Unit 3: Hematology: Blood Dr. Moattar Raza Rizvi Physiology
advertisement

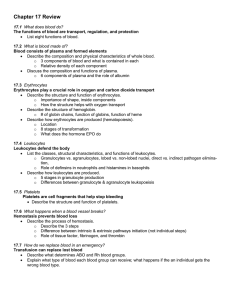
Unit 3: Hematology: Blood Dr. Moattar Raza Rizvi Physiology Basic functions of Blood Trasports • Oxygen and nutrients (removes waste products) • Hormones delivered to target organs Regulates • Body temperature, pH Protects • Against blood/fluid loss via hemostasis (coagulation) • Against infection via contribution to inflammatory and immune responses. Blood: Properties • • • • • • • • Sticky Opaque Salty-metallic taste Color varies according to oxygen content More dense than water and 5x more viscous pH: 7.35-7.45 (reservoir for bicarbonate ions) Temperature: 38°C Volume (4-6 litres; adult). The Composition of Whole Blood • Blood is the body’s only fluid tissue (a connective tissue) • 2 major components – Liquid = plasma (55%) – Formed elements (45%) • Erythrocytes, or red blood cells (RBCs) • Leukocytes, or white blood cells (WBCs) • Platelets or Thrombocytes The Composition of Whole Blood: Plasma Plasma (55% of whole blood) Buffy coat: leukocyctes and platelets (<1% of whole blood) 1 Withdraw blood and place in tube 2 Centrifuge Formed elements Erythrocytes (45% of whole blood) • Hematocrit • Males: 47% ± 5% • Females: 42% ± 5% The Composition of Whole Blood: Plasma • Hematocrit • Males: 47% ± 5% • Females: 42% ± 5% The Composition of Whole Blood: Plasma • Blood plasma components: – Water = 90-92% – Proteins = 6-8% • Albumins; maintain osmotic pressure and viscosity of the blood • Globulins – Alpha and beta globulins are used for transport purposes – Gamma globulins are the immunoglobulins (IgG, IgA, etc) – – – – • Fibrinogen; a clotting protein Organic nutrients – glucose, carbohydrates, amino acids Electrolytes – sodium, potassium, calcium, chloride, bicarbonate Nonprotein nitrogenous substances – lactic acid, urea, creatinine Respiratory gases – oxygen and carbon dioxide The Composition of Whole Blood: Formed Elements Formed Elements • Formed elements comprise 45% of blood • Erythrocytes, leukocytes, and platelets make up the formed elements – Only WBCs are complete cells – RBCs have no nuclei or organelles, and platelets are just cell fragments • Most formed elements survive in the bloodstream for only a few days • Most blood cells do not divide but are renewed by cells in bone marrow Erythrocytes (RBCs) • Biconcave disc – Folding increases surface area (30% more surface area) – Plasma membrane contains spectrin • Give erythrocytes their flexibility • Anucleate, no centrioles, no organelles – End result - no cell division – No mitochondria means they generate ATP anaerobically • Filled with hemoglobin (Hb) - 97% of cell contents – Hb functions in gas transport • Hb + O2 HbO2 (oxyhemoglobin) • Most numerous of the formed elements – Females: 4.3–5.2 million cells/cubic millimeter – Males: 5.2–5.8 million cells/cubic millimeter Erythrocytes (RBCs) Erythrocytes (RBCs) Function • Erythrocytes are dedicated to respiratory gas transport • Hemoglobin reversibly binds with oxygen and most oxygen in the blood is bound to hemoglobin – Hb functions in gas transport • Hb + O2 HbO2 (oxyhemoglobin) • Composition of hemoglobin – A protein called globin • made up of two alpha and two beta chains – A heme molecule • Each heme group bears an atom of iron, which can bind to one oxygen molecule • Each hemoglobin molecule thus can transport four molecules of oxygen Structure of Hemoglobin Hemoglobin • Oxyhemoglobin – hemoglobin bound to oxygen – Oxygen loading takes place in the lungs • Deoxyhemoglobin – hemoglobin after oxygen diffuses into tissues (reduced Hb) • Carbaminohemoglobin – hemoglobin bound to carbon dioxide – Carbon dioxide loading takes place in the tissues Life Cycle of Red Blood Cells The life span of an erythrocyte is 100–120 days Travels about 750 miles in that time Iron is transported from liver in blood plasma by beta-globulins as transferrin Erythropoietin Mechanism Start Normal blood oxygen levels Increases O2-carrying ability of blood Stimulus: Hypoxia due to decreased RBC count, decreased availability of O2 to blood, or increased tissue demands for O2 Reduces O2 levels in blood Enhanced erythropoiesis increases RBC count Erythropoietin stimulates red bone marrow Kidney (and liver to a smaller extent) releases erythropoietin Production of Erythrocytes • Hematopoiesis – blood cell formation • Production of Erythrocytes: Erythropoiesis – Occurs in the red bone marrow (myeloid tissue) • Axial skeleton and girdles • Epiphyses of the humerus and femur • Marrow contains immature erythrocytes Blood Hematocrit • The % volume occupied by red blood cells is known as the hematocrit. • Volume occupied by white blood cells is relatively small. Hematocrit under various circumstances Leukocytes (WBCs) • Leukocytes, the only blood components that are complete cells: – 4,800 - 10,000/cubic millimeter – Protect the body from infectious microorganisms – Can leave capillaries via diapedesis – Move through tissue spaces (amoeboid motion) – Many are phagocytic (possess numerous lysosomes) • Two major types of leukocytes – Granulocytes: Neutrophils, Eosinophils, Basophils – Agranulocytes: Monocytes, Lymphyocytes • Leukocytosis – WBC count over 11,000/mm3 – Normal response to bacterial or viral invasion • Leukopenia - a decrease in WBC count below 4,800/mm3 • Leukemia - a cancer of WBC Granulocytes Are all phagocytic cells Cell Type Neutrophils Characteristic features Account for 65-75% of total WBC’s Multilobed nucleus AKA “polys” or PMN’s Major Functions Ingest and destroy invading microorganisms Participate in acute inflammation (polymorphonuclear) Eosinophils Eosinophils account for 1–4% of WBCs Bilobed nucleus Phagocytic especially against parasitic infection Basophils Account for 0.5-1% of all WBCs Have U- or S-shaped nuclei Migrate to tissues to become mast cells; release of histamine contributes to inflammation Helps in allergic reactions Agranulocytes Cell Type Characteristic features Major Functions Monocyte Monocytes account for 3–7% They leave the circulation, enter of leukocytes tissue, and differentiate into They are the largest macrophages leukocytes They have purple-staining, Uor kidney-shaped nuclei Lymphocyte Account for 20-25% or more of WBCs and: Have large, dark-purple, circular nuclei with a thin rim of blue cytoplasm Most important cells of the immune system There are two types of lymphocytes: T cells and B cells T cells - attack foreign cells directly B cells give rise to plasma cells, which produce antibodies Platelets • Their granules contain serotonin, Ca2+, enzymes, ADP, and platelet-derived growth factor (PDGF) • Platelets function in the clotting mechanism by forming a temporary plug that helps seal breaks in blood vessels • Platelets not involved in clotting are kept inactive by Nitric Oxide (NO) and prostaglandins • Survive 5-9 days Normal blood cellular elements & typical human blood cell count Human Blood Groups • RBC membranes have glycoprotein antigens on their external surfaces • These antigens are: – Unique to the individual – Recognized as foreign if transfused into another individual – Promoters of agglutination and are referred to as agglutinogens • Presence or absence of these antigens is used to classify blood groups ABO Blood Groups • The ABO blood groups consists of: – Two antigens (A and B) on the surface of the RBCs – Two antibodies in the plasma (anti-A and anti-B) • An individual with ABO blood may have various types of antigens and spontaneously preformed antibodies • Agglutinogens and their corresponding antibodies cannot be mixed without serious hemolytic reactions Blood Groups • There are 4 blood types – – – – – A, B, AB, O Type A has “A” antigen, and B antibodies Type B has “B” antigen, and A antibodies Type AB has “A” and “B” antigen, and NO antibodies Type O has NO antigen and “A” and “B” antibodies Rh Blood Groups • Presence of the Rh agglutinogens on RBCs is indicated as Rh+; 85% of population is + • Lack of antigen indicated as Rh -; 15% of popn. • Anti-Rh antibodies are not spontaneously formed only in Rh– individuals Transfusion Reactions Hemostasis Blood Clotting Hemostasis is the complex process by which platelets, plasma, and coagulation factors interact to control bleeding. When a blood vessel ruptures, local vasoconstriction (decrease in the caliber of blood vessels) occurs to decrease blood flow to the area. Platelets and clotting factors become activated when exposed to the collagen layer of the damaged blood vessel. Platelets clump together (aggregate) by binding to the collagen, forming a loose platelet plug. Hemostasis Hemostasis = Opposite of hemorrhage stops bleeding Too little hemostasis too much bleeding Too much hemostasis thrombi / emboli Three major steps: 1.Vasoconstriction 2.Platelet plug Temporarily blocks the hole 1.Platelet-derived cytokines further the process 3.Coagulation cascade (= clot formation seals hole until tissues repaired) 1.Two pathways: Extrinsic and Intrinsic 4.After vessel repair, plasmin dissolves the clot StepsofHemostasis How Blood clots Two coagulation pathways converge onto common pathway 1.Intrinsic Pathway. Collagen exposure. All factors needed are present in blood. Slower. 2.Extrinsic Pathway. Uses Tissue Factors released by injured cells and a shortcut. How Blood clots Coagulation Factors Made up of plasma proteins—except for factor IV (calcium), which is a mineral, and factor III (thromboplastin), which is a lipoprotein released from tissue Produced in the liver Activated in a chain reaction, with each one in turn activating the next factor in the chain. Factor I Fibrinogen Factor II Prothrombin Factor III Tissue thromboplastin • Converts prothrombin to thrombin as blood starts to clot • Converts to fibrin when blood clots • Inactive precursor to thrombin Factor IV Consists of calcium ions Factor V Labile factor (proaccelerin) Factor VII proconvertin • Functions during the combined pathway phase of the coagulation system • Activated by Factor III in the extrinsic system • Required throughout the entire clotting sequence Coagulation Factors Factor VIII Factor IX • Antihemophilic factor • Required during the intrinsic phase of the coagulation system. • Plasma thromboplastin component • Required in the intrinsic phase of the coagulation system Factor XI Factor XII • Plasma thromboplastin antecedent • Required in the intrinsic system • Hageman factor • Required in the intrinsic system Factor X • Stuart factor (StuartPrower factor) • Required in the combined pathway of the coagulation system Factor XIII • Fibrin-stabilizing factor • Required to stabilize fibrin strands in the combined pathway phase of the coagulation system Roles of thrombin in hemostasis Anticoagulants • Clotting تخثرcan be prevented by Ca+2 chelators (e.g. sodium citrate or EDTA) • or heparin which activates antithrombin III (blocks thrombin) • Coumarin blocks clotting by inhibiting activation of Vit K • Vit K works indirectly by reducing Ca+2 availability Complete the following questions: 1. Diapedesis is the process by which the WBC’s comes out of blood capillaries. 2. Erythropoiesis is the formation of red blood cells. 3. Erythrocytopenia is the decrease in the number of RBC. 4. Hematocrit is the percentage of blood cells in the blood. 5. Instrument used to determine RBC count Hematocytometer 6. Hemolysis is breaking of RBC. 7. Hemometer instrument used to know percentage of hemoglobin in blood. 8. Leukocytosis is increase in number of WBC’s 9. Erythrocytosis is increase in number of RBC’s. 10. Leukopenia is decrease in number of WBC’s. 11. Red blood cells in human does not contain nucleus and mitochondria 12. Give the terms used for decrease in RBC and WBC count. 13. Blood is fluid connective tissue 1. 2. 3. 4. 5. 6. 7. 8. Write the functions of blood? Write the composition of blood? Write the different types of White blood cells? What is hemoglobin and its function? What is the life span of RBC? Write the functions of platelets? Name the different types of blood groups in our body. Name the antigens and antibodies present in blood group A, B, AB and O? 9. Name any 3 blood anticoagulants? 10. Name the plasma proteins found in blood with function? 11. Define blood coagulation? The property of blood to change from fluid to get state within a few minutes after it comes in contact with air is blood coagulation. 12. What is the role of vitamin K? Vitamin K is essential for the formation of blood clot.