Morning Report
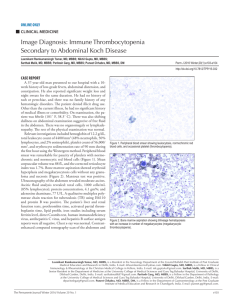
advertisement

Morning Report July 6, 2012 In the ER… 18 month old male with bruising and a bloody nose History ROS: Fell off chair 3 days ago, now mother noticing increasing size of bruise with no other known trauma, +bruising, +epistaxis, +small spots on entire body when woke up this morning URI ~1 week ago now resolved No fevers, no night sweats, no weight loss, no n/v/d, normal appetite and activity level, no gross hematuria PMHx: Full term, no complications. Not circumcised. Immunizations UTD – received 12 mo vaccines ~6 months. No medications. No history of eczema. Social Hx: LAHW mother, father, older sister, 1 cat. Family Hx: No bleeding disorders Physical Exam Temp 37.0 HR 115 RR 18 O2 sat 99% on RA BP 87/46 Gen: Well-appearing, well nourished, no distress. Running around the room HEENT: Anicteric sclera. Scattered bruises throughout the scalp. No rhinorrhea or congestion. Dried blood in right nare. MMM. Petechiae on OP and palate. Blood blister on upper lip mucosa. Scattered petechiae around mouth CV: RRR, no murmurs, 2+ pulses throughout Resp: CTAB/L, no wheezing, no rhonchi Abd: Soft, NT, normoactive BS. No distension, no masses. No HSM. MSK: Normal ROM LAD: Shotty anterior and posterior cervical adenopathy, all <1 cm Neuro: No focal deficits Skin: Petechiae, purpura throughout extremities, torso and abdomen. No jaundice or pallor One liner 18 mo M with no significant PMH presenting with sudden onset bruising and petechiae Work-up “Lab is calling to report a critical lab…” Platelets 5 Platelets Live 7-10 days Thrombocytopenia <150K No symptoms >100K Minimal symptoms 50-100K Mild (cutaneous) symptoms 20-50K Moderate (cutaneous + mucosal) symptoms 5-20K Severe symptoms (mucosal + CNS) <5K Thrombocytopenia Increased destruction Decreased production Name that syndrome! thrombocytopenia Kasabach-Merritt syndrome Sequestration of platelets and coagulation activation in large vascular malformations Fanconi anemia Fanconi anemia ≠ Fanconi syndrome! Autosomal recessive Hypopigmented macules, café-au-lait macules Abnormalities of thumbs Microcephaly Urogenital abnormalities Short stature Wiskott-Aldrich syndrome X-linked recessive Abnormal gene on proximal arm of X chromosome Atopic dermatitis Thrombocytopenic purpura Increased susceptibility to infections Thrombocytopenia-absent radii syndrome (TAR) ?defect of megakaryocyte Normal erythroid and myeloid maturation Bilateral absent radii Normal thumbs Skeletal, GU, heart anomalies Bernard-Soulier syndrome Autosomal recessive Dysfunction/absence of platelet receptor for von Willebrand factor Prolonged bleeding time Easy bruising, severe hemorrhage with trauma/surgery Increased destruction Disseminated intravascular coagulation (DIC) Hemolytic-uremic syndrome (HUS) Thrombotic thrombocytopenic purpura (TTP) Kasabach-Merritt syndrome Immune thrombocytopenic purpura (ITP) Drug induced Mechanical platelet destruction Platelet sequestration Decreased production Bone marrow failure or infiltrate Acquired aplastic anemia Leukemia, infectious granuloma Fanconi anemia Infection Nutritional Thrombocytopenia and absent radii (TAR) Wiskott-Aldrich syndrome Bernard-Soulier syndrome Cyanotic congenital heart disease Back to our patient… CBC 9.9>12.6/37.1<5, Smear: no schistocytes, +megakaryocytes Type and Screen O+, Antibody negative, Coombs negative ANA: pending Autoplatelet antibody: pending PT 12.6 PTT 27.5 INR 1.0 BMP normal LDH normal U/A 5-10 RBC, no WBC, no casts, no bacteria CRP <3 Immune Thrombocytopenic Purpura Isolated thrombocytopenia Immune mediated destruction of normal platelets Epidemiology ½ of cases occur in pediatric patients 2-10 year olds, peak 2-5 year olds Most common cause of isolated thrombocytopenia in otherwise well children 60% of cases occur within 1 month of an infection Seen following MMR vaccine Clinical manifestations Cutaneous bleeding Mucosal bleeding Absence of other symptoms Guidelines Diagnosis History, physical, CBC, smear Consider bone marrow biopsy if: Fever Bone/joint pain +family history HIV risk factors Skeletal or soft tissue morphologic abnormalities non-petechial rash Lymphadenopathy Abnormal Hgb, WBC, white cell morphology To Treat or Not to Treat Children with no or mild bleeding (skin manifestations only) be managed with observation* alone regardless of platelet count Essential components: anticipatory guidance, follow-up, reliable parents All patients: restrict activity (no contact sports), avoid medications with antiplatelet or anticoagulant activity *can be done as an outpatient Treat… Any child with significant bleeding (mucosal bleeding) regardless of platelet count Children with platelet count < 10K and cutaneous bleeding Choices: IVIG Anti-D immunoglobulin Steroids IVIG IVIG can be used if a more rapid increase in the platelet count is desired Meta-analysis comparing IVIG to steroids Primary outcome: platelets > 25K Steroids 26% less likely to achieve outcome IVIG Prevention of reticuloendothelial uptake of autoantibody-coated platelets IVIG Interaction of the autoantibodies with anti-idiotype antibodies in the IVIG Giving IVIG Single dose, 0.8-1 g/kg Side effects Fever Nausea, vomiting Headache Aseptic meningitis Anaphylaxis Renal failure Live vaccines must wait Rhogam Hgb >10, Rho(D) positive Side effects: fever, chills, hemolytic anemia Steroids Reduce antibody production Reduce reticuloendothelial system phagocytosis of antibody-coated platelets Improve vascular integrity Improve platelet production Prognosis 20% go on to have chronic ITP (> 6-12 months) Intracranial hemorrhage is rare – incidence of 0.1-0.5% Compare 5 yo M with ALL s/p chemotherapy with a platelet count of 5K 5 yo M with ITP with a platelet count of 5K PREP 2007 In examining a 4-year-old girl who is new to your practice, you discover that she has rudimentary thumbs and is well below the 5th percentile for both weight and height. You also observe irregular hyperpigmentation on the trunk and anogenital areas. Of the following, the MOST likely hematologic disorder associated with these findings is: A. Acute lymphoblastic leukemia B. Bloom syndrome C. Diamond-Blackfan anemia D. Fanconi anemia E. Thrombocytopenia and absent radii (TAR) syndrome PREP 2005 An otherwise well 4-year-old boy is brought to your office because his mother has noticed bruising over the past 2 weeks. On physical examination he appears well and has no hepatosplenomegaly or adenopathy. There are scattered petechiae on the right upper arm, resolving bruises on the legs, and no evidence of new bruises. A complete blood count shows a platelet count of 50 x 103/mcL. The white blood cell and differential counts, hemoglobin, and hematocrit are normal Of the following, the BEST next step in the management of this patient is to recommend: A. administration of intravenous immunoglobulin therapy B. administration of oral corticosteroid therapy C. avoidance of sulfonamides D. hospitalization for observation E. performance of a bone marrow examination Goals and Objectives Review the differential diagnosis for thrombocytopenia and syndromes associated with thrombocytopenia Review the pathophysiology of ITP Review the current approach to diagnosis and management of ITP References http://www.uptodate.com/contents/treatment-and-prognosis-of-immune-idiopathicthrombocytopenic-purpura-in-children?source=search_result&selectedTitle=3%7E150 http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-immune-idiopathicthrombocytopenic-purpura-in-children?source=search_result&selectedTitle=4%7E150 Beck CE, Nathan PC, Parkin PC, Blanchette VS, Macarthur C. Corticosteroids versus intravenous immune globulin for the treatment of acute immune thrombocytopenic purpura in c hildren: a systematic review and meta-analysis of randomized-controlled trials. J Pediatr. 2005; 147 (4):521527. Buchanan GR. Thrombocytopenia during childhood: what the pediatrician needs to know. Peds in Review. Nov 2005; 401-409. Consolini DM. Thrombocytopenia in infants and childrewn. Peds in Review. April 2011; 135-151. Nuenert C, Lim C. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood (2011) 117: 4190-4207