served procedural mortality rates for both off- editorials
advertisement

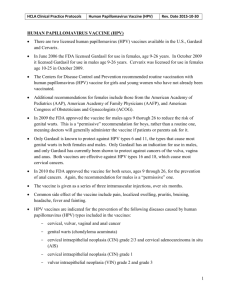
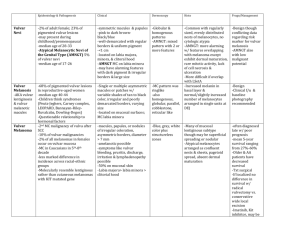
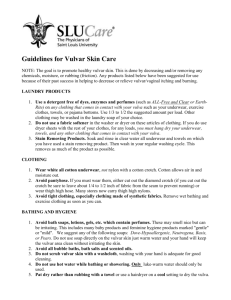
editorials served procedural mortality rates for both offpump and on-pump CABG were excellent and well below those predicted according to standard risk models. Third, neurocognitive testing was performed in only half the survivors and, in contrast with the results of a previous study,7 did not show any longitudinal deficits in either surgical group. Finally, some will argue that newer off-pump techniques and improved medications for secondary prevention make the findings of the trial less applicable for contemporary care. However, several trials comparing off-pump with on-pump CABG are currently under way that can broaden our understanding.8,9 In summary, the ROOBY trial did not support off-pump procedures as an advance that should generally supplant traditional techniques. As such, it will probably remain a technique reserved for selected patients and skilled surgeon advocates. However, the trial should truly be seen as a very positive one. It clearly showed the feasibility and willingness of surgeons to subject new surgical innovations to large-scale rigorous evaluation. Investigators in future trials involving CABG will need to consider other proposed innovations, including the evolving use of endovascular vein-graft harvesting methods, hybrid PCI–CABG techniques, and even robotic procedures. Although the results of such studies will not always show that the new approach is an advance, much can be learned from this type of systematic study. Through this process of innovation and evaluation, cardiac surgery will continue to evolve and lead to improved outcomes for its recipients. Dr. Peterson reports being principal investigator for the Society of Thoracic Surgeons National Adult Cardiac Surgery Database Warehouse, Duke Clinical Research Institute, Durham, NC. No other potential conflict of interest relevant to this editorial was reported. From the Duke Clinical Research Institute, Duke University Medical Center, Durham, NC. 1. Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation 2004;110:1168-76. [Erratum, Circulation 2005;111:2014.] 2. Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics — 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119(3):e21-e181. [Erratum, Circulation 2009;119(3):e182.] 3. Peterson ED, Mark DB. Off-pump bypass surgery — ready for the big dance? JAMA 2004;291:1897-9. 4. Feng ZZ, Shi J, Zhao XW, Xu ZF. Meta-analysis of on-pump and off-pump coronary arterial revascularization. Ann Thorac Surg 2009;87:757-65. [Erratum, Ann Thorac Surg 2009;87: 2008.] 5. Shroyer AL, Grover FL, Hattler B, et al. On-pump versus offpump coronary-artery bypass surgery. N Engl J Med 2009; 361:1827-37. 6. Magee MJ, Coombs LP, Peterson ED, Mack MJ. Patient selection and current practice patterns for off-pump coronary artery bypass surgery. Circulation 2003;108:Suppl 1:II-9–II-14. 7. Newman MF, Mathew JP, Grocott HP, et al. Central nervous system injury associated with cardiac surgery. Lancet 2006; 368:694-703. 8. The German Off Pump Coronary Artery Bypass in Elderly Study (GOPCABE). ClinicalTrials.gov, July 2008. (Accessed October 15, 2009, at http://clinicaltrials.gov/ct2/show/NCT00719667? term=off+pump&rank=1.) 9. The Danish On-Pump, Off-Pump Randomization Study (DOORS). ClinicalTrials.gov, August 2005. (Accessed October 15, 2009, at http://clinicaltrials.gov/ct2/show/NCT00123981? term=off+pump&rank=6.) Copyright © 2009 Massachusetts Medical Society. Human Papillomavirus Vaccine for Cancer Prevention Olivera J. Finn, Ph.D., and Robert P. Edwards, M.D. Cancer immunoprevention has become synonymous with the vaccines that have been approved for the prevention of infection with highly transmissible strains of human papillomavirus (HPV) that establish chronic infection and cause cervical and other cancers.1 Although many cancers may have a viral origin,2 only a small number of viruses have been implicated as causes of human cancer. Cancer having a viral origin provides an opportunity to develop virus-specific vaccines that lower infection rates and consequently lower the incidence of cancer; this is what the HPV vaccine is expected to do for cervical cancer and what the hepatitis B vaccine has already done for hepatocellular carcinoma.3 The question has been raised whether the same or similar HPV vaccines can be used in persons already infected with HPV to clear chronic infection or interrupt the process of oncogenesis that may have already started (in cervical or vulvar intraepithelial neoplasia) or progressed to cervical, vulvar, or other cancers. The past few decades of research in immunology have shown that cancer vaccines must elicit cellular as well as hu- n engl j med 361;19 nejm.org november 5, 2009 Downloaded from www.nejm.org at UC SHARED JOURNAL COLLECTION on July 3, 2010 . Copyright © 2009 Massachusetts Medical Society. All rights reserved. 1899 The n e w e ng l a n d j o u r na l moral immune responses to be effective.4 Inasmuch as the current HPV vaccine is primarily designed to elicit neutralizing antiviral antibodies to prevent initial infection, different types of HPV vaccines are required to target HPV not as a virus but as a tumor antigen. In this issue of the Journal, Kenter et al.5 report on the clinical and immunologic responses induced by an HPV vaccine composed of synthetic long peptides containing the HPV type 16 (HPV-16) epitopes E6 and E7 in patients with HPV-16–associated, grade 3 vulvar intraepithelial neoplasia. This article is the latest in a series of articles by the same authors who over the past several years have tested this vaccine in preclinical settings for its tumor-rejection potential6 and for its safety and immunogenicity in end-stage cervical cancer.7 Twenty women with HPV-16–positive, grade 3 vulvar intraepithelial neoplasia were vaccinated with a mixture of peptides derived from HPV-16 oncoproteins E6 and E7 in incomplete Freund’s adjuvant (Montanide ISA-51). The peptides were 30 to 40 amino acids in length. Strong CD4+ and CD8+ T-cell responses were generated in all patients, and at 12 months of follow-up, 15 of 19 patients showed an objective clinical response as measured by symptom relief, the reduced size or disappearance of lesions, and the loss of HPV-16 DNA. Nine women had a complete response and remained disease-free at 24 months of follow-up. This study is important for several reasons. In the context of the previous studies by this group of investigators,6,7 it suggests that more effective immune responses can be generated against precursor lesions than against late-stage disease. Many cancer vaccines based on nonviral tumorassociated antigens have been judged to be suboptimal because of their lack of efficacy in advanced disease, yet they might perform very differently if used in patients with premalignant disease.8 Until recently, the treatment of vulvar intraepithelial neoplasia was limited to ablation with a carbon dioxide laser for low-grade lesions or wide local excision for high-grade vulvar intraepithelial neoplasia.9 Recurrence is the rule, and multiple treatments and excisions are required. Less invasive therapeutic approaches that provide durable protection from recurrence are needed. The study reported here provides support for immunotherapy as one such approach. Many different formulations of cancer vaccines have been proposed and tested over the years, es1900 of m e dic i n e pecially in the therapeutic setting, where the potential for greater efficacy has been matched by the greater complexity of design and delivery. This complexity requires sophisticated laboratories in major medical centers to complete the studies. If vaccines are to make a difference in the incidence of cancer worldwide, practicality must be one of the most important requirements. A synthetic peptide vaccine such as the one described in the article by Kenter et al. fulfills that requirement. The benefit of a therapeutic approach to this disease based on an immune response has been foreshadowed by trials of imiquimod cream, an immune-response modulator that binds to toll-like receptor 7 and promotes type 1 T-cell–mediated immunity. A recent trial of imiquimod10 randomly assigned 52 women with multifocal grade 2 or 3 vulvar intraepithelial neoplasia to receive either imiquimod or a placebo cream. Complete lesion regression occurred at 20 weeks in nine patients treated with imiquimod and in no patients in the placebo group; this regression was associated with clearance of HPV DNA from the lesion as well as an increase in infiltrating dendritic cells, CD8+ T cells, and CD94+ natural killer cells. Long-lasting clinical responses occurred in both the vaccine trial and the imiquimod trial, but both trials were limited to small numbers of patients and a short follow-up time. These promising approaches must be developed further to provide an alternative to standard surgical excision and ablation of vulvar intraepithelial neoplasia, especially since this disease is increasingly diagnosed in young women. The ultimate goal should be to further improve the efficacy of the HPV vaccine by combining it with immunotherapeutic reagents with a proven ability to augment T-cell responses.11 Kenter et al. focused here on HPV-16–positive, grade 3 vulvar intraepithelial neoplasia lesions and HPV-16–specific immunotherapy. However, at least 14 common types of HPV (e.g., types 6, 11, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59) are detected in grades 1 through 3 vulvar intraepithelial neoplasia,12 and eventually these types need to be considered for inclusion in the vaccine. HPV-negative vulvar intraepithelial neoplasia lesions also may give rise to epithelial cancers. These lesions might share with other epithelial premalignant lesions many nonviral tumor antigens first detected in epithelial tumors and later detected in their precursor lesions. Thus, tumor-associated antigens n engl j med 361;19 nejm.org november 5, 2009 Downloaded from www.nejm.org at UC SHARED JOURNAL COLLECTION on July 3, 2010 . Copyright © 2009 Massachusetts Medical Society. All rights reserved. editorials common to several epithelial cancers such as pancreatic epithelial neoplasms, ductal carcinoma in situ of the breast, or adenomatous polyps (precursors to colon cancer) should be evaluated as potential target antigens in vulvar intraepithelial neoplasia. A project carried out by the National Cancer Institute in collaboration with tumor immunologists13 prioritized cancer antigens to assist investigators in selecting the most promising antigens for further development. The list of the top 100 antigens includes HPV-16 oncoproteins E6 and E7 as well as others that are probably expressed in vulvar cancer and vulvar intraepithelial neoplasia and could be used in the development of vaccines for HPV-negative tumors. Long synthetic peptides derived from some of these antigens could be added to the peptides in the HPV vaccine reported on by Kenter et al. to cover most, if not all, vulvar intraepithelial neoplasia. Dr. Edwards reports receiving consulting fees from Fresenius and grant support from Sanofi-Aventis. No other potential conflict of interest relevant to this article was reported. From the Departments of Immunology (O.J.F.) and Obstetrics and Gynecology (R.P.E.), University of Pittsburgh School of Medicine, Pittsburgh. 1. zur Hausen H. Papillomaviruses causing cancer: evasion from host-cell control in early events in carcinogenesis. J Natl Cancer Inst 2000;92:690-8. 2. Idem. The search for infectious causes of human cancers: where and why. Virology 2009;392:1-10. 3. Chang MH. Cancer prevention by vaccination against hepatitis B. Recent Results Cancer Res 2009;181:85-94. 4. Finn OJ. Cancer immunology. N Engl J Med 2008;358:270415. 5. Kenter GG, Welters MJP, Valentijn ARPM, et al. Vaccination against HPV-16 oncoproteins for vulvar intraepithelial neoplasia. N Engl J Med 2009;361:1838-47. 6. Zwaveling S, Ferreira Mota SC, Nouta J, et al. Established human papillomavirus type 16-expressing tumors are effectively eradicated following vaccination with long peptides. J Immunol 2002;169:350-8. 7. Kenter GG, Welters MJ, Valentijn AR, et al. Phase I immunotherapeutic trial with long peptides spanning the E6 and E7 sequences of high-risk human papillomavirus 16 in end-stage cervical cancer patients shows low toxicity and robust immunogenicity. Clin Cancer Res 2008;14:169-77. 8. Finn OJ. Premalignant lesions as targets for cancer vaccines. J Exp Med 2003;198:1623-6. 9. Hillemanns P, Wang X, Staehle S, Michels W, Dannecker C. Evaluation of different treatment modalities for vulvar intraepithelial neoplasia (VIN): CO(2) laser vaporization, photodynamic therapy, excision and vulvectomy. Gynecol Oncol 2006;100:271-5. 10. van Seters M, van Beurden M, ten Kate FJW, et al. Treatment of vulvar intraepithelial neoplasia with topical imiquimod. N Engl J Med 2008;358:1465-73. 11. Cheever MA. Twelve immunotherapy drugs that could cure cancers. Immunol Rev 2008;222:357-68. 12. Garland SM, Insinga RP, Sings HL, Haupt RM, Joura EA. Human papillomavirus infections and vulvar disease development. Cancer Epidemiol Biomarkers Prev 2009;18:1777-84. 13. Cheever MA, Allison JP, Ferris AS, et al. The prioritization of cancer antigens: a national cancer institute pilot project for the acceleration of translational research. Clin Cancer Res 2009; 15:5323-37. Copyright © 2009 Massachusetts Medical Society. End Run around Epo H. Franklin Bunn, M.D. Recombinant human erythropoietin is arguably the most successful therapeutic application of recombinant DNA technology to date. Since the initial reports — which appeared 22 and 23 years ago1,2 — documented a cure of the anemia of chronic kidney disease with recombinant human erythropoietin, well over a million patients have been treated with it effectively and with minimal drug-related toxicity. Moreover, recombinant human erythropoietin has also been effective in the treatment of patients with cancer, particularly when anemia has been aggravated by chemotherapy. Although recombinant human erythropoietin merits high marks for efficacy and safety, concerns have arisen about two distinct types of adverse effects. From 2000 through 2004, severe pure red-cell aplasia developed in several hundred patients with chronic kidney disease, primarily in Europe, after subcutaneous administration of recombinant human erythropoietin.3 Auto­ antibodies in the serum of these patients neutralized both recombinant human erythropoietin and endogenous erythropoietin. It is likely that in this cluster of cases, antibodies arose in part because of a defective formulation of the recombinant human erythropoietin that enabled the formation of neoantigens. Moreover, subcutaneous self-administration poses problems with storage and handling that could impair the stability of the molecule and enhance the formation of antibodies. With improved formulation and intravenous administration, the incidence of this complication has fallen to the extremely low, pre- n engl j med 361;19 nejm.org november 5, 2009 Downloaded from www.nejm.org at UC SHARED JOURNAL COLLECTION on July 3, 2010 . Copyright © 2009 Massachusetts Medical Society. All rights reserved. 1901