LYSOSOMAL STORAGE DISORDERS: FROM BASIC SCIENCE TO PUBLIC HEALTH Anatália Labilloy
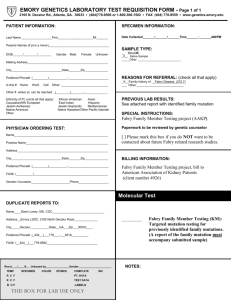
advertisement
LYSOSOMAL STORAGE DISORDERS: FROM BASIC SCIENCE TO PUBLIC HEALTH by Anatália Labilloy MD, Universidade Federal do Piauí, Brazil, 2010 Submitted to the Graduate Faculty of Department of Human Genetics Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2013 University of Pittsburgh Graduate School of Public Health This essay is submitted by Anatália Labilloy on April 8th 2013 and approved by Essay Advisor: David Finegold, MD Professor Department of Human Genetics Graduate School of Public Health University of Pittsburgh ________________________ Essay Reader: Karen Cuenco, PhD Assistant Professor Department of Oral Biology Center for Craniofacial Human Genetics School of Dental Medicine University of Pittsburgh ________________________ ii Copyright © by Anatália Labilloy 2013 iii David Finegold, MD LYSOSOMAL STORAGE DISORDERS: FROM BASIC SCIENCE TO PUBLIC HEALTH Anatália Labilloy, MPH University of Pittsburgh, 2013 ABSTRACT According to the first Principle of the Ethical Practice of Public Health by the Public Health Leadership Society, “Humans have a right to the resources necessary for health.” When dealing with rare inheritable conditions, oftentimes disease mechanisms remain largely unknown. The uniqueness of rare conditions render healthcare professionals unaware of their existence or of ways to deliver best medical care adapted to individual patients’ needs. Lysosomal Storage Disorders constitute a group of more than 50 rare heritable conditions that share some pathological and biochemical features and result in significant morbidity and early death. Most of the pathophysiological aspects of individual disorders of this group remain uncharacterized. Advances in clinical development of therapies in the past two decades have improved clinical outcomes for patients with some of these diseases, but progress still needs to be made for better management of some of the complications of these disorders. The cost associated with some of these therapeutic options still represents a limiting factor to access, especially in developing countries. This study’s primary aim was to foster basic science research in the field of lysosomal storage disorders by developing and iv characterizing a cell model for Fabry disease that can be used to understand disease pathogenesis for drug development. An additional aim was to develop a strategic plan for a public health genetics program with focus on Lysosomal Storage Disorders in an underprivileged state in a developing country. This study’s public health significance lies in the continuation of efforts to understand disease mechanisms, which potentially allow development of new therapeutic approaches through basic and clinical science research. In addition, efforts to increase awareness of these disorders among healthcare professionals, and to integrate research findings into clinical practice, fostering the delivery of evidence-based medical care in the field are of public health relevance and necessary to improve health of patients with Lysosomal Storage Disorders. v TABLE OF CONTENTS ACKNOWLEDGEMENTS…………………………………………….………………………XII 1. DEVELOPMENT OF A CELL MODEL OF FABRY DISEASE IN RENAL TUBULAR EPITHELIAL CELLS……………………………………………………………….……………1 1.1 INTRODUCTION AND BACKGROUND………….………..………………………….1 1.1.1 FABRY DISEASE DIAGNOSIS AND TREATMENT…………………………..9 1.1.2 MODELS OF FABRY DISEASE…………………….………………………....12 1.1.3 PUBLIC HEALTH RELEVANCE……………….………………………………14 1.2 METHODS……………………………………….……………………………………..16 1.3 RESULTS……………………………………………………………………………….18 1.4 DISCUSSION……………………………….…………………………………..………21 2. A PUBLIC HEALTH GENETICS PLAN FOR PIAUÍ STATE WITH FOCUS ON LYSOSOMAL STORAGE DISORDERS…………………………………………………….23 2.1INTRODUCTION AND BACKGROUND……………………………………………...23 2.1.1 HEALTHCARE IN BRAZIL……………..….…………………………………...23 2.1.2 PIAUÍ STATE DEMOGRAPHICS…….………………………………………..24 2.1.3 PIAUÍ STATE HEALTH DEPARTMENT……………..……………………….26 2.1.4 GENETICS IN BRAZIL……………….………………..……………………….28 2.1.4.1 NEWBORN SCREENING IN BRAZIL………………………………29 2.1.4.2 CURRENT GENETICS SERVICES IN PIAUÍ STATE………….…32 2.1.4.3 LYSOSOMAL STORAGE DISORDERS IN BRAZIL AND PIAUÍ STATE….........................................................................................................................33 2.2 NEEDS ASSESSMENT AND DEVELOPMENT OF A PUBLIC HEALTH GENETICS STATE PLAN IN LYSOSOMAL STORAGE DISORDERS………...……….34 2.2.1 MISSION………………....…………………………………………………..…...34 vi 2.2.2 ASSUMPTIONS……………………………………………….…………………35 2.2.3 NEEDS ASSESSMENT……………………………………………………………..35 2.2.4 GOALS, OBJECTIVES AND ACTIVITIES…..…………………………………….37 2.2.4.1 GOAL 1…………………………………………………………………….......37 2.2.4.2 GOAL 2…………………………………………………………………………39 2.2.4.3 GOAL 3…………………………………………………………………………40 2.2.5 PROGRAM DEVELOPMENT STRATEGY………………………………………..40 2.2.6 EVALUATION PLAN…………………………………………………..…………….41 2.2.7 EXPECTED OUTCOMES AND IMPACT………………………………………….44 2.2.8 CHALLENGES……………………………………………………………………….45 3. FINAL CONSIDERATIONS AND FUTURE DIRECTIONS……..……………………..45 APPENDIX A: LYSOSOMAL STORAGE DISORDERS……………………………….….48 APPENDIX B: GOVERNMENTAL AND NON-GOVERNMENTAL ORGANIZATIONS PROVIDING CARE FOR INDIVIDUALS WITH DISABILITIES/SPECIAL NEEDS IN PIAUÍ STATE, BRAZIL………………………………………………………………………..50 BIBLIOGRAPHY…………………………………………………………………………….....52 vii LIST OF ABBREVIATIONS α-Gal A Alpha-galactosidase A CNS Central Nervous System eGFR estimated Glomerular Filtration Rate ERT Enzyme replacement therapy Gb3 Globlotriaosylceramide GSL Glycosphingolipid HIV human immunodeficiency virus IFN Interferon LSD Lysosomal Storage Disorder M6P Mannose-6-phosphate MDCK Madin-Darby canine kidney MHC major histocompatibility complex MRI Magnetic Resonance Imaging mRNA messenger ribonucleic acid siRNA small interfering ribonucleic acid SRT Substrate Reduction Therapy SUS Brazilian Unified Health System TIA Transient Ischemic attack viii NPHPSP National Public Health Performance Standards Program ix LIST OF TABLES Table 1: Lysosomal Storage Disorders with available treatment ………………………….6 Table 2: The Essential Public Health Services………..……………………………………14 x LIST OF FIGURES Figure 1: Fabry disease progresses with age, resulting in multisystem involvement and early death. ...............................................................................………..………………….2 Figure 2: Disorders of GSL and ganglioside metabolism and their relationship. .......... …5 Figure 3: Efficient silencing of α-Gal A expression in MDCK cells by siRNA transfection ..................................................................................................................................... 18 Figure 4: α-Gal A silenced MDCK cells have increased levels of Gb3......................... 19 Figure 5: Electron micrographs of MDCK cells treated with control and α-Gal A siRNA.20 Figure 6: Accumulation of "zebra bodies in α-Gal A siRNA treated MDCK cells............ 21 Figure 7: Strategy for the Program Development phase of a Public Health Genetics Plan for Piauí State with Focus on LSDs. .............................................................................. 40 xi ACKNOWLEDGEMENTS Another cycle has ended for others to begin. The accomplishments that I have achieved during my academic studies leading to a Master in Public Health in Public Health Genetics at the University of Pittsburgh were unparalleled. The difficulties and barriers existed, but with determination, hard work and full support from the professors of the Department of Human Genetics and from my wonderful classmates the path was smooth and the professional and personal achievements were very fruitful. I would like to express my sincere gratitude to my thesis advisor Dr David Finegold for guiding and supporting me over the progress of my graduate studies, and for being an example of passionate scientist and caring doctor. I would also like to thank Karen Cuenco for accepting to be part of my thesis committee and her helpful advices, Dr Robert Ferrell for inspiring conversations and my academic advisor Dr Candance Kammerer for the patience and invaluable guidance. I am especially thankful to Dr Ora Weisz for introducing me to key concepts in basic science research in cell biology, a field that was new to me. She has encouraged me and served as a role model of a successful scientist, leader and woman. Jennifer Bruns was also essential to this work for her friendship and technical support with the experiments in developing the renal cell model. I couldn’t have worked in a better environment than the one I found at Dr Weisz’s lab. xii Foremost I would like to thank my family for always being there for me, my husband Guillaume for his love, patience and understanding and my parents for having always invested in my education and for showing full support even being so far away. You are the foundation for my academic success. Lastly, I would also like to acknowledge the financial support from Shire HGT as a grant to the Graduate School of Public Health for a scholarship in the field of Lysosomal Storage Disorders. xiii 1. DEVELOPMENT OF A CELL MODEL OF FABRY DISEASE IN RENAL TUBULAR EPITHELIAL CELLS 1.1 Introduction and Background Fabry disease is an X-linked lysosomal storage disorder (LSD) caused by abnormal function of the lysosomal hydrolase α-galactosidase A (α-Gal A), encoded by the gene GLA. [1] Deficiency of α-Gal A leads to progressive accumulation of its substrates, neutral glycosphingolipids (GSLs) with terminal αD-galactosyl residues, mainly globotriaosylceramide (Gb3), in a variety of cell types. [2] Fabry disease occurs in both males and females, and classic clinical presentation of the disease includes renal, cardiovascular, cerebrovascular, neurological, gastroenterological, dermatological, ocular, and auditory findings, among others, resulting in significant morbidity and early death. [3, 4] Figure 1 shows a diagram with some of the clinical findings of Fabry disease and its disease progression with age. The first signs and symptoms of Fabry disease often appear in the first decade of life, mostly presenting as neuropathic pain, gastrointestinal symptoms, and impaired quality of life. Some pediatric patients may also present with serious complications of Fabry disease and multi-system organ involvement. Data from Fabry registry have show a mean age of onset of symptoms of 6 years for boys and 9 years for girls. [5-7] 1 alpha-galactosidase A deficiency Progression with age glycosphingolipid accumulation neuropathic pain, exercise intolerance, gastrointestinal symptoms, cornea verticillata and angiokeratomas microalbuminur ia, proteinuria hyperfiltration, isosthenuria End-Stage renal Disease hypertrophic cardiomyopath y, short PR interval, arrhythmias Systolic and diastolic dysfunction, myocardial infarction MRI white matter lesions, vertebrobasilar dolichoectasia, pulvinar sign TIA and strokes Considerable morbidity and mortality Figure 1: Fabry disease progresses with age, resulting in multisystem involvement and early death. Progression in any organ system can proceed independently from the others. MRI: magnetic resonance imaging; TIA: transient ischemic attack. Adapted from [8] Some patients may never display the classic phenotype, presenting a milder form of the disease. In fact, “cardiac variants” and “renal variants” of Fabry disease have been described, where patients present disease limited to only one or few organs. [9] The kidney is one of the most affected organs in individuals with Fabry disease. While advanced stages of renal chronic disease usually present in middle adulthood, the first histological signs of Fabry nephropathy have been seen as early as in utero. [5] Additionally, children with Fabry disease can 2 present early signs of kidney involvement such as hyperfiltration, microalbuminuria, and overt proteinuria [10, 11]. Within the kidney, podocytes seem to be the most involved cell type, showing a greater degree of vacuolization. However, Gb3 inclusions are also observed in proximal and distal tubules as well as mesangial, endothelial, and vascular smooth muscle cells. As Fabry nephropathy progresses, mesangial expansion, interstitial fibrosis, tubular atrophy, and glomerulosclerosis are observed. [12]. Fabry disease is the second most common disease of its group of LSDs, behind only Gaucher disease, an autosomal recessive form of LSD characterized in its most common form mainly by spleen, liver, lungs, bone and bone marrow involvement. [13] Currently, more than 50 disorders have been clinically categorized as LSDs, resulting from deficient activity of specific lysosomal enzymes or abnormalities in transmembrane proteins as well as in proteins involved in lysosomal biogenesis. [14] Appendix A presents a comprehensive list of LSDs. Although individually rare, the estimated combined prevalence of this group of conditions ranges from 1:4,000 to 1:8,000 births. [15] In spite of being considered panethnic, Individual estimates of incidence vary from study population and some disorders of this group are thought to be underdiagnosed; some disorders of this group such as Gaucher disease, mucolipidosis type IV, Tay-Sachs disease and Niemann-Pick disease have increased incidence in Ashkenazi Jews, attributed to historical founder effects and genetic drift.[16] In spite of their genetic heterogeneity, LSDs share the phenotype of accumulation of one or several substrates within lysosomes and in non- 3 lysosomal compartments, as well as some clinical and biochemical features [17, 18]. Figure 2 shows the biochemical link among several LSDs. As lysosomal sphingolipid degradation occurs in a step-wise manner, the product of degradation of one enzyme serves as the substrate for the subsequent reaction. In addition, two or more pathways can be interconnected, presenting the same final product. As an example, lactosylceramide acts as a product of both alphagalactosidase A degradation of Gb3 and of sialidase degradation of GM3. Moreover, the same sphingolipid activator protein (SAP), which are proteins required for hydrolysis of sphingolipids, can participate in different steps of GSL metabolism. [19] Specific treatment is available for several LSDs, and early diagnosis and management translates into better outcomes for patients. Treatment options either clinically available or under research development for disorders of this group include enzyme replacement therapy (ERT), substrate reduction therapy (SRT), hematopoietic stem cell therapy (HSCT), chemical chaperones, cell therapy and gene therapy. [27] Table 1 shows a list of treatable LSDs with their respective estimated incidence and treatment options available or under development. 4 Figure 2: Disorders of GSL and ganglioside metabolism and their relationship. Abbreviations: DHCer (dihydroceramide), S1P (sphingosine 1-phosphate), SM (sphingomyelin) . [19] Several studies have estimated the prevalence of Fabry disease to range between 1:40,000 and 1:117,000 live births. [20] With recent advances in highthroughput multiplex enzyme assays using tandem mass spectrometry, allowing feasibility for larger scale screening tests, some countries have started pilot 5 newborn screening programs for some LSDs, including Fabry disease. [21, 22] Surprisingly, newborn screening data suggests a much higher incidence of Fabry disease than initially thought, ranging from 1:3,859 newborns in Austria [23] and 1:3,100 in Italy [24] to as high as 1:557 births in Taiwan [25]. This suggests that the disease might be greatly under-diagnosed worldwide. In the United States, pilot newborn screening studies for Fabry disease and other LSDs are currently being performed. If expanded to the whole country, more than 1,000 babies are expected to be diagnosed with the disease each year in the United States, based upon estimates from European countries [23-24]. However, newborn screening for LSDs remains controversial, since specific treatment is unavailable for some conditions of the group. In addition, the onset of symptoms for some LSDs may not occur until adulthood, in those circumstances neonatal diagnosis may not interfere with the clinical course of the disease. [26] Table 1: Lysosomal Storage Disorders with available treatment. Disease Treatment available Aspartylglucosaminuria HSCT available Fabry disease ERT available, Chaperones in CD Fucosidosis HSCT available Gaucher disease ERT, SRT and HSCT available Krabbe disease HSCT available α-Mannosidosis HSCT available, ERT in CD Metachromatic leukodystrophy IT-ERT in CD, gene therapy in CD MPS I ERT and HSCT available MPS II ERT available; IT-ERT in CD MPS III (all types) IT- ( in CD or MPS IIIA; SRT in CD; GT in CD 6 Table 1 continued MPS IV A ERT in CD MPS VI ERT available, HSCT available Mucolipidosis II/III HSCT in CD Neuronal ceroid lipofuscinosis Cell therapy in CD, gene therapy in CD Niemann-Pick B ERT in CD Niemann-Pick C SRT available, HSCT in CD for NPC2 Pompe disease ERT available Sandhoff disease Chaperones in CD for late-onset forms Tay-Sachs disease Chaperones in CD for late-onset forms Adapted from ref. [27] The lysosomal hydrolase α-Gal A enzyme is encoded by the gene GLA, located in Xq22. The GLA gene is comprised of seven exons and 12,436 base pairs. [1] In the lysosome lumen, α-Gal A is found as a homodimer, each monomer presenting a N-terminal, which contains the active site, and a Cterminal. [28] According to the Human Gene Mutation Database, over 600 mutations have been described for Fabry disease. (http://www.hgmd.org). The majority of mutations in GLA gene leading to Fabry disease are missense and translate into a disruption of the hydrophobic core of α-Gal A, which makes Fabry disease primarily a disease of protein-folding. [29] Gb3, also known as CD77 and Pk, is the primary glycosphingolipid degraded by α-Gal A. Biosynthesis of Gb3 from lactosylceramide is performed by the type II membrane protein alpha-1,4-galactosyltransferase (A4GALT) in the Golgi apparatus. [30] After its synthesis, Gb3 is then incorporated into the plasma membrane and intracellular membranes, with a preference for sphingolipid and 7 cholesterol enriched microdomains (aka, lipid rafts). This glycosphingolipid can also shed from the plasma membrane, being found in the plasma associated with lipoproteins, preferentially LDL. [31] Gb3’s deacylated form, globotriaosylsphingosine, aka lyso-Gb3, is also elevated in Fabry disease. Lyso-Gb3 is degraded by α-Gal A at a rate 50 times lower than Gb3, and presents inhibitory properties over both native and recombinant α-Gal A. [32] Thus, lyso-Gb3 might have additional direct contribution to the pathogenesis of the disease and in organ-response to therapy. Gb3 has been implicated in a variety of cellular processes. As an example, Gb3 is the receptor for the subunit B of Shiga and Shiga-like toxins (Stx) produced by bacteria as Escherichia coli and Citrobacter freundii. [33, 34] Gb3 is also one of the several glycolipids that act as co-receptor for gp120 in HIV entry, being required in CD4/CXCR4-dependent fusion. [35, 36] In fact, this interaction is being further explored in the development of new therapies for HIV, as the Gb3 analog adamantylGb3 inhibits HIV infection in vitro. [37] As a component of sphingolipid- cholesterol enriched microdomains, Gb3 is thought to play a role in signal transduction, with major involvement in inflammation and immune responses. Gb3 is involved in CD19-mediated adhesion and is required for both interferon-alpha induced growth inhibition and for the plasma membrane localization of Hsp70 [38, 39]. In addition, MHC class II and type 1 IFN receptor molecules present binding domains for Gb3, corroborating with its role in immune response [40, 41]. Moreover, Gb3, along 8 with other globo series glycosphingolipids, can be a mediator of the cSrc kinase, beta-catenin, and caspase signaling pathways [42]. Increase in levels of Gb3 is not a specific finding of Fabry disease. Although to a lesser extent than in Fabry disease, Gb3 levels are elevated in Niemann-Pick C, another LSD, which is consistent with the fact that these conditions share some of their pathophysiology. [43] Greater Gb3 levels can also be seen in more common disorders. Cells in pre-cancerous and cancerous states, such as colorectal adenoma, Burkitt’s lymphoma, breast cancer, and testicular carcinoma may also present increased levels of Gb3. [44] Interestingly, this increase in Gb3 levels is considered a sign of bad prognosis in these conditions, being associated with multidrug resistance and greater invasiveness. [45] However, both the underlying mechanism for such an increase in Gb3 levels and the cellular consequences culminating in greater tumor aggressiveness remain unclear. Some cytokines such as TNF-alpha and Interleukin-1 are shown to up-regulate Gb3 levels [46, 47] nevertheless the pathophysiological impact of such increases also needs to be better understood. 1.1.1 Fabry disease Diagnosis and Treatment Due to the presence of several signs and symptoms that mimic common disorders, the absence of pathognomonic clinical features, and marked phenotypical heterogeneity, clinical diagnosis of Fabry disease is usually delayed and involve visits to several medical specialists and misdiagnoses. [48] After onset of clinical manifestation, overall diagnostic delays are about 15 years for both genders [49], with possiblly even longer delays in developing countries. 9 Some of the misdiagnoses include rheumatoid arthritis, rheumatic fever, systemic lupus erythematous, Raynaud’s disease, celiac disease, and multiple sclerosis, among others. [9] After clinical suspicion is raised, demonstration of deficient αGal A in leukocytes in males is sufficient to establish a diagnosis of Fabry disease in males, and may be followed by mutational analysis of GLA gene. An initial screening through plasma enzyme activity in dried blood spots can be performed in males, but should be confirmed by leukocyte enzyme activity/genotyping. For females, disease status should be determined by mutation analysis of GLA since α-Gal A enzyme activity may be within the normal range in females even in the presence of overt disease. [50] In the recent years, there have been increased screening efforts for diagnosis of Fabry disease in high-risk adult populations. These efforts included screening for Fabry disease among patients with end-stage renal disease [51], unexplained hypertrophic cardiomyopathy [52, 53] and young patients presenting with stroke but no apparent predisposing factor [54]. Most of the studies focused in male patients due to the low sensitivity of the enzyme activity analysis in females, who usually require genotyping, a more expensive and laborious method, for definite diagnosis. These studies have shown prevalence of Fabry disease in high-risk populations ranging from 0 to 12 percent. Although the presence of residual α-Gal A activity is associated with slower progression of Fabry nephropathy, α-Gal A in plasma or leukocyte enzyme activity levels do not always correlate with disease phenotype. Similarly, conservative amino acid changes in GLA gene may be associated with slower 10 progression of the disease, but genotype-phenotype correlations have not been fully established for Fabry disease. Phenotype heterogeneity may play a role even within a single family of individuals sharing the same genotype. [55] Currently, the only commercially available treatment option for patients with Fabry disease consists of recombinant enzyme replacement therapy (ERT) administered intravenously. There are two approved forms of recombinant enzyme: agalsidase alfa and agalsidase beta. Agalsidase alfa is engineered in a human fibroblast cell line and presents amino acid sequence identical to that of native human α-Gal A, being glycosylated with both sialic acid and mannose-6phosphate (M6P) residues. Its administration occurs intravenously at a dose of 0.2 mg/Kg every other week. [56] Agalsidase beta is produced in Chinese hamster ovary cells, also presenting the same amino acid sequence as the native human α-Gal A. The approved dose for its intravenous administration is 1 mg/Kg every other week. [57] The pattern of glycosylation as well as M6P receptor binding and M6P receptor mediated endocytosis slightly differs between the two recombinant enzymes. Agalsidase beta presents a higher number of fully sialylated oligossacharides and a higher level of phosphorylation in comparison to agalsidase alfa. However, these discrepancies do not seem to translate in functionally relevant differences. [58, 59] Long-term ERT significantly improves overall clinical status of individuals with the disease, mainly by reducing neuropathic pain, decreasing cardiomyopathy, and improving quality of life. [60-62] However, both ERT regimens are only able to slightly retard the progression of chronic kidney 11 disease, and a steady decline of eGFR is still observed despite long-term treatment. [63, 64] Moreover, as the intravenously administered enzyme does not cross the blood brain barrier, disease progression in the CNS resulting in white matter lesions and strokes remains unchanged in spite of ERT. [65] A better comprehension of the pathophysiology of Fabry disease could provide the means to develop better clinical approaches and novel pharmacological targets in the management of Fabry disease patients. Other treatment options are currently under investigation. Results of a phase II clinical trial for the pharmacological chaperone Migalastat HCl were recently published, showing that its oral administration in patients with responsive mutations increased blood α-Gal A activity by 50 percent. [66] The iminosugar binds and stabilizes the nascent enzyme in the ER, restoring its efficient trafficking to lysosomes in the cases where proper trafficking of the misfolded enzyme is the main contributing factor for enzyme deficiency. [67] A phase III clinical trial for migalastat is currently ongoing. A plant cell-expressed recombinant α-Gal A, PRX-102, is also under a phase I/II clinical trial study for treatment of Fabry disease. The recombinant enzyme has undergone chemical modifications to improve enzyme activity and stability and to decrease its immunogenicity. [68] 1.1.2 Models of Fabry Disease Although naturally occurring animal models have been reported for other LSDs, no animals have been identified with Fabry disease. A knockout mouse 12 model for Fabry disease with lack of α-Gal A activity was developed and described by Oshima et al. [69] However, use of this knockout mice model in translational research has been controversial; while the mice present some histological changes compatible with Fabry disease, both male and female mice appear to be clinically normal,[69] or present mild phenotype as they age [70, 71], not reflecting what occurs in humans with classic phenotype. Establishment of cell models have also been an useful as a tool for testing hypotheses of disease pathogenesis, for identifying biomarkers of disease progression and clinical prognosis, and for early-stages drug development and testing for several human diseases. One of the technologies being used to study protein function in the context of a living cell and to generate knockdown of proteins of interest for human disease is RNA interference (RNAi). Small interfering RNA (siRNA) molecules serve as a template to the multi-protein complex RISC (RNA induced silencing complex) for recognition of complementary mRNA of interest, which results in activation of RNAse, culminating in cleavage and degradation of the mRNA and consequent loss of protein translation. [72] siRNA mediated transient silencing of α-Gal A could mimic the loss of protein activity observed in Fabry disease in different cell types. This technology would be of particular significance for kidney cells, as the pathophysiology of Fabry nephropathy is poorly understood and the kidneys of Fabry patients have little response to therapy, making kidney cells a good target for the studies on disease pathogenesis and drug discovery. 13 Madin-Darby canine kidney (MDCK) cells, isolated from dog kidney cortex and easily cultivated as polarized monolayers in vitro, have been studied and characterized extensively as a model for the study of renal cell function. [73]. In this study, we have designed, developed and characterized a renal epithelial tubular cell model for the study of the effects of deficiency of α-Gal A. 1.1.3 Public Health Relevance The National Public Health Performance Standards Program (NPHPSP) through the Core Public Health Functions Steering Committee has established in 1994 the “Ten Essential Public Health Services”, which constitute the essential framework for the core public health activities. Error! Reference source not found. shows a list of the Essential Public Health Services. The 10th essential public health service, “research for new insights and innovative solutions to health problems” can be interpreted as the responsibility of public health systems to investigate human diseases and their mechanisms, search for elucidation of their pathophysiology as well as promote means of developing new therapies. Table The Essential Public Health Services Table 2 2: continued 1. Monitor health status to identify and solve community health problems 2. Diagnose and investigate health problems and health hazards in the community 3. Inform, educate, and empower people about health issues 4. Mobilize community partnerships and action to identify and solve health problems 5. Develop policies and plans that support individuals and community health efforts 6. Enforce laws and regulations that protect health and ensure safety 7. Link people to needed personal health services and assure the provision of health care when otherwise available 8. Assure competent public and personal health care workforce 14 Progress in basic science research involving the development of cell 9. Evaluate effectiveness, accessibility, and quality of personal and populationbased health services 10. Research for new insights and innovative solutions to health problems models for human diseases are an essential first step for understanding the cellular dysfunctions underlying disease mechanisms, for identifying prognostic factors and biomarkers of disease progression, and for evaluating therapeutic approaches to cure diseases. These models are especially crucial in cases where mouse models do not replicate human disease phenotypes, such as in Fabry disease. Moreover, a better understanding of the pathophysiology of this relatively rare condition can potentially help unravel pathogenic mechanisms underlying some common diseases. In fact, Fabry nephropathy resembles diabetic nephropathy in humans. [74] Moreover, a link between glycosphingolipid metabolism and development and progression of diabetic nephropathy and metabolic syndrome has been suggested. [75] Furthermore, as previously mentioned, Gb3 is also elevated in certain cancers. This increase is associated with metastasis and tumor aggressiveness and a decreased response to chemotherapy drugs. In addition, some LSDs within the group of sphingolipidosis may also play a role in complex disorders. For instance, mutations in GBA, the gene encoding beta-glucocerebrosidase and causing Gaucher’s disease, have been found to be the most common risk factor ever described for Parkinson’s disease. [76] As this disease also presents elevated levels of sphingolipids, elucidation of disease mechanisms for Fabry disease may lead to new avenues 15 of investigation of the link between Parkinson disease and the LSD Gaucher disease. 1.2 Methods Cell culture. Madin-Darby canine kidney (MDCK) cells were incubated on 10 cm plastic dishes in MEM with 10% fetal bovine serum (FBS) at 37 oC with 5% CO2. Nonpolarized cells were cultured on 12 mm permeable supports with 0.4 m pores for four to six days prior to the experiments. siRNA knockdown. We designed a small interfering RNA (siRNA) for transient knockdown of the canine α-Gal A targeting the following sequence 5’GATAGATCTGCTGAAATT-3’. siRNA against firefly luciferase targeting the sequence 5’-GAATATTGTTGCACGATTT-3’ was used as a control. The custom siRNA duplex and control siRNA constructs were purchased from Dharmacon. MDCK cells were transfected with either α-Gal A or control siRNA using Lipofectamine™ 2000 transfection reagent (Invitrogen, Inc) and Opti-MEM® I Reduced Serum Media (Invitrogen, Inc). Briefly, 2.6 μg of either α-Gal A or control siRNA were incubated with 10 μL of lipofectamine and 250 μL of OptiMEM for 30 minutes at room temperature. 125 μL of the transfection mix and 5 x 105 subconfluent MDCK cells suspended in 333 μL of MEM were added to upper chamber of a 12-well transwell filter and briefly homogenized. Growth media was replaced within 6 to 8 hours of transfection and every other day subsequently. Experiments were performed three to six days later. 16 RT-PCR. Isolation of total RNA was performed using kit RNAquous (Ambion) according to manufacture’s recommendations. Purified total RNA underwent reverse transcription by incubation with Moloney murine leukemia virus reverse transcriptase (Ambion) at 42°C for 1 hour. PCR for canine alpha-galactosidase was carried out using Phusion ® High-Fidelity PCR kit (New England BioLabs, Inc.), having as sense primer 5’-TGTGCAACGTTGACTGCCAAGAAG-3’ and the anti-sense primer 5 ’- TCCTGCAGGTTTACCATAGCCACA-3’. As a control, RTPCR for canine beta-actin was also carried out using the sense primer 5’CTGCTGGAAGGTGGACAG-3’ and the anti-sense primer 5’- ACCTTCAACTCCATCATGAAG-3’. Denaturing temperature was 95oC, annealing temperature was 58oC, and extension temperature of 68oC, with 25 cycles of amplification. Indirect Immunofluorescence and confocal microscopy. Immunofluorescence was performed according to the protocol described by Mattila et al. [77] Anti-CD77 monoclonal antibody (clone 38-13, Abcam), which recognizes Gb3, was used at a dilution of 1:10. Goat anti-rat secondary antibodies (Alexa 488 and Cy5) were used at a dilution of 1:500. Capture of images was performed on an Olympus Fluoview FV1000 laser-scanning confocal microscope in the RenalElectrolyte Division, University of Pittsburgh School of Medicine. Electron microscopy. Membranes containing monolayers of α-Gal A knockdown and control MDCK cells were fixed in 2.5% of glutaraldehyde, 2% of paraformaldehyde in PBS and post-fixed in 1% Osmium tetroxide. Samples were 17 then dehydrated in graded series of ethanol solutions and embedded in EPON according to standard procedures. Ultra-thin sections were stained with uranyl acetate and lead citrate and examined using a JEOL electron microscope, in collaboration with Dr Willi Halfter, University of Pittsburgh. 1.3 Results Silencing of α-Gal A in MDCK cells In order to confirm knockdown of the protein of interest at the mRNA level, RT-PCR for α-Gal A was performed. Canine beta-actin was used as a PCR control. Significant reduction of α-Gal A mRNA was observed in the α-Gal A silenced MDCK cells compared to control, without significant differences in betaactin levels (Figure 3). Figure 3: Efficient silencing of α-Gal A expression in MDCK cells by siRNA transfection. MDCK cells were transfected with siRNA targeting canine α-Gal A or firefly luciferase (control) and processed for RTPCR after three days to determine the extent of GLA mRNA reduction. Accumulation of Gb3 in MDCK cells silenced for α-Gal A 18 In order to evaluate the effect of α-Gal A silencing in MDCK cells on metabolism of neutral D-α-galactosyl GSL, levels of Gb3 were investigated using specific monoclonal antibody against CD77, its membrane-bound form, followed by indirect immunofluorescence. Intensity and pattern of Gb3 staining were compared between cells transfected with either α-Gal A or non-silencing siRNA using fluorescence microscopy. A drastic increase in Gb3 staining intensity, in a punctate pattern, was observed in α-Gal A silenced cells after three days of transfection compared to non-silenced MDCK cells ( Figure 4). Figure 4 α-Gal A silenced MDCK cells have increased levels of Gb3.. MDCK cells were treated with control (left panel) or α-Gal A (right panel) siRNA for six days, then processed for indirect immunofluorescence with anti-CD77 (Gb3) antibody (red). Immunofluorescence microscopy images were acquired and processed using identical settings. Ultrastructural changes induced by α-Gal A silencing Light and electron microscopy of biopsied tissues of patients with Fabry disease usually show celldisease usually show cell-type specific ultra-structural changes that are characteristic of LSDs. In characteristic of LSDs. In cell types with greater degree of lipid deposition, electron microscopy electron microscopy shows several degrees of intracellular vacuolization and the presence of 19 presence of membranous concentric or parallel shapes of packing of lipid aggregates in the aggregates in the lysosomes, also called “zebra bodies”, are especially found. [78, 79] To further [78, 79] To further investigate ultrastructural changes induced by α-Gal A transient silencing, transient silencing, electron microscopy was performed after six days of transient α-Gal A α-Gal A knockdown. We observed a greater number of round electron-dense structures in α-Gal A structures in α-Gal A silenced MDCK cells, corresponding to lysosomes (Figure 5). Furthermore, We have visualized in the α-Gal A silenced cells some lamellar myelin-like structures, corresponding to “zebra bodies” ( Figure 6). Figure 5: Electron micrographs of MDCK cells treated with control and α-Gal A siRNA. MDCK cells were transfected with control (left panel) or α-Gal A siRNA (right panel) and plated on permeable support for 3 days before processing for transmission electron microscopy. Increased osmiophilic bodies (arrows) are seen in the GLA-siRNA treated MDCK cells. 6,000x magnification. 20 Figure 6: Accumulation of "zebra bodies in α-Gal A siRNA treated MDCK cells. Electron micrograph of a lysosome containing transversely-stacked, osmiophilic myelin-like membranes, also called a “zebra body”, in MDCK cells transiently silenced with α-Gal A siRNA. 60,000x magnification. 1.4 Discussion In this study, we have developed an in vitro model of Fabry disease in renal tubular epithelial cells using RNAi technology. The α-Gal A silenced cells present a dramatic increase in membrane-bound Gb3 levels, as well as ultrastructural changes compatible with Fabry disease, such as increased number of electron-dense structures corresponding to lysosomes and the characteristic presence of “zebra bodies”. Due to its effectiveness in showing disease phenotype in a short period of time, as well as its reproducibility, this model might be of great utility for testing hypotheses on disease pathogenesis and in highthroughput initial screening in drug development not only for Fabry disease, but also for common disorders in which overexpression or decreased metabolism of the GSL may also be found, such as certain types of cancer. 21 Post-transcriptional gene silencing using RNAi technologies has proven to be effective and easily reproducible. In the past few years, it has been widely used for developing disease models such as well as for targeted therapy for a variety of disorders. [80] However, some limitations are foreseen. Although presenting less potential biological risks than the use of lentiviral vectors for stable expression, silencing for a particular gene using siRNA molecules remains effective only for up to few days after the administration of their transfection in cell culture systems due to successive cell divisions and the action of cellular nucleases. [80] Therefore, for maintenance of disease status and study of effects of chronic exposure to substrates, successive transfections might be necessary. The extensive use of MDCK cells in research has made them a wellcharacterized cell line in the study of intracellular events and renal cell function. However, a foreseen limitation in the use of MDCKs in translational research, as it is with other species, is that although a considerable homology between the human and canine genome exists, there might be some traits that are speciesspecific and cannot be extrapolated to humans. [81] Although presenting limitations, cell models continue to represent essential tools for understanding the fundamental bases of disease, for identifying prognostic factors and biomarkers of disease progression, and for the initial steps in the development and evaluation of therapeutic approaches to treat human disease. These models are especially crucial in cases where knockout mice do not present the same phenotype as humans, presenting challenges for translational research. 22 2. A PUBLIC HEALTH GENETICS PLAN FOR PIAUI STATE WITH FOCUS ON LYSOSOMAL STORAGE DISORDERS 2.1 Introduction and Background 2.1.1 Healthcare in Brazil Brazil is the fifth most populous country in the world, and the sixth biggest world economy by nominal GDP, according to the United Nations. According to the World Bank, Brazil’s gross national income per capita is 11,420 USD, (compared to 48,820 USD in the United States) which categorizes Brazil as an upper middle-income country by the World Bank. In spite of the recent economic growth, the country’s development indicators still classify it as a developing economy according to the International Monetary Fund. [82, 83] Provision of public health care in Brazil is considered a right to all citizens and a responsibility and obligation of the State, being provided in public institutions free of charge. The national health policy had its principles and directives set by the Constitution of 1988, which established the Brazilian Unified Health System (in Portuguese, SUS). Although private hospitals and private health insurances are available in the country, according to the National Health Agency, 74.9 percent of the Brazilian population rely only on SUS to receive medical care. [84, 85] Some of the difficulties faced by the population in regard to public healthcare services in Brazil include: lack of access to services in remote areas 23 due to scarce number of healthcare professionals, delays in obtaining medical appointments with specialists, lower number of beds than the demand in tertiary care hospitals, especially at Intensive Care Units and significant overcrowding of Emergency Care Units. [86] In 1998, the Brazilian National Health Council approved a National Drug Policy Act that aims to promote access to and rational use of medicines that are considered essential. The National Drug Policy Act sets which drugs classify as essential, as well as the standards for policies and regulation in drug discovery, clinical trials and drug approval in the country. The act assigns individual states the responsibility of promoting access to medications that are considered exceptional, which are medicines that are the standard of care for a condition but constitute an economic burden to individual patients. [87] 2.1.2 Piauí State Demographics Piauí State is composed of 224 counties and covers an area of 251,577.738 square kilometers (equivalent to 97,134.7 square miles) with a density of 32.1 persons per square mile. According to the Brazilian Institute of Statistics and Geography (IBGE) demographic census, the 2010 population for Piauí State was 3,118,360. The economy is primarily based on the teritary sector (services), industry (chemical and textile), agriculture (soybean, cotton, rice, sugar cane, and cassava) and free-range livestock farming. Teresina is the capital of the state and the most populous city. Other major cities include Parnaíba, Picos, Piripiri and Floriano.[88] 24 Piauí state has the lowest gross state domestic product in Brazil. Data from 2009 show that the per capita gross state domestic product for Piaui was 6,051.10 Brazilian reais (BRL), which currently corresponds to 2,964.63 USD1. Data from 2003 by IBGE have shown that 53.11 percent of the population in Piaui state lives below poverty level taking into account the micro-level estimation of poverty and inequality by Elbers, Lanjouw and Lanjouw [89]. In 2010, median household income for Piauí state was 900 BRL per month, corresponding to a yearly income of 5,296.2 USD per household1. In rural areas of the state, the median monthly household income is 518 BRL (3,045.24 USD/year1). In 79.41 percent of the households in Piauí state, per capita income was less than minimal wage for Brazil, which was 510 BRL per month (2,987.52 USD/year) for the country in 2010. [88] The majority of the population (69 percent) is multi-ethnic, mainly due to miscegenation between individuals with European lineage and Amerindians (originating “caboclos”). Caucasians represent 24 percent of the population. Black individuals represent only seven percent of the population, mainly due to the economic activity during the colonization period, which did not favor African slavery.[88] According to IBGE in 2009 there were 2,093 healthcare units in Piaui state, 75.5 percent of which had public healthcare coverage through SUS. There are 3,125 registered physicians in the State, representing a physician density rate of ten physicians for each 10,000 people. 83.1 percent of the households 1 Convertion based on exchange rate data obtained on 01/02/2013, 1 BRL = 0.49 USD. Provided by Citibank N/A. 25 rely on the state for healthcare, and only 12.6 percent of state population has some sort of private health insurance. [88] 2.1.3 Piauí State Health Department According to the Brazilian National Health Council, the following actions constitute duties of Brazilian State Health Departments, according to the Basic Operational Norms of the Brazilian Unified Health System (published in the Official Gazette on 11/06/1996) [90]: - Planning and implementation of a State Health Plan containing strategies, priorities and goals of actions and services, including the integration of plans of the several county health departments; - Structuring and operation of the state component of the National Audit Office; - Structuring and operation of epidemiological data processing systems for delivery of services and for critical inputs; - Structuring and operation of epidemiological surveillance systems, including also health surveillance and monitoring food and nutrition; - Structuring and operation of human resources and of science and technology; - Elaboration of the state component of nationwide public health programs for health threats that have a risk of spreading beyond its territorial boundary; - Elaboration of the state component of the network of public health laboratories; 26 - Structuring and operation of the state component of pharmaceutical care; - State responsibility regarding the provision of outpatient and hospital services of high cost, treatment away from home and the availability of exceptional medicines and supplies; - Setting and operating policies regarding the use of blood and blood components, - Hiring and support of qualified permanent technical staff, able to fully accomplish the duties of the state health department; - Implementation of mechanisms to integrate the policies and actions of relevance to the health of the population; examples of which are those related to sanitation, water, housing and environmental health. The Piauí State Health Department stated mission is to coordinate and implement the operations of the National Health System in the State in order to ensure increased and timely access to healthcare services and appropriate and humanized care in the context of health promotion, prevention and recovery, as well as to ensure quality management of local health departments, aiming to improve health indicators and quality of life of the state population.[91] The Piauí State Health Department stated values include [91]: - Assurance of universality, thoroughness, equity and accessibility to healthcare services and actions, humanization and commitment; 27 with continuity, responsibility, - Exercise of participatory management, fostering transversality of health policies, programs, actions and services and strengthening the social Participation. 2.1.4 Genetics in Brazil Genetic diseases and birth defects are currently the second most common cause of infant mortality in Brazil. As health indicators consistent with developing countries have significantly improved in the last few years, the country has observed a drastic decrease in infant morbidity and mortality related to poor sanitary conditions, malnutrition and infectious diseases. Therefore, genetic diseases arose as a significant public health issue in the country. [86] Genetics as a medical specialty is still considerably young in the country. The first Medical Genetics residency was established in 1977 at Hospital das Clínicas de Ribeirão Preto, University of São Paulo. In 1983, the Brazilian Federal Council of Medicine recognized Medical Genetics as a medical specialty. Currently, there are 11 Medical Genetics residency programs in Brazil, offering a total of 21 new positions per year. There are no genetic counseling programs in the country, and medical geneticists perform this role. However, there are only 121 medical geneticists in Brazil, 85 percent of which are concentrated in the South and South East regions. [86] Dr Raskin, president of the Brazilian Society of Medical Genetics, estimates that the waiting time for a first time appointment in medical genetics in the country can be as long as one year. [92] In October of 2004 the Brazilian Ministry of Health established a workgroup in Clinical Genetics, which was responsible to plan and implement a 28 National Public Health Policy in Clinical Genetics and to incorporate genetics within the Brazilian public health system, which became effective in 2009. [93, 94] 2.1.4.1 Newborn Screening in Brazil On June 6th 2001, the Brazilian Ministry of Health implemented the National Newborn Screening Program, through the act GM/MS n. 822. The specific aims of the program included [95]: - Detection of metabolic conditions in a pre-symptomatic stage; - Coverage of 100 percent of live newborns; - Active search of screened newborns in the case of a positive initial result; - Diagnostic confirmation, as well as follow-up and appropriate early intervention measures of all identified newborns, in order to minimize their morbidity and mortality. In order to select which conditions should be screened for, the Brazilian Ministry of Health considered the need to select conditions that could be screened and managed taking into account the health system diversity throughout the country. Conditions that could be diagnosed early in their course, through screening tests with high sensitivity and confirmatory tests with high specificity should be priority. Additionally conditions should have an economically feasible and cost-effective available treatment that positively interferes with the disease natural history. [96] 29 The Ministry of Health also established that the program should be carried out and articulated in a partnership with the State Health Departments. Consequently, at least one Newborn Screening Reference Center was implemented in each of the 27 states in Brazil. These centers are responsible for coordinating the local networks of newborn screening present in each state and are composed of a multi-disciplinary team for medical care, composed of physicians, dietitians, psychologists, and social workers. As different states presented different healthcare system organizations, the Ministry of Health felt the need to implement the national program in phases. Consequently, the following phases of operation were established [96]: ● Phase I: screening, confirmatory tests, follow-up and management of PKU and congenital hypothyroidism; ● Phase II: screening, confirmatory tests, follow-up and management of PKU, congenital hypothyroidism, sickle cell disease and other hemoglobinopathies. ● Phase III: screening, confirmatory tests, follow-up and management of PKU, congenital hypothyroidism, sickle cell disease and other hemoglobinopathies and cystic fibrosis. Private laboratories also provide newborn screening, however, these are not integrated into a public health program, thus lacking the coordinated structure for follow-up and management of newborns with positive screening tests. There are three different groups of screening tests: basic, plus and master. The basic screening comprises the conditions covered by the phase III of the National 30 Newborn Screening Program, the plus performs screening for ten conditions while the master performs screening of 46 conditions. Health insurance reimbursement policies are not uniform. The cost of the screening for phase I is approximately 7.50 US dollars per sample, while for phases II and III cost 12 USD and 20 USD per sample, respectively. For confirmatory exams, the cost can vary from 15 to 40 USD per sample. [96] The cost to the parents for the master screening in case of non-coverage by private health insurance is about 120 USD. In 2005, through the act 6197/05, the screening for biotinidase deficiency was also introduced in the public health system. [97] However, the screening for this condition, although established by law, has not yet been introduced in most of the states in Brazil. The Newborn screening program in Brazil has still suboptimal achievements. Only three out of 27 states have achieved phase III program, which allows screening for only four conditions. Newborn screening coverage varies from 52.41 to 100 percent, with an average of 78.92 percent for the year of 2007. In the same year, for 3,035,096 live-births and approximately 2,400,000 screened newborns, 108 cases of PKU were detected, 1,231 cases of congenital hypothyroidism, 1,140 cases of hemoglobinopathies and 58 cases of cystic fibrosis, totalizing 2,537 cases. Data from 2007 also showed that 16,408 children and adults have been followed so far after a diagnosis was received through the newborn screening program, but those values can be underestimate since they represent only results from the governmental funded healthcare and no integrative effort exist with private newborn screening. [98] 31 2.1.4.2 Current Genetics Services in Piauí State According to the Brazilian Society of Medical Genetics, currently there no medical geneticists or clinical genetics laboratories are presented in Piaui State. [99] The genetic-related resources available in Piauí State are the following: - Hospital Infantil Lucidio Portela (Lucidio Portela Children’s Hospital), located in Teresina, serves as the Newborn Screening Reference Center for the State and is overseen by the State Office for Healthcare for Individuals with Disabilities (CAPD). - Central Laboratory of Piauí State (LACEN) located in Teresina, is the only laboratory responsible for running the laboratory tests for the State Newborn screening program, and is overseen by the State Office for Healthcare for Individuals with Disabilities (CAPD). A comprehensive list of not-for-profit organizations in the state that provide care and services to people with mental and physical disabilities, including those with hereditary causes, can be seen in Appendix B. 2.1.4.3 Lysosomal Storage Disorders in Brazil and Piauí State The exact prevalence of LSDs in Brazil and Piauí State are not known due to the lack of an integrated epidemiological surveillance service for genetic diseases in the country. Gaucher disease, the most prevalent LSD, affects more than 600 individuals in Brazil according to the Brazilian Gaucher Disease Patient Association. [100] 32 Several individual states, through resolution by the Brazilian Ministry of Health, have included imiglucerase, one of the treatment options of ERT for Gaucher disease, in the list of treatments covered by the Brazilian Unified Health System, which ensures treatment for this condition without any additional cost to the patients and their families. Some individual states, such as Sao Paulo State, have set up guidelines for indications of therapy and follow-up evaluations and tests for patients with the disease. In case of no appropriate follow-up insignificant clinical response to the medication, the patient undergoes additional evaluation prior to continue with therapy, in an attempt to optimize the treatment since the cost is considerable for Brazilian’s public health system. [101, 102] At present, treatments for other LSDs have not been included in the list of covered “exceptional drugs”. Besides Gaucher disease, specific treatment through either ERT or substrate reduction therapy (SRT) is available for Fabry disease, Mucopolysaccharidosis type I, Mucopolysaccharidosis type II, Mucopolysaccharidosis type IV, Pompe Disease and Niemann-Pick disease type C in developed countries. [103] Some of the diagnosed patients have been seeking access to these treatments through legal measures. According to the Fabry Registry 2007 Annual Report, age of diagnosis for Fabry patients in Brazil averages 53 years old in males and 70 years old in females, which represents an extremely high frequency of late diagnosis of the disease in the country.[104] Screenings for Fabry disease were performed in high-risk populations in Brazil in some individual states, with special focus on individuals with end-stage 33 renal disease of undetermined cause. [105, 106] In Piauí State, screening among 350 male hemodialysis patients resulted in diagnosis of Fabry disease in two individuals. The age of the patients was 57 and 74 years, and the first signs and symptoms of Fabry disease started decades prior to the diagnosis. One of the individuals had a classic form of Fabry disease and died due to a massive myocardial infarction several days after receiving the diagnosis of Fabry disease. A diagnosis of Fabry disease was not suspected in any of the individuals [107] Further family screening in one of the individuals resulted in diagnosis of Fabry disease in additional 61 individuals, the majority of them living in a remote village in the South of Piaui State with scarce access to medical care [unpublished data from the author]. 2.2 Needs Assessment and Development of a Public Health Genetics State Plan in Lysosomal Storage Disorders 2.2.1 Mission Our mission is to improve health and quality of life of individuals with LSDs living in Piaui State, an underprivileged state in Brazil, by developing the needed infrastructure for proper clinical management and prompt diagnosis of patients with LSD, delivering state-of-the-art medical care, and by educating physicians and the public in genetics and LSDs. 2.2.2 Assumptions - A significant delay of diagnosis and marked underdiagnosis of LSDs occur in Piaui State, resulting in preventable morbidity and mortality; 34 - This delay in diagnosis occurs in part due to: o Lack of awareness of LSDs among healthcare professionals and of proper training of primary care physicians and specialists in recognizing disease phenotypes that could be compatible with LSDs. o Lack of genetics laboratory and clinic for diagnosis and management of patients with LSDs o 2.2.3 Needs Assessment Some of the following facts were observed by analyzing the current healthcare situation in Piauí State and in Brazil, with focus on the provision of genetics services, especially the ones with direct or indirect impact in delivery of medical care for patients with LSDs: - Lack of coordinated national genetics infrastructure - Lack of genetics infrastructure in the State, - Although some genetics-related activities take place in Piauí state, there is no centralized state genetics department or program. - Genetics expertise among healthcare providers is insufficient to meet patients’ needs. - Lack of effective public policies in genetics that take place uniformly across the country, including appropriate coverage by public or private health insurances for diagnostic and follow-up tests, medical appointments 35 and genetic counseling, as well as for treatment of genetic disorders, when indicated. A thorough needs assessment will be performed through focus group interviews involving healthcare professionals, social workers, patients with LSD and their family members. Additionally, surveys disseminated to physicians of different specialties will be conducted prior to the implementation of the plan and after its establishment, and these resources will be used to guide program planning and implementation. 2.2.4 Goals, Objectives and Activities: 2.2.4.1 Goal 1 - Build the public health infrastructure needed to diagnose and provide appropriate clinical care to individuals with LSDs in Piauí State, Brazil - Objective 1.1: Engage key stakeholders o Some of the foreseen stakeholders for the development of a LSD program in Piauí State include: patients with LSDs and their families, healthcare professionals, hospitals, clinical laboratories, schools of Medicine, Piauí State Medical Council, Piauí State Health Department, Brazilian Ministry of Health, health insurance companies and SUS (Unified Healthcare System). - Objective 1.2: Build State Capacity and Self-Efficacy o Workforce: recruit and train staff and volunteers 36 o Seek for short and long-term funding for program staff and activities o Ensure quality and sustainability of LSD genetics services Consult with LSD experts to set standards of care Consult with policy makers o Establish and coordinate partnerships Partner with existing public clinical laboratory in establishing the required equipment and supplies for running diagnostic and follow-up tests for the different LSDs. Partner with reference university hospital for creating and establishing a LSD medical genetics clinic and a program office o Reimbursement and coverage – Seek for implementation of the legislation that regulates the coverage of genetics services by both public and private healthcare systems. o Promote universal access for those in need Establish regular outreach clinic in key cities of the state Facilitate scheduling of medical appointments through the use of a 1-800 hotline and online appointments - Objective 1.3: Surveillance 37 o Obtain data from the laboratories that perform clinical diagnosis of LSDs in Brazil to estimate data on the current prevalence of the disease in Piauí State. o Annually assess incidence data for LSDs in Piauí State by number of individuals diagnosed with LSD in Piauí State both through and outside the program, as well as monitor health outcomes for individuals being followed through the program. o Maintain accessible epidemiological data in the program website 2.2.4.2 Goal 2: Increase awareness and foster knowledge in the field of LSD among healthcare professionals and priority populations in Piaui State, Brazil - Objective 2.1: Educate physicians o Develop and maintain a program website, where we will maintain up-to-date information on recommendations and guidelines in diagnosis, follow-up and treatment of patients with LSD. o Deliver talks in medical conferences and meetings - Objective 2.2: Educate medical and allied health sciences students o Deliver talks as part of the current academic curriculum of the schools 38 o Discuss with course directors the need of the introduction of a Medical Genetics course or of improvement of the syllabus in the curriculum of Schools of Medicine. - Objective 2.3: Educate laboratory personnel in technical performance of LSD diagnostic and follow-up tests o Provide workshops to laboratory personnel in biochemical and molecular approaches for the diagnosis of LSDs - Objective 2.4: Educate patients and family members o Provide culturally appropriate learning material in the disease o Provide genetic counseling o 2.2.4.3 Goal 3: Reduce mortality and morbidity from LSDs in Piauí State - Objective 3.1: improve access to genetics services o Establish the first genetics clinics with focus on LSD in Piauí State - Objective 3.2: promote early and appropriate diagnosis of LSDs o Establish a Biochemical and Molecular Genetics Laboratory with focus on LSDs - Objective 3.3: promote use of up-to-date evidence-based medical practice in the management of LSDs. 2.2.5 Program Development Strategy Figure 7 represents a diagram with a summary of the planned strategy for the development phase of the LSD program in Piauí State. 39 Formation of working group Determination of Program Strategy Stakeholders and Needs Assessment Program logic and evaluation plan Seek funding Medical Talks on LSD Establishment of Genetics laboratory Establishment of Genetics clinic Figure 7. Strategy for the Program Development phase of a Public Health Genetics Plan for Piauí State with Focus on LSDs. Adapted from [108] 2.2.6 Evaluation plan We will perform both process and outcome evaluations throughout the establishment of the program, in the following issues: relevance/needs assessment of LSDs in the State, design and delivery of the program and success of the program and its activities. Some of the evaluation questions to be addressed, as well as the indicators and data sources that will be utilized in the evaluation plan are described bellow. Evaluation issues: 1. Relevance/Needs assessment a. What is the magnitude of LSDs in Piaui State? 40 i. We will investigate along with the only two clinical laboratories that perform diagnostic tests in LSD in Brazil the actual number of individuals diagnosed with LSDs in the past ten years. b. Is the current prevalence along with what is expected based in worldwide prevalence data? i. Based on reported data of incidence for the different LSDs, we will compare obtained prevalence with expected prevalence for LSDs based on reports from other populations. c. What is the existing laboratory structure for running LSDs diagnosis and follow-up tests in Piaui State? i. In consultancy with experienced Biochemical and Molecular Genetics Laboratory directors, we will determine the current structure and what are the needs in terms of equipment, supplies and specialized training for running diagnostic and follow-up tests in LACEN, the reference laboratory for newborn screening in Piauí State. d. What is the current level of knowledge in LSDs among physicians and students in the health sciences? i. Prior to the delivery of medical conferences for healthcare professionals and students in the health sciences, we will administer pre-tests with general questions in genetics, 41 diagnosis and treatment of lysosomal storage disorders in order to obtain a baseline on the general knowledge among these professionals in regard to proper diagnosis and management of LSDs. ii. We will also administer pre-tests along with the surveys to physicians from different specialties during the needs assessment process. 2. Design and delivery a. Has the program changed awareness of relevance of LSDs? i. Immediately after the delivery of medical conferences for healthcare professionals and students in the health sciences, we will administer post-tests to evaluate the acquired knowledge in the field of LSD through our talks. If agreed, we will also contact the professionals by email one year after the participation in our talks and re-administer the post-test to these professionals in order to determine a longer-term assimilated knowledge. b. Does the program follow updated recommendations and guidelines for diagnosis, follow-up and treatment of LSDs? i. We will have external consultancy from LSD experts, which will evaluate the recommendations and guidelines found in our website, and will also observe and evaluate the activities 42 of the clinic during one week a year to ensure delivery of updated medical care. c. Is the program integrated to healthcare systems and adequate to reality and community needs? i. We will evaluate the incorporation of the genetic clinic into the health system of the state based on the number of referrals from different medical specialties and also evaluate the number and quality of the outreach clinic services. d. Which improvements could be made to the program to better serve the community and healthcare professionals? i. We will perform periodic surveys among program staff, patients and family members and healthcare professionals and gather information on what could be improved in the delivery of care in LSD. 3. Success a. Were the expected outcomes achieved? i. We will annually assess and publically report: 1. Attendance rate to education sessions performed throughout the program 2. Pre- and post-test results applied before and after each education session 3. Number of screening and diagnosis tests run in the biochemical and molecular genetics laboratory 43 4. Number of referral visits to the Medical Genetics LSD clinic 5. Number of diagnosed individuals with LSDs 6. Health outcomes for individuals being followed through the program, with elaboration of periodic reports 2.2.7 Expected Outcomes and Impact Short-Term Outcomes: - Infra-structure for a Medical Genetics clinic and a Biochemical and Molecular Genetics Laboratory with focus on LSD - Increased awareness in the relevance of the field of LSDs among the medical community - Increased knowledge in current recommendations on the diagnosis and management of patients with LSDs among the medical community Medium-Term Outcomes: - Increased screening and diagnosis of patients with LSDs - Early diagnosis and intervention of patients with LSDs - Proper management of the comorbidities frequently found in patients with LSDs - Proper genetic counseling of patients with LSD and their family members at risk - Patient and family education on the disease 44 Long-Term Outcomes: - Decreased morbidity and mortality and increased quality of life of patients with manageable LSDs in Piauí State 2.2.8 Challenges Some of the foreseen challenges in the development and execution of a Public Health Genetics Plan with Focus on LSDs include: - Scarcity of public funding for program development and implementation in genetics in Brazil o We will also seek funding through public-private partnerships and apply for international grants, always optimizing the use of already existing resources in the state in order to reduce costs. - Scarcity of well-trained professionals in the field of LSD and genetics in general to compose the program staff o Healthcare professionals recruited for the program will be trained in a reference center in LSD prior to the start of the activities - Some of the remote areas of the State have difficult access (i.e. crumbling roads and highways) The outreach clinics will be planned ahead, allowing extra time for possible intercurrences. 3.0 Final Considerations and Future Directions In this study, we developed and fully characterized a cell model for Fabry disease, a Lysosomal Storage Disorder, in renal tubular epithelial cells. Further 45 studies that could be performed in these cells include proteomics and cell signaling arrays to investigate possible qualitative and quantitative changes in protein expression and signal transduction in renal tubular cells silenced for αGal A. We could also study intracellular events and function of specific organelles in the lieu of Fabry disease. As the methods become fully optimized and expertise becomes available, other cell models of interest could also be developed, especially from the main organs of involvement of the disease, such as cardiomyocytes for the study of cardiomyopathy and glial cells for the study of the CNS involvement. The effect of novel forms or SRTs or ERTs or manipulation of new pathways could also be studied in a high-throughput manner. Additionally, here we design the framework for a Public Health Genetics Plan for Piauí State, the lowest income state in Brazil, a developing country. We have discussed relevant background information, and important policy issues. We purpose a comprehensive program aiming to increase awareness and knowledge in the field, promptly diagnose and promote health and quality of life for individuals with LSD in Piauí State, including components of needs assessment and a robust evaluation plan. A Public Health Genetics Plan for Piauí State could serve as a pilot for implementation of similar programs in developing countries. 46 Appendix A – Lysosomal Storage disorders by subgroup Protein DEFECTS IN GLYCAN DEGRADATION Defects in glycoprotein degradation α-Sialidase Galactosialidosis α-Mannosidase β-Mannosidase Glycosylasparaginase α-Fucosidase α-N-Acetylglucosaminidase Defects in glycolipid degradation A. GM1 Ganglioside β-Galactosidase β-Hexosaminidase α-subunit β-Hexosaminidase β-subunit GM2 activator protein Glucocerebrosidase Saposin C B. Defects in the degradation of sulfatide Arylsulfatase A Saposin B Formyl-Glycin generating enzyme Disease Sialidosis Cathepsin A α-Mannosidosis β-Mannosidosis Aspartylglucosaminuria Fucosidosis Schindler GM1 gangliosidosis / MPS IVB GM2-gangliosidosis (Tay-Sachs) GM2-gangliosidosis (Sandhoff) GM2 gangliosidosis Gaucher disease Gaucher disease Metachromatic leukodystrophy Metachromatic leukodystrophy Multiple sulfatase deficiency 47 β-Galactosylceramidase (Krabbe) C. Defects in degradation of globotriaosylceramide α-Galactosidase A Defects in degradation of Glycosaminoglycan (Mucopolysaccharidoses) A. Degradation of heparan sulphate Iduronate sulfatase α-Iduronidase Heparan N-sulfatase Acetyl-CoA transferase N-acetyl glucosaminidase β-glucuronidase N-acetyl glucosamine 6-sulfatase Degradation of other mucopolysaccharides N-Acetylgalactosamine 4-sulfatase Galactose 6-sulfatase Hyaluronidase Defects in degradation of glycogen α-Glucosidase DEFECTS IN LIPID DEGRADATION Defects in degradation of sphingomyelin Acid sphingomyelinase Acid ceramidase Defects in degradation of triglycerides and cholesteryls ester Acid lipase DEFECTS IN PROTEIN DEGRADATION Cathepsin K Tripeptidyl peptidase Palmitoyl-protein thioesterase DEFECTS IN LYSOSOMAL TRANSPORTERS Cystinosin (cystin transport) Sialin (sialic acid transport) DEFECTS IN LYSOSOMAL TRAFFICKING PROTEINS UDP-N-acetylglucosamine Phosphotransferase γ-subunit Mucolipin-1(cation channel) LAMP-2 NPC1 CLN3 CLN 6 Globoid cell leukodystrophy Fabry MPS II (Hunter) MPS 1 (Hurler, Scheie) MPS IIIa (Sanfilippo A) MPS IIIc (Sanfilippo C) MPS IIIb (Sanfilippo B) MPS VII (Sly) MPS IIId (Sanfilippo D) MPS VI MPS IVA (Morquio A) MPS IX Pompe Niemann Pick type A and B Farber lipogranulomatosis Wolman and cholesteryl ester storage disease Pycnodystostosis Ceroide lipofuscinosis 2 Ceroide lipofuscinosis 1 Cystinosis Salla disease Mucolipidosis III (I-cell) Mucolipidosis IV Danon Niemann Pick type C Ceroid lipofuscinosis Ceroid lipofuscinosis 6 48 CLN 8 LYST MYOV RAB27A Melanophilin AP3 β-subunit Ceroid lipofuscinosis 8 Chediak-Higashi Griscelli Type 1 Griscelli Type 2 Griscelli Type 3 Hermansky Pudliak 2 Adapted from ref [109] Appendix B – Governmental and non-governmental organizations providing care for individuals with disabilities/special needs in Piauí state, Brazil.* Special need Autism Blindness Physical disability Intellectual disability Resource Associação de amigos dos autistas do Piauí Associação dos cegos do Piauí CAP - Centro de apoio pegagógico às pessoas portadoras de deficiência visual ASCEB - Núcleo Associação dos Cegos de Água Branca Associação dos deficientes físicos de Teresina City Teresina Teresina Teresina Sociedade de Apoio ao Deficiente Físico Associação dos Cadeirantes do Município de Teresina SADEFINP - Sociedade de Apoio ao Deficiente Físico do Norte do Piauí CIES - Centro integrado de educação especial Teresina Teresina Fundação Viver com digndade - Lar Renascer Pastoral da Esperança APAE - Centro de Recuperação e Profissionalização Integrado Cristina Leite CHAC - Centro de Habilitação Ana Cordeiro Instituto Panda - Núcleo de Apoio à Pessoa com Teresina 49 Água Branca Teresina Barras Teresina Teresina Teresina Teresina Deficiência/Paralisia Cerebral Associação Pestalozzi "Casa Odylo Costa Filho" Escola de Educação Especial Prof Cordão Deafness Others APADA - Associação de pais e amigos dos deficientes auditivos ASTE - Associação dos surdos de Teresina CAS - Centro de Apoio Pedagógico ao Surdo APAE - Escola de Educação Especial Prof Consuelo Pinheiro AMH - Associação de mielomeningocele e/ou hidrocefalia de Teresina AOSEPI - Associação dos ostomizados do Estado do Piauí FCD - Fraternidade Cristã de Doentes e Deficientes Pastoral da Amizade CEPI - Centro de Profissionalização Integrado UEESPI - Unidade de Educação Especial PNES - Programa TEC NEP - Educação, tecnologia e profissionalização para pessoas com necessidades especiais SINE - Serviço Nacional de Empregos CONEDE-PI Conselho Estadual de Defesa dos Direitos da Pessoa com Deficiência CONEDE-TE Conselho Municipal de Defesa dos Direitos da Pessoa Com Deficiência FUNDECAP - Fundação dos Deficientes de Capitão de Campos CIEE- Centro de Integração Empresa Escola Núcleo de Reabilitação Profissional SEINT - Ministério do Trabalho e Emprego - Seção de Inspeção do Trabalho - Grupo Pro Igualdade Instituto Professor Magalhães IEDE - Instituto Educacional de Desenvolvimento Integrado Escola Viva Escola Castelinho Colégio Base Dez *Adapted from: http://www.seid.pi.gov.br/entidades.php 50 Teresina Campo Maior Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Capitão de Campos Teresina Teresina Teresina Teresina Teresina Teresina Teresina Teresina Bibliography 1. Bishop, D.F., et al., Human alpha-galactosidase A: nucleotide sequence of a cDNA clone encoding the mature enzyme. Proc Natl Acad Sci U S A, 1986. 83(13): p. 4859-63. 2. Desnick, R.J., Y.A. Ioannou, and C.M. Eng, eds. alpha-galactosidase A deficiency: Fabry disease. 8th ed. The Metabolic and Molecular Bases of Inherited Disease, ed. C.R. Scriver, et al.2001, McGraw-Hill: New York. 3733-3774. 3. Eng, C.M., et al., Fabry disease: baseline medical characteristics of a cohort of 1765 males and females in the Fabry Registry. Journal of inherited metabolic disease, 2007. 30(2): p. 184-92. 4. Waldek, S., et al., Life expectancy and cause of death in males and females with Fabry disease: findings from the Fabry Registry. Genetics in medicine : official journal of the American College of Medical Genetics, 2009. 11(11): p. 790-6. 5. Hopkin, R.J., et al., Characterization of Fabry disease in 352 pediatric patients in the Fabry Registry. Pediatr Res, 2008. 64(5): p. 550-5. 6. Ramaswami, U., et al., Fabry disease in children and response to enzyme replacement therapy: results from the Fabry Outcome Survey. Clin Genet, 2011. 51 7. Tondel, C., et al., Prominence of glomerular and vascular changes in renal biopsies in children and adolescents with Fabry disease and microalbuminuria. Clin Ther, 2008. 30 Suppl B: p. S42. 8. Zarate, Y.A. and R.J. Hopkin, Fabry's disease. Lancet, 2008. 372(9647): p. 1427-35. 9. Germain, D.P., Fabry disease. Orphanet J Rare Dis, 2010. 5: p. 30. 10. Hulkova, H., et al., [Postmortem diagnosis of Fabry disease in a female heterozygote leading to the detection of undiagnosed manifest disease in the family]. Cas Lek Cesk, 1999. 138(21): p. 660-4. 11. Ramaswami, U., et al., Assessment of renal pathology and dysfunction in children with Fabry disease. Clin J Am Soc Nephrol, 2010. 5(2): p. 365-70. 12. Fogo, A.B., et al., Scoring system for renal pathology in Fabry disease: report of the International Study Group of Fabry Nephropathy (ISGFN). Nephrol Dial Transplant, 2010. 25(7): p. 2168-77. 13. Cox, T.M. and J.P. Schofield, Gaucher's disease: clinical features and natural history. Bailliere's clinical haematology, 1997. 10(4): p. 657-89. 14. Fuller, M., P.J. Meikle, and J.J. Hopwood, Epidemiology of lysosomal storage diseases: an overview. 2006. 15. Poupetova, H., et al., The birth prevalence of lysosomal storage disorders in the Czech Republic: comparison with data in different populations. J Inherit Metab Dis, 2010. 33(4): p. 387-96. 16. Risch, N., et al., Geographic distribution of disease mutations in the Ashkenazi Jewish population supports genetic drift over selection. American journal of human genetics, 2003. 72(4): p. 812-22. 17. Cox, T.M. and M.B. Cachon-Gonzalez, The cellular pathology of lysosomal diseases. J Pathol, 2012. 226(2): p. 241-54. 18. Ballabio, A. and V. Gieselmann, Lysosomal disorders: from storage to cellular damage. Biochim Biophys Acta, 2009. 1793(4): p. 684-96. 19. Xu, Y.H., et al., Multi-system disorders of glycosphingolipid and ganglioside metabolism. Journal of lipid research, 2010. 51(7): p. 1643-75. 20. Meikle, P.J., et al., Prevalence of lysosomal storage disorders. JAMA, 1999. 281(3): p. 249-54. 52 21. Dajnoki, A., et al., Newborn screening for Fabry disease by measuring GLA activity using tandem mass spectrometry. Clin Chim Acta, 2010. 411(19-20): p. 1428-31. 22. Spacil, Z., et al., Comparative triplex tandem mass spectrometry assays of lysosomal enzyme activities in dried blood spots using fast liquid chromatography: application to newborn screening of Pompe, Fabry, and Hurler diseases. Anal Chem, 2011. 83(12): p. 4822-8. 23. Mechtler, T.P., et al., Neonatal screening for lysosomal storage disorders: feasibility and incidence from a nationwide study in Austria. Lancet, 2012. 379(9813): p. 335-41. 24. Spada, M., et al., High incidence of later-onset fabry disease revealed by newborn screening. Am J Hum Genet, 2006. 79(1): p. 31-40. 25. Chien, Y.H., et al., Fabry Disease: Incidence of the Common Later-Onset alpha Galactosidase A IVS4+919G>A Mutation in Taiwanese Newborns -- Superiority of DNA-Based to Enzyme-Based Newborn Screening for Common Mutations. Mol Med, 2012. 26. Ross, L.F., Newborn screening for lysosomal storage diseases: an ethical and policy analysis. Journal of inherited metabolic disease, 2012. 35(4): p. 627-34. 27. Giugliani, R., Newborn screening for lysosomal diseases: current status and potential interface with population medical genetics in Latin America. Journal of inherited metabolic disease, 2012. 35(5): p. 871-7. 28. Garman, S.C. and D.N. Garboczi, The molecular defect leading to Fabry disease: structure of human alpha-galactosidase. J Mol Biol, 2004. 337(2): p. 319-35. 29. Garman, S.C., Structure-function relationships in alpha-galactosidase A. Acta Paediatr Suppl, 2007. 96(455): p. 6-16. 30. Okuda, T., et al., Targeted disruption of Gb3/CD77 synthase gene resulted in the complete deletion of globo-series glycosphingolipids and loss of sensitivity to verotoxins. J Biol Chem, 2006. 281(15): p. 10230-5. 31. Dawson, G., A.W. Kruski, and A.M. Scanu, Distribution of glycosphingolipids in the serum lipoproteins of normal human subjects and patients with hypo- and hyperlipidemias. J Lipid Res, 1976. 17(2): p. 125-31. 32. Aerts, J.M., et al., Elevated globotriaosylsphingosine is a hallmark of Fabry disease. Proc Natl Acad Sci U S A, 2008. 105(8): p. 2812-7. 53 33. Warnier, M., et al., Trafficking of Shiga toxin/Shiga-like toxin-1 in human glomerular microvascular endothelial cells and human mesangial cells. Kidney Int, 2006. 70(12): p. 2085-91. 34. Nyholm, P.G., J.L. Brunton, and C.A. Lingwood, Modelling of the interaction of verotoxin-1 (VT1) with its glycolipid receptor, globotriaosylceramide (Gb3). Int J Biol Macromol, 1995. 17(3-4): p. 199-204. 35. Fantini, J., et al., Role of glycosphingolipid microdomains in CD4-dependent HIV-1 fusion. Glycoconj J, 2000. 17(3 -4): p. 199-204. 36. Puri, A., et al., Role of glycosphingolipids in HIV-1 entry: requirement of globotriosylceramide (Gb3) in CD4/CXCR4-dependent fusion. Biosci Rep, 1999. 19(4): p. 317-25. 37. Lund, N., et al., A novel soluble mimic of the glycolipid, globotriaosyl ceramide inhibits HIV infection. AIDS, 2006. 20(3): p. 333-43. 38. Gehrmann, M., et al., Tumor-specific Hsp70 plasma membrane localization is enabled by the glycosphingolipid Gb3. PLoS One, 2008. 3(4): p. e1925. 39. Maloney, M.D., B. Binnington-Boyd, and C.A. Lingwood, Globotriaosyl ceramide modulates interferon-alpha-induced growth inhibition and CD19 expression in Burkitt's lymphoma cells. Glycoconj J, 1999. 16(12): p. 821-8. 40. George, T., et al., MHC class II proteins contain a potential binding site for the verotoxin receptor glycolipid CD77. Cell Mol Biol (Noisy-le-grand), 2001. 47(7): p. 1179-85. 41. Ghislain, J., C.A. Lingwood, and E.N. Fish, Evidence for glycosphingolipid modification of the type 1 IFN receptor. J Immunol, 1994. 153(8): p. 3655-63. 42. Liu, Y.Y., et al., Glucosylceramide synthase upregulates MDR1 expression in the regulation of cancer drug resistance through cSrc and beta-catenin signaling. Mol Cancer, 2010. 9: p. 145. 43. Harzer, K. and B. Kustermann-Kuhn, Quantified increases of cholesterol, total lipid and globotriaosylceramide in filipin-positive Niemann-Pick type C fibroblasts. Clin Chim Acta, 2001. 305(1-2): p. 65-73. 44. Kovbasnjuk, O., et al., The glycosphingolipid globotriaosylceramide in the metastatic transformation of colon cancer. Proc Natl Acad Sci U S A, 2005. 102(52): p. 19087-92. 45. De Rosa, M.F., et al., Inhibition of multidrug resistance by adamantylgb3, a globotriaosylceramide analog. J Biol Chem, 2008. 283(8): p. 4501-11. 54 46. Van de Kar, N.C., L.A. Monnens, and V.W. Van Hinsbergh, Tumor necrosis factor and interleukin 1 induce expression of the glycolipid verotoxin receptor in human endothelial cells. Implications for the pathogenesis of the haemolytic uraemic syndrome. Behring Inst Mitt, 1993(92): p. 202-9. 47. Eisenhauer, P.B., et al., Tumor necrosis factor alpha increases human cerebral endothelial cell Gb3 and sensitivity to Shiga toxin. Infect Immun, 2001. 69(3): p. 1889-94. 48. Lidove, O., et al., Fabry disease 'The New Great Imposter': results of the French Observatoire in Internal Medicine Departments (FIMeD). Clin Genet, 2011. 49. Wilcox, W.R., et al., Females with Fabry disease frequently have major organ involvement: lessons from the Fabry Registry. Mol Genet Metab, 2008. 93(2): p. 112-28. 50. Martins, A.M., et al., Guidelines to diagnosis and monitoring of Fabry disease and review of treatment experiences. The Journal of pediatrics, 2009. 155(4 Suppl): p. S19-31. 51. Wallin, E.F., M.R. Clatworthy, and N.R. Pritchard, Fabry disease: results of the first UK hemodialysis screening study. Clin Nephrol, 2011. 75(6): p. 506-10. 52. Elliott, P., et al., Prevalence of Anderson-Fabry disease in patients with hypertrophic cardiomyopathy: the European Anderson-Fabry Disease survey. Heart, 2011. 97(23): p. 1957-60. 53. Hagege, A.A., et al., Screening patients with hypertrophic cardiomyopathy for Fabry disease using a filter-paper test: the FOCUS study. Heart, 2011. 97(2): p. 131-6. 54. Baptista, M.V., et al., Mutations of the GLA gene in young patients with stroke: the PORTYSTROKE study--screening genetic conditions in Portuguese young stroke patients. Stroke, 2010. 41(3): p. 431-6. 55. Branton, M.H., et al., Natural history of Fabry renal disease: influence of alphagalactosidase A activity and genetic mutations on clinical course. Medicine, 2002. 81(2): p. 122-38. 56. Beck, M., Agalsidase alfa--a preparation for enzyme replacement therapy in Anderson-Fabry disease. Expert Opin Investig Drugs, 2002. 11(6): p. 851-8. 57. Wilcox, W.R., et al., Long-term safety and efficacy of enzyme replacement therapy for Fabry disease. Am J Hum Genet, 2004. 75(1): p. 65-74. 55 58. Lee, K., et al., A biochemical and pharmacological comparison of enzyme replacement therapies for the glycolipid storage disorder Fabry disease. Glycobiology, 2003. 13(4): p. 305-13. 59. Clarke, J.T., et al., The pharmacology of multiple regimens of agalsidase alfa enzyme replacement therapy for Fabry disease. Genet Med, 2007. 9(8): p. 5049. 60. Caballero, L., et al., Enzyme replacement therapy in Fabry disease: influence on cardiac manifestations. Curr Med Chem, 2010. 17(16): p. 1679-89. 61. Ramaswami, U., Update on role of agalsidase alfa in management of Fabry disease. Drug Des Devel Ther, 2011. 5: p. 155-73. 62. Watt, T., et al., Agalsidase beta treatment is associated with improved quality of life in patients with Fabry disease: findings from the Fabry Registry. Genet Med, 2010. 12(11): p. 703-12. 63. Feriozzi, S., et al., The Effectiveness of Long-Term Agalsidase Alfa Therapy in the Treatment of Fabry Nephropathy. Clin J Am Soc Nephrol, 2012. 7(1): p. 6069. 64. Warnock, D.G., et al., Renal outcomes of agalsidase beta treatment for Fabry disease: role of proteinuria and timing of treatment initiation. Nephrol Dial Transplant, 2011. 65. Buechner, S., et al., Central nervous system involvement in Anderson-Fabry disease: a clinical and MRI retrospective study. J Neurol Neurosurg Psychiatry, 2008. 79(11): p. 1249-54. 66. Germain, D.P., et al., Safety and pharmacodynamic effects of a pharmacological chaperone on alpha-galactosidase A activity and globotriaosylceramide clearance in Fabry disease: report from two phase 2 clinical studies. Orphanet journal of rare diseases, 2012. 7: p. 91. 67. Benjamin, E.R., et al., The pharmacological chaperone 1deoxygalactonojirimycin increases alpha-galactosidase A levels in Fabry patient cell lines. J Inherit Metab Dis, 2009. 32(3): p. 424-40. 68. Protalix-Biotherapeutics. PRX-102. Available from: http://www.protalix.com/product-development/prx-102.asp. Accessed on 01/03/2013. 69. Ohshima, T., et al., alpha-Galactosidase A deficient mice: a model of Fabry disease. Proc Natl Acad Sci U S A, 1997. 94(6): p. 2540-4. 56 70. Eitzman, D.T., et al., Fabry disease in mice is associated with age-dependent susceptibility to vascular thrombosis. Journal of the American Society of Nephrology : JASN, 2003. 14(2): p. 298-302. 71. Ohshima, T., et al., Aging accentuates and bone marrow transplantation ameliorates metabolic defects in Fabry disease mice. Proceedings of the National Academy of Sciences of the United States of America, 1999. 96(11): p. 6423-7. 72. Bartz, S. and A.L. Jackson, How will RNAi facilitate drug development? Science's STKE : signal transduction knowledge environment, 2005. 2005(295): p. pe39. 73. Simmons, N.L., Cultured monolayers of MDCK cells: a novel model system for the study of epithelial development and function. Gen Pharmacol, 1982. 13(4): p. 287-91. 74. Ortiz, A., et al., Recommendations and guidelines for the diagnosis and treatment of Fabry nephropathy in adults. Nature clinical practice. Nephrology, 2008. 4(6): p. 327-36. 75. Mather, A.R. and L.J. Siskind, Glycosphingolipids and kidney disease. Adv Exp Med Biol, 2011. 721: p. 121-38. 76. Lesage, S., et al., Large-scale screening of the Gaucher's disease-related glucocerebrosidase gene in Europeans with Parkinson's disease. Hum Mol Genet, 2011. 20(1): p. 202-10. 77. Mattila, P.E., et al., Multiple Biosynthetic Trafficking Routes for Apically Secreted Proteins in MDCK Cells. Traffic, 2012. 13(3): p. 433-42. 78. Fischer, E.G., M.J. Moore, and D.J. Lager, Fabry disease: a morphologic study of 11 cases. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc, 2006. 19(10): p. 1295-301. 79. Thurberg, B.L., et al., Cardiac microvascular pathology in Fabry disease: evaluation of endomyocardial biopsies before and after enzyme replacement therapy. Circulation, 2009. 119(19): p. 2561-7. 80. Sindhu, A., P. Arora, and A. Chaudhury, Illuminating the gateway of gene silencing: perspective of RNA interference technology in clinical therapeutics. Molecular biotechnology, 2012. 51(3): p. 289-302. 81. Ostrander, E.A. and R.K. Wayne, The canine genome. Genome research, 2005. 15(12): p. 1706-16. 57 82. World-dataBank. World Development indicators. Available from: http://databank.worldbank.org/ddp/home.do. Accessed on 01/05/2013. 83. Nielsen, L. International Monetary Fund. Classifications of Countries Based on Their Level of Development: How it is Doen and How it Could be Done. . Available from: : http://www.imf.org/external/pubs/ft/wp/2011/wp1131.pdf. Accessed on 01/05/2013. 84. ANS. Agência Nacional de Saúde Complementar - Dados Gerais. 2012; Available from: http://www.ans.gov.br/index.php/materiais-parapesquisas/perfil-do-setor/dados-gerais. Accessed on 01/06/2013. 85. Saúde, M.d. Lei n 8.080 - Lei Orgânica da Saúde. 1990; Available from: http://portal.saude.gov.br/portal/arquivos/pdf/lei8080.pdf. Accessed on 01/07/2013. 86. Melo, D.G. and J. Sequeiros, The challenges of incorporating genetic testing in the unified national health system in Brazil. Genetic testing and molecular biomarkers, 2012. 16(7): p. 651-5. 87. Saúde, M.d. Portaria MS n. 3.916 - Política Nacional de Medicamentos. 1998; Available from: http://pfdc.pgr.mpf.gov.br/atuacao-e-conteudos-deapoio/legislacao/saude/portarias/portaria_MS_3.916.1998. Accessed on 01/07/2013. 88. Estatística, I.B.d.G.e. Censo Demográfico. Estados: Piauí. 2010; Available from: http://www.ibge.gov.br/estadosat/perfil.php?sigla=pi. Accessed on 01/07/2013. 89. Elbers, C.L., J.O.; Lanjouw, P., Micro-level Estimation of Poverty and Inequality. Econometrica, 2002. 71(1): p. 355-364. 90. Saúde, C.N.D. Norma Operacional Básica do Sistema Único de Saúde - SUS. 1996; Available from: http://conselho.saude.gov.br/legislacao/nobsus96.htm - 6. Accessed on 01/03/2013. 91. Piauí, S.d.E.d.S.d. Portal da Saúde: Missão e Valores. 2012; Available from: http://www.saude.pi.gov.br/paginas/37-missao-e-valores. Accessed on 01/04/2013. 92. Raskin, S. Raras e Subdiagnosticadas: Um Dia para as Raras (para a Associação Brasileira de Pacientes Portadores de Doença de Fabry e Seus Familiares). 2010; Available from: http://www.fabry.org.br/noticiasimprensa-integra.php?cd=13. Accessed on 01/04/2013. 58 93. Saúde, M.d. Portaria n. 2.380/GM - Grupo de Trabalho de Genética Clínica. 2004; Available from: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2004/GM/GM-2380.htm. Accesssed on 01/05/2013. 94. Saúde, M.d. Portaria n. 81- Política Nacional de Atenção Integral em Genética Clínica. 2009; Available from: http://portal.saude.gov.br/portal/saude/Gestor/visualizar_texto.cfm?idtxt=3 0616. Accessed on 01/03/2013. 95. Carvalho, T.M. Histórico do Programa Nacional de Triagem Neonatal Apresentação. Sociedade Brasileira de Triagem Neonatal. Available from: http://www.sbtn.org.br/pg_historico_apresentacao.htm. Accessed on 01/05/2013. 96. Ambulatorial, S.d.A.à.S.C.-G.d.M.C., Manual de Normas Técnicas e Rotinas Operacionais do Programa de Triagem Neonatal2003, Brasília, DF: Ministério da Saúde. 97. Jurídica, C. Teste do Pezinho pode trazer mais um diagnóstico. 2006; Available from: http://www.centraljuridica.com/click.php?mid=3377. Accessed on 01/05/2013. 98. Saúde, M.d. Indicadores do Programa Nacional de Triagem Neonatal. 2008; Available from: http://portal.saude.gov.br/portal/arquivos/pdf/INDICADORES_TRIAGEM_ NEONATAL.pdf. Accessed on 01/05/2013. 99. Sociedade Brasileira de Genética Médica. http://www.sbgm.org.br/. Accessed on 01/05/2013. 100. Martins, A.M., et al., Recommendations on diagnosis, treatment, and monitoring for Gaucher disease. The Journal of pediatrics, 2009. 155(4 Suppl): p. S10-8. 101. Secretaria de Saúde do Estado de Mato Grosso do Sul - Portaria n. 1.318/GM. 2002; Available from: http://pfdc.pgr.mpf.gov.br/atuacao-e-conteudos-deapoio/legislacao/saude/portarias/portaria_MS_1318.2002. Accessed on 01/06/2013. 102. Saúde, M.d. Secretaria de Assistência a Saúde do Estado de São Paulo. Protocolos Clínicos e Diretrizes Terapêuticas. Medicamentos Excepcionais. Doença de Gaucher. . 2002; Available from: http://dtr2001.saude.gov.br/sas/dsra/protocolos/do_d11_00.htm. Accessed on 01/06/2013. 59 Available from: 103. Wyatt, K., et al., The effectiveness and cost-effectiveness of enzyme and substrate replacement therapies: a longitudinal cohort study of people with lysosomal storage disorders. Health technology assessment, 2012. 16(39): p. 1-543. 104. Genzyme. Fabry RADAR 2007: The Fabry Registry Aggregate Data Annual Report. 2007; Available from: http://www.fabry.org/fsig.nsf/PDFs/PDFsR/$File/2007_RADAR.pdf. Accessed on 01/03/2013. 105. Marinho, L.A.L.R., J.F.M.; Oliveira, T.C.; Sabóia, T.M. , Prevalência da doença de fabry em pacientes portadores de doençarenal crônica submetidos à hemodiálise em Natal – RN / Prevalence of fabry disease in patients with chronic kidney disease onhemodialysis in Natal – RN, Brazil. J Bras Nefrol, 2007. 29(4): p. 235-238. 106. Porsch, D.B., Doença de Fabry em Pacientes Submetidos à Hemodiálise no Rio Grande do Sul: Estudo de Prevalência e Relato Clínico, in Medicine2008, Universidade Federal do Piauí: Porto Alegre. 107. Vale, N.F.D.S., A.B.R.; Veras, A.B.; Monteiro, F.M.R.; Sousa, J.L.M.; Bezerra, V.L.; Martins, A.M.; D'Almeida, V.; Castro, J.A.F.; Monte Neto, J.T.; Melo, A.P.R.; Monte, S.J.H., Diagnosis of Fabry disease in Subjects on Hemodialysis in Piauí State: Role of Screening and Case Studies. . J Bras Nefrol, 2008. 30(4): p. 25963. 108. Gaff, C.L., et al., A model for the development of genetics education programs for health professionals. Genetics in medicine : official journal of the American College of Medical Genetics, 2007. 9(7): p. 451-7. 109. Greiner-Tollersrud, O.K.B., T., Lysosomal Storage Disorders, in Madame Curie Bioscience Database [Internet]2000, Landes Bioscience: Austin (TX). 60