Thrombocytopenia in neonates Adapted from a presentation by Bronwyn Waddell, MS 4
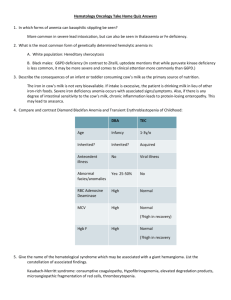
advertisement

Thrombocytopenia in neonates Adapted from a presentation by Bronwyn Waddell, MS 4 NICU Sub-internship 9-17-04 Definition Thrombocytopenia < 150,000/µL (150 x 109/L) – Rare in general population (<1%); 22% in NICU – Many healthy newborns b/w 100,000 150,000/µL. – Average platelet counts lower in preterm infants • Reflects increase during gestation, from 187,000 to 274,000/µL at 15 and 40 weeks – Severe reductions (<50,000/µL) and/or persistent thrombocytopenia can result in bleeding. – Severe and/or persistent thrombocytopenia requires evaluation, even in an asymptomatic infant. Evaluation of the thrombocytopenic neonate Based on recognizing typical patterns – 1) Immune – 2) Infectious – 3) Genetic – 4) Drug-induced – 5) Disseminated intravascular coagulation – 6) Placental insufficiency – 7) Miscellaneous Algorithm in Evaluation Does thrombocytopenia fit pattern of pathophysiologic process? (Table 1) – Proceed to confirmatory testing Further evaluation is indicated if – It does not fit one of these patterns – The dx is not confirmed by appropriate testing – It is more severe/prolonged than fits dx – It does not respond to appropriate tx Category Subtype Severity Onset Resolution Mechanism Immune Alloimmune Autoimmune Severe Moderate Early Early Days - wks Incr. Wks - mos consumption Infection Bacterial Viral Fungal Variable Variable Severe Variable Early Late 1-7 days Variable 2-7 days Chromosomal Bone marrow failures Familial TCP Moderate Severe Early Early Days - wks Decreased Variable production Mild-mod Early Never Drugs Modsevere Late 8 days (med) Variable DIC Severe Variable Variable Inc consump PIH/ IUGR Mild-mod Early 7-10 days Dec prodxn NEC Mod-sev Late 7-10 days Inc consump Genetic disorder Mixed Evaluation in early thrombocytopenia: Mild to Moderate Neonate with early thrombocytopenia (<72 hrs) – First distinguish b/w mild-mod and severe • Mild (100-150 x 109/L) or moderate (50-100 x 109/L). • PIH and IUGR are common causes of early thrombocytopenia among premature infants • Generally, resolves spontaneously by day 7-10 of life • Other labs include PT, PTT, D-dimers, cx Evaluation in early severe thrombocytopenia Severe/prolonged should trigger evaluation for other disease processes – Well-appearing infant: most common cause in immediate post-natal period is immune thrombocytopenia from anti-plt Ab across placenta – Ill-appearing infant: consider other causes • Sepsis, DIC (freq post severe perinatal asphyxia) • Viral infections and congenital toxoplasmosis If tests fail to confirm dx, base further w/u on PE, response to plt transfusion, and mechanistic eval Physical Examination Dysmorphic features suggestive of chromosomal disorders provide dx clues: – Trisomy 21, 13, 18, Turner, Noonan syndrome, DiGeorge/velocardiofacial syndrome – HSM, abd masses (renal v thrombosis), forearm/thumb abnormalities (TAR/Fanconi’s) – Decreased pronation/supination of forearm (congenital amegakaryocytic TCP w/proximal radial-ulnar synostosis) Increased destruction Immune thrombocytopenia (0.3%) – Neonatal alloimmune thrombocytopenia (NAIT) • Mom forms IgG class antiplatelet Ab against the "foreign" antigen (dad’s) • Clinical features: mom asx, baby may have petechiae, ecchymosis • Labs: plts (often < 10,000/µL), antigen testing of parents’ plts, mother's serum for antiplatelet alloantibody • Management: well, term infants transfused if plt <20,000/µL or if bld – Transfusion threshold higher (<50,000/µL) in preterm/term infants who are ill or have risk factors. • Initial evaluation: head CT to r/o hemorrhage (10-20%) • Adequate plt counts maintained during 1st 72-96 hrs (highest bld risk) • Tx with high-dose intravenous gamma-globulin (IVIG) may be effective Increased Destruction: Immune Thrombocytopenia Autoimmune thrombocytopenia: – Mediated by maternal Ab that react with maternal and infant platelets. – Occurs in maternal autoimmune disorders, including ITP and SLE – Dx apparent from mother's PMH and maternal thrombocytopenia – Mothers of infants with unexplained neonatal thrombocytopenia autoimmune disorder? – Healthy women w/o hx of autoimmune d/o sometimes develop gestational thrombocytopenia that usually is mild, transient, and benign. Clinical features: Petechiae, bruising, and bleeding. – 90% infants have moderately severe thrombocytopenia in range of 20,000 to 50,000/µL – Risk in infant correlates with severity of ITP in the mother: • Mother s/p splenectomy, plts < 50 in preg, or older sibling w/neonatal affects – Plts decrease sharply during the several days after birth; nadir at 2-5 days Management: transfusion, IVIG, or prednisone for severe TCP or clinical bleeding – Plt trx may not be as effective as in NAIT: autoAb usually react w/donor Drug related thrombocytopenia Drug-related thrombocytopenia: – Mechanism is accelerated plt destruction caused by drugdependent Abs. – BM suppression may occur post chemo to mom or newborn infant – Maternal thrombocytopenia post drug exposure mediated by IgG Infant's platelet count should be monitored if exposed to quinidine, penicillins, digoxin, and antiepileptic drugs; indomethacin, heparin-induced thrombocytopenia less common Management — If drug-associated thrombocytopenia is suspected, the offending agent should be withdrawn. – Transfusions should be given for low platelet counts (<20,000/µL) or for bleeding. – If an immune-mediated condition is suspected, IVIG can be used while awaiting confirmation. Peripheral Consumption Hypersplenism: thrombocytopenia may be associated with an enlarged spleen. – Underlying disorders: hemolytic anemia, congenital hepatitis, congenital viral infection, and portal vein thrombosis – Management: Dx and tx of underlying cause. • Plt transfusions PRN. Splenectomy if bleeding uncontrollable. Kasabach-Merritt: DIC, hemangiomas (kaposiform hemangioendotheliomas) – shortened platelet survival caused by sequestration of plts in AVM. – Lesions noted at birth in approximately 50 % of patients • Trunk (including retroperitoneum), arms and shoulder, lower extremity, and cervicofacial – Severe thrombocytopenia, hypofibrinogenemia, elevated fibrin degradation products, and fragmentation of red blood cells – Management: resolution of hemangioma, support hemostasis w/trx – Tx: prednisone, interferon alpha, surgery, embolization, vincristine, cyclophosphamide, actinomycin D Peripheral Consumption Disseminated intravascular coagulationthrombosis and hemorrhage. – Complication of underlying illness, typically sepsis, asphyxia, MAS, severe RDS. – Dx suggested by associated illness, clinical presentation, and presence of microangiopathic changes on the peripheral blood smear. – Confirming labs: prolonged PT and PTT, decreased fibrinogen, increased D-dimer – Tx: directed at the underlying cause of DIC: platelets and FFP to maintain plt >50,000/µL and PT time within physiologic range. Fibrinogen concentration is maintained >100 mg/dL with infusion of cryoprecipitate. Infection: bacterial, viral, and fungal organisms. – Bacterial mechanisms for thrombocytopenia include DIC, endothelial damage, antibody-mediated, and platelet aggregation caused by adherence of bacterial products to platelet membranes. • Decreased plt production due to injury to megakaryocytes in BM also possible – Viral: congenital rubella and cytomegalovirus. • Mechanisms include platelet aggregation, loss of sialic acid from the platelet membrane caused by viral neuraminidase, and megakaryocyte degeneration. • Splenomegaly and reticuloendothelial hyperactivity may play a role. Management: tx underlying infection, platelet transfusions if associated bld Peripheral Consumption Necrotizing enterocolitis: GI necrosis in 2-10% of infants <1500 g. – thrombocytopenia from platelet destruction – In early stages, declining plts correlate with necrotic bowel and worsening disease. – Levels of cytokines, including platelet activating factor (PAF), are increased in premature infants with NEC and correlate w/ disease severity – Intestinal damage and inflammatory cell recruitment result from a cascade of cellular events that may be mediated at least in part by PAF Thrombosis: low plts often accompanies thrombosis in newborns. – Patients should be evaluated for a thromboembolic disorder if thrombocytopenia cannot be explained by other conditions. Decreased platelet production Often associated with genetic disorders: result in isolated thrombocytopenia or syndrome Thrombocytopenia-absent radius syndrome: severe thrombocytopenia and bilateral absent radii; thumbs are always present – Also hypoplasia or absence of the ulna, or abnormal or absent humerus. – Congenital heart disease, usually ASD or TOF, occurs in 1/3 of pts – plt <10,000 - 30,000/µL at birth-1st postnatal week in 59 % – Mortality is significant in neonate and early infancy, primarily due to ICH. • If pt survives this period, spontaneous resolution usually occurs after 1st year – Tx: supportive with platelet transfusions given when needed. Fanconi anemia: thrombocytopenia from FA is rare in the neonatal period. – Pancytopenia typically diagnosed at six to nine years old – Condition recognized in newborn by characteristic congenital malformations in 60-70%: • Hypopigmented spots, abnormality of thumbs, microcephaly, café-au-lait spots, and urogenital abnormalities; short stature of prenatal onset Our DNCC Guidelines for platelet transfusion Transfuse 10-15 mL/kg leukoreduced, irradiated platelets over 0.5-1 hour for: – – – – Infants w/o signs of acute bld, but plt <20,000 Infant w/hemorrhage and plt <50,000 Consider w/bld and plt <100,000, esp ICH risk Consider trx at predetermined value (20-100) depending on infant’s status (d/w attending) Transfusion precautions Neonates should receive 10-15 ml/kg of CMV-safe (CMV Ab-) or leukoreduced plts – Increases count by >50 x 109 Neonates are at increased risk for transfusion-associated GVHD – Irradiated bld products for immunodeficiency, intrauterine or exchange transfusions, or blood trx from relative or HLA-selected donor Conclusion: Neonatal Thrombocytopenia Common in NICU (sick and premature) Differentiate and tx based on severity Recognition of etiology based on typical patterns associated with specific pathophysiologic processes Work up and treat per algorithm and current clinical guidelines – Pursue immune etiology in infant w/persistent thrombocytopenia Sources/References Sola M. Evaluation and treatment of severe and prolonged thrombocytopenia in neonates. Clin Perinatol; 2004:31(1) Saxonhouse M, Sola M. Platelet function in term and preterm neonates. Clin Perinatol 2004;31(1) Andrew et al. A randomized, controlled trial of platelet transfusions in thrombocytopenic premature infants. J Pediatr 1993;123:285-91. Murray NA. Evaluation and treatment of thrombocytopenia in the neonatal intensive care unit. Acta Paediatr Suppl 2002;91:74-81. Sola, MC, Del Vecchio, A, Rimsza, LM. Evaluation and treatment of thrombocytopenia in the neonatal intensive care unit. Clin Perinatol 2000; 27:655. Jones, KL. Smith's Recognizable Patterns of Human Malformations, 5th ed. WB Saunders, Philadelphia 1997 Tomer et al. Autologous platelet kinetics in patients with severe thrombocytopenia. J Lab Clin Med 1991;118:546-54. UpToDate Version 12.1: search term neonatal thrombocytopenia