The Increasing Cost of Obesity: Th I
advertisement
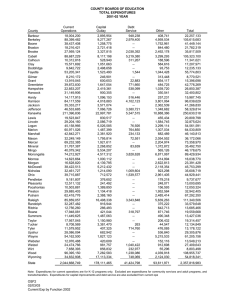
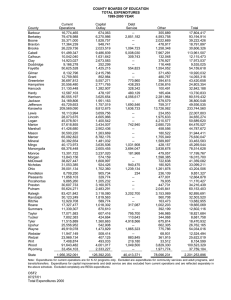
The Increasing Cost of Obesity: Th IImpactt off Ph The Physical i lA Activity ti it and d Obesity Ob it on Medical Expenditures 1998-2006 Jeroen van Meijgaard – UCLA School of Public Health Academy Health June 2010 BACKGROUND Obesity has been associated with morbidity and higher medical expenditures p Lack of physical activity has also been associated with morbidity (and mortality), independent of obesity; and thus likely with medical expenditures Physical activity and obesity are correlated in the population, yet few studies analyze independent impact on medical expenditures Some evidence that the impact of obesity on mortality has lessened over time Use nationally representative study over 9 years to evaluate independent impact of physical activity and obesity on medical expenditures and changes over time DATA – NHIS LINKED WITH MEPS Medical Expenditures Panel Survey (MEPS) is a subsample of individuals in the National Health Interview Survey (NHIS) MEPS is conducted 1-2 years after NHIS NHIS has self reported weight and height (BMI), leisure time physical activity activity, other health behaviors, behaviors as well as health conditions and socio-economic variables MEPS collects direct personal medical expenditures for each individual, regardless of source of payment, for a ous types of o expenditures e pe d tu es various NHIS data collection has been consistent since 1997 DATA – SAMPLE CHARACTERISTICS 1997-2005 NHIS data at baseline linked with 1 year expenditure data from 1998-2006 MEPS N=40,886: N 40 886 (18 (18-64: 64 32 32,803; 803 65+ 65+: 8 8,803) 803) Mean expenditures: $3,951 ($, 2003) No expenditures: p 13.3% Female: 57.4% BMI: • 18.5-24.9: 18 5 24 9: 38.0% 38 0% • 25.0-29.9: 35.4% • 30.0-34.9: 15.7% • 35.0-39.9: 5.6% • 40.0+: 3.2% Physical Activity: • None: 40.5% • 0.1-15.9 METhrs/wk: 30.5% • 16.0+ METhrs/wk: 28.9% METHODS Use GLM to estimate mean expenditures conditional on variables i bl off iinterest: E ( Expenditures) exp W W P P WPWxP Y Y WY YxW A A O1O1 O 2 O2 AO 2 AxO2 Analysis y is stratified by y Gender and Age g ((<65;; ≥65)) Separate Age indicator for 5-year age groups (A) Indicator for Period ((Y): ) 1998-2002 vs 2003-2006 Incorporate interaction for BMI (W) and PA (P) Incorporate interaction for Period (Y) and BMI (W) Other regressors include cancer status at baseline, usual care indicators and activityy limits RESULTS – IMPACT OF PA AND BMI ON EXPENDITURES Normal Weight Overweight g Obese I Obese II Obese III Age < 65 Age ≥ 65 Male Female Male Female $ 2,341 $ 3,158 $ 7,013 $ 7,285 + $ 225 + $ 138 + $ 284 – $ 187 + $ 994 + $ 708 + $ 2,205 + $ 1,421 + $ 813 + $ 848 + $ 2,640 , + $ 1,543 , + $ 791 + $ 885 + $ 3,608 + $ 650 Sedentary $ 2,752 Somewhat Active – $ 111 Very Active – $ 92 $ 3,545 – $ 189 – $ 186 $ 7,653 $ 7,948 – $ 613 – $ 379 + $ 628 – $ 1,207 Note: N t P P-value l < 5% shown h iin b bold ld – P-values P l and d confidence fid iintervals t l were obtained using simulation methods RESULTS – CHANGE OVER TIME Normal Weight Overweight g Obese I Obese II Obese III Age < 65 Male Female +1.6% +17.2% +13.4% +29.2% +12.9% +26.6% +12.2% +4.0% +14.9% +49.6% Age ≥ 65 Male Female +25.0% +42.9% – 6.2% – 8.6% +13.6% +14.3% –1.7% +92.0% +12.0% +2.4% BMI≥25 vs. [18.5-24.9] [18.5 24.9] BMI≥30 vs. [25.0-29.9] [25.0 29.9] +13.5% +11.6% 11.6% – – – – +9.7% +16.4% 16.4% +27.2% +10.0% 10.0% – – – – +28.5% +37.2% 37.2% Note: P-value < 5% shown in bold – P-values and confidence intervals were obtained using simulation methods DISCUSSION Substantial impact of overweight and obesity on medical expenditures p Impact of BMI on expenditures is changing over time • More rapid increase of expenditures among obese • Among elderly, shift of minimum to overweight Minimal impact of physical activity on medical expenditures, but not clear why it does not track impact on morbidity and mortality • Possibly due to injury related expenditures • Is higher level of PA associated with higher propensity to seek preventive care and other services • Maybe PA differentially impacts acute versus chronic conditions