Reducing Regional Disparities in Health Spending: Framing the Debate Maine Medical Center
advertisement
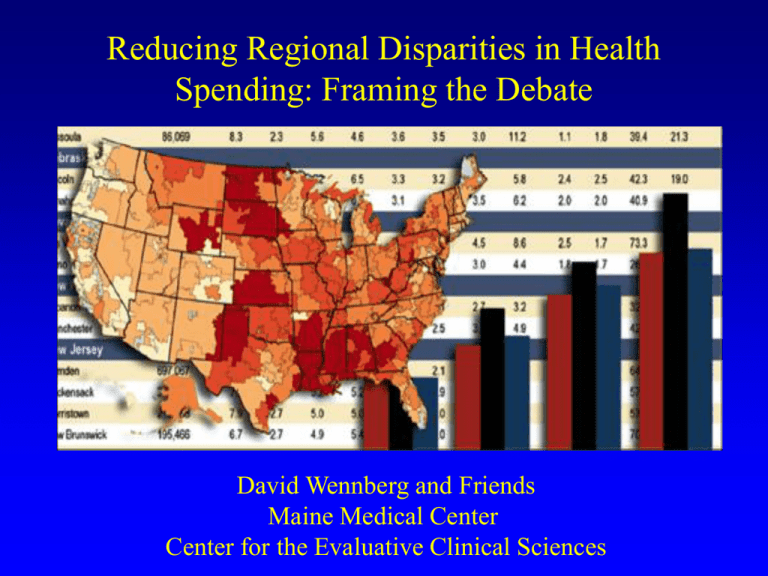
Reducing Regional Disparities in Health Spending: Framing the Debate David Wennberg and Friends Maine Medical Center Center for the Evaluative Clinical Sciences Regional disparities in health care spending Part 1 -- Unwarranted variations in U.S. health care: findings from the ‘Is More Better?’ studies Part 2 -- What can be done about it? Elliott Fisher, MD, MPH Therese Stukel, PhD Dan Gottlieb, MS F. L. Lucas, PhD Etoile Pinder, MS Unwarranted variations in medical practice: a framework for thinking about the delivery (or non-delivery) of care… Unwarranted? Variations that cannot be explained by: Illness or need --- and dictates of evidence based medicine Patient Preferences Categories of variation Effective care Preference sensitive care Supply-sensitive services Causes and remedies differ for each category Dartmouth Atlas of Health Care United States Hospital Referral Regions Elderly (U.S. Medicare) Study Design Myocardial Infarction Colorectal Cancer Hip Fracture Medicare Population (MCBS) Step 1: Select Cohorts Step 2: Group by regional spending level -- assigned based upon End-ofLife Expenditure Index Step 3: Validation (1) are patients the same at baseline? (2) does subsequent treatment differ? Step 4: Assess outcomes Follow cohorts for up to five years. Q1 HRRs Low Q2 HRRs Q3 HRRs Q4 HRRs Spending Process / Quality of Care / Survival Q5 HRRs High Regional Variations in the End-of-Life Expenditure Index (EOL-EI) and average per-capita Medicare spending EOL-EI $ 9,074 $ 10,636 $11,559 $ 12,598 $ 14,644 Spending $ 3,922 $ 4,439 $ 4,940 $ 5,444 $ 6,304 EOL-EI highly correlated (r = 0.81) with average per-capita Medicare spending Effective Care Services of proven effectiveness…. It involves no significant tradeoffs--all with specific needs should receive them Conflict between patients and providers is minimal Effective Care: Ratio of Rates in Highest vs Lowest Spending Regions 0.5 1.00 1.5 2.0 25 3.0 0.5 1.00 1.5 2.0 25 3.0 Acute MI Reperfusion in 12 hours for AMI Aspirin at admission Beta Blockers at admission Aspirin at Discharge Beta Blockers at discharge Exercise Test w/in 30 d General Population Mammogram, Women 65-69 Pap Smear, Women 65+ Flu shot during past year Pneumococcal Immunization (ever) Lower in High Spending Regions Higher in High Spending Regions Preference-Sensitive Care Involves tradeoffs among outcomes Decision should reflect preferences of patient Scientific uncertainty often substantial Preference-Sensitive Care: Highest vs Lowest Spending Regions 0.5 1.00 1.5 2.0 25 3.0 1.00 1.5 2.0 25 3.0 Procedures after AMI Angiography Angiography among appropriate cases Coronary Angioplasty Coronary Artery Bypass Surgery (CABG) Major Surgery (all cohorts combined) Cholecystectomy Cataract Extraction Hernia Repair Total Hip Replacement Total Knee Replacement Back Surgery Carotid Endarterectomy 0.5 Lower in High Spending Regions Higher in High Spending Regions Supply Sensitive Services Care strongly correlated with supply Generally provided in absence of strong clinical theory Evidence weak or non-existent on benefits. Supply-Sensitive Care : Highest vs Lowest Spending Regions 0.5 1.00 1.5 2.0 25 3.0 1.00 1.5 2.0 25 3.0 Physician Visits Office Visits Inpatient Visits Initial Inpatient Specialist Consultations % of Patients seeing 10 or more MDs Psychotherapy Visits Diagnostic Cardiology Procedures Electrocardiogram Echocardiogram Ambulatory ECG (Holter) Imaging Tests Chest X-ray CT / MRI Brain Ventilation Perfusion Scan 0.5 Lower in High Spending Regions Higher in High Spending Regions Supply-Sensitive Care : Highest vs Lowest Spending Regions 0.5 1.00 1.5 2.0 25 3.0 0.5 1.00 1.5 2.0 25 3.0 Specialist Procedures Upper GI Endoscopy Bronchoscopy Pulmonary Function Test Electroencephelogram (EEG) Hospital Utilization Discharges Total Inpatient Days Inpatient Days in ICU or CCU Care in Last Six Months of Life Inpatient Days ICU or CCU days Feeding Tube Placement Emergency Intubation Vena Cava Filter Lower in High Spending Regions Higher in High Spending Regions Findings Mortality Relative Risk of Death across Quintiles of Spending Decreased Risk 0.95 Hip Fracture Q1 Q2 Q3 Q4 Q5 Colorectal Cancer Q1 Q2 Q3 Q4 Q5 Myocardial Infarction Q1 Q2 Q3 Q4 Q5 0.95 Increased Risk 1.00 1.05 1.10 1.00 1.05 1.10 Change in relative risk of death per 10% increment in regional practice intensity: Acute Myocardial Infarction Cohort Decreased Risk 0.98 Increased Risk 1.00 1.02 1.04 1.00 1.02 1.04 Age < 80 Age > 80 Female Male Black Non-black Non-Q MI Anterior MI Inferior MI Other location Low risk (<15% 1yr) Moderate (15-30%) High Risk (> 30%) 0.98 Summary of Findings Increased spending across regions is largely devoted to “supply-sensitive services” Visit frequency, specialist services, tests, inpatient and ICU care. Residents of higher spending regions: Slightly worse basic access to care Equal use of major (potentially beneficial) procedures Quality measures generally somewhat worse No gain in function, survival or satisfaction Implications Costs reflect the capacity of the system Spending and capacity: the role of beds and medical specialists High MD High Bed 1.35 1.34 Low MD High Bed High MD Low Bed 1.59 1.19 1.18 Low MD Low Bed Implications Costs reflect the capacity of the system Greater capacity is not necessarily better Implications Costs reflect the capacity of the system Greater capacity is not necessarily better We’re wasting 30% of current spending on supply sensitive care alone… Regional disparities in health care spending Part 1 -- Unwarranted variations in U.S. health care: findings from the ‘Is More Better?’ studies Part 2 -- What can be done about it? Principles to Guide Interventions Variation Effective Care Cause Remedy Poorly understood care processes Develop systems of care capable of improvement Failure to learn Reward those who provide high quality care Construct benefits to ‘incent’ beneficiaries to become active consumers and to seek ‘high quality providers’ Principles to Guide Interventions Variation Cause Remedy Effective Care and Patient Safety Poorly understood care processes Develop systems of care capable of improvement Preference Sensitive Care MD-dominated decisions Shared Decision Making Construct Benefits to ‘Steer’ insured to high quality providers AND ‘incent’ them to seek SDM information and coaching Reward providers for participating in SDM Principles to Guide Interventions Variation Cause Remedy Effective Care and Patient Safety Poorly understood care processes Develop systems of care capable of improvement Preference Sensitive Care MD-dominated decisions Shared Decision making Supply Sensitive Care Variations in supply Assumption that more is better Micro: selective contracting with longitudinally efficient providers Demand excellence in effective care and preference sensitive care Macro: discourage continual increases in system capacity Regional disparities in health care spending Part 1 -- Unwarranted variations in U.S. health care: findings from the ‘Is More Better?’ studies Part 2 -- What can be done about it?