336. Pan IW, Mallick R, Dhanda R, Nadler E. Treatment patterns and outcomes in patients with non-squamous advanced non-small cell lung
cancer receiving second-line treatment in a community-based oncology
network. Lung Cancer 2013;82(3):469–476.
337. Papavasiliou P, Chun YS, Hoffman JP. How to define and manage borderline
resectable pancreatic cancer. Surg Clin North Am 2013;93(3):663–674.
338. Pearson EJ, Mennel R. Eosinophilic small bowel enteritis in response to
folinic acid, fluorouracil, and oxaliplatin chemotherapy. Proc (Bayl Univ
Med Cent) 2013;26(3):288–289.
339. Piazzi G, Selgrad M, Garcia M, Ceccarelli C, Fini L, Bianchi P, Laghi
L, D’Angelo L, Paterini P, Malfertheiner P, Chieco P, Boland CR,
Bazzoli F, Ricciardiello L. Van-Gogh-like 2 antagonises the canonical
WNT pathway and is methylated in colorectal cancers. Br J Cancer
2013;108(8):1750–1756.
340. Procopio G, Bellmunt J, Dutcher J, Bracarda S, Knox J, Brueckner
A, Molnar I, Escudier B, Hutson TE. Sorafenib tolerability in elderly
patients with advanced renal cell carcinoma: results from a large pooled
analysis. Br J Cancer 2013;108(2):311–318.
341. Rhees J, Arnold M, Boland CR. Inversion of exons 1-7 of the MSH2
gene is a frequent cause of unexplained Lynch syndrome in one local
population. Fam Cancer 2013 Oct 11 [Epub ahead of print].
342. Ribas A, Zhang W, Chang I, Shirai K, Ernstoff MS, Daud A, Cowey
CL, Daniels G, Seja E, O’Laco E, Glaspy JA, Chmielowski B, Hill T, Joe
AK, Grippo JF. The effects of a high-fat meal on single-dose vemurafenib
pharmacokinetics. J Clin Pharmacol 2013 Dec 28 [Epub ahead of print].
343. Richey SL, Hutson TE. Angiopoietins and non-vascular endothelial
growth factor antiangiogenic targets in advanced renal cell carcinoma.
Cancer J 2013;19(4):307–310.
344. Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P,
Fizazi K, Mainwaring P, Piulats JM, Ng S, Carles J, Mulders PF, Basch E,
Small EJ, Saad F, Schrijvers D, Van Poppel H, Mukherjee SD, Suttmann
2013 publications of the Baylor Health Care System medical and scientific staff
191
345.
346.
347.
348.
349.
350.
351.
352.
353.
354.
355.
356.
357.
358.
192
H, Gerritsen WR, Flaig TW, George DJ, Yu EY, Efstathiou E, Pantuck A,
Winquist E, Higano CS, Taplin ME, Park Y, Kheoh T, Griffin T, Scher
HI, Rathkopf DE; COU-AA-302 Investigators (Hutson T). Abiraterone
in metastatic prostate cancer without previous chemotherapy. N Engl J
Med 2013;368(2):138–148.
Sadamori H, Yagi T, Shigeyasu K, Umeda Y, Sugihara M, Yokomichi N,
Ohara T, Nishida N, Nagasaka T, Goel A, Fujiwara T. Advanced hepatocellular carcinoma with lymph node metastases showing epithelial to
mesenchymal transition effectively treated with systemic chemotherapy:
report of a case. Hepatol Res 2013;43(12):1368–1373.
Sanmukhani J, Satodia V, Trivedi J, Patel T, Tiwari D, Panchal B, Goel A,
Tripathi CB. Efficacy and safety of curcumin in major depressive disorder: a
randomized controlled trial. Phytother Res 2013 Jul 6 [Epub ahead of print].
Semple J, Metcalfe KA, Lynch HT, Kim-Sing C, Senter L, Pal T, Ainsworth
P, Lubinski J, Tung N, Eng C, Gilchrist D, Blum J, Neuhausen SL, Singer
CF, Ghadirian P, Sun P, Narod SA; The Hereditary Breast Cancer Clinical
Study Group. International rates of breast reconstruction after prophylactic
mastectomy in BRCA1 and BRCA2 mutation carriers. Ann Surg Oncol
2013;20(12):3817–3822.
Shakibaei M, Mobasheri A, Lueders C, Busch F, Shayan P, Goel A.
Curcumin enhances the effect of chemotherapy against colorectal cancer
cells by inhibition of NF-κB and Src protein kinase signaling pathways.
PLoS One 2013;8(2):e57218.
Shaughnessy P, Uberti J, Devine S, Maziarz RT, Vose J, Micallef I,
Jacobsen E, McCarty J, Stiff P, Artz A, Ball ED, Berryman R, Dugan
M, Joyce R, Hsu FJ, Johns D, McSweeney P. Plerixafor and G-CSF for
autologous stem cell mobilization in patients with NHL, Hodgkin’s
lymphoma and multiple myeloma: results from the expanded access
program. Bone Marrow Transplant 2013;48(6):777–781.
Shia J, Zhang L, Shike M, Guo M, Stadler Z, Xiong X, Tang LH, Vakiani
E, Katabi N, Wang H, Bacares R, Ruggeri J, Boland CR, Ladanyi M,
Klimstra DS. Secondary mutation in a coding mononucleotide tract in
MSH6 causes loss of immunoexpression of MSH6 in colorectal carcinomas
with MLH1/PMS2 deficiency. Mod Pathol 2013;26(1):131–138.
Shigeyasu K, Tanakaya K, Nagasaka T, Aoki H, Fujiwara T, Sugano K,
Ishikawa H, Yoshida T, Moriya Y, Furukawa Y, Goel A, Takeuchi H. Early
detection of metachronous bile duct cancer in Lynch syndrome: report
of a case. Surg Today 2013 Jul 31 [Epub ahead of print].
Smith JW 2nd, Vukelja S, Rabe A, Wentworth-Hartung N, Koutrelakos N,
Shao SH, Whittaker T, Wang Y, Asmar L, McDowell DO, Mukhopadhyay
P, O’Shaughnessy J. Phase II randomized trial of weekly and every-3-week
ixabepilone in metastatic breast cancer patients. Breast Cancer Res Treat
2013;142(2):381–388.
Stone MJ, Bogen SA. Role of plasmapheresis in Waldenström’s macroglobulinemia. Clin Lymphoma Myeloma Leuk 2013;13(2):238–240.
Storb R, Gyurkocza B, Storer BE, Sorror ML, Blume K, Niederwieser D,
Chauncey TR, Pulsipher MA, Petersen FB, Sahebi F, Agura ED, Hari P,
Bruno B, McSweeney PA, Maris MB, Maziarz RT, Langston AA, Bethge
W, Vindeløv L, Franke GN, Laport GG, Yeager AM, Hübel K, Deeg
HJ, Georges GE, Flowers ME, Martin PJ, Mielcarek M, Woolfrey AE,
Maloney DG, Sandmaier BM. Graft-versus-host disease and graft-versustumor effects after allogeneic hematopoietic cell transplantation. J Clin
Oncol 2013;31(12):1530–1538.
Toiyama Y, Hur K, Tanaka K, Inoue Y, Kusunoki M, Boland CR, Goel
A. Serum miR-200c is a novel prognostic and metastasis-predictive
biomarker in patients with colorectal cancer. Ann Surg 2013 Aug 26
[Epub ahead of print].
Toiyama Y, Takahashi M, Hur K, Nagasaka T, Tanaka K, Inoue Y, Kusunoki M,
Boland CR, Goel A. Serum miR-21 as a diagnostic and prognostic biomarker
in colorectal cancer. J Natl Cancer Inst 2013;105(12):849–859.
Toiyama Y, Yasuda H, Saigusa S, Tanaka K, Inoue Y, Goel A, Kusunoki
M. Increased expression of Slug and Vimentin as novel predictive biomarkers for lymph node metastasis and poor prognosis in colorectal
cancer. Carcinogenesis 2013;34(11):2548–2557.
Trunzer K, Pavlick AC, Schuchter L, Gonzalez R, McArthur GA, Hutson
TE, Moschos SJ, Flaherty KT, Kim KB, Weber JS, Hersey P, Long GV,
Lawrence D, Ott PA, Amaravadi RK, Lewis KD, Puzanov I, Lo RS,
359.
360.
361.
362.
363.
Koehler A, Kockx M, Spleiss O, Schell-Steven A, Gilbert HN, Cockey
L, Bollag G, Lee RJ, Joe AK, Sosman JA, Ribas A. Pharmacodynamic
effects and mechanisms of resistance to vemurafenib in patients with
metastatic melanoma. J Clin Oncol 2013;31(14):1767–1774.
Van Vrancken M, Mir M, Herlihy W. Basal cell adenoma of the breast.
Proc (Bayl Univ Med Cent) 2013;26(4):396–397.
Van Vrancken MJ, Keglovits L, Krause J. Plasmablastic lymphoma following
transplantation. Proc (Bayl Univ Med Cent) 2013;26(2):152–155.
Vogelzang NJ, Bhor M, Liu Z, Dhanda R, Hutson TE. Everolimus vs.
temsirolimus for advanced renal cell carcinoma: use and use of resources in
the US Oncology Network. Clin Genitourin Cancer 2013;11(2):115–120.
Warlick SD, Paulson K, Brazauskas R, Zhong X, Miller AM, Camitta
BM, George B, Savani BN, Ustun C, Marks DI, Waller EK, Baron F,
Freytes CO, Socie G, Akpek G, Schouten HC, Lazarus HM, Horwitz
EM, Koreth J, Cahn JY, Bornhauser M, Seftel M, Cairo MS, Laughlin
MJ, Sabloff M, Ringdén O, Gale RP, Kamble RT, Vij R, Gergis U,
Mathews V, Saber W, Chen YB, Liesveld JL, Cutler CS, Ghobadi A, Uy
GL, Eapen M, Weisdorf DJ, Litzow MR. Effect of post remission therapy
prior to reduced intensity conditioning allogeneic transplantation for
acute myeloid leukemia in first complete remission. Biol Blood Marrow
Transplant 2013 Oct 31 [Epub ahead of print].
Wodarz D, Boland CR, Goel A, Komarova NL. Methylation kinetics
and CpG-island methylator phenotype status in colorectal cancer cell
lines. Biol Direct 2013;8:14.
ORAL AND MAXILLOFACIAL SURGERY
364. Gonçalves JR, Gomes LC, Vianna AP, Rodrigues DB, Gonçalves DA,
Wolford LM. Airway space changes after maxillomandibular counterclockwise rotation and mandibular advancement with TMJ Concepts®
total joint prostheses: three-dimensional assessment. Int J Oral Maxillofac
Surg 2013;42(8):1014–1022.
365. Goncalves JR, Wolford LM, Cassano DS, da Porciuncula G, Paniagua
B, Cevidanes LH. Temporomandibular joint condylar changes following
maxillomandibular advancement and articular disc repositioning. J Oral
Maxillofac Surg 2013;71(10):1759.e1–e15.
366. Movahed R, Morales-Ryan C, Allen WR, Warren S, Wolford LM. Outcome
assessment of 603 cases of concomitant inferior turbinectomy and Le Fort I
osteotomy. Proc (Bayl Univ Med Cent) 2013;26(4):376–381.
367. Movahed R, Pinto LP, Morales-Ryan C, Allen WR, Wolford LM.
Application of cranial bone grafts for reconstruction of maxillofacial
deformities. Proc (Bayl Univ Med Cent) 2013;26(3):252–255.
368. Movahed R, Teschke M, Wolford LM. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery utilizing computer-assisted surgical simulation. J Oral
Maxillofac Surg 2013;71(12):2123–2129.
369. Wolford LM, Movahed R, Perez DE. A classification system for conditions causing condylar hyperplasia. J Oral Maxillofac Surg 2013 Dec 31
[Epub ahead of print].
370. Wolford LW, Rodrigues DB. Nerve grafts and conduits. In Miloro M, ed.
Trigeminal Nerve Injuries. Berlin: Springer-Verlag, 2013:271–290.
ORTHOPAEDIC SURGERY
371. Barber FA, Dockery WD, Cowden CH 3rd. The degradation outcome of
biocomposite suture anchors made from poly L-lactide-co-glycolide and
β-tricalcium phosphate. Arthroscopy 2013;29(11):1834–1839.
372. Brodsky JW, Coleman SC, Smith S, Polo FE, Tenenbaum S. Hindfoot
motion following STAR total ankle arthroplasty: a multisegment foot
model gait study. Foot Ankle Int 2013;34(11):1479–1485.
373. Brodsky JW, Jung KS, Tenenbaum S. Primary synovial chondromatosis of the subtalar joint presenting as ankle instability. Foot Ankle Int
2013;34(10):1447–1450.
374. Burkhead WZ Jr, Moen TC, Rudolph GH. General surgical principles
of open rotator cuff repair in the management of failed arthroscopic cuff
repairs. Instr Course Lect 2013;62:105–114.
375. Chao JC, Charlick D, Tocci S, Brodsky JW. Radiographic and clinical
outcomes of joint-preserving procedures for hallux valgus in rheumatoid
arthritis. Foot Ankle Int 2013;34(12):1638–1644.
Baylor University Medical Center Proceedings
Volume 27, Number 2
376. Choi JH, Coleman SC, Tenenbaum S, Polo FE, Brodsky JW. Prospective
study of the effect on gait of a two-component total ankle replacement.
Foot Ankle Int 2013;34(11):1472–1478.
377. Choi JH, Zide JR, Coleman SC, Brodsky JW. Prospective study of the
treatment of adult primary hallux valgus with scarf osteotomy and soft
tissue realignment. Foot Ankle Int 2013;34(5):684–690.
378. Cooper DE, Fouts B. Single-portal arthroscopy: report of a new technique.
Arthrosc Tech 2013;2(3):e265–e269.
379. Flavin R, Coleman SC, Tenenbaum S, Brodsky JW. Comparison of
gait after total ankle arthroplasty and ankle arthrodesis. Foot Ankle Int
2013;34(10):1340–1348.
380. Grear BJ, Rabinovich A, Brodsky JW. Charcot arthropathy of the
foot and ankle associated with rheumatoid arthritis. Foot Ankle Int
2013;34(11):1541–1547.
381. Hung M, Baumhauer JF, Latt LD, Saltzman CL, SooHoo NF, Hunt
KJ; National Orthopaedic Foot & Ankle Outcomes Research Network.
Validation of PROMIS® Physical Function computerized adaptive tests
for orthopaedic foot and ankle outcome research. Clin Orthop Relat Res
2013;471(11):3466–3474.
382. Jockel JR, Brodsky JW. Single-stage flexor tendon transfer for the treatment of severe concomitant peroneus longus and brevis tendon tears.
Foot Ankle Int 2013;34(5):666–672.
383. Martin HD, Palmer IJ. History and physical examination of the hip: the
basics. Curr Rev Musculoskelet Med 2013;6(3):219–225.
384. Park AE. Anterior lumbar interbody fusion. In Flatow E, Chiang Colvin
A, eds. Atlas of Essential Orthopaedic Procedures. Rosemont, IL: American
Academy of Orthopaedic Surgeons, 2013.
OTOLARYNGOLOGY
385. Brown RF, Ducic Y. Aggressive surgical resection of anaplastic thyroid
carcinoma may provide long-term survival in selected patients. Otolaryngol
Head Neck Surg 2013;148(4):564–571.
386. Ducic Y, Defatta R, Wolfswinkel EM, Weathers WM, Hollier LH Jr. Tunneling
technique for expedited fibula free tissue harvest. Craniomaxillofac Trauma
Reconstr 2013;6(4):233–236.
387. Lee T, Sawhney R, Ducic Y. Miniplate fixation of fractures of the
symphyseal and parasymphyseal regions of the mandible: a review of
218 patients. JAMA Facial Plast Surg 2013;15(2):121–125.
388. Rihani J, Lee MR, Lee T, Ducic Y. Flap selection and functional outcomes
in total glossectomy with laryngeal preservation. Otolaryngol Head Neck
Surg 2013;149(4):547–553.
389. Rihani J, Lee T, Ducic Y. Secondary onlay free flap reconstruction of glossectomy defects following initial successful flap restoration. Otolaryngol Head
Neck Surg 2013;149(2):232–234.
390. Sawhney R, Brown R, Ducic Y. Condylar fractures. Otolaryngol Clin
North Am 2013;46(5):779–790.
391. Sawhney R, Ducic Y. Management of pathologic fractures of the
mandible secondary to osteoradionecrosis. Otolaryngol Head Neck
Surg 2013;148(1):54–58.
PATHOLOGY
Note: See also Oncology and other departments in which pathologists were first
authors or coauthors.
392. Hinson SA, Silva EG, Pinto K. Ovarian serous cystadenofibromas
associated with a low-grade serous carcinoma of the peritoneum. Ann
Diagn Pathol 2013;17(3):302–304.
393. Van Vrancken MJ, Benavides R, Wians FH Jr. Identification of designer
drug 2C-E (4-ethyl-2, 5-dimethoxy-phenethylamine) in urine following
a drug overdose. Proc (Bayl Univ Med Cent) 2013;26(1):58–61.
PULMONOLOGY/INTENSIVE CARE/SLEEP MEDICINE
394. Adesina A, Mason C, Mora A. Pneumatosis intestinalis with fatal air
emboli in a scleroderma patient. Chest 2013;144(4):340A.
395. Afzal A, Kim E, Mora A. When a monster throws a fit. Chest
2013;144(4):966A.
396. Henry D, Rosenthal L, Dedrick D, Taylor D. Understanding patient
responses to insomnia. Behav Sleep Med 2013;11(1):40–55.
April 2014
397. Henry D, Rosenthal L. “Listening for his breath”: the significance of gender
and partner reporting on the diagnosis, management, and treatment of
obstructive sleep apnea. Soc Sci Med 2013;79:48–56.
398. Mora A, Tsai-Nguyen G, Columbus C. 2012 West Nile virus outbreak—who
were the critically ill patients? Chest 2013;144(4):381A.
399. Mora M, Smialek B, Swink A, Ganesh A, Ferguson B, Belknap C,
Al-Ameri Y, Turoff A. Achieving targeted tidal volumes through lean
process improvement. Chest 2013;144(4):522A.
400. Whiteley A, Podduturi V, Guileyardo J, Mora A. Occult lymphoma
compounds lactic acidosis. Chest 2013;144(4):346A.
RADIOLOGY
Note: See also Oncology and other departments in which radiologists were first
authors or coauthors.
401. Dobbs NB, Latifi HR. Diffuse FDG uptake due to fat necrosis following
transverse rectus abdominus myocutaneous (TRAM) flap reconstruction.
Clin Nucl Med 2013;38(8):652–654.
402. Glass SB, Shah ZA. Clinical utility of positron emission mammography.
Proc (Bayl Univ Med Cent) 2013;26(3):314–319.
403. Ha KY, DeLeon P, DeLeon W. Invasive mucinous carcinoma of the
breast. Proc (Bayl Univ Med Cent) 2013;26(3):295–297.
404. Ha KY, DeLeon P, Hamilton R. Breast fibromatosis mimicking breast
carcinoma. Proc (Bayl Univ Med Cent) 2013;26(1):22–24.
405. Ha KY, Glass SB, Laurie L. Inflammatory breast cancer. Proc (Bayl Univ
Med Cent) 2013;26(2):149–151.
406. Ha KY, Parish D, Hamilton R, Wang JC. Fat necrosis in the breast
from methylene blue dye injection. Proc (Bayl Univ Med Cent) 2013;
26(3):298–299.
407. Ha KY, Wang JC, Gill JI. Lymphoma in the breast. Proc (Bayl Univ Med
Cent) 2013;26(2):146–148.
408. Heithaus RE, Hogan R. Images in clinical medicine. Unblinded by the
lights. N Engl J Med 2013;369(7):659.
409. Kershen LM, Marichal DA. Endovascular treatment of stent fracture and
pseudoaneurysm formation in arteriovenous fistula dialysis access. Proc
(Bayl Univ Med Cent) 2013;26(1):47–49.
410. Levine HR, Tingle E, Carter B, Dockery D. Synovial metastasis from
lung cancer. Proc (Bayl Univ Med Cent) 2013;26(1):25–27.
411. Lindsey SS, Kallmes DF, Opatowsky MJ, Broyles EA, Layton KF. Impact
of sham-controlled vertebroplasty trials on referral patterns at two academic
medical centers. Proc (Bayl Univ Med Cent) 2013;26(2):103–105.
412. McDonald JS, Carter RE, Layton KF, Mocco J, Madigan JB, Tawk
RG, Hanel RA, Roy SS, Cloft HJ, Klunder AM, Suh SH, Kallmes
DF. Interobserver variability in retreatment decisions of recurrent and
residual aneurysms. AJNR Am J Neuroradiol 2013;34(5):1035–1039.
413. Nickell LT, Schucany WG, Opatowsky MJ. Kummell disease. Proc (Bayl
Univ Med Cent) 2013;26(3):300–301.
414. Ray MJ, Mohammad F, Taylor WB, Cura M, Savage C. Comparison of fluoroscopic operator eye exposures when working from femoral region, side,
or head of patient. Proc (Bayl Univ Med Cent) 2013;26(3):243–246.
415. Saad AF, Bidiwala SB, Layton KF, Snipes GJ, Opatowsky MJ. Fourth
ventricular subependymoma presenting as worsening headache. Proc
(Bayl Univ Med Cent) 2013;26(1):52–54.
416. Saad AF, Ford KL III, dePrisco G, Smerud MJ. Adrenomegaly and
septic adrenal hemorrhage (Waterhouse-Friderichsen syndrome) in the
setting of congenital adrenal hyperplasia. Proc (Bayl Univ Med Cent)
2013;26(3):268–269.
417. Yactor AR, Michell MN, Koch MS, Leete TG, Shah ZA, Carter BW.
Percutaneous tattoo pigment simulating calcific deposits in axillary lymph
nodes. Proc (Bayl Univ Med Cent) 2013;26(1):28–29.
418. Yactor AR, Zarghouni M, Spigel JJ. Unusual dermal pleomorphic calcific
deposits in a case of inflammatory breast carcinoma. Proc (Bayl Univ Med
Cent) 2013;26(4):393–394.
419. Zarghouni M, Kershen ML, Skaggs L, Bhatki A, Gilbert SC, Gomez
CE, Opatowsky MJ. Endolymphatic sac tumor and otalgia. Proc (Bayl
Univ Med Cent) 2013;26(2):159–160.
420. Zarghouni M, Marichal D. Persistent bilateral proatlantal type II artery.
Proc (Bayl Univ Med Cent) 2013;26(1):50–51.
2013 publications of the Baylor Health Care System medical and scientific staff
193
RHEUMATOLOGY
421. Becker AM, Dao KH, Han BK, Kornu R, Lakhanpal S, Mobley AB,
Li QZ, Lian Y, Wu T, Reimold AM, Olsen NJ, Karp DR, Chowdhury
FZ, Farrar JD, Satterthwaite AB, Mohan C, Lipsky PE, Wakeland
EK, Davis LS. SLE peripheral blood B cell, T cell and myeloid cell
transcriptomes display unique profiles and each subset contributes to
the interferon signature. PLoS One 2013;8(6):e67003.
422. Bykerk VP, Cush J, Winthrop K, Calabrese L, Lortholary O, de Longueville
M, van Vollenhoven R, Mariette X. Update on the safety profile of certolizumab pegol in rheumatoid arthritis: an integrated analysis from clinical
trials. Ann Rheum Dis 2013 Oct 3 [Epub ahead of print].
423. Cush JJ. Autoinflammatory syndromes. Dermatol Clin 2013;31(3):
471–480.
424. Cush JJ. Infection update. Drug Safety Quarterly 2013;4(2):1–3.
425. Cush JJ. TNF inhibitors and severe hepatic injury. Drug Safety Quarterly
2013;4(3):3.
426. Cush JJ, Dao KH, Orozco C. TNF inhibitors and heart failure. Drug
Safety Quarterly 2013;4(1):1–2.
427. Cush JJ, Weinblatt ME, Kavanaugh A, eds. Rheumatoid Arthritis, 4th
ed. New York: Professional Communications, 2013.
428. Furst DE, Mandell B, Calabrese LH, Cather JC, Clauw DJ, Deodhar
A, Kremer JM, Lewiecki EM, McMahon M, T Ritchlin C. Proceedings
of the 5th annual Perspectives in Rheumatic Diseases. Semin Arthritis
Rheum 2013;43(3):416–419.
429. Guiducci C, Gong M, Cepika AM, Xu Z, Tripodo C, Bennett L,
Crain C, Quartier P, Cush JJ, Pascual V, Coffman RL, Barrat FJ. RNA
recognition by human TLR8 can lead to autoimmune inflammation.
J Exp Med 2013;210(13):2903–2919.
430. Hsia EC, Cush JJ, Matteson EL, Beutler A, Doyle MK, Hsu B, Xu S,
Rahman MU. Comprehensive tuberculosis screening program in patients
with inflammatory arthritides treated with golimumab, a human antitumor necrosis factor antibody, in phase III clinical trials. Arthritis Care
Res (Hoboken) 2013;65(2):309–313.
431. Kavanaugh A, Fleischmann R, Bergman MJ, Ruderman E, Troum O, Wells
AF, Martin G, Calabrese LH, Gibofsky A, Strand V, Cush JJ. Proceedings
of the 2013 Rheumatology Winter Clinical Symposia. Semin Arthritis
Rheum 2013;42(6):667–673.
432. van der Heijde D, Tanaka Y, Fleischmann R, Keystone E, Kremer J, Zerbini
C, Cardiel MH, Cohen S, Nash P, Song YW, Tegzová D, Wyman BT,
Gruben D, Benda B, Wallenstein G, Krishnaswami S, Zwillich SH, Bradley
JD, Connell CA; ORAL Scan Investigators. Tofacitinib (CP-690,550) in
patients with rheumatoid arthritis receiving methotrexate: twelve-month
data from a twenty-four-month phase III randomized radiographic study.
Arthritis Rheum 2013;65(3):559–570.
433. Weinblatt ME, Kremer J, Cush J, Rigby W, Teng LL, Devenport J,
Singh N, Lepley D, Genovese MC. Tocilizumab as monotherapy or in
combination with nonbiologic disease-modifying antirheumatic drugs:
twenty-four-week results of an open-label, clinical practice study. Arthritis
Care Res (Hoboken) 2013;65(3):362–371.
SURGERY
Note: Most surgery articles are subclassified by specialty, even if general surgeons
were first authors or coauthors.
434. Crapko M, Fleshman J. Minimally invasive surgery for rectal cancer. Ann
Surg Oncol 2013 Sep 4 [Epub ahead of print].
435. de Montbrun SL, Roberts PL, Lowry AC, Ault GT, Burnstein MJ,
Cataldo PA, Dozois EJ, Dunn GD, Fleshman J, Isenberg GA, Mahmoud
NN, Reznick RK, Satterthwaite L, Schoetz D Jr, Trudel JL, Weiss EG,
Wexner SD, MacRae H. A novel approach to assessing technical competence of colorectal surgery residents: the development and evaluation
of the Colorectal Objective Structured Assessment of Technical Skill
(COSATS). Ann Surg 2013;258(6):1001–1006.
436. Dharmarajan S, Newberry EP, Montenegro G, Nalbantoglu I, Davis
VR, Clanahan MJ, Blanc V, Xie Y, Luo J, Fleshman JW Jr, Kennedy
S, Davidson NO. Liver fatty acid-binding protein (L-Fabp) modifies
intestinal fatty acid composition and adenoma formation in ApcMin/+
mice. Cancer Prev Res (Phila) 2013;6(10):1026–1037.
194
437. Fleshman J. Laparoscopic approaches in oncology. Surg Oncol Clin N
Am 2013;22(1):xi.
438. Fleshman JW. Multidisciplinary treatment of rectal cancer: the way of
the future. JAMA Surg 2013;148(8):778.
439. Grimm L Jr, Fleshman JW. Modern rectal cancer surgery—total mesorectal
excision—the standard of care. Sem Colon Rectal Surg 2013;24(3):125–131.
440. Klos CL, Safar B, Hunt SR, Wise PE, Birnbaum EH, Mutch MG, Fleshman
JW, Dharmarajan S. Accordion complication grading predicts short-term
outcome after right colectomy. J Surg Res 2013 Nov 19 [Epub ahead of
print].
441. Klos CL, Safar B, Jamal N, Hunt SR, Wise PE, Birnbaum EH, Fleshman
JW, Mutch MG, Dharmarajan S. Obesity increases risk for pouch-related
complications following restorative proctocolectomy with ileal pouchanal anastomosis (IPAA). J Gastrointest Surg 2013 Oct 4 [Epub ahead
of print].
442. Strouch MJ, Zhou G, Fleshman JW, Birnbaum EH, Hunt SR, Mutch
MG. Time to initiation of postoperative chemotherapy: an outcome
measure for patients undergoing laparoscopic resection for rectal cancer.
Dis Colon Rectum 2013;56(8):945–951.
TRANSPLANTATION (ORGAN AND PANCREATIC CELLS)
443. Allam SR, Krüger B, Mehrotra A, Schiano T, Schröppel B, Murphy
B. The association of IL28B polymorphism and graft survival in
patients with hepatitis C undergoing liver transplantation. PLoS One
2013;8(1):e54854.
444. Armstead SI, Hellmark T, Wieslander J, Zhou XJ, Saxena R, Rajora N.
A Case of Alport syndrome with posttransplant antiglomerular basement
membrane disease despite negative antiglomerular basement membrane antibodies by EIA treated with plasmapheresis and intravenous
immunoglobulin. Case Rep Transplant 2013;2013:164016.
445. Asrani SK. Liver transplantation for nonalcoholic steatohepatitis. Clin
Gastroenterol Hepatol 2013 Nov 19 [Epub ahead of print].
446. Asrani SK, Kim WR, Edwards EB, Larson JJ, Thabut G, Kremers WK,
Therneau TM, Heimbach J. Impact of the center on graft failure after
liver transplantation. Liver Transpl 2013;19(9):957–964.
447. Benjamin MM, Dasher KJ, Trotter JF. A comparison of outcomes between
OKT3 and antithymocyte globulin for treatment of steroid-resistant rejection in hepatitis C liver transplant recipients. Transplantation 2013 Oct
17 [Epub ahead of print].
448. Biggins SW, Trotter J, Gralla J, Burton JR Jr, Bambha KM, Dodge J,
Brocato M, Cheng L, McQueen M, Forman L, Chang M, Kam I, Everson
G, Spritz RA, Klintmalm G, Rosen HR. Differential effects of donor
and recipient IL28B and DDX58 SNPs on severity of HCV after liver
transplantation. J Hepatol 2013;58(5):969–976.
449. Campsen J, Zimmerman M, Trotter J, Hong J, Freise C, Brown R,
Cameron A, Ghobrial M, Kam I, Busuttil R, Saab S, Holt C, Emond
J, Stiles J, Lukose T, Chang M, Klintmalm G. Liver transplantation for
hepatitis B liver disease and concomitant hepatocellular carcinoma in
the United States with hepatitis B immunoglobulin and nucleoside/
nucleotide analogues. Liver Transpl 2013;19(9):1020–1029.
450. Campsen J, Zimmerman M, Trotter J, Hong J, Freise C, Brown RS Jr,
Cameron A, Ghobrial M, Kam I, Busuttil R, Saab S, Holt C, Emond
JC, Stiles JB, Lukose T, Chang MS, Klintmalm G. Multicenter review of
liver transplant for hepatitis B-related liver disease: disparities in gender
and ethnicity. Clin Transplant 2013;27(6):829–837.
451. Freeman J, Emond J, Gillespie BW, Appelbaum PS, Weinrieb R, HillCallahan P, Gordon EJ, Terrault N, Trotter J, Ashworth A, Dew MA,
Pruett T; A2ALL Study Group. Computerized assessment of competencerelated abilities in living liver donors: the Adult-to-Adult Living Donor
Liver Transplantation Cohort Study. Clin Transplant 2013;27(4):633–645.
452. Goldberg D, French B, Trotter J, Shetty K, Schiano T, Reddy KR, Halpern
SD. Underreporting of liver transplant waitlist removals due to death
or clinical deterioration: results at four major centers. Transplantation
2013;96(2):211–216.
453. Ikemoto T, Takita M, Levy MF, Shimada M, Naziruddin B. CD11b+ cells
in donor-specific transfusion prolonged allogenic skin graft survival through
indoleamine 2,3-dioxygenase. Cell Immunol 2013;283(1–2):81–90.
Baylor University Medical Center Proceedings
Volume 27, Number 2
454. Israni AK, Xiong H, Liu J, Salkowski N, Trotter JF, Snyder JJ, Kasiske BL.
Predicting end-stage renal disease after liver transplant. Am J Transplant
2013;13(7):1782–1792.
455. Kaneku H, O’Leary JG, Banuelos N, Jennings LW, Susskind BM,
Klintmalm GB, Terasaki PI. De novo donor-specific HLA antibodies
decrease patient and graft survival in liver transplant recipients. Am J
Transplant 2013;13(6):1541–1548.
456. Kim PT, Jang JH, Atenafu EG, Fischer S, Greig PD, McGilvray ID, Wei
AC, Gallinger S, Cleary SP. Outcomes after hepatic resection and subsequent multimodal treatment of recurrence for multifocal hepatocellular
carcinoma. Br J Surg 2013;100(11):1516–1522.
457. Kim PT, Onaca N, Chinnakotla S, Davis GL, Jennings LW, McKenna
GJ, Ruiz RM, Levy MF, Goldstein R, Klintmalm GB. Tumor biology and
pre-transplant locoregional treatments determine outcomes in patients
with T3 hepatocellular carcinoma undergoing liver transplantation. Clin
Transplant 2013;27(2):311–318.
458. Kim PT, Temple S, Atenafu EG, Cleary SP, Moulton CA, McGilvray
ID, Gallinger S, Greig PD, Wei AC. Aberrant right hepatic artery in
pancreaticoduodenectomy for adenocarcinoma: impact on resectability
and postoperative outcomes. HPB (Oxford) 2013 Jun 19 [Epub ahead
of print].
459. Kim PT, Wei AC, Atenafu EG, Cavallucci D, Cleary SP, Moulton CA, Greig
PD, Gallinger S, Serra S, McGilvray ID. Planned versus unplanned portal
vein resections during pancreaticoduodenectomy for adenocarcinoma. Br J
Surg 2013;100(10):1349–1356.
460. Klintmalm G, O’Farrelly C. Taking the rap: multiple effects of blocking
mammalian target of rapamycin. Hepatology 2013;57(1):1–3.
461. McKenna GJ, Trotter JF, Klintmalm E, Ruiz R, Onaca N, Testa G,
Saracino G, Levy MF, Goldstein RM, Klintmalm GB. Sirolimus and
cardiovascular disease risk in liver transplantation. Transplantation
2013;95(1):215–221.
462. Mengel M, Campbell P, Gebel H, Randhawa P, Rodriguez ER, Colvin R,
Conway J, Hachem R, Halloran PF, Keshavjee S, Nickerson P, Murphey
C, O’Leary J, Reeve J, Tinckam K, Reed EF. Precision diagnostics in transplantation: from bench to bedside. Am J Transplant 2013;13(3):562–568.
463. O’Leary JG, Gebel HM, Ruiz R, Bray RA, Marr JD, Zhou XJ, Shiller
SM, Susskind BM, Kirk AD, Klintmalm GB. Class II alloantibody and
mortality in simultaneous liver-kidney transplantation. Am J Transplant
2013;13(4):954–960.
464. O’Leary JG, Kaneku H, Jennings LW, Bañuelos N, Susskind BM,
Terasaki PI, Klintmalm GB. Preformed class II donor-specific antibodies are associated with an increased risk of early rejection after liver
transplantation. Liver Transpl 2013;19(9):973–980.
465. O’Leary JG, Klintmalm GB. Impact of donor-specific antibodies on results of
liver transplantation. Curr Opin Organ Transplant 2013;18(3):279–284.
466. O’Leary JG, McKenna GJ, Klintmalm GB, Davis GL. Effect of telaprevir
on the pharmacokinetics of sirolimus in liver transplant recipients. Liver
Transpl 2013;19(4):463–465.
467. Perrillo R, Buti M, Durand F, Charlton M, Gadano A, Cantisani G,
Loong CC, Brown K, Hu W, Lopez-Talavera JC, Llamoso C. Entecavir
and hepatitis B immune globulin in patients undergoing liver transplantation for chronic hepatitis B. Liver Transpl 2013;19(8):887–895.
468. Saliba F, De Simone P, Nevens F, De Carlis L, Metselaar HJ, Beckebaum
S, Jonas S, Sudan D, Fischer L, Duvoux C, Chavin KD, Koneru B,
Huang MA, Chapman WC, Foltys D, Dong G, Lopez PM, Fung J, Junge
G; H2304 Study Group. Renal function at two years in liver transplant
patients receiving everolimus: results of a randomized, multicenter study.
Am J Transplant 2013;13(7):1734–1745.
469. SoRelle JA, Itoh T, Peng H, Kanak MA, Sugimoto K, Matsumoto S,
Levy MF, Lawrence MC, Naziruddin B. Withaferin A inhibits pro-inflammatory cytokine induced damage to islets in culture and following
transplantation. Diabetologia 2013;56(4):814–824.
470. Takita M, Itoh T, Matsumoto S, Shimoda M, Chujo D, Iwahashi S,
Tamura Y, Onaca N, Naziruddin B, Bartlett BL, Levy MF. Autoimmune chronic pancreatitis with IgG4-related pancreatic pseudocyst in
a patient undergoing total pancreatectomy followed by autologous islet
transplantation: a case report. Pancreas 2013;42(1):175–177.
April 2014
471. Takita M, Nigar S, Levy MF, Naziruddin B. Beta cell function after islet
transplantation. In Escher AP, Li A, eds. Type 1 Diabetes. Rijeka, Croatia:
InTech, 2013:167–194.
472. Teperman L, Moonka D, Sebastian A, Sher L, Marotta P, Marsh C,
Koneru B, Goss J, Preston D, Roberts JP; Spare-the-Nephron Trial
Liver Transplantation Study Group. Calcineurin inhibitor-free mycophenolate mofetil/sirolimus maintenance in liver transplantation:
the randomized spare-the-nephron trial. Liver Transpl 2013;19(7):
675–689.
473. Trotter JF. Is disease recurrence still relevant to graft survival? Liver Transpl
2013;19(Suppl 2):S49–S55.
474. Trotter JF, Grafals M, Alsina AE. Early use of renal-sparing agents
in liver transplantation: a closer look. Liver Transpl 2013;19(8):
826–842.
475. Tsubokura M, Takita M, Matsumura T, Hara K, Tanimoto T, Kobayashi
K, Hamaki T, Oiso G, Kami M, Okawada T, Tachiya H. Changes in
metabolic profiles after the Great East Japan Earthquake: a retrospective
observational study. BMC Public Health 2013;13:267.
476. Wait MA, Ramsay MAE, Hardaway BW, Capehart JE, Rosenblatt RL.
Chylopericardium following orthotopic lung transplantation. Proc (Bayl
Univ Med Cent) 2013;26(3):280–282.
477. Wong F, O’Leary JG, Reddy KR, Patton H, Kamath PS, Fallon MB,
Garcia-Tsao G, Subramanian RM, Malik R, Maliakkal B, Thacker LR,
Bajaj JS. Validation of the new consensus definition of acute kidney injury
in predicting mortality in infected cirrhotic patients. Gastroenterology
2013;145:1280.
TRAUMA
478. Bombardier CH, Fann JR, Wilson CS, Heinemann AW, Richards JS,
Warren AM, Brooks L, Warms CA, Temkin NR, Tate DG. A randomized controlled trial of venlafaxine XR for major depressive disorder after
spinal cord injury: methods and lessons learned. J Spinal Cord Med 2013
Jun 26 [Epub ahead of print].
479. Dahdah MN, Barisa MT, Schmidt K, Barnes SA, Dubiel R, Dunklin C,
Harper C, Callender L, Wilson A, Diaz-Arrastia R, Shafi S. Comparative
effectiveness of traumatic brain injury rehabilitation: differential outcomes across TBI model systems centers. J Head Trauma Rehabil 2013
Sep 18 [Epub ahead of print].
480. Dickson S. Hypoxic and ischemic brain injury. In Stucky KJ, Kirkwood
MW, Donders J, eds. Clinical Neuropsychology Study Guide and Board
Review. New York: Oxford University Press.
481. Driver S, Irwin K, Woolsey A, Warren AM. Piloting a physical activity
centred education programme for adults with a brain injury. Brain Inj
2013;27(10):1173–1180.
482. Field C, Walters S, Marti CN, Jun J, Foreman M, Brown C. A multisite
randomized controlled trial of brief intervention to reduce drinking in
the trauma care setting: how brief is brief? Ann Surg 2013 Nov 20 [Epub
ahead of print].
483. Kenedi H, Campbell Vance J, Foreman M, Graybeal D, Reynolds J,
Dollaghan C, Santos TO, Gibson M, Burgardt M. Positive and negative
clinical indicators of the free water protocol in an acute care setting: two
pilot studies. J Head Trauma Rehabil 2013;28(5).
484. Self M, Driver S, Stevens L, Warren AM. Physical activity experiences
of individuals living with a traumatic brain injury: a qualitative research
exploration. Adapt Phys Activ Q 2013;30(1):20–39.
485. Thaler NS, Reger SL, Ringdahl EN, Mayfield JW, Goldstein G, Allen
DN. Neuropsychological profiles of six children with anoxic brain injury.
Child Neuropsychol 2013;19(5):479–494.
486. Warren AM, Hamilton R, Roden-Foreman K. Up close but not too
personal: establishing appropriate boundaries with individuals following
SCI. Sexuality and Disability 2013;31(4):303–311.
487. Warren AM, Jones AL, Shafi S, Roden-Foreman K, Bennett M, Foreman ML. Does caring for trauma patients lead to psychological stress in
surgeons? J Trauma Acute Care Surg 2013;75(1):179–184.
488. Warren AM, Stucky K, Sherman JJ. Rehabilitation psychology’s
role in the level I trauma center. J Trauma Acute Care Surg 2013;
74(5):1357–1362.
2013 publications of the Baylor Health Care System medical and scientific staff
195
489. Zgaljardic DJ, Oden KE, Dickson S, Plenger PM, Lambert ME, Miller
R. Naming Test of the Neuropsychological Assessment Battery: reliability
and validity in a sample of patients with acquired brain injury. Arch Clin
Neuropsychol 2013;28(8):859–865.
ETHICS
490. Houston S, Casanova MA, Leveille M, Schmidt KL, Barnes SA,
Trungale KR, Fine RL. The intensity and frequency of moral distress
among different healthcare disciplines. J Clin Ethics 2013;24(2):
98–112.
EDITORIALS AND MISCELLANEOUS
491. Allison B, Scheihing CH, Roberts WC. Tributes to George E. Hurt Jr.,
MD. Proc (Bayl Univ Med Cent) 2013;26(2):194–195.
492. DeMarco DC. Thirty years of innovation in gastroenterology: a personal
history. Proc (Bayl Univ Med Cent) 2013;26(3):311–313.
493. Edwards WLJ, Roberts WC. William Leslie Jack Edwards,
MD: a conversation with the editor. Proc (Bayl Univ Med Cent)
2013;26(3):322–330.
494. Ewing JI, Denham CA, Osborne CR, Green NB, Divers J, Pippen JE Jr.
Our experience as a Health Volunteers Overseas–sponsored team in Huế,
Vietnam. Proc (Bayl Univ Med Cent) 2013;26(2):137–141.
495. Frost S. Tribute to Elgin W. Ware Jr., MD. Proc (Bayl Univ Med Cent)
2013;26(2):199.
496. Goldstein AU, Ramsay MA. Tributes to Harold C. Urschel Jr., MD. Proc
(Bayl Univ Med Cent) 2013;26(2):196–198.
497. Greenfield LJ, Roberts WC. Lazar John Greenfield, MD: an interview
with the editor. Am J Cardiol 2013;112(9):1523–1532.
498. Hasse JM. Editor’s note. Nutr Clin Pract 2013;28(1):112; 28(3):288.
499. Hasse JM. Malnutrition. Nutr Clin Pract 2013;28(6):637–638.
500. Hasse JM. Nutrition support is a relatively new field. Nutr Clin Pract
2013;28(5):540.
501. Hasse JM. Research and publishing. Nutr Clin Pract 2013;28(2):152.
502. Hoppenstein J. Avocations. Proc (Bayl Univ Med Cent) 2013;26(1):27;
26(2):165; 26(3):255.
503. Khan A. Avocations. Proc (Bayl Univ Med Cent) 2013;26(1):24; 26(2):167.
504. O’Brien JC. My surgical heroes. Proc (Bayl Univ Med Cent) 2013;26(1):
67–75.
196
505. Phillips SJ, Roberts WC. Steven John Phillips, PhD: a conversation with
the editor with an emphasis on hospital and research safety. Proc (Bayl
Univ Med Cent) 2013;26(3):331–339.
506. Polter DE. Review of For the Love of Wild Things. Proc (Bayl Univ Med
Cent) 2013;26(4):427.
507. Ramsay MA, Usman M, De Vol E. In response to bioacoustics, breaths
and biostatistics. Anesth Analg 2013;117(6):1508.
508. Roberts WC. Facts and ideas from anywhere. Proc (Bayl Univ Med Cent)
2013;26(1):76–86.
509. Roberts WC. Facts and ideas from anywhere. Proc (Bayl Univ Med Cent)
2013;26(2):202–211.
510. Roberts WC. Facts and ideas from anywhere. Proc (Bayl Univ Med Cent)
2013;26(3):344–357.
511. Roberts WC. Facts and ideas from anywhere. Proc (Bayl Univ Med Cent)
2013;26(4):432–441.
512. Roberts WC. Good books in cardiovascular disease appearing in 2012
and early 2013. Am J Cardiol 2013;111:1829–1830.
513. Roberts WC. Proceedings of the editorial board meeting of The American Journal of Cardiology on March 10, 2013. Am J Cardiol 2013;112(1):139–141.
514. Rosenthal J. Avocations. Proc (Bayl Univ Med Cent) 2013;26(1):54;
26(2):158; 26(3):342; 26(4):386.
515. Rosenthal RL. Throw the stethoscope away: a historical essay. Am J
Cardiol 2013;111(12):1823–1828.
516. Rosenthal RL. What we counted. Am J Cardiol 2013;111(7):1073–1075.
517. Schiller LR. Review of Geriatric Gastroenterology. Proc (Bayl Univ Med
Cent) 2013;26(3):340.
518. Schiller LR. Together we do great things. Am J Gastroenterol 2013;108(1):5–6.
519. Schussler JM. Invited commentary: Depression and cardiovascular
disease: association, causation, and the right thing to do. Proc (Bayl Univ
Med Cent) 2013;26(1):10.
Note: This list (finalized on February 10, 2014) was based on submissions
from medical and allied health staff and on PubMed searches. Although the
list is representative of the year’s publications, some articles and book chapters
were undoubtedly missed, since not all researchers respond to the request for
publications. Staff are encouraged to submit their publications each year. For
more information or to submit publications for this list, please contact Cynthia
Orticio (cynthiao@BaylorHealth.edu).
Baylor University Medical Center Proceedings
Volume 27, Number 2
Volume 27
Number 2
April 2014
Baylor University Medical Center Proceedings
Multipatient Studies
79 Validation of Rules of TwoTM as a paradigm for assessing asthma
control
83
M. Millard, M. Hart, and S. Barnes
Impact of a surveillance screening program on rates of methicillinresistant Staphylococcus aureus infections with a comparison of
surgical versus nonsurgical patients
125 Triple-hit lymphoma
Improving hospital staff compliance with environmental cleaning
behavior
L. Ramphal, S. Suzuki, I. M. McCracken, and A. Addai
92
Ethnic disparities in the prevalence of the metabolic syndrome in
American adults: data from the Examination of National Health and
Nutrition Examination Survey 1999–2010
L. Ramphal, J. Zhang, and S. Suzuki
96
A cohort analysis of the cardiovascular risk factors in the employees of
a pediatric hospital from 2009 to 2012
L. Ramphal, J. Zhang, and S. Suzuki
100
Volume 27, Number 2 • April 2014
Baylor University Medical Center, Dallas, Texas
Factors affecting adherence to a quality improvement checklist on an
inpatient hepatology service
E. B. Tapper and M. Lai
103
Characteristics of Native Americans with HIV and implications for
care
C. Connel, J. S. Stroup, J. R. Stephens, and E. Martin
106
Comparison of the frequency and level of serum total cholesterol
>300 mg/dL in patients at the same Texas hospital in a single
month in 1993 and in 2013
W. C. Roberts, J. M. Ko, and R. Benavides Jr.
D. L. Glancy and D. L. Prout Jr.
N. Pemmaraju, J. Gill, S. Gupta, and J. R. Krause
128 Small bowel intussusception causing a postoperative bowel obstruction
following laparoscopic low anterior resection in an adult
A. S. Hussain, R. Warrier, and H. T. Papaconstantinou
131 Fatal abdominal hemorrhage associated with gallbladder perforation
due to large gallstones
L. R. Soto, H. R. Levine, S. A. Celinski, and J. M. Guileyardo
133 Methemoglobinemia precipitated by benzocaine used during
intubation
A. Afzal, R. Collazo, A. Z. Fenves, and J. Schwartz
136 Where is that hemodialysis catheter (superior vena cava or aorta)?
A case of intraarterial catheter placement
V. Tan and J. C. Schwartz
139 Renal failure due to Capnocytophaga canimorsus generalized
Shwartzman reaction from a dog bite (DF-2 nephropathy)
V. Tan and J. C. Schwartz
141 Imaging manifestations of a dreaded obstetric complication in the
immediate postpartum period
H. Levine, M. Zarghouni, and W. Cannon
143 Fetal demise due to cord entanglement in the early second trimester
R. N. Ergin, M. Yayla, and A. S. Ergin
145 Ingrown toenails (unguis incarnatus): nail braces/bracing treatment
Case Studies
108 Opsoclonus myoclonus syndrome: an unusual presentation for West
Nile virus encephalitis
A. Afzal, S. Ashraf, and S. Shamim
111
Fatal Clostridium septicum infection in a patient with a hematological
malignancy
R. Panikkath, V. Konala, D. Panikkath, E. Umyarova, and F. Hardwicke
113
Pages 77–196
Bilateral diaphragmatic paralysis associated with the use of the tumor
necrosis factor-alpha inhibitor adalimumab
M. M. Benjamin, A. W. Martin, and R. L. Rosenblatt
116
Celiac artery disease and fatal rupture of a hepatic artery aneurysm in
the Ehlers-Danlos syndrome
A. Nat, T. George, G. Mak, A. Sharma, A. Nat, and R. Lebel
118
120
To access Baylor’s physicians, clinical services, or
educational programs, contact the Baylor Physician
ConsultLine: 1-800-9BAYLOR (1-800-922-9567)
D. L. Glancy and M. Singh
124 Inverted P waves, QRS complexes, and T waves in lead I in a 64-yearold woman
A. Jennings, M. Bennett, T. Fisher, and A. Cook
88
123 Irregular cardiac rhythm with wide QRS complexes
The most common cause of hemoptysis worldwide: a fluke?
Editorials, Tributes, Book Review
150 Tributes to George J. Race, MD, PhD
W. L. J. Edwards, J. W. Fay, M. Ramsay, A. D. Roberts Jr., and M. J. Stone
153 Cardiologist in the shadow of Angkor Wat: a medical mission to
Cambodia
J. D. Cantwell
156 A tale of Congress, continuing medical education, and the history of
medicine
C. Partin, H. I. Kushner, and M. E. Kollmer Horton
161 Mentoring: a tale of two poems, filling graveyards, and learning the art
of medicine
C. Partin
A. Nat, A. Nat, A. Sharma, G. Shastri, and M. C. Iannuzzi
163 HIPAA: a flawed piece of legislation
Stress-induced (takotsubo) cardiomyopathy following thoracic epidural
steroid injection for postherpetic neuralgia
166 Book review: Selected Roberts Papers from Seven Generations
N. P. McKernan, B. J. Rondeau, and R. K. McAllister
122
A. Chiriac, C. Solovan, and P. Brzezinski
Invited commentary: Takotsubo cardiomyopathy following epidural
steroid injection: yet another way to break the heart
A. B. Weisse
F. D. Winter Jr.
168 From the editor: Facts and ideas from anywhere
W. C. Roberts
J. M. Schussler
www.BaylorHealth.edu/Proceedings
Indexed in PubMed, with full text available through PubMed Central