Derbyshire Community Health Services NHS Foundation Trust Annual Quality Account 2014/15
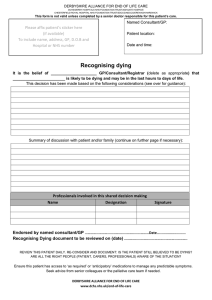
advertisement

Derbyshire Community Health Services NHS Foundation Trust Annual Quality Account 2014/15 Contents Part 1 ........................................................................................................................................................ 3 Introduction ............................................................................................................................................... 3 Declaration of Accuracy............................................................................................................................. 3 Part 2 ........................................................................................................................................................ 4 Driving quality improvements..................................................................................................................... 4 2014/15 Quality priorities ........................................................................................................................... 4 Part 3 .......................................................................................................................................................11 Evidence of quality improvements for 2014/15 .........................................................................................12 What have we done to improve patient safety? ........................................................................................12 Ensuring services are clinically effective ...................................................................................................25 What we have done to improve patient experience? ................................................................................32 Ensuring our services are responsive to patients’ needs ..........................................................................40 Appendix 1 - Workforce ............................................................................................................................47 Appendix 2 - Information Governance Toolkit submission for 2014/15 .....................................................53 Appendix 3 - Third party statements - CCGs/Healthwatch ........................................................................54 Appendix 4 - Statement of Directors’ responsibilities in respect of the Quality Account ............................58 Appendix 5 - Independent Auditors ..........................................................................................................59 Appendix 6 - The Core Quality Account Indicators ...................................................................................60 Glossary ...................................................................................................................................................63 2 Part 1 Introduction Welcome to our Quality Report for 2014/15 which sets out what we have done to safeguard and improve the quality of our services during the year, where we still need to make improvements and what we want to achieve in 2015/16. Here at Derbyshire Community Health Services NHS Foundation Trust (DCHS) our vision is to be the best provider of local healthcare and a great place to work. During the year we have implemented a wide range of service developments and quality improvements in support of this vision. This report is an important part of discharging our accountability to the local communities that we serve and describing the progress we have made. The organisation became an NHS Foundation Trust on the 1 November 2014, increasing our local accountability through the establishment of an elected Council of Governors. This report covers the quality of our services across the entire 2014/15 year, including the seven months we were an NHS Trust. We feel that we have made good progress in the year in continuing to improve the safety and effectiveness of our services, as well as the experience of our care, for everyone that we support. This progress and the high quality of care our 4,400 colleagues provide was recognised by the Care Quality Commission (CQC) during the year when they undertook a full inspection of the Trust. They noted that the Trust provided safe care delivered by staff who were dedicated and compassionate and who demonstrated excellent commitment in providing the best care they could and putting patients’ needs at the centre of their care. They did highlight isolated areas where we were not found to be meeting the full range of essential quality standards and we have successfully and effectively addressed these in the year. Tracy Allen, Chief Executive and Prem Singh, Chairman Declaration of Accuracy I confirm that to the best of my knowledge the information presented in our Annual Quality Report is accurate Signature Tracy Allen, Chief Executive Are we accessible to you? This publication is available on request in other formats (for example, large print, easy read, Braille or audio version) and languages. For free translation and/or other formats please call 01773 525099 extension 5587, or email us at: communications@dchs.nhs.uk To see the full list of the services we provide, please visit www.dchs.nhs.uk or call us on 01773 525099 for support. 3 Part 2 Driving quality improvements 2014/15 Quality priorities This quality report demonstrates our achievements for the year 2014/15, describes the areas where we would still like to make improvements and our quality objectives for the coming year. Our quality improvement priorities are identified within the Trust’s overarching annual objectives, known as the Big 9. During 2014/15 we set ourselves three key quality priorities - known as the Big 3 - to focus the whole organisation on quality improvement in areas of patient safety, clinical effectiveness and patient experience. These priorities were to: keep people safe - reducing the number of serious medication errors by 50% keep patients (and families) at the centre of care - to establish 10 active patient engagement groups ensure care is effective - 95% of patients with diabetes to have an appropriate care plan We are pleased to report that we have achieved all of these objectives, reducing our medication errors resulting in serious harm from 14 in 2013/14 to 0 in 2014/15. DCHS BIG 3 In addition to our organisation-wide quality improvement targets in 2014/15 we have been working to achieve a combination of quality objectives and service improvements which we set ourselves, together with quality targets which are set out in our contract with local health service commissioners. These are reported in more detail in the body of this report. Our quality priorities build upon what we already know about our services, what our patients have told us are important to them and in response both to commissioners’ and national priorities. We also place a great emphasis on learning from our staff who are at the frontline of care delivery and we have developed an effective network of ways to engage with them and hear their feedback. We are particularly proud of our annual staff survey results 2014, which listed us as the best performing trust, based on feedback from our staff. Things we want to do better in 2015/16 We are continually striving to improve the quality of the services we provide and to learn from things that did not go so well. For 2015/16 our Board of Directors has agreed three strategic quality improvement objectives: 1) Patient Safety - Improvement in information sharing Ensuring that clinicians have up-to-date information regarding their patients at all times is vital to the delivery of effective, safe and responsive healthcare. During 2015/16 we will be asking our 4 staff to ask patients, at initial consultation, if they give consent to their health records being shared with other health practitioners to ensure better continuity of care. 2) Clinical Effectiveness - To increase the number of referrals to Smoking Cessation services made by DCHS staff Smoking has been demonstrated as one of the most significant issues with regard to poor health in our population. All health professionals have a responsibility to advise patients on the ill effects of smoking and to sign post them to services which can support them to stop. 3) Patient Experience - Identify where patients with a learning disability access our services Individuals with a learning disability can access any of our services and as such have a right to care and treatment appropriate to their needs. This target will help us to identify the specific needs of patients with a learning disability and the changes we need to make to ensure they can access our services equitably. In addition we will continue to strengthen our internal processes for quality improvement and assurance using our Quality Improvement and Assurance Framework. Monitoring and measuring quality We are actively committed to being able to demonstrate the consistency and quality of our services. We want our patients and their families to feel safe and well looked after. We recognise the need for a continuous focus on improving our quality assurance measures. During 2014/15 we have developed further processes for assuring the quality of our services. We have implemented the Quality Improvement and Assurance Framework. Quality Improvement and Assurance Framework DCHS Way Clinical & Quality strategy Patient experience and engagement Effective communication Highest quality staff Raising concerns & whistleblowing Board to ‘ward’ engagement Staff engagement & feedback Staff selection, training and development Governance structure Board development Risk strategy and policy Management structure and job roles Data quality Integrated performance dashboard Patient and carer feedback This tiered approach to quality assurance includes: Rapid Response monitoring Individual practitioners and teams - working to agreed standards, policies and professional Intelligence monitoring guidelines. Benchmarking Peer review - Quality Always is our trust-wide clinical assessment and accreditation model which aims to draw together all standards against which clinical teams are measured. Most importantly the fundamental standards defined by the CQC are included and as such this will be our primary method for assessing ongoing compliance with CQC standards. Board quality and safety visits - which ensure frontline staff are able to engage with board members, senior managers and governors about things that concern them and which may prevent them providing best care consistently. Independent review - working with our commissioners, external partners and professional bodies to provide independent assurance of the quality of our services. 5 Quality Always is underpinned by a robust approach to clinical leadership, in line with our People and Organisational Effectiveness Strategy. A focus on capability and development will ensure that we continue to develop our clinical leaders in line with the rapidly changing healthcare environment. In addition to our Quality Improvement and Assurance Framework, we have a comprehensive governance structure to monitor our compliance with essential standards of care, the quality of service delivery and progress against key priorities. This is supported by a detailed clinical dashboard to monitor key performance indicators, which in turn is supported by a data quality kite assurance process. Monthly reports on the quality of services are presented to the Quality Services Committee and to the Board of Directors and these meetings are underpinned by a broad range of quality groups providing assurance on specialist topic areas. We meet with our commissioners every month via the Quality Assurance Group which monitors and reports on our quality schedule, our performance against Commissioning for Quality and Innovation targets and any other issues which positively or negatively impact on the quality of our services. During 2015/16 we will continue to strengthen our assurance processes and roll out Quality Always, our clinical peer assessment and assurance process. We will be working with Southern Derbyshire Clinical Commissioning Group (SDCCG) to establish an additional quality assurance group focused on services commissioned directly by them. Our services in 2014/15 During 2014/15 the DCHS provided and/or sub-contracted 36 relevant health services. The income generated by the relevant health services reviewed in 2014/15 represents 100% of the total income generated from the provision of relevant health services by DCHS for 2014/15. Of these services, 32 were NHS commissioned services (£144m) and a further four were commissioned by local authorities (£9m). Services included rehabilitation, community nursing, health visiting, school nursing, sexual health services, community dental services for patients with mental health problems and learning disabilities, as well as a wide range of planned care services such as podiatry, physiotherapy, speech and language therapy and occupational therapy. Strategically we have continued to redesign our services with an aim to support our patients as close to home as possible. As part of our duty of care we continuously review the quality of all our services. DCHS has reviewed all the data available to them on the quality of care in all of these NHS services. It is important that we focus carefully on the way we spend the money allocated to us for provision of our services. We need to ensure we are able to deliver best value for money at all times, whilst also striving to provide the very best care for people in our local community. National clinical audits During 2014/15 a total of six national clinical audits and no national confidential enquiries covered NHS services that DCHS provides. During that period DCHS participated in 83% national clinical audits and 0% national confidential enquiries which it was eligible to participate in. 6 The national clinical audits and national confidential enquiries that DCHS was eligible to participate in during 2014/15 are as follows: Audit title National COPD audit Sentinel stroke national audit National PROMs programme National audit of intermediate care National diabetic foot care audit NCEPOD sepsis audit The national clinical audits and national confidential enquiries that DCHS participated in during 2014/15 are as follows: Audit title National COPD audit National PROMs programme National audit of intermediate care National diabetic foot care audit NCEPOD sepsis audit Our participation in the Sentinel stroke audit is currently being scoped both in terms of eligible clinical services and workload implications for data collection. It is anticipated that we will join this audit fully in 2015/16. The national clinical audits and national confidential enquiries that DCHS participated in, and for which data collection was completed during 2014/15, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by terms of that audit or enquiry. Audit title Percentage of the number of registered cases submitted National COPD audit Participation ongoing National PROMs programme National audit of intermediate care Limited participation – less than 12% in Q1 and Q2. Future improvement in recruitment expected. No target set. 12 patients recruited to the PREM part of the audit – 100% National diabetic foot care audit Participation ongoing NCEPOD sepsis audit Organisational audit only DCHS always reviews national reports in conjunction with local results. The reports of two national clinical audits were reviewed by DCHS in 2014/15 and DCHS intends to take the following actions to improve the quality of healthcare provided: • • The national audit of intermediate care has reported its results and we reviewed the DCHS results against the national benchmarks in March 2015 in order to agree an improvement action plan. The PROMs results are reported slowly after each quarter and only Q1 is available so far. DCHS is implementing a plan to improve patient recruitment for groin hernia day surgery over the next 7 • year before it can utilise the pre- and post-op outcomes data for a local patient outcome improvement plan, given the low level of activity in DCHS for this surgical procedure. The remaining audits have not been completed and reported yet. The number of patients receiving relevant NHS services provided or subcontracted by DCHS in 2014/15 that were recruited during that period to participate in research approved by a research ethics committee were: Name of study Number of participants Dementia and Imagination 11 Nourishing Start for Health 3 Electrical muscle stimulation dysphagia study 3 Further information on our approach to clinical audit is detailed in section 3 of the report. Commissioning for Quality and Innovation (CQUIN) A proportion of DCHS income in 2014/15 was conditional on achieving quality improvement and innovation goals agreed between DCHS and North Derbyshire Clinical Commissioning Group (CCG) as the lead commissioner on behalf of our four CCGs. This was part of our contract for the provision of NHS services, through the Commissioning for Quality and Innovation payment framework. Total CQUIN contract value for 2014/15 was £3,181,922 and we are predicted to earn approximately 96% of this value, taking into consideration that we are likely to receive 20% of the final payment for the Safety Thermometer CQUIN in relation to the stretched target of reducing pressure ulcer prevalence (CQUIN value of £165,460). This indicates a total CQUIN payment of £3,049,554. Further details of the agreed goals for 2014/15 and for the following 12 month period are available in section 3. Care Quality Commission (CQC) DCHS is required to register with the CQC and its current registration status is: registered with the CQC with no conditions attached to registration. The CQC has not taken enforcement action against DCHS during 2014/15. DCHS is subject to periodic reviews by the CQC and the last comprehensive inspection was between 26 February and 4 March 2014 with a further focused inspection between 11 and 12 November 2014. The CQC’s assessment following that review was that the Trust is fully compliant with all essential standards. DCHS volunteered to be in the first wave of new style CQC inspections and worked with the Commission to develop their new inspection tool. Included within their inspection were the following services: • Community services for children and families • Community services for adults with long-term conditions • End of life care • Learning disability services • Minor injury services • Dental services • Elective care services • Mental health services. There was a great deal to be proud of within the outcomes of the March 2014 inspection report. It was reported that: ‘patients were overwhelmingly positive about the care and treatment they received’ and ‘patients and their families were treated with compassion and respect, and were involved in their care and well informed’. 8 The CQC did however find some areas for improvement. These included a focus on medication and equipment safety, the need to develop personalised care plans further for patients, and to ensure thorough processes were undertaken to support patients with cognitive impairment to make decisions regarding consent to treatment. A number of other suggestions to enhance the care we provided were also made. Our staff responded to these challenges with enthusiasm and were justly rewarded for their efforts when the CQC revisited us in the autumn and found the organisation to be fully compliant with all essential standards of care. The CQC reported that we had responded positively to the findings of the previous inspection and that we had taken appropriate action to achieve compliance with essential standards. Staff felt that the action taken had made a positive difference. In January 2015 the CQC undertook unannounced Mental Health Act 1983 visits to Spencer and Riverside wards, part of our older peoples’ mental health services. These visits are part of the statutory inspection regime for services provided under the auspices of the Mental Health Act. Again, the caring attitude of our staff was positively reported. Some minor improvements in the management of patient records were identified. However, overall the services were evaluated extremely positively. As a pilot for the new style CQC visits, we were not rated as part of these inspections. However, a letter written to Monitor by Sir Mike Richards, Chief Inspector of Hospitals, supported us at DCHS to progress our ambition to become a Foundation Trust, which we achieved in November 2014. At DCHS we continue to develop our quality assurance processes and this will be driven through our Quality Always approach described in more detail later in this report. In addition we will continue to work to improve standards and implement suggested improvements made during CQC’s assessment, including embedding changes with regard to care of people with mental health conditions, specifically personalised care planning and ensuring effective consent for patients with limited capacity. We will continue to strengthen our arrangements for clinical supervision and care planning for all our patients. Ensuring safe staffing levels is a key priority for us and with our commissioners we will continue to review demand and ensure staffing levels reflect national best practice standards. DCHS has made the following progress by 31 March 2015 in taking such action. Older people’s mental health We have reviewed and implemented new documentation to improve personalised care planning, improved training opportunities for staff with regard to the Mental Health Act, including taking consent from patients with limited capacity, and reviewed our service level agreements with partner organisations. Policies underpinning practice have been reviewed and staff supported in their implementation. We have developed our strategy of care for patients with dementia and are now taking this for approval through our governance processes. Medicines management We have strengthened our governance arrangements regarding medicines storage and revised the processes for monitoring and assessing patient group directions. Improvements in medicines management have been evidenced through achieving our patient safety objective for 2014/15, during which time we had no medicines management incidents resulting in serious harm to patients. Equipment management We have reviewed and strengthened arrangements for checking medical equipment. Estate management We continue to manage our estate to ensure that it meets the needs of our individual patient groups, protects our patients from harm and affords them privacy and dignity as appropriate. During the year improvements included refurbishing the ward at Whitworth Hospital to ensure it provides a dementia friendly environment, and improvements to roads and crossings at Walton hospital in Chesterfield. Safe staffing Ensuring we have the right number of staff with the right skills to meet our patients’ needs is an essential foundation for good care. We have reviewed the number of nurses for our inpatient wards, in line with national Safer Staffing guidance, and we monitor this on a continuous basis, 9 reporting centrally through the Unify System. We are participating in work nationally to agree safer staffing levels for other community services including community nursing, health visiting, learning disability services and mental health services. We have completed a review of workload and skill mix with our community nursing teams and are working with our commissioners to agree appropriate staffing levels, based on the acuity of the patient caseload. We are rolling out our e-rostering tool and associated Safe Care acuity tool which facilitates assessment of patient acuity during the 24-hour period. As a consequence of this work we are able to provide assurance to our patients and their carers that we have the right staff on duty to meet their needs, which is evidenced with ward-based staffing boards indicating required and actual staff on duty at any given period. Clinical supervision Staff development events regarding clinical supervision have provided advice and guidance on the value of supervision and the need for clear documentation. Participation in clinical supervision is now linked with annual appraisal. Documentation in patient records Documentation of risk assessment processes have been streamlined to reduce the bureaucratic burden and to support personalised care planning. We are working towards migration of documents onto our electronic patient care system and continue to audit records on a regular basis to ensure they meet the required standard. This has demonstrated that there has been significant improvement in personalised care planning and management of consent with patients. Quality governance and assurance Our new quality improvement and assurance model has been introduced and we are rolling out our Quality Always peer assessment and assurance programme across the organisation. We have invested in a series of workshops for clinical staff to ensure they understand the purpose of the programme and their role within it. . DCHS has not participated in any special reviews or investigations during the reporting period. Secondary uses service data DCHS submitted records during 2014/15 to the secondary uses service for inclusion in the Hospital Episode statistics, which are included in the latest published data. The percentage of records in the published data up to and including March 2015: which included the patient’s valid NHS number was: 100% for admitted patient care 100% for outpatient care 99.3% for accident and emergency care which included the patient’s general medical practice code was: 100% for admitted patient care 100% for outpatient care 100% for accident and emergency care Information governance DCHS’ information governance assessment report overall score for 2014/15 was 73% and was graded green from the IGT grading scheme). 95.8% of staff completed information governance training in year. Further detail on our information governance toolkit score can be found at appendix 2. Clinical coding audit DCHS was not subject to the Payment by Results clinical coding audit during 2014/15 undertaken by the Audit Commission. 10 Part 3 Review of quality improvements for 2014/15 Commissioning for Quality and Innovation (CQUIN) For 2014/15, at DCHS we jointly agreed nine CQUIN measures with our commissioners, demonstrating our continuous commitment to improving services in terms of quality outcomes for patients, carers and service users. These quality indicators support and ensure ongoing innovation and improvement across all of our services and in defined areas of clinical care. The nine CQUINs were classified into three national, one regional and five local improvement areas. The three national areas were: Friends and Family Test (FFT) - we have been an early adopter of the Friends and Family Test initiative and have promoted its use across all services as an integral part of our patient engagement strategy, as well as asking our staff the FFT question through the annual staff survey. Feedback from the FFT has helped us to improve our services in line with user expectations. NHS Patient Safety Thermometer - the national safety thermometer tool requires us to collect data on four ‘harms’ related to patient safety, in order to understand better how often these harms occur and to put into place strategies which prevent or minimise harm in the future. The four harms include: venous thromboembolisms (VTE), falls, urinary tract infections and pressure ulcers. Training in dementia awareness - during the last year our primary focus has been on training community staff, in conjunction with providing support to carers of patients with dementia through the First Contact referral initiative. Whilst fully supported across our inpatient wards, the First Contact approach has been particularly successful across our community services, championed by our care coordinators who support patients and carers in the community with regard to admission avoidance and in receiving the care they need following discharge from hospital. The regional CQUIN was: Improving patient experience and complaints - we committed to undertaking a peer review of our complaints standards and processes against the national Patient Association methodology in order to highlight areas for improvement. The outcome of the report demonstrated that the complaints reviewed were satisfactory, with one complaint reviewed as demonstrating good practice. The five local targets were: Pressure ulcers - our community nursing services undertook a review of how our staff engage with patients in preventing the development of pressure ulcers with a view to understanding why this is not always successful. Supporting work included patient interviews, a review of equipment and the development of comprehensive guidance and documentation for patients and staff. We are continuing to work with staff to embed lessons learned and improve practice. A DVD is being produced to support staff training. Compassion and culture – we are committed to delivering against the national agenda for the provision of compassionate care as part of embedding positive culture and values across the organisation. A number of work streams were developed which aimed to enhance our patients’ experience of compassionate care across the organisation. These included developing a valuesbased recruitment process, commencing the roll-out of our Quality Always model of accreditation for our inpatient wards and promoting the work of our Care Makers. End of life - following the national review of the Liverpool Care Pathway and its subsequent replacement with a new End of Life ‘toolkit’, DCHS committed to supporting staff in understanding how to enhance and deliver quality care in the last days and hours of a patient’s life within the new framework. This continues to be supported by a comprehensive training programme and crossorganisational workshops. Community nursing - staffing for quality - this CQUIN focused on an innovative and comprehensive review of activity across our Community Nursing services in order to determine 11 what safe and effective staffing levels are required to ensure consistent quality of care for patients. Specifically we considered: the time required to deliver quality care; what the patient need is in terms of acuity and dependency, and what the available nursing resource, skill mix and training requirements are across the county in relation to the demand. This important piece of work will help shape the future community models across Derbyshire in 2015/16. Discharge planning and patient flow - we continued the good work started in 2013/14 in improving the quality of our patient discharges, the flow processes and practices across organisations within the local health community. This has included sharing of best practice, strengthening communication across different organisations and supporting a joined-up approach to developing solutions to common challenges. Working as part of the wider health and social care system we have been able to improve the safe discharge of patients from acute care and ensure that the emergency care system works in an optimal way. Developing services responsive to our patients’ needs Evidence of quality improvements for 2014/15 This section describes in more detail our successes during the last year. We are also keen to present examples of where we could do better, to ensure we give an open and balanced account. To help understand this information we have presented this in the following sections: What have we done to improve patient safety? Safe care and the safety thermometer We continue to contribute to the national Harm Free Care agenda and monitor and report on a monthly basis using the patient safety thermometer which looks at prevalence of the four harms on a fixed day each month. The four harms are: falls, venous thromboembolism, tissue damage and urinary catheter infections. 2014/15 Harm free care scores (Target for year 93%) Across DCHS 92.37 Rehabilitation wards 87.22 Older people’s mental health wards District nursing Learning disability services 100 92.65 100 12 The table above illustrates our overall harm free percentage score of 92.37%, as well as the scores for different services we provide. Unfortunately we fell just short of our overall improvement target of 93% for the year with our rehabilitation wards failing the target primarily due to the number of patients with pressure ulcers being admitted to the wards, discussed further on page 15. Falls Encouraging patients to mobilise and maintain independence is a key objective of many of our services and it is to be expected that on occasion some patients may fall. However, this has to be managed in an appropriate way and the risk of injury from a fall avoided. Where injuries occur due to a fall, detailed investigations take place to identify the cause. In 2013/14 we identified that patients within our older people’s mental health services were more at risk of serious injury from a fall than those being cared for in a rehabilitation ward. As a consequence, during 2014/15, we improved access to physiotherapists for these patients and introduced a general physician to the team to support the work of the psychiatric doctors. Our general physician reviews all aspects of the patients’ care and pays particular notice to their medications, diet and fluids, mobility and the general wellbeing of individual patients to help improve mobility and balance. Last year we also improved staff falls training and personalised care planning and we are in the process of recruiting a falls prevention practitioner to work with our multidisciplinary team to improve our understanding of predisposing factors to falls and how they can be prevented. We are also introducing the use of robotic seals which have been found to reduce anxiety and agitation in patients with dementia, so reducing the risk of a fall. Across our rehabilitation wards we have introduced coloured wrist bands to identify those patients with a higher mobility need and those who are at risk of falling. Falls Partnership Service Managing falls is also a feature of our wider health community work. In November 2013 Hardwick Clinical Commissioning Group commissioned and launched a Falls Partnership Service (FPS) working collaboratively with us at DCHS and also East Midlands Ambulance Service NHS Trust (EMAS) and Chesterfield Royal Hospital NHS Foundation Trust. The FPS provides a fully integrated response to people over 50 years who have fallen in their usual place of residence. The FPS integrates into the emergency ambulance pathway and is provided as an alternative to an emergency ambulance crew attending the patient, following appropriate triage by ambulance control. The FPS also takes referrals directly from GPs. Between 1 April 2014 and 31 March 2015 633 patient referrals into the service were visited by the FPS team. 13 391 patients referred into the FPS team avoided a hospital admission and remained at home/usual place of residence following their fall. Between 1 April and 31 March 2015 the FPS attended: 283 callouts for EMAS, this is in addition to the 633 patients already referred into the FPS. In addition to this we can evidence that between 1 April 2014 and 31 March 2015 503 patients had not been admitted into hospital 30 days after their fall. The team can now admit directly to the Elderly Medical Unit and the Adult Reablement Unit when appropriate, thus avoiding unnecessary waiting times for elderly patients in A&E. The team liaises closely with the Clinical Navigation Team and Rapid Response Team at Chesterfield Royal Hospital to improve the patient pathway and ensure safe/timely discharge planning for patients who are admitted to A&E. They are also building links with the equivalent team at Kings Mill Hospital, part of Sherwood Forest Hospitals NHS Foundation Trust in Mansfield. Pressure ulcers Pressure ulcers caused by damage to skin integrity continues to be one of the most challenging areas of quality improvement for our clinical teams. There are a wide range of influencing factors which include input from a variety of care teams across the health and social care community, patient choice and compliance, ability to monitor and supervise in a home setting, use and availability of equipment. One of the key priority areas relating to quality improvement in 2014/15 was to reduce the number of pressure ulcers developing and/or deteriorating while patients are in the care of our staff. Operational managers at all levels and clinical teams were required to engage fully in the harm free care agenda – understanding their roles and responsibilities and to provide evidence to both our Trust Board and the wider health community. We set out to achieve zero avoidable pressure ulcers acquired under our care during 2014/15, caused by an omission in our care planning or delivery. Whilst we have seen improvements in a number of service areas unfortunately we have not yet achieved zero avoidable pressure ulcers across all of our services. We are continuing to see a downward trend in severity of the pressure ulcers developing within our care. It is also apparent that we are seeing a general reduction in pressure ulcers within the wider community as collaborative work with other agencies and the public is helping to increase awareness and ownership of the problem. It is believed that the majority of pressure ulcers are avoidable and we are determined to prevent harm to all of our patients, so we will continue to have pressure ulcer reduction as a key priority going into next year. From our analysis of incidents and data reporting we can see that clinical teams are being more proactive in ensuring all measures are put in place to avoid deterioration of ulcers and that improvements in root cause analysis by managers ensures that learning is shared across the organisation. Supported by our team of specialist tissue viability nurses, our multidisciplinary teams are working more closely together to ensure effective communications are in place to help promote continuity of prevention strategies. Through patient stories our Board of Directors is listening to the views of staff and patients and supporting initiatives that will help us improve and maintain individualised patient centred care. Through these patients’ stories we have raised our awareness of the issues that are important to our patients, which have included the use of equipment by patients at home. As a result we asked our Board Members to experience what it feels like to use such equipment so that we have a greater understanding of the impact on the patient’s ability to remain independent and mobile. This has prompted us to review our equipment catalogue to include alternative options based on what patients have told us about what they require. The chart below provides a breakdown of where the reported incidents of pressure damage within DCHS have occurred. We are working with other healthcare providers to identify how the number of patients 14 referred to our services with existing pressure damage can be reduced. It is anticipated that this number will reduce during 2015/16. The graph below clearly highlights that the majority of the pressure damage reported within DCHS occurs within our community-based services where there is less control of the patient’s environment. Our community services are working closely with patients, carers, family members and other organisations to increase awareness of how to prevent pressure damage occurring. This work is starting to take effect as the severity and size of the pressure damage has significantly reduced over the last year. Although the incidence within community hospitals is small, this is a controlled environment and further work is required to reduce this number even further. Percentage of pressure ulcers which developed or deteriorated whilst in DCHS care by service area The graphs below compare the incidence of avoidable pressure damage from 2014/15 to 2013/14. The root cause analysis process has highlighted that avoidable pressure damage usually occurs when: staff do not respond in a timely manner to a change in the patient’s condition and therefore, the plan of care does not always reflect the patient’s actual needs or staff have not checked the patient’s skin on a regular basis which would highlight any early signs of skin damage. 15 The teams involved in these patients are working to improve their response time and ensure that care does reflect patient need. Venous thromboembolism (VTE) Venous thromboembolisms are blood clots in major veins which can lead to serious complications. As a service we ensure all our patients at risk of VTE undergo an appropriate risk assessment and have a personalised care plan in place for avoidance of VTE. During 2014/15 we have seen very few VTEs, suggesting that our risk management strategies are appropriate. New VTE’s % Sample size Mar14 Apr14 May14 Jun14 Jul14 Aug14 Sep14 Oct14 Nov14 Dec14 Jan15 Feb15 Mar15 3 2 0 2 3 2 2 1 0 1 1 2 0 0.19 0.12 0 0.13 0.18 0.13 0.12 0.06 0 0.06 0.06 0.12 0 1593 1651 1618 1551 1647 1510 1622 1662 1617 1672 1677 1633 1614 16 Catheter related infections Some of our patients need help with continence which is supported by the use of a catheter. Catheters bypass the body’s natural defences against infection and therefore, if not managed carefully, can be a source of patient harm. At DCHS we minimise the use of catheters as far as possible, and where infections do occur we ensure that each case is carefully investigated to understand the cause. During 2013/14 there were 94 cases of catheter related infections and in 2014/15 this number has reduced to 55 cases. Medicines management The use of medicines to support and improve patients’ health is the most common medical intervention used within the NHS and as an NHS Trust we have a responsibility that this is undertaken by staff who have been adequately trained and who can practice safely. In DCHS we pride ourselves on the fact that we have a rigorous process in place that provides us with assurance that our staff follow safe medicines practice. Given the very large volume of medicines prescribed, dispensed and administered each day across our service it is inevitable that some errors do occur. Our high level of reporting in relation to errors is important and demonstrates that our staff understand the significance of errors and the opportunity to learn from errors when shared with colleagues. We are pleased to report that during 2014/15 at DCHS we have had no medication errors resulting in significant harm to a patient and that we have an excellent reputation for the reporting of near-misses from which we can review policies, procedures and training. All medication errors are reviewed for trends bimonthly by our medication safety team that consists of ward nurses, community nurses, pharmacists, prescribers and staff from our safety and learning teams. Following the identification that many of the administration errors were simply caused by ‘human error’, there was a widespread campaign within DCHS to remind all staff who administer medicines of the basic “5 Rights” of medicines administration. Figure: “5 Rights” of safe medicines administration Following on from this, our specialist diabetes nurses have created, with our workforce planning and development team a “5 Rights” card specifically for the administration of insulin. This is a diary sized information card that can be carried by our nursing staff, as an aide-memoire. To support this, specific training has been delivered to band 6 and band 7 community nurses reiterating safe insulin practice. In addition, the diabetes specialist nurses within the workforce planning and development team are developing an eLearning programme around diabetes and insulin administration for DCHS staff to access online. A bimonthly newsletter continues to be produced and distributed to clinical teams to update them of all current medication-related issues. These include local and national guidance, updated local policies or procedures and articles relating to medication training or audits undertaken. 17 National Institute for Health and Care Excellence (NICE) - technology appraisals relating to medicines All NICE technology appraisals related to medicines are discussed at the Derbyshire Joint Area Prescribing Committee, which has representation from all four local NHS Foundation Trusts and all four Clinical Commissioning Groups in Derbyshire. A decision is then taken to assign them with a particular traffic light status according to the Derbyshire medicines management system. This designatory status is related to whether they may be prescribed by practitioners in the community or reserved for prescribing only by specialists. Infection prevention and control Reducing the risk of infection and preventing cross infection continues to be an important aspect of our daily work in our hospitals and in the wider community. We continue to be monitored nationally on the incidence of methicillin resistant staphylococcus aureus (MRSA) blood stream infections (bacteraemia) and clostridium difficile infections. We are pleased to report that for another year there have been no MRSA bacteraemia (blood borne infection) reported within our services. Over the past year we have had 12 positive clostridium difficile infections diagnosed within our services. As of 2014/15, the 12 patients have undergone a review and, in line with new national guidance, any lapse in care identified. Of the 12 patients, we have identified five significant lapses in care which is 42% of those patients treated for clostridium difficile infection. The Infection Prevention and Control Team is working with the services to ensure that these lapses are addressed and do not recur during 2015/16. There are examples of good practice which demonstrate individualised care for patients with clostridium difficile infection. For example patients with dementia or who are low in mood due to the need to isolate to prevent cross infection. Norovirus Seasonal diarrhoea and vomiting caused by norovirus can have a significant impact on inpatient wards and care homes due to its highly contagious nature. The graph below shows how many norovirus outbreaks we have had this year. Each outbreak is reviewed and any lessons to be learnt shared across the organisation. The main trend identified relates to communication between the different services to ensure that the correct information is shared to enable effective and timely decision-making. 18 Hand hygiene compliance Our infection control champions have continued to promote good hand washing practice through regular audits and training sessions with their teams. We have seen a slight dip in performance when compared with last year, with the overall compliance rate reporting 99.22% against our target of 100%. We continue to work with the teams and infection control champions to ensure that good practice is consistently adopted across the whole organisation. Patient manual handling team Ensuring that our patients are moved safely, and our staff are protected from injury, is a high priority. Our specialist team work with our staff to ensure we provide our patients with equipment and promote techniques that are effective in supporting and maintaining their level of independence and safety when moving. Our specialist team have continued to see an increase in the number of referrals for the following specialist and complex care needs assessments: bariatric therapeutic special circumstances emergency handling dental 19 non concordance environment issues We have continued our ongoing work with our staff to reduce the incidence of musculoskeletal injuries by ensuring that they have the skills to assess patients’ needs and provide appropriate care. Training is designed to give staff the skills they need specific to their role. We have also invested in a new specialist bed for patients with complex care needs being cared for in our community hospitals, which will support staff to care for patients safely and provide an improvement to our wards. The specialist team and our clinical navigation service have reviewed our admission processes to effect a smoother transfer of patients into one of our community hospitals or services. Safeguarding children and adults Safeguarding our clients from actual or potential harm continues to be a fundamental responsibility delegated to all of our staff. The safeguarding team employs specialist safeguarding nurses who work with staff and patients to ensure that as an organisation we discharge that function effectively. During 2014/15 the safeguarding team has continued to provide specialist safeguarding training, advice and supervision for our staff. The key improvements this year include: bespoke safeguarding training that has been delivered to staff working in children’s services, minor injury units, learning disability services and older people’s mental health units delivery of the ‘Think Family’ national agenda via staff training and briefings. Think Family encourages staff to consider where there may be a risk to a child or vulnerable adult in a family where another adult is being treated external partnership work with partners regarding the Prevent agenda. The Prevent agenda raises staff awareness with regard to potential terrorist activity development of a Prevent policy an update to the safeguarding adults, children and security policy to reflect the issues raised by Sir David Nicolson in relation to the Savile Inquiry continued collaborative work with partner agencies, including projects focusing on domestic violence, substance misuse, safeguarding thresholds and IT solutions working with partner agencies on issues such as co-location arrangements of health staff in social care, attendance at court and legal meetings, multi-agency risk assessment conferences (MARAC), and multi-agency public protection arrangements (MAPPA) participation in multi-agency information sharing events such as the development of vulnerable adults at risk meetings (VARM) to discuss safeguarding cases the introduction of regular supervision and advice clinics for DCHS staff in hospital and clinic environments funding for ‘Best Interest’ assessor training for the safeguarding adult team Monday to Friday (9am – 5pm) safeguarding advice line for children and adult services funding of an additional safeguarding nurse to lead on the care home and community agenda establishment of a safeguarding governance group that reports to our Quality Services Committee. Patient safety Incident reporting Staff continue to retain a strong safety culture in relation to reporting patient safety incidents. This is assisted by the provision of a monthly report outlining incidents and risks which are due to be reviewed and which enable improvements to occur. More rigorous processes for review have been developed and risks now form a standing item for discussion within all directorate governance meetings. 20 The following data represents incidents reported from 1 April 2014 to 31 March 2015 and are based on all Patient Safety Incidents (not all of which have been reviewed and approved at the time of writing). “Never Events” During 2014/15 there have been no “‘Never Events” in services at DCHS. Never events are defined as incidents that are wholly preventable. During this reporting period 12 incidents were reported under the heading of “Never Events” as potential incidents, however, none of the incidents resulted in serious harm, due to being identified and mitigated in a short time period or because the error had no trajectory to cause harm. Category Classification Details Number Actions Maladministration of Insulin Near miss Never Event All incidents had potential to cause harm though did not result in actual severe harm. 9 The MOST group reviews all medication incidents and checks that improvements measures identified in agreed actions are completed. Additional training has been implemented and numbers of incidence in the latter part of the year have reduced. Wrong route administration Near Miss Never Event No resulting harm 1 As above action Retained foreign object post operation Prevented Never Event No resulting harm 2 WHO theatre checklist actions were revisited and strengthened, including a revised check list with double checks in place. No further incidents. Quality checks The Patient Safety Team reviews every patient safety incident reported, providing quality checks which include: seeking additional detail or clarification; ensuring clear definition of incident and removing patient identifiers. The data is then shared with the National Reporting and Learning System (NRLS). A monitoring system is in place to check progress against identified root cause analysis to ensure completion within the risk management policy timeframe. Table 1: During the reporting period, a total of 9,559 patient safety incidents (PSIs) were reported, of which 8,917 (93%) resulted in no or minor harm; 632 (7%) resulted in significant harm (262/43% of these were inherited incidents i.e. pressure ulcer incidents observed on admission to DCHS); and 8 (0.08%) resulted in major harm; these related to Grade 4 pressure ulcers. There were 2 (0.02%) catastrophic incidents reported, one relating to notification of an infant death and one death of a deteriorating patient on a ward (this was subsequently deemed not to be a patient safety incident as the patient’s death was anticipated and all care measures were in place). Table 1 Incidents by severity No injury or harm Minor harm/injury Significant harm/injury Major harm/injury including permanent disability Death or multiple deaths or catastrophic event affecting DCHS (e.g. flood/fire) Totals: 3756 5161 632 8 2 9559 21 Table 2 below illustrates the top five reported incidents and trends over the past three years. Incidents by category 2014/2015 Pressure relief care Slips, trips and falls (patient) Injury or damage to skin (not pressure ulcer) Medication Ambulance/taxi transport issue Totals: Incidents by category 2013/2014 3,941 1,186 573 457 398 6,555 Pressure relief care Slips, trips and falls (patient) Ambulance/taxi transport issue Violence/abuse/ harassment Medication Totals: Incidents by category 2012/2013 3,705 1,456 659 615 528 6,963 Pressure relief care Slips, trips and falls (patient) Ambulance/taxi transport issue Violence/abuse/ harassment Medication Totals: 2,577 1,544 624 525 404 5,674 Pressure relief care - there has been a 12.4% increase in reported pressure damage compared to the same period in 2013/14. Some of this will be related to improved awareness and a resultant increase in reporting as our training and education programme raises awareness amongst clinical staff. We also know that our staff are treating more and more patients each year, with ever increasing numbers of frail and elderly patients. Significantly, 53% of incidents relate to inherited pressure ulcers i.e. those occurring prior to admission to DCHS care. Focused and dedicated care improvements, support and monitoring is provided to clinicians by the specialists within the Safe Care Group including improved access to the tissue viability nurse specialists, and work continues in partnership with our commissioners to address wider public health and health economy issues. Ambulance/transport /taxi issues - there has been a 25% decrease in reported incidents related to transport issues. It is difficult to determine if care by ambulance transport providers has improved or whether staff have reduced reporting due to awareness that concerns are being addressed. The current service is subject to a competitive tender at the time of this report being written and the trust will continue to monitor performance against contractual standards. Violence/abuse/harassment - there has been a marked decrease (46%) in reported incidents related to patient violence and aggression. This is attributed to improved staff/patient ratios, resulting in improved levels of observation by staff, increased anticipatory/intervention measures and a reduction in the numbers of inpatients. Table 3 shows the number of falls reported in 2014/15, compared with 2013/14, has reduced overall by 18%. Improvements made following Root Cause Analysis include increasing medical and physiotherapy provision in our older people mental health wards, ensuring the continued acuity of patients is met, and the introduction of a wristband scheme which alerts staff to patients at risk of falling. Initiatives to be introduced include using Paro seals which are a therapeutic robot baby harp seal, intended to have a calming effect on patients and elicit emotional responses from them. 22 Table 3 Falls incidents by severity 2014/15 No injury or harm Falls incidents by severity 2013/14 713 Minor harm/injury No injury or harm 907 Minor harm/injury 440 Significant harm/injury Major harm/injury including permanent disability Death or multiple deaths or catastrophic event affecting DCHS (e.g. flood/fire) Totals: 33 0 0 1,186 519 Significant harm/injury 27 Major harm/injury including permanent disability 3 Death or multiple deaths or catastrophic event affecting DCHS (e.g. flood/fire) Totals: 0 1,456 Risk management and protecting quality The Risk Management Policy has undergone a periodic review with significant assurance received from 360 Assurance for the risk management processes in place. The review has streamlined and strengthened areas of responsibility to enable improved understanding and implementation of policy contents. Additional to this, to assist in achieving increased awareness and ownership, each assistant director receives a monthly report of all open risks for their directorate (excluding BAF) - to confirm and challenge that risks are being reported, escalated and appropriately addressed. The head of patient safety & risk management attends the director of operations’ senior management team monthly meeting where there is a dedicated risk management review session. Each governance stream has both incidents and risks as a standing item on governance meeting agendas. New last year was the introduction of a quarterly Quality Services Committee meeting to provide opportunity to review the whole risk register and provide additional confirm and challenge to operational services. Incidents are being mapped to ensure that risks appropriately reflect areas of concern. Risk management is based on a fair culture that encourages an organisation-wide environment of openness and learning. Training & other patient safety resources Following popular and very good evaluation, root cause analysis and risk management training continued to be provided by the patient safety team during 2014/15 and will continue to be available on a monthly basis with additional and bespoke sessions arranged as required. There is currently a dynamic and interactive eLearning risk management package being developed which is anticipated to be launched in the Spring of 2015 this will increase the opportunities for staff to improve their risk management knowledge base. Central Alert System & STEIS The Central Alert System (CAS) is a national reporting system alerting health organisations to safety issues. During 2014/15 a total of 170 alerts were received, only 39 (23%) applicable to us at DCHS. Each alert was distributed and followed up without any breeches occurring in meeting any required actions and or deadlines set by NHS England. During 2014/15, 204 serious incidents have occurred, with a formal root cause analysis provided to the CCG. Actions and recommendations from root cause analyses are disseminated through our Learning the Lessons group. 23 Table 4 Central Alerting System 1/04/2014 to 31/03/2015 Alerts Received During Period Total Relevant 22 Not Relevant 23 On-going Response not required Medical Devices Alerts (MDA) 53 8 Chief Medical Officer Messaging 9 Estates & Facilities Notification (EFN) 59 Drug Alerts 19 19 MHRA Dear Doctors Letter 3 3 NHS England PSA 17 TOTAL 160 9 7 10 50 6 2 1 Table 5 STEIS Reportable Incidents 01/04/2014 to 31/03/2015 C. Diff & Health Acquired Infections 1 Communicable Disease & Infection Issue 8 Delayed Diagnosis 1 Pressure Ulcer Grade 3 134 Pressure Ulcer Grade 4 12 Slips, Trips & Falls 29 VTE TOTAL 9 194 24 Ensuring services are clinically effective Clinical effectiveness We ensure that the services we provide achieve meaningful outcomes for patients and carers in a variety of ways: Clinical audit - measures care and treatment against established standards Service evaluation - monitors how well a service delivers care and treatment Evidence-based practice - ensures that care and treatment follow proven best practice Patient outcomes - measures improvements in the health and well-being of the people who use our services We have maintained a commitment to improve patient outcomes through the use of clinical audit. This approach has also influenced service improvements. One of our audits in 2014 involved a review of wheelchair use. The results from this audit enabled us to develop our staff training to improve the safe use of wheelchairs. Audit continues to influence the care of our patients at the end of their lives and ensures we achieve the highest standards at this very sensitive time. To ensure that the individual needs of our patients are met we audit the records of patients who receive End of Life Care. We will continue to develop the concept of clinical effectiveness within our services. This will ensure our patient care is led by clinicians and continues to be effective and responsive. We will improve the way we measure the outcomes of treatment. National clinical audits The following national audits (from the NCAPOP list for 2014/15) have been selected as relevant to the clinical services provided by DCHS. We participate in far fewer national audits as a community trust compared with an acute trust, as the programme has historically been biased to acute services, though this is now changing as the NCAPOP list broadens to include more audits on long term conditions (e.g. the national COPD audit), or existing audits broaden their scope (e.g. the Sentinel Stroke Audit). This year we are participating in six national audits, compared with only two we joined last year. Some outcomes from these audits are not yet available at the time of this report. Ref number (DCHS Priority Audit Programme) 17 18 Audit title Percentage of cases submitted National COPD Audit – Rehabilitation Clinical Audit and Rehabilitation Organisational Audit parts of this programme No data available as the clinical audit started in January 2015 and will complete in July 2015 Sentinel Stroke National Audit Not yet participating. Outcome if known Actions to be taken This audit has just commenced and the results will not be available till September 2015 for the clinical audit and November 2015 for the organisational audit No data yet submitted. Data collection for both parts of the audit has commenced. Scoping of services to include in this audit is underway. We are also identifying the workload implications for clinicians collecting and inputting audit data, before registering to participate. 25 Ref number (DCHS Priority Audit Programme) 19 Audit title Percentage of cases submitted Outcome if known Actions to be taken Quarter 1 and 2 results show low levels of participation therefore the clinical improvement information is too small to be acted on yet. Our trust has maintained our position of generally being in the middle of the range of national benchmarks reported for this audit. Improvement is expected when the Q4 results for 2014/15 are published, following an action plan to increase patient participation. We will review our future participation in this subscription audit as our service models for Intermediate Care are changing and it is not clear how we can use the data collected by this audit to improve our services. National PROMs Programme Result to end of Q2 less than 15% of Groin Hernia surgery patient participated at our Ilkeston Day Treatment Centre. 20 National Audit of Intermediate Care – organisational audit. N/A for the organisational audit. 21 National Diabetic Foot Care Audit No data yet available as this audit started in July 2014 and will complete in June 2015 This audit has recently commenced in Podiatry services and Report due in March 2016. To ensure that the results are fed back to DCHS Podiatry services and any improvements required are planned for. 22 NCEPOD Sepsis Audit There was a pre-set sample of 13 questionnaires from the audit organisers for DCHS No outcomes have been reported to the DCHS by the audit organisers yet. To ensure that the results are fed back to DCHS Medical and Nurse prescribers and any improvements required are planned for. Local clinical audits The reports of 19 local clinical audits were reviewed by the provider in 2014/15 and DCHS intends to take the following actions to improve the quality of healthcare provided as summarised within the clinical outcomes/recommendations column. Reference No DCHS priority audit programme 1 Audit Title End Of Life Progress against Audit Plan A revised audit tool for Community Nursing and Inpatients was launched in Oct 2014 to reflect the 5 Priorities of Care. Data collection continuing. Reports quarterly to QSC. Findings shared with End of Life Group, CIPP, ANP, Clinical Outcomes / Recommendations Q4 report received. 100% of audited deaths in community hospitals were expected deaths. Recommendations – Attendance at team meetings to improve completion of audit within Community Teams. EOL audit to be tabled at ICM meetings. 26 Reference No DCHS priority audit programme Audit Title Progress against Audit Plan Clinical Outcomes / Recommendations Matrons and ICM meetings. Explore integration of Recognising Dying Form within Community teams. Increase attendance at Individualised Care Planning training. Case note review of sepsis patients. 2 Falls Prevention Core data collected as part of the Clinical Records Audit. This to be integrated into the broader Falls report re Falls Bracelets Project and tracking incidents via Datix. Audit Report due May 2015. Falls wrist band project to be rolled out across all wards. Q4 data shows improved scores on many of the indicators, e.g. asking patients about recent falls and including information on falls in ward discharge letters. 3 Frail Elderly Clinical Records Audit of small sample to look at outcomes from care plans proposed. Reviewed Mar/Apr with Locality Managers for Chesterfield and NE Derbys, in view of move to "hub" approach to re-evaluate the audit plan for 2015/16 programme. Audit in planning stage. No timetable set for reports. 5a Mental Capacity Act (previously OPMH) Case Notes Audit Data collection completed for OPMH/LD inpatient and residential services. DoLs audit questions have been added to Case Notes audit tool for rollout. New timetable for rollout of audit and re-audit of OPMHH agreed with ICBS Quality Team for 2015/16 programme. Results show high level of assurance re process, but variable recording and need for staff guidance re Best Interests Decisions involving degrees of restriction. Re-audit planned for Q1 2015/16. Rollout to other sectors is in planning. 5b Mental Capacity Act (previously OPMH) DoLs Audit Data collection completed, Final report received from Helen Head/Margaret ParryHughes Report shows need to improve recording and review of DoLs in OPMH inpatient wards. Now part of the Case Notes Audit. 5c Mental Capacity Act (previously OPMH) Carers Experience Recruitment of Carers on OPMH/LD inpatient and residential services is ongoing, but failed to recruit any patients in the audit period. Now being extended to end of Q4. Report rescheduled for Q1 2015/16 from Patient Experience Team 5d Mental Capacity Act (previously OPMH) Amcat Staff asked to use MHF Amcat tool after MC assessment. Rollout as per clinical records audit. Data requested for Report rescheduled for Q1 2015/16 due to data quality issues with download from MHF. 27 Reference No DCHS priority audit programme Audit Title Progress against Audit Plan Clinical Outcomes / Recommendations analysis up to end of November. Issues with data quality in report from MHF. 6a Medicines management controlled drugs management Data collection ongoing. Q4 report due May 2015. A new way of scoring the CD audits has been agreed at the Matrons’ meeting and this will be used in the Q4 CD audit report. This will grade the standards according to risk, so some standards may be breached a small number of times without the ward or department failing the complete audit. The results are now in and the report is currently being written and will be presented to the Matrons’ meeting on June 8th 6b Medicines management treatment cards Reporting twice a year, data collection ongoing. Second report for 2014/15 due in May 2015. The Q4 treatment Card audit results are currently being collated and will be presented to the Matrons’ meeting and also discussed with the Medical Director and the Clinical Assistant with regards to the standards of individual prescribers. This report will be completed during June 2015. 6c Medicines management omitted doses Rolling audit reported to Inpatient Matrons Group. Second report for 2014/15 due in May 2015. The Q4 Omitted Doses report is currently being written by the Head of Medicines Management, in conjunction with Quality Always and will be presented to the th Matrons’ meeting on June 8 . 7a Control of Infection antimicrobial prescribing Q4 Community Hospitals Report The indication was recorded in the medical notes for all the courses prescribed. The indication was recorded on the treatment card either by the prescriber or the ward clinical pharmacist for 10 of the antibiotic courses prescribed (71.4%) which shows increased compliance with the “Start Smart then Focus” guidance compared to the previous audit where for 68.4% of the courses the indication was recorded on the treatment card. More detailed finds are detailed within the clinical effectiveness reporting system. Completed. 28 Reference No DCHS priority audit programme 7b Audit Title Control of Infection Progress against Audit Plan Data collection ongoing. Q4 report completed. Hand Hygiene Clinical Outcomes / Recommendations 96.05% of services reported 100% hand hygiene compliance which is an increase of 1.27% from Quarter 3 2014/15. Of the 68 services/teams involved in the hand hygiene audit programme 30 services are completing audits in line with the IP&C requirements. The managers of the remaining 38 services/teams who currently have audits outstanding have been notified and are monitored via the IP&C Committee. Some of the difficulties have related to staff changes and training of replacement Champions. 7c Control of Infection Data collection ongoing. Q4 report completed The majority of patients are isolated in a timely manner. Delays have occurred where symptoms were initially attributed to an underlying bowel condition and, in one case, the patient’s symptoms commenced late at night and to isolate the patient would have involved moving other sleeping patients. Training on IP&C issues will continue as part of mandatory programme Isolation audit 8 Clinical Records Data collection ongoing. Q3 report due in February 2015 now overdue. Q4 report is due in May 2015. Q2 sustains the Q1 improvement by a further 2% in overall scores to 76%, also reflected in the Q2 "core legal questions" score. Standard 6 (re completeness of the record) remains the lowest scoring standard, and work is ongoing to support clinicians to reduce ambiguity over the meaning of incomplete sections of forms. The rollout of electronic records is thought to have contributed to this sustained improvement. 12 Identifying LD Patients Plan to a) identify services using TPP LD flag, b) identify equities data re LD in CRA, c) set up rolling quarterly records audit of 5 services drawn from where LD flag in use in TPP, sampling just LD patients, brief set of questions looking at adjustments (including categories of adjustments The Commissioners target of 95% of audited records showing a full care planning cycle for reasonable adjustment for people with a Learning Disability has not been met. Issues identified including how reasonable adjustments for an LD are included in a care or treatment plan, confusion over identifying an LD, and ensuring 29 Reference No DCHS priority audit programme Audit Title Progress against Audit Plan Clinical Outcomes / Recommendations made) and recording of LD in records. that all electronic records have the right documentation. Audit working group to address these issues. This will become one of DCHS BIG 3 quality initiatives for 2015/16 13 Equality and Diversity Data collection ongoing. This year's overall result of 65.5% shows an 8% improvement over the 2013/14 results, particularly for identifying transgendered patients, though this remains relatively low compared to the higher scores for other questions for gender and sexual identity and identifying disabilities. 14 Safeguarding Children Markers of Good Practice Self-assessment completed through the year Report by end of Q4 15 Safeguarding Vulnerable Adults Assessment Framework Self-assessment completed through the year Report by end of Q4 23 Antipsychotic Audit Registration Form with plan and audit questions based on the POMH antipsychotics audit agreed with MH trust medics. Jnr DRs on OPMH wards collecting data. Data to be analysed in May 2015. Report due in June 15 Research and development The DCHS research team provides support to staff across the Trust, to Derbyshire County Public Health Service and the four local CCGs. We work in partnership with other key research organisations in Derbyshire, including: Collaboration for Leadership in Health Research and Care – East Midlands Clinical Research Network East Midlands Derby Hospitals NHS Foundation Trust East Midlands Academic Science Network. In 2014/15 DCHS patients have been recruited to the following national research studies which were approved by a research ethics committee: Dementia and Imagination - 11 Nourishing Start for Health (NOSH) - 3 Electrical muscle stimulation dysphagia study - 3 Big CACTUS - A study to assess the clinical and cost effectiveness of aphasia computer treatment versus usual stimulation or attention control long-term post-stroke 2 DCHS has also participated in the national guidance for measuring assistive technology, domestic violence and women with learning difficulties studies, which involve clinical staff. 30 All these studies are on the National Institute of Health Research portfolio. This means that this research is seen as having national significance. A total of 23 clinical staff participated in these projects. They work in three specialties within DCHS: speech and language therapy, older people’s mental health and health visiting. In addition in the NOSH study 15 health visitors attended an induction session. The project research team was invited to attend a Chesterfield health visitor general meeting on two occasions to give brief presentations, one introducing the project and one giving a brief summary of feasibility findings. A further four portfolio studies are in the process of being approved or set up at the moment. Comprehensive geriatric assessment CODES - Cognitive behavioural therapy vs standardised medical care for adults with Dissociative non-Epileptic Seizures: A multicentre randomised controlled trial Rehabilitation of memory following traumatic brain injury Confidence after Stroke Measure. Our participation in clinical research demonstrates our commitment to improving the quality of care we offer and to making our contribution to wider health improvement. It means that our clinical staff are more likely to stay up-to-date with the latest possible treatments and we know that active participation in research leads to successful patient outcomes. In addition, work continued on another local study which was approved by a research ethics committee. This concerned a financial incentive to stop smoking in pregnancy, the project involved DCHS stop smoking staff, the research team and midwives from Chesterfield Royal Hospital NHS Foundation Trust. Focus on dementia Our clinical strategy has a key work stream on dementia care and to underpin this we have participated in a local research project ‘Dementia and Imagination.’ This £1.2 million national research study, aims to improve the quality of life of patients with dementia by helping them to engage, or stay engaged, in social activities and relationships through a visual arts intervention. The project delivers 12 weekly sessions of arts-based activities, specifically designed for people with dementia. The study has taken place on two inpatient wards in two hospitals in Derbyshire, as well as involving patients from the community via a day unit. The sessions are facilitated by trained artists and include the display and discussion of current exhibitions at Nottingham Contemporary Gallery, one of the research project partners.. The sessions engage participants in thinking and discussing various artworks, before all are invited to create their own works of art using a wide variety of media and techniques. At the end of each 'wave' of sessions, a community exhibition takes place in order to engage the public in thinking about dementia in more dementia-friendly ways. We hope that this work will be seen as best practice across the health and social care community and influence the way in which future services are commissioned. 31 What we have done to improve patient experience? Caring Always - The DCHS Experience During 2014/15 we worked with patients, staff and our public governors to agree eight promises about what it should feel like to use our services. We call these promises ‘Caring Always’. 1. During your time with us you will feel welcomed and valued. You will feel that your care meets your individual needs. 2. You will have the opportunity to discuss with us what is going to happen at every stage. 3. You will understand the choices that you can make about your care. You will be supported to make the best choices for you. 4. You will have all the support you need to feel comfortable and safe. 5. You will know who is providing your care and what to expect. You will have clear information about how and when they can be contacted. 6. You will feel confident that you are being looked after by well trained staff who have the time to care. 7. You will feel able to choose how much we involve your family, friends and carers. 8. You will feel able to tell us how we could improve. Feedback The promises inform patients and their families on how they should expect to feel. We ask them to feedback to us about how we keep those promises. We can use their feedback to make improvements. There is a growing number of ways for people to give us that feedback: • By telling any of our staff • Friends and Family Test (FFT) • Contacting the Patient Experience Team – by phone, email or through the DCHS website • By making a formal complaint • A new ‘Raising Concerns’ App • By telling their story • Through a follow-up phone call after discharge from hospital • Online: using Twitter, Patient Opinion, NHS Choices, or our DCHS website • Through a patient participation or service user group • Through Healthwatch Derbyshire. We are proud to say that of the 24,809 patients who completed the Friends and Family Test this year, 97.2% said that they would recommend us to their friends and family if they needed similar care or treatment. We also asked patients to tell us about their experiences and how we could improve the services they used. The comments we receive are used to make improvements in local services and are shared across the organisation through “You Said, We Did”. 32 Examples of improvements are given below. 33 A plan for Carers has been developed and further improvements in the way we support carers will be made in the year ahead. Complaints Responding to patients and carers whose expectations of service have not been met continues to be a priority for us at DCHS. During the year we have worked on improving our complaint response times and the content of our responses. Every complaint or concern is handled by the patient experience team in accordance with the Local Authority Social Services and NHS Complaints (England) Regulations (2009). The patient experience team supports complainants through the process, in line with principles of good practice published by the Parliamentary and Health Service Ombudsman and endorsed by the Local Government Ombudsman. During 2014/15 the patient experience team received and responded to 583 enquiries, concerns and complaints compared with 627 in 2013/14 (these figures have not been adjusted for any change in our service or activity). Of these, 118 complaints required an investigation under the NHS complaints process. Four complaints were referred to the Parliamentary and Health Service Ombudsman, two of which have not been upheld and we are awaiting the outcomes of the remaining two investigations. 34 Of the 118 complaints received 57% related to all aspects of clinical care, 11% related to appointments and 14% related to communication. At DCHS we are continuously making improvements to the way we manage complaints so that we learn lessons and provide effective support to people who have made a complaint. The second Francis Report (2013) gave us further opportunities to improve our management of complaints and support for people who want to raise concerns about our services. In line with new national guidance we have participated in our first External Complaints Peer Review Panel held during November 2014. We were pleased with the overall results of this first peer review which stated “It is exceptional that Derbyshire Community Services NHS Trust demonstrated satisfactory practice or above for all six complaints” This worthwhile process will continue to be developed in conjunction with our commissioners and will continue to support us in driving up our performance in relation to management of complaints. Friends and Family Test (FFT) DCHS continue to perform well with regard to the question “Would you recommend this trust to your friends and family?” We take feedback across all our services on a monthly basis and have worked specifically on getting feedback from some of our harder to reach groups including children and patients with a learning disability. Patient stories Patient stories are a rich and valuable source of feedback from our patients and their carers and are used regularly across the organisation including at our monthly Trust Board meetings, quality service committee and safeguarding meetings. This year we have also introduced a staff story at our quality people committee to learn more about the support our staff have received and need. These stories provide a platform for sharing learning across our organisation and further afield and have been used to inform partner organisations and our commissioners of service user needs. Dignity in Care DCHS continues to work with Derbyshire County Council (DCC) towards its Dignity in Care awards Currently we have 67 bronze services engaged in this scheme which drives improvement in dignity in care and is assessed independently by colleagues from our CCG and DCC with 19 services currently 35 working towards it. During 2014/15 five teams have achieved their silver dignity in care awards and six further teams are working towards it. PLACE 2014 NHS England recommends that all hospitals providing NHS‐funded care undertake an annual assessment of the quality of non‐clinical services and the condition of their buildings. These assessments are referred to as Patient‐Led Assessments of the Care Environment (PLACE). Our assessment teams consisted of patient assessors and staff assessors of equal proportion (i.e. 4 plus 4). The CQC will use data from the PLACE collection in formulating Quality and Risk Profiles of DCHS as a healthcare provider. Scores summary for DCHS for 2014 The percentage scores for each category below have been awarded by the NHS Information Centre based on the information returned by us for 2014 Assessments. Cleanliness Food Privacy & Dignity Condition & Maintenance Ash Green 99.91% 92.86% 86.93% 97.59% Babington 98.76% 97.47% 91.83% 91.88% Bolsover 99.60% 97.45% 89.22% 98.00% Cavendish 99.78% 94.89% 81.80% 95.92% Clay Cross 99.72% 96.61% 80.47% 96.15% Ilkeston 98.75% 96.06% 91.83% 98.29% Newholme 99.79% 96.88% 87.20% 95.63% Ripley 99.35% 93.54% 92.61% 96.97% St Oswalds 100.00% 94.99% 94.15% 98.71% Walton 100.00% 90.83% 92.42% 95.08% Whitworth 99.78% 93.13% 85.20% 98.40% Hospital The overall scores for our hospitals were very favourable, as indicated below: DCHS overall organisational scores: Cleanliness Food Privacy & Dignity DCHS 99.59% 94.97% 88.51% Condition & Maintenance 96.60% National Averages 95.75% 85.42% 88.90% 88.78% All our hospitals have achieved a score above the national average for cleanliness, food, condition and maintenance. Food, nutrition and hydration August saw the national launch of the new NHS catering standards for patients and staff. We have reviewed the standards and agreed an action plan to address any shortfalls. One of the main changes we will be looking at will be the provision of catering services within the staff and visitor dining rooms and our vending machines, to ensure that we offer healthy eating options on all of our menus. 36 We continue to produce freshly cooked food using fresh produce from local suppliers. This year we have completed a number of food evaluations, including the supply to our community hospitals of fresh fruit and vegetables and the supply of fresh meat. In December new legislation was introduced relating to the presence of allergens in food. Patients, staff and visitors should be informed of the presence of any one of the 14 Allergens that could be found in the food prepared or bought in by external suppliers. We have reviewed how we cater for our most vulnerable patients who may be at risk of malnutrition. In order for patients to receive the assistance they require during mealtimes, we have reviewed our Protected Mealtime Policy to ensure that the mealtimes are protected and that a Registered Nurse is always available to supervise the meal service. We have also purchased new crockery and water jugs that are colour coded orange to identify patients who are at a risk of dehydration or who need nutritional support. We have undertaken a food evaluation of the textured modified food we supply for patients with swallowing difficulties to optimise the presentation, taste and overall quality of the food. We have recruited a nutritional nurse specialist, who offers support, advice and guidance to patients and clinicians. The nutrition nurse specialist has been concentrating on arranging the training for clinical staff around the Malnutrition Universal Screening Tool (MUST) and training relating to completing the nutrition treatment plans. Nutrition link leads have been established on all the wards, providing training and support through regular meetings. This will be extended out to our community teams over the next year. Making equality, diversity and inclusion a reality at DCHS As an organisation, we are passionate about people – our service users and our employees – and want to make a real and positive difference to people’s lives. DCHS’s vision for equality, as clearly stated in our Equalities Strategy, is that we are: ‘a healthcare community that promotes equality, values diversity and radiates inclusive practice in both employment and service delivery. We want to attract, recruit and retain a wide range of staff from all sections of society to work in a positive, inclusive and nurturing environment. We also want to deliver, with dignity and respect, inclusive and accessible services that meet our patients’ individual needs.’ Over the past year, we have made further progress in embedding improved equalities practice in everything we do. Some of our achievements include: Developed and signed off our new Equalities Strategy that clearly communicates our equalities aspirations for the future and how these will be achieved Created a new Equalities Action Plan, based on our priority objectives that were identified through public consultation. This is being actively performance managed by our Equality, Diversity and Inclusion Leadership Forum that reports directly to our Quality People and Quality Service Committees Developed two new equalities polices – our new Trans Equality Policy and Equality, Diversity and Inclusion Policy Established an Equalities Forum Theatre group, which has travelled across the County to deliver engaging and participative training sessions tackling issues of inequality and discrimination Procured equalities eLearning and created an ‘Introduction to Equality and Diversity at DCHS’ video that is being used for the induction of new employees into the Trust and at the Essential Learning which all employees undertake every 2 years. Continued to deliver our Sexual Orientation Equality Masterclasses across all service areas to raise awareness of homophobia, transphobia and heterosexism and to support staff to improve their equalities practice Delivered a training session on equality, diversity and inclusion to Public and Staff Governors 37 Worked with the British Deaf Association (BDA), local deaf forums and service users to sign the BDA’s British Sign Language (BSL) Charter Improved our approach to Equality Impact Assessments or Analysis so that it is undertaken for all key decisions that are relevant to equality Run sessions promoting the importance of equality monitoring to all staff as part of the Staff Briefing sessions delivered across the county Produced a comprehensive Workforce Equality Data and Analysis report (for 2013), a copy of which is available on our website Produced a Service User Equality Data and Analysis report (for 2013), which is also available on our website Undertaken a comprehensive equality analysis of our 2013 Staff Survey results, which resulted in additional equality related actions being embedded within the Trusts Staff Survey Action Plan Established a third Employee Network Group for our staff with a disability or long-term health condition; this brings our total number of groups to three, as we have already established groups for our lesbian, gay, bisexual and trans staff and our black and other ethnic minority staff. Membership of all three groups is open – and actively promoted - to equality allies, irrespective of characteristic, who are passionate about equality and want to help DCHS to achieve it Undertook a 360 Assurance review of our approach to embedding good equalities practice. This review gave the organisation significant assurance that the work being undertaken to progress the equalities agenda within the organisation is fulfilling its legal duties under Equalities Legislation and the requirements of Department of Health’s Equality Delivery System 2 Increased our ranking in the Stonewall Workplace Equality Index in 2014 (to 168th from 230th the previous year) Made further progress on embedding Health Care For All (HC4A) to improve our approach to providing services to people with a learning disability, and their overall experience of our services Celebrated LGBT History Month in February 2014 and commemorated the International Day Against Homophobia and Transphobia (IDAHO), and celebrated Black History Month in October 2014; Established our first Access to Healthcare Forum which is representative of all protected characteristics. This Forum will help us to check our equalities practice and identify new priority equality objectives and actions for 2015 and beyond. 38 Further information about DCHS’ approach to equality, diversity and inclusion can be found on our website at: http://www.dchs.nhs.uk/home/about/equalityanddiversity Picture of members of our Employee Network Groups Making every contact count Making every contact count (MECC) has been a successful initiative across DCHS since 2010, raising staff awareness of their responsibility to help patients, carers, families, friends and colleagues to adopt a healthier lifestyle. We have increased staff awareness of MECC by providing training and awareness raising sessions to over 3,500 DCHS staff. We have amended our documentation to make sure we can identify and audit MECC activity, which helps patients and staff to address lifestyle choices that are impacting on their personal health. We have evaluated training given to planned care services with very positive outcomes. The initiative is now truly embedded in the culture and ethos of the Trust with staff seeing MECC as part of their role. A team of staff participated in the DCHS Improving Leaders Capability Programme, were tasked with reviewing the MECC programme, within their own areas, and reported: ‘The conclusion was that MECC discussions were happening on a daily basis. We found that MECC was about changing attitudes and culture within teams – the importance of promoting health and conversations being individually tailored to patient needs. It was noted that MECC was not just a tick box exercise but about lifestyle choices, having everyday conversations about health promotion.’ Being a responsible employer we have used MECC to engage with our own staff and ensure that we provide them with the opportunity to improve their own wellbeing. DCHS received the Royal Society for Public Health (RSPH) Health and Wellbeing Award for three years (the highest classification) for the Trusts commitment to promote health amongst its workforce the impact this has had on staff wellbeing and attitudes to health. We were proud to be recognised nationally in 2014 by being shortlisted for the Nursing Times Award for Excellence in Supporting Staff Health and Wellbeing. Healthcare for All (HC4A) Throughout 2014/15 DCHS continued to monitor and seek to improve access to its services and processes for people with a learning disability. As in previous years our focus has been about improving the ways in which we identify service users with a learning disability and then assessing and making the necessary reasonable adjustments that that individual or their carer needs to ensure they achieve their optimum clinical outcomes along with the best healthcare experience possible. This is the essence of true ‘patient centred care’ and our approach in DCHS continues to be that reasonable adjustments, though essential for, are not just for people with a learning disability and should be identified, implemented and shared for all our patients as part of patient centred care and discharge planning. “Quality Always” and the DCHS “Equality and Diversity Strategy” together with the new “Equality Delivery System” are the mechanisms by which we now monitor how well we are doing and the delivery of improvements identified by individual services and the organisation. 39 The principles of “Healthcare for All” and how it fits with patient centred care remained a “golden thread” in our new Corporate Induction and “Fundamentals in Care” programmes for new staff and our “Essential” training programmes for new and established staff. In January 2015 DCHS participated in the Derbyshire Joint Health and Social Care Learning Disability Self-Assessment Framework and our Specialist Learning Disability Services lead on our input and commitment to the “Derbyshire Transforming Care” care concordant. Ensuring our services are responsive to patients’ needs DCHS monitors carefully the how its services perform with regard to waiting times and responsiveness to patients. During 2014/15, as part of our comprehensive monitoring dashboard, we have chosen three specific metrics to report on within our quality report. Minor Injury Unit waiting times DCHS has four Minor Injury Units providing urgent care as part of the wider out of hours and emergency care pathway across the health community. Ensuring our patients receive timely care is a key priority and this is measured against a four-hour standard set by the Department of Health. As the table below illustrates we have performed well in this area. DCHS considers that this data is as described for the following reasons: there are proper internal controls for the collection and reporting of this measure of performance and the controls are subject to quality assessment using the trusts data kite mark quality assurance system. 2013/14 Apr-13 May-13 Jun-13 Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14 2013/14 Outturn 4 Hour Wait for A&E Attendances (%) 99.8% 100.0% 99.9% 99.7% 99.9% 99.9% 99.9% 99.9% 99.9% 99.7% 99.8% 99.9% 99.9% 2014/15 Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15 Year to Date 4 Hour Wait for A&E Attendances (%) 99.5% 99.8% 100.0% 100.0% 99.9% 100.0% 100.0% 100.0% 99.9% 99.9% 99.9% 99.5% 99.95% DCHS will continue to monitor the quality of its services using its Quality Always framework and to work with the wider health community to maintain the high percentage performance within its minor injuries departments. Comparative Data A&E 4 Hour Wait It should be noted that DCHS emergency provision is limited to four minor injury units and that comparative data includes data from type 1 accident and emergency departments. Period Q3 2015/16 Q4 2015/16 Performance Rank Total In Cohort Nat. Average Highest 99.96% 73 247 95.0% 66 Trusts 99.94% 78 245 94.2% 67 Trusts Lowest Cambridge University Hospitals NHS Trust Hull & East Yorkshire Hospitals NHS Trust 40 Referral to treatment times When our patients need care we aim to see them and undertake their treatment as quickly as possible. The table below reports on our performance in year against the 18 week referral to treatment times and demonstrates that performance has been consistently good in all areas. DCHS considers that this data is as described for the following reasons: there are proper internal controls for the collection and reporting of this measure of performance and the controls are subject to quality assessment using the trusts data kite mark quality assurance system. The exception is in relation to RTT for the dental pathway where plans are in place to improve data collection and validation through 2015/16. 2014/15 Referral to Treatment Times Incomplete pathway (where treatment is part of a pathway) against a standard of 92% RTT Waits admitted patients seen within 18 weeks - 90% (target) (%) RTT Waits - non admitted patients seen within 18 weeks - 95% (target) (%) Apr-14 May14 Jun-14 Jul-14 Aug-14 Sep14 Oct-14 Nov14 Dec14 Jan15 Feb15 Mar-15 Year to Date 99.0% 99.0% 100.0% 98.9% 99.4% 98.0% 98.0% 97.8% 98.8% 99.9% 99.9% 97.65% 98.86% 94.0% 95.0% 93.3.% 93.1% 90.1% 94.7% 95.2% 92.8% 95.5% 93.3% 92.5% 94% 93.63% 99.0% 99.0% 99.2% 98.6% 100.0% 98.5% 97.5% 99.6% 98.4% 98.8% 98.9% 98.9% 98.87% DCHS intends to develop the data collection and validation processes for the RTT indicator for dental pathways in advance of including the figures within the 2015/16 quality report. Comparative data – Referral to Treatment Times Incomplete Pathway Total In Cohort Period Performance Rank Feb-15 99.00% 26 187 Mar-15 97.60% 45 186 Nat. Average Highest Lowest 94.4% Northamptonshire Healthcare NHS Foundation Trust North East London NHS Foundation Trust 94.4% Bradford District Care Trust North East London NHS Foundation Trust Delayed transfers of care When patients are ready for discharge from our services it is important that we are able to transfer them to their next place of care as soon as possible. The measurement of this metric allows us to understand what issues delay transfers of care and to work with partner agencies to improve this. This metric is measured against a target of <7.5% of patients being delayed. The table below gives comparative data for the last two years and demonstrates that whilst we have met this target in year there have been individual months were we have fallen below the standard. Where this occurs an investigation is undertaken to identify and learn from the cause. Most often delays are due to patients requiring complex and specialist care packages within a long term residential setting. DCHS considers that this data is as described for the following reasons: there are proper internal controls for the collection and reporting of this measure of performance and the controls are subject to quality assessment using the trusts data kite mark quality assurance system. 41 2013/14 Apr-13 May-13 Jun-13 Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14 2013/14 Outturn Delayed Transfers of Care 2.4% 4.9% 6.0% 2.8% 4.5% 8.3% 7.7% 10.0% 10.6% 6.2% 7.8% 7.0% 6.6% 2014/15 Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15 Year to Date Delayed Transfers of Care 7.1% 3.2% 4.6% 4.3% 5.3% 3.8% 8.7% 8.7% 7.9% 4.7% 3.7% 1.0% 6.1% DCHS has taken the following actions to improve the delayed transfers of care percentage, we have reviewed the clinical pathway management within our older peoples mental health wards and worked with partners across health and social care to ensure that effective discharge plans are in place for patients. Comparative data - DTOC Monitor Compliance Calculation No national comparator data available Development of a multidisciplinary foot care service at Buxton Hospital Patients with diabetes are at risk of developing complex foot conditions which can severely impact on their quality of life. In January 2014 in conjunction with our colleagues at Stepping Hill Hospital we established a new foot care service. The service is led by the Consultant Podiatric Surgery team in liaison with a consultant diabetologist. This service enables patients who have complicated foot problems to be seen locally by a multidisciplinary team instead of having to be seen within an acute hospital. The staff have developed their clinical skills to be able to offer intravenous antibiotics to patients who require these, this allows the patients to receive intravenous antibiotics either as an outpatient at Buxton Hospital or an inpatient at the Cavendish Hospital, thus enabling patients to receive a local service and reducing demand on our acute hospitals. DCHS in-reach service DCHS has been commissioned to provide an in-reach service to our Derbyshire acute hospitals. The purpose of the service is to provide a multi-disciplinary team to work in partnership with Social Care to assess patients in acute hospitals and clinically navigate individuals to the most appropriate service to meet their on-going care needs. Currently DCHS has teams based at Chesterfield Royal Hospital (CRH) and Royal Derby Hospitals. In addition, the Chesterfield Royal in-reach team also provides a weekly service to Kings Mill Hospital, Mansfield as well as Stepping Hill and Macclesfield acute hospitals. The teams have developed positive working relationships with acute hospital staff improving timely access to the wide range of available community services and facilitating safe discharges or transfers of care. The CRH In-Reach team operate seven days per week which has reduced surges in activity and improved patient flow to Community Services, enabling patients’ needs to be met in the right place, at the right time by the right service. It is the intention that the RDH team will become a seven day service in the near future. Measure RTT Waits admitted patients seen within 18 weeks - 90% (target) (%) RTT Waits - non admitted patients seen within 18 weeks - 95% (target) (%) Apr14 May14 Jun14 Jul14 Aug14 Sep14 Oct14 Nov14 Dec14 Jan15 Feb15 Mar15 94.0% 95.0% 93.3% 93.1% 86.7% 94.7% 95.2% 92.8% 95.5% 93.3% 92.5% 94.0% 99.0% 99.0% 99.2% 98.6% 100.0% 98.5% 97.5% 99.6% 98.4% 98.8% 98.9% 98.9% 42 The teams collect data to evidence the impact of the service. During December 2014 and January 2015 there was a 30.5% increase in transfers from acute hospitals to DCHS Community Hospitals and a 15.2% increase in transfers at weekends which has supported the reduction of acute hospital bed pressures. The team also collate evidence of gaps and duplication in community service provision to support future service improvement initiatives. “Working together to deliver the best possible care for the people of Swadlincote locality, when and where they need it" This is the vision of the Swadlincote Integrated Community Team who continue to make phenomenal progress developing partnership working with adult social care, GPs, voluntary sector, mental health services, the CCG and with cross border health and social care providers. The integrated team comprises of community matrons, community nurses, therapists, care coordinators, support workers and admin staff who work together to provide responsive high quality care around the needs of their community. With a rapidly increasing ageing local population and with areas of deprivation partnership working with adult social care is vital in meeting the challenge of providing great care. The teams work together to provide preventative and responsive services. The teams are fully engaged in the working with the newly commissioned Care Coordinators supporting the new community support teams. Other recent partnership developments are the formation of the Single Point of Access Rapid Response Service and the intermediate care beds at Oakland Village. Some members of the team work jointly with social care in the reablement service providing short term care and rehabilitation. At Oakland Intermediate Care Unit the therapists work together with adult care providing rehabilitation and care for patients who are either "stepped up" from the community or "stepped down" from Queens Medical Centre, Nottingham. The team have been praised for their flexible and open minded approach which helps to facilitate partnership working. Trust and respect has been built between both partners. The Single Point of Access (SPA) responds to referrals for urgent, rapid response assessments within 2 hours. The team have had considerable success together with adult social care in maintaining some very complex patients in their own homes - reducing unnecessary hospital admissions and making a real difference to patients. The team take a lead role in the Swadlincote Integrated Care Group, a local forum of health and social care leads, the voluntary sector and the CCG. At this forum service transformation is discussed with engagement from all parties. The team are not standing still and further developments are already underway with the virtual ward, the voluntary sector and with mental health to enhance local services. We are immensely proud of the partnership working achieved by this team and the benefits it is bringing to patients every day. Telehealth pilot In 2013 £250,000 of non-recurrent funding was identified by the four Derbyshire CCGs, for implementation of a telehealth service which was delivered by our DCHS Heart Failure Service. The heart failure telehealth service went live in September 2013. Telehealth services offer a way to remotely monitor patients with long term conditions (LTCs) such as heart failure, in order to reduce unplanned admissions to hospital and to allow clinically appropriate interventions to be made in a timely manner. Heart failure patients on the heart failure specialist nurse caseload were recruited using a set of agreed clinical criteria. A monitoring profile was created for each individual patient with parameters set for vital signs recordings, such as blood pressure and weight. If a patient failed to complete their readings within the agreed timeframe then the telehealth system produced a non-conformance alert. If a patient returned vital signs readings outside their set parameters, or indicated via their answers to a questionnaire that their condition may be deteriorating, then a red alert was produced. 43 All alerts are monitored by heart failure nurses five days a week and are triaged and actioned according to special alert pathways. Information from the evaluation of this pilot will be used to influence commissioning decisions for future service development. Key Data and information related to the telehealth service pilot. Patients and carers were invited to participate in a patient satisfaction survey and heart failure staff were surveyed as to their opinion of the telehealth service. Heart failure related inpatient admissions costs for patients before the use of telehealth amounted to £168, 978 while during the period of telehealth use the heart failure inpatient costs were £35,814. This is a saving of £133,164. Before the use of telehealth a total of 55 patients were admitted to an acute hospital for heart failure related activity a total of 61 times using 637 bed days. During the period of telehealth use a total of 13 patients were admitted to an acute hospital for heart failure related activity a total of 20 times using 222 bed days. This is a reduction in the number of admissions by 41, the number of patients admitted reduced by 42 and the number of bed days saved was 415. The cost for running the telehealth service during the period of the evaluation was approximately £152,000. It should be noted that costs of approximately £17,000 were associated with set up of the service and will not be incurred again. The mean Length of Stay (LoS) prior to use of telehealth for all patients was 11.5 days with inpatient spells ranging between 0 days and 30 days. In contrast the mean LoS post introduction of telehealth rose to 18.5 days with inpatient spells ranging between 0 days and 49 days. This showed an increase of mean length of stay by seven days. This was not an expected outcome but may reflect a change in the complexity of the patients admitted to hospital as part of the telehealth service. This indicates that more complex patients were admitted to hospital during the pilot of the telehealth service while less complex patients, who may previously have been admitted to an acute bed, were managed at home by heart failure specialist nurses. A patient satisfaction survey was issued to telehealth service patients, who had been using the equipment for up to 12 months, with a 46% rate of return. The results of the patient survey showed that 91% either agreed or strongly agreed that they felt more involved in their care by participating in the programme. 82% either agreed or strongly agreed that using the equipment gave them peace of mind and reduced their anxiety about their heart failure. 82% of respondents also strongly agreed or agreed that they felt that the telehealth service helped their heart failure specialist nurse manage their care better. The results from the staff survey were also encouraging with 100% of respondents agreeing or strongly agreeing that the telehealth service helped them to provide better care for their patient. 100% of respondents also agreed or strongly agreed that the service gave their patient more peace of mind on discharge from hospital. All respondents agreed or strongly agreed that information gained from the telehealth service enabled them to look after their patient more efficiently. Non-weight bearing pathway The non-weight bearing pathway pilot is an initiative utilising System Resilience monies which has been set up to provide a service for patients who are unable to weight bear for a period of time and would otherwise remain in an acute hospital bed for their non-weight bearing period. It is a therapy led service with a small team of clinicians including therapists, a nurse and generic support workers. Patients are referred by Chesterfield Royal Hospital once they have been assessed as unable to return home for their non-weight bearing period, are medically stable and are safe to be discharged into a community setting. The patient is then assessed by the team and, once accepted onto the pathway, a bed is commissioned for the non-weight bearing period, usually in a residential or nursing home. During 44 this time the patient is monitored by the team and an individual exercise programme is set up by the therapists. They are visited regularly by the generic support worker in order to keep the patient as mobile as possible in the non-affected limbs until they have a follow up outpatient appointment at the hospital. A member of the team accompanies the patient to follow up appointments and once the patient is able to weight bear they are assessed and referred to the most appropriate rehabilitation service. This may be at home with intermediate care, an intermediate care bed or in a community hospital. The non-weight bearing team then hand over patient care back into mainstream community services. Erewash care home support service Erewash CCG has commissioned a new service to provide local care homes with dedicated specialist nursing support. The team provide continuity of care, via a rapid response service and regular ward rounds with the aim of reducing unnecessary admissions to hospital and to reduce the number of visits to care homes that GP’s have to make, therefore enabling more appointments to be available in the GP surgeries. The service is delivered by a small team of advanced nurse practitioners (ANP’s) linking closely to the GP practices and supported by care coordinators. ANPs are able to assess, diagnose, investigate and treat a wide range of conditions and illnesses. Although the service only started towards the end of 2014 the early information is demonstrating a real impact on reducing the number of care home patients admitted to hospital and who continue to be successfully cared for in the environment in which they are familiar. Erewash welcome home service We recognise that settling in at home following a spell at an acute hospital can be difficult, sometimes resulting in a readmission if the necessary components are not in place. This may be as simple as not having food in the fridge, or not being able to make it upstairs to bed on the first night, to more complex issues e.g. not having the right equipment or medications in place. The Erewash welcome home service was established with the aim of reducing the number of older people readmitted to Nottingham University Hospital (NUH) shortly after discharge. The service forms part of the Erewash Integrated Care Team and involves care coordinators, linked to GP practices, proactively contacting by telephone, every patient over the age of 65 as near to the day of discharge as possible. Staff check patients awareness of their health needs, understanding of their medication, mobility, access to appropriate food and drink, and that their home is adequately heated. If any concerns are identified the care coordinators make relevant contact / referrals to address them. The partnership working enables patients to remain at home and avoids readmissions to hospital. Dental services - accessible patient information The dental service is currently striving to ensure the availability of an identified range of patient information leaflets. These will be related to oral and dental care for those people with a learning disability. A good way for us to improve our communication is by using different written formats. In addition to our Communicate in Print - Widgit symbols package, we have now purchased Photo-symbols to create further Easy Read information. It is important to be responsive to our patient’s needs and inform our patient’s how to continue self-care once they are within their own home environment. The range of key subjects in Easy Read will also explain ‘the process of and risk’ as well as ‘instruction’ leaflets on oral health or dental treatments. The Oral Health Promotion team are currently working with the public and multi-agency teams at Health Care For All and the Learning Disability Good Health Group meetings. These groups have given valuable suggestions in presenting these leaflets. Dental nurses who have attended our Certificate in Special Care Dental Nursing course were asked to create Easy Read leaflets. This awareness of other accessible information formats was to highlight the 45 need and importance of providing Easy Read leaflets to the public accessing general dental practices within the Midlands. The Francis Report – how we have responded In response to the Francis Report (February 2013) DCHS established a Francis Working Group which reported monthly to our Quality Services Committee (QSC) until March 2014 with a detailed outcome report going to QSC in March 2014 prior to a detailed report on the actions in response to Francis featuring in the Quality Account 2013/14. In addition the Board of Directors approved the Derbyshire Community Health Services’ Response to the Government Response to the Robert Francis QC’s Inquiry into Mid Staffordshire NHS FT at the January 2014 Board and this was published on the public facing website. It was agreed at the March 2014 QSC that the reporting mechanism for each remaining work stream (Safe Staffing, Clinical Supervision, Developing an Open and Transparent Culture, Complaints Reporting including better complaints information and Patient Safety) would be monitored by the Deputy Chief Nurse formally reviewed and reported six monthly to Quality Services Committee. These key elements form strands of work that are embedded within our established governance processes. 46 Appendix 1 - Workforce 2014 NHS staff survey In 2014 we used our NHS Staff Survey to invite staff to take time out to tell us what they thought about the organisation and their working lives. This was performed independently by the Picker Institute Europe which ensured absolute confidentiality and supported detailed analysis. We received a 62.1% response rate to our full census which enabled us to have a rich source of data to look at the key areas we can improve for our staff. NHS England published its Staff Survey results in February 2015, taking a sample to provide results across 29 key findings, benchmarked against all other Community Trusts. The table below gives a summary of ranking, compared with all Community Trusts in 2014. 29 Key findings: Above (better than) average Below (better than) average Average Above (worse than) average Below (worse than) average 2014 12 5 11 1 0 Overall staff engagement The overall staff engagement score for 2014 is 3.83 and was above (better than) average when compared with trusts of a similar type, this has increased from 3.76 in 2013. It also compares favourably against a national NHS engagement score of 3.76 and national Community Trust engagement score of 3.75. The overall indicator of staff engagement is calculated by NHS England using the questions that make up key findings 22, 24 and 25. These key findings relate to the following aspects of staff engagement: Staff members’ perceived ability to contribute to improvements at work Staff members’ willingness to recommend the trust as a place to work or receive treatment The extent to which staff feel motivated and engaged with their work Staff friends and family test questions The table below shows how we compare with other Community Trusts in England to the two key staff friends and family test questions: Birmingham Community Healthcare NHS Trust 48.03 If a friend or relative needed treatment I would be happy with the standard of care provided by this organisation 61.55 Bridgewater Community Healthcare NHS Trust 44.19 63.71 Cambridgeshire Community Services NHS Trust 58.55 65.73 Central London Community Healthcare NHS Trust 44.13 54.73 Derbyshire Community Health Services NHS Foundation Trust 54.24 65.12 Hertfordshire Community NHS Trust 46.69 59.14 Hounslow And Richmond Community Healthcare NHS Trust 52.66 62.24 Kent Community Health NHS Trust 46.84 60.10 I would recommend my organisation as a place to work 47 Leeds Community Healthcare NHS Trust 36.30 If a friend or relative needed treatment I would be happy with the standard of care provided by this organisation 56.28 Lincolnshire Community Health Services NHS Trust 47.51 62.23 Liverpool Community Health NHS Trust 36.75 55.08 Norfolk Community Health And Care NHS Trust 36.80 54.06 Shropshire Community Health NHS Trust 44.89 60.00 Solent NHS Trust 44.69 60.64 Staffordshire And Stoke On Trent Partnership NHS Trust 43.39 55.42 Sussex Community NHS Trust 50.61 59.80 The Gloucestershire Care Services National Health Service Trust 47.06 59.86 Torbay and Southern Devon Health and Care NHS Trust 55.31 62.09 Wirral Community NHS Trust 50.15 66.16 I would recommend my organisation as a place to work Top 5 ranking areas This page highlights the 5 key findings for which DCHS compare most favourably with other Community Trusts in England. KF3: Work pressure felt by staff (2.89 compared to average of 3.11) KF11: Percentage of staff suffering from work-related stress in the last 12 months (7% variance from average) KF1: Percentage of staff feeling satisfied with the quality of work and patient care they are able to deliver (7% variance from average) KF5: Percentage of staff working extra hours (6% variance from average) KF8: Percentage of staff having well-structured appraisals in the last 12 months (10% variance from average) Bottom 5 ranking areas This page highlights the 5 key findings for which DCHS compare least favourably with other Community Trusts in England. It is suggested that these areas might be seen as a starting point for local action to improve as an employer. According to the National NHS England data the five key findings for which DCHS compares least favourably with other Community Trusts in England are: KF17: Percentage of staff experiencing physical violence from staff in the last 12 months (1% variance from average) KF28: Percentage of staff experiencing discrimination at work in the last 12 months (1% variance from average) KF16: Percentage of staff experiencing physical violence from patients, relatives or the public in the last 12 months (no variance from average) KF26: Percentage of staff having equality and diversity training in the last 12 months (1% variance from average) KF22: Percentage of staff able to contribute to improvements at work (no variance from average) Key areas of improvement According to the National NHS England data our key areas of improvement are as follows: KF20: Percentage of staff feeling pressure in the last 3 months to attend work when feeling unwell (7% decrease since 2013) 48 KF9: Support from immediate managers (3.63 in 2013 to 3.80 in 2014) KF4: Effective team working (3.76 in 2013 to 3.88 in 2014) KF23: Staff job satisfaction (3.61 in 2013 to 3.75 in 2014) KF16: Percentage of staff experiencing physical violence from patients, relatives or the public in the last 12 months (12% in 2013 to 8% in 2014) Pulse Checks The DCHS pulse check was launched back in July 2013 and provides an indicator throughout the year as to how staff, as employees, are feeling. The pulse checks are run on a quarterly basis and provide an opportunity for staff to give anonymous feedback on how well they feel they are being managed, engaged and supported. This is now linked with our Staff Friends and Family Test. It allows DCHS senior leaders to work closely with their teams about the issues that are important to them. The pulse checks provide information to facilitate focus and relevant action to be taken each quarter rather than once a year. The way they are structured facilitates swift feedback after the questionnaire has been completed. The positive impact high staff engagement can have on other Trust KPIs - such as attendance, patient safety and productivity - is recognised and well researched. It is also a significant measure for the leader as to how well they are engaging with their teams to deliver the results we need, primarily around quality care for our patients. The trust wide response rates for each quarter to date are: July 2013: 39% October 2013: 37% January 2014: 36% April 2014: 31% July 2014: 38% January 2015: 33% The overall engagement scores for each quarter to date are: July 2013: 77% October 2013: 77% January 2014: 79% April 2014: 76% July 2014: 76% January 2015: 77% Our Staff FFT scores for the past 2 Pulse Checks are as follows: How likely are you to recommend DCHS to friends and family if they needed care or treatment? July 2014: 90% January 2015: 89% How likely are you to recommend DCHS to friends and family as a place to work? July 2014: 71% January 2015: 71% Raising concerns DCHS is committed to achieving the highest possible standards and actively encourages openness and honesty in the workplace. This year we have developed an ‘App’ to assist staff who wish to raise a concern as part of our ongoing commitment to creating a culture where members of staff are encouraged and empowered to raise concerns without fear of recrimination. We have reviewed our Whistleblowing Policy to make it simpler for staff to understand and clarified how concerns will be dealt with. We are looking at new ways of feeding back to staff so that they feel confident we have dealt appropriately with the concerns they have raised. 49 In the last year we have received a small number of formal concerns raised through our Whistleblowing Policy. All of these have been thoroughly investigated and detailed action plans have been produced to ensure that any issues that need addressing are dealt with. We have implemented a new process which entails the Chief Executive, Senior Independent Director and Trust Secretary reviewing the action plans on a regular basis and receiving assurances from the relevant managers that they have been implemented. How we develop and support our staff Staff appraisals Staff Training Learning and Development Leadership Development Appraisals The introduction of a revised leadership appraisal system in 2012 has enabled alignment of the NHS Leadership Framework, DCHS Way appraisal process and KPI’s. The process is now embedded within the Trust providing a valuable mechanism for measuring performance whilst, also identifying the development areas and support required by staff so as to enable them to achieve their full potential. In 2015 we intend to enhance e-appraisal systems piloted in April 2014 and we will roll out the use of eappraisals across all directorates. Appraisal training continues to be offered across the Trust to ensure both the appraiser and appraisee are equipped with the knowledge and skills to develop and receive an effective, meaningful appraisal. 86% of our staff received an appraisal within the year and we will be working hard during the coming year to improve on this. Training We have a dedicated development centre which provides a wide range of in-house training opportunities for the workforce. The development centre houses a skills lab, IT training suite plus clinical and nonclinical training rooms. Training programmes are also commissioned from external providers to meet workforce needs. In 2015 we plan to revise our annual training needs analysis process so as to ensure better alignment with Health Education England commissioning cycle. The development of divisional training plans linked to organisation objectives and business plans will also assist in the identification of workforce development needs particularly, in relation to the knowledge skills and competences required for delivery of integrated care. We also plan to strengthen the clinical practice facilitator role, to provide training locally and support changes in delivery of care while ensuring quality is maintained. Learning and development We are committed to provide a learning environment that supports and enables our workforce to attain the right skills, competence and professional capabilities to deliver excellent care in a challenging and changing environment. As we develop new services and models of care we will use a broad range of development opportunities to equip our staff with the qualities, skills and competencies to fulfil and enhance their roles and career progression to deliver high quality, efficient and effective services. This will be achieved through the provision of development opportunities such as rotations to enhance job enrichment and growth opportunities supported by strong preceptorship and mentorship. In addition increasing the number of Advanced Clinical Practitioners will be integral to supporting new models of care delivery. All new staff undertake an in-house induction programme over 5 days to ensure they receive all training relevant to their role prior to commencing in post. We launched a new induction programme in 2014 and we are pleased to say that 100% of staff attended the corporate induction within the first month of employment. 50 % DCHS Compliance (April 2014) % DCHS Compliance st (March 31 2015) % DCHS Target Essential learning 95% 93% 95% Information governance 91% 95% 95% Fire training 91% 92% 95% Appraisal 92% 93% 100% Training programmes reported against a target of 95% of available staff All clinical support staff undertake a 10 day fundamentals in care course prior to commencing in post. The fundamentals in care course will ensure all clinical support staff meet the criteria for the Care Certificate to be launched in April 2015. Staff will be supported to undertake a diploma in health / health and social care within 18 months of commencement in post. In 2014 we recruited an e-learning co-ordinator / developer. In the past 12 months we have seen a steady increase in staff undertaking some elements of mandatory training via eLearning. We will continue to increase the number of eLearning packages and provide IT access and training to all staff to enable increased productivity, efficiency and engagement in the work place. The Mental Health Lead Trainer has successfully delivered Dementia Friend courses across the trust. Dementia training is a key priority so as to ensure patients with Dementia and their carers receive excellent care. We aim to significantly increase the number of Dementia champions within the trust this year. Future plans include a review of existing essential and clinical essential training programme so as to streamline programme delivery, increasing apprenticeship and traineeship opportunities across the trust, in particular, encouraging clinical apprenticeships. There will be an increased focus on the impact of learning and development on practice. This will be captured by reviewing and implementing effective evaluation of learning and development programmes. During 2015 we plan to submit a 5 year learning and development strategy to the board for approval, outlining our learning and development priorities for 2015-2020. It will provide a framework for improvement and success, a key aspect of the strategy will be the commitment to continue to develop as a learning organisation promoting a culture of reflection, innovation and shared learning and passion for continuous professional development. Leadership development Leadership Development is a key priority for 2015, we will continue to develop our leaders through a range of targeted leadership interventions so as to equip our clinical leaders, business leaders and people managers with the necessary values, skills, behaviours and experience to maximise their potential in leading the trust forward. We will build the capacity and capability of our clinical leaders through a robust development and assessment model through our Quality Always programme both developing the capability of our clinical leaders as well as further developing our systems of assessment and outcome measures in care delivery. Fire safety training Since April 2014 fire training figures as reported to board have continued to be around the 90% mark based over rolling 12 month period, i.e. March 2014 – April 2015 the figure is 92% (3875 staff). This figure includes all staff who have attended essential training, induction, e-learning, completed the internal fire workbooks or attended a face-to-face fire training session at one of our sites. In addition to the standard fire training sessions specialist training sessions are also held for Nominated officer fire and fire warden roles and also training in the use of evacuation equipment such as ski sheets, pads and evacuation chairs where required. 51 Reporting of Injuries, Diseases and Dangerous Occurrence Regulations (RIDDOR) Staff health and safety At DCHS we take Health and Safety very seriously, our objective is to ensure that ALL our staff to go home safely at the end of each and every day. Our approach to Staying Safe is simple. We believe that all injuries are preventable and through good leadership and engagement of staff you can create a safety culture in which everyone takes responsibility for health and safety both on a personal and a collective level. In 2015/15 we have had 942 reported incidents versus 912 in 213/14. Out of the 942 incidents reported there were 552 with no harm or injury, 375 minor injuries and 15 RIDDOR Reportable injuries. Staff Minor Injury Incidents by Category Collision Contact with hazard Exposure to harmful agent Display Screen Equipment Environmental Issues Equipment (not medical device) Ergodynamics Lifting / handling injury Needle stick / Sharps Injuries Occupational Stress Road Traffic Accident Slips, trips and falls Trapped Violence / abuse / harassment Totals: 2014/15 29 38 2 2 6 8 1 45 24 6 7 53 10 144 375 2013/14 52 54 7 0 7 6 3 51 30 6 8 57 15 143 439 In 2014/15 we have had a 17.06% decrease in incidents. Reporting of injuries, diseases and dangerous occurrence regulations (RIDDOR) This requires us to report any workplace incident that falls into a specific category to the Health & Safety Executive (HSE). Workplace injuries are reportable to the HSE if they are a result of our work activity and constitute a major injury or absence from work for more than seven days. If a visitor or member of the public visiting one of our hospitals suffered a major injury as a result of our work activity we would also have to report this to the HSE. We had 15 RIDDOR reportable injuries to staff in 2014/15 and none to members of the public or visitors. Staff RIDDOR Incidents by Category Collision Contact with hazard Exposure to harmful agent Ergodynamics Lifting / handling injury Slips, trips and falls Violence / abuse / harassment Totals: 2014/15 1 0 1 1 5 5 2 15 52 Appendix 2 - Information Governance Toolkit submission for 2014/15 We are required to make sure that the information we hold about patients and staff is held and managed safely and confidentially and that it is used only for the purpose for which it was collected. The Information Governance Group is responsible for maintaining and improving the Information Governance Toolkit scores. We can confirm that we had no requirements that were not applicable and all requirements were answered. Level 0 Level 1 Level 2 Level 3 Total Req’ts Overall Score (%) Information Governance Management 0 0 2 3 5 86% Confidentiality and Data Protection Assurance 0 0 7 2 9 74% Information Security Assurance 0 0 13 2 15 71% Clinical Information Assurance 0 0 5 0 5 66% Secondary Use Assurance 0 0 1 1 2 83% Corporate Information Assurance 0 0 3 0 3 66% Overall 0 0 31 8 39 73% Assessment 53 Appendix 3 - Third party statements - CCGs/Healthwatch Healthwatch Derbyshire is able to comment on the 2014/15 Quality Report as a member of the Trust’s Patient Experience Group and as a contributor of patient feedback for action, triangulation and feedback from the Trust about processes and actions. Healthwatch Derbyshire has passed on a range of patient feedback during this period, both positive and negative, about a wide range of Trust services. The Trust have responded to Healthwatch regularly to keep us abreast of any action and learning from both specific comments and any emerging themes. This Quality Report refers to the patient feedback provided by Healthwatch Derbyshire, and many other sources in a section called ‘What have we done to improve Patient Experience?’ The feedback section comprehensively sets out the range of feedback available to the Trust, but does not always set out to the reader how all of this feedback is actively used by the organisation. This might be helpful to include in future, by demonstrating through real examples how this feedback has been taken through a process to have an impact on patient experience. Along similar lines, the 2014 NHS staff survey is shown in this report, along with the staff, friends and family test. These results give the reader a good assessment of scores in these areas. However further information about how these results have been hard wired in to some of the Trust’s strategic plans would be useful to summarise for the reader. This report provides a useful summary of the position of DCHS as a provider, its performance over 2014/15 and its plans for 2015/16. It would just be useful to the reader to draw more obvious parallels between the range of performance data and feedback systems, to understand how this is used by the organisation to learn and influence its priorities going forward. With kind regards Tammi Wright Office Manager Healthwatch Derbyshire 54 North Derbyshire Clinical Commissioning Group Quality Report 2014/15 Derbyshire Community Health Services Foundation Trust Commissioner Statement General Comments NHS North Derbyshire Clinical Commissioning Group (NDCCG) is responsible for providing the commissioner statement on the quality account provided by Derbyshire Community Health Services Foundation Trust (DCHSFT) and in doing so has provided NHS Hardwick Clinical Commissioning Group, NHS Southern Derbyshire Clinical Commissioning Group and NHS Erewash Clinical Commissioning Group as associate commissioners with the opportunity to make comments and contribute to the commissioner statement. Careful consideration has been given to the content and accuracy in line with the national guidance. NDCCG can confirm that DCHSFT has produced a Quality Account that meets the guidance and that the information provided appears to be accurate and representative of the information available to NDCCG through contract monitoring and quality assurance processes during the year. Measuring and Improving Performance The Quality Account describes the quality of services provided this year by DCHSFT measured against national, regional and local standards as detailed within the NHS contract and also within the local quality schedule and quality incentive scheme (CQUIN). The Trust has worked well to achieve all of the requirements set out for them in the Quality Schedule and fully achieved eight of the nine CQUIN measures. The indicator not fully achieved was that relating to reduction of pressure ulcers, 1 of the 4 harms outlined in the NHS Safety Thermometer, we would however like to note the significant improvements in care and considerable efforts made by staff in working on this indicator even though the final target was not achieved and look to the outcomes in 2015/16 as this work continues. The 3 quality priorities outlined by DCHSFT for improvement over the year have been achieved. It is clear that the Trust’s commitment to these areas has continued to lead to significant achievements and developments which have enhanced patient care. It is noted from the Quality account that this work has led to a particular reduction in the number of medication errors and has reduced medication errors resulting in serious harm from 14 in 2013/14 to 0 in 2014/15. All DCHSFT services continue to perform well against the Friends and Family Test as a measure of patient experience and have continued to perform above local and national averages. The same has been achieved for the annual PLACE assessments (Patient Led Assessments of the Care Environment). We are also pleased to note that in their drive to improve dignity in care, 61 services have achieved the Bronze Dignity in care award and 5 have achieved their Silver award. A significant amount of work and focus has gone into dementia across the year, improving care and support for patients as well as carers. This work has also engaged the public in thinking about dementia in more dementia friendly ways through a local research project and the outcome has resulted in best practice examples which have been shared across the health and social care community. The Trust has also fully implemented and achieved the dementia CQUIN this year and has provided a good base for the National Dementia CQUIN 2015/16. 55 The most challenging area of quality improvement for DCHSFT continues to be pressure ulcers. Despite improvements in service areas the target of zero tolerance has not been met. We are pleased to see a downward trend in the severity of pressure ulcers occurring in DCHSFT care and greater collaborative working with other agencies across the health community. Commissioners will continue to closely monitor progress in this area and work jointly with providers to raise public awareness and ownership of the problem. In relation to patient safety Commissioners continue to receive all serious incident reports and root cause analysis work. Improvements have been sustained in the timeliness of the reports as has the focus on themes and evidencing of Improvements as the result of action plans. Commissioners will continue to work closely and collaboratively with DCHSFT across the coming year. The three strategic quality objectives that DCHSFT has set for 2015/16 reflect the key quality domains and ongoing commitment to learn from experience and improve the quality of care provision – Reducing pressure ulcer prevalence Delivering consistently safe and effective discharges Improving rates of breast feeding initiation through to sustainment Additional comments The Quality Account is an annual report to the public that aims to demonstrate that the Trust is assessing quality across the healthcare services provided. The Trust has worked collaboratively with commissioners and all key stakeholders to ensure patients receive high quality care in the right care setting. NHS North Derbyshire Clinical Commissioning Group and associate commissioners look forward to continuing to work with the Trust to commission and deliver this high quality patient care. Jayne Stringfellow Chief Nurse & Quality Officer On behalf of NHS North Derbyshire Clinical Commissioning Group 28th April 2015 56 East Midlands Academic Health Science Network Patient Safety Collaborative Quality Account Statement (2015) EMAHSN has established a local Patient Safety Collaborative whose role is to offer staff, service users, carers and patients the opportunity to work together to tackle specific patient safety problems, improve the safety of systems of care, build patient safety improvement capability and focus on actions that make the biggest difference using evidence based improvement methodologies. Derbyshire Community Health Services NHS FT is committed to working with the EMPSC and has pledged to contribute to the emergent safety priories below (omit any not relevant) Discharge, transfers and transitions Suicide, delirium and restraint The deteriorating patient The older person: focussing on what ‘good safety’ looks like in the care home setting. In addition we pledge to support the core priorities identified below: Developing a safety culture/leadership Measurement for improvement Capability building No formal response has been received from the Improvement and Scrutiny Committee at Derbyshire County Council . 57 Appendix 4 - Statement of Directors’ responsibilities in respect of the Quality Account The directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 as amended to prepare Quality Accounts for each financial year. Monitor has issued guidance to NHS foundation trust boards on the form and content of annual Quality Accounts (which incorporate the above legal requirements) and on the arrangements that foundation trust boards should put in place to support the data quality for the preparation of the Quality Account. In preparing the Quality Account, directors are required to take steps to satisfy themselves that: The content of the Quality Account meets the requirements set out in the NHS Foundation Trust Annual Reporting Manual 2014/15 The content of the Quality Account is not inconsistent with internal and external sources of information including: Board minutes and papers for the period April 2014 to May 2015 Papers relating to quality reported to the board over the period April 2014 to May 2015 Feedback from commissioners dated 6th May 2015 Feedback from Governors dated 24/02/2015 / 26/02/2015, 02/03/2015 & 13/05/2015 Feedback from Healthwatch dated 07/04/2015 Feedback from Overview and Scrutiny Committee ,(declined by DCC) The trusts complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009 dated March 2015 The national patient survey – n/a to DCHS The national staff survey dated 02/2015 The Head of Internal Audit’s annual opinion over the trust’s control environment dated 09/04/2015 (interim report) Care Quality Commission Intelligent Monitoring report (not available for community trusts) The Quality Account presents a balanced picture of the NHS foundation trust’s performance over the period covered; the performance information reported in the Quality Account is reliable and accurate: There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice Data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Account has been prepared in accordance with Monitor’s annual reporting guidance (which incorporates the Quality Account Regulations) (published at www.monitor-nhsft.gov.uk/annualreportingmanual) as well as the standards to support data quality for the preparation of the Quality Account (available at www.monitornhsft.gov.uk/annualreportingmanual) The directors confirm to the best of their knowledge and belief that they have complied with the above requirements in preparing the Quality Account. By order of the Board 58 Appendix 5 - Independent Auditors 59 Appendix 6 - The Core Quality Account Indicators The last indicator, Friends and Family Test – Patient, is for consideration and is not a statutory requirement. Prescribed Information Related NHS Outcomes DPC Framework Domain & who will report on them The data made available to the National Health 1: Preventing People from dying No Service prematurely trust or NHS foundation trust by the Health and 2: Enhancing quality of life for Social people with long-term conditions Care Information Centre with regard to— Acute trusts (a) the value and banding of the summary hospital-level mortality indicator (“SHMI”) for the trust for the reporting period; and (b) The percentage of patient deaths with palliative care coded at either diagnosis or specialty level for the trust for the reporting period. *The palliative care indicator is a contextual indicator. The data made available to the National Health 1: Preventing People from dying No Service prematurely trust or NHS foundation trust by the Health and 2: Enhancing quality of life for Social Care Information Centre with regard to the people with long-term conditions percentage of patients on Care Programme All trusts providing mental health Approach who were followed up within 7 days services after discharge from psychiatric in-patient care during the reporting period. The data made available to the National Health 1: Preventing People from dying No Service prematurely trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the Ambulance trusts percentage of Category A telephone calls (Red 1 and Red 2 calls) resulting in an emergency response by the trust at the scene of the emergency within 8 minutes of receipt of that call during the reporting period. The data made available to the National Health 1: Preventing People from dying No Service trust or NHS foundation trust by the Health prematurely and Social Care Information Centre with regard to Ambulance trusts the percentage of category A telephone calls resulting in an ambulance response by the trust at the scene of the emergency within 19 minutes of receipt of that call during the reporting period. The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients with a pre-existing diagnosis of suspected ST elevation myocardial infarction who received an appropriate care bundle from the trust during the reporting period. 1: Preventing People from dying prematurely 3: Helping people to recover from episodes of ill health or following injury No Ambulance trusts 60 The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients with suspected stroke assessed face to face who received an appropriate care bundle from the trust during the reporting period. The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of admissions to acute wards for which the Crisis Resolution Home Treatment Team acted as a gatekeeper during the reporting period. The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the trust’s patient reported outcome measures scores for— (i) groin hernia surgery, (ii) varicose vein surgery (iii) hip replacement surgery, and (iv) knee replacement surgery, during the reporting period. The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients aged— (i) 0 to 14; and (ii) 15 or over, Readmitted to a hospital which forms part of the trust within 28 days of being discharged from a hospital which forms part of the trust during the reporting period. The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the trust’s responsiveness to the personal needs of its patients during the reporting period. 1: Preventing People from dying prematurely 3: Helping people to recover from episodes of ill health or following injury No The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the trust’s “Patient experience of community mental health services” Indicator score with regard to a patient’s experience of contact with a health or social care worker during the reporting period. 2: Enhancing quality of life No for people with long-term conditions 4: Ensuring that people have a positive experience of care Ambulance trusts 2: Enhancing quality of life No for people with long-term conditions All trusts providing mental health services 3: Helping people to recover from episodes of ill health or following injury No All acute trusts 3: Helping people to recover from episodes of ill health or following injury Yes All trusts 4: Ensuring that people have a positive experience of care To include FFT final score All acute trusts All trusts providing mental health services 61 The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients who were admitted to hospital and who were risk assessed for venous thromboembolism during the reporting period. 5: Treating and caring for Yes people in a safe environment and protecting them from avoidable harm The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the rate per 100,000 bed days of cases of C difficile infection reported within the trust amongst patients aged 2 or over during the reporting period. The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the number and, where available, rate of patient safety incidents reported within the trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death. 5: Treating and caring for We use per people in a safe environment and 1,000 protecting them from avoidable harm occupied bed days All acute trusts All acute trusts 5: Treating and caring for Number of people in a safe environment and incidents protecting them from avoidable harm (causing harm or otherwise) All trusts per 1,000 WTE budgeted staff (no) We also record never events Friends and Family Test - Question Number 12d – 4: Ensuring that people have a Staff – The data made available by National positive experience of care Health Service Trust or NHS Foundation Trust by the Health and Social Care Information Centre ‘If a All acute trusts friend or relative needed treatment I would be happy with the standard of care provided by this We just record organisation' for each acute & acute specialist the friends trust who took part in the staff survey. and family score on the Friends and Family Test – Patient. The data made 4: Ensuring that people have a Board report available by National Health Service Trust or NHS positive experience of care. Foundation Trust by the Health and Social Care This indicator is not a statutory Information Centre for all acute providers of adult requirement. NHS funded care, covering services for inpatients All acute trusts and patients discharged from Accident and Emergency (types 1 and 2) 62 Glossary APO AQP ARU AV BAF CCG CFD CFT CQC CQUIN CRHFT DCC DCHS DHFT DHU DTC EoL EMU ERE FT GP HCAI HCCG HFN HFSN KPIs LD LoS MIU MRSA MUST NDCCG NED NHS NICE NUH OPMH PLACE PROMS SLT SPA VTE WTE – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – Autonomous Provider Organisation Any Qualified Provider Adult Reablement Unit Amber Valley Board Assurance Framework Clinical Commissioning Group Chesterfield Community Foundation Trust Care Quality Commission Commissioning for Quality and Innovation Chesterfield Royal Hospital Foundation Trust Derbyshire County Council Derbyshire Community Health Services NHS Foundation Trust Derby Hospitals NHS Foundation Trust Derbyshire Health United Diagnostic & Treatment Centre End of Life Elderly Medical Unit Erewash Foundation Trust General Practice Healthcare Associated Infection Hardwick Clinical Commissioning Group Heart Failure Nurse Heart Failure Specialist Nurse Key Performance Indicators Learning Disabilities Length of Stay Minor Injury Unit Methicillin-resistant Staphylococcus aureus Malnutrition Universal Screening Tool North Derbyshire Clinical Commissioning Group North East Derbyshire National Health Service National Institute for Clinical Excellence Nottingham University Hospital Older Peoples Mental Health Patient-Led Assessments of the Care Environment Patient Reported Outcome Measures Speech & Language Therapy Single Point of Access Venous-thrombo Embolism Whole Time Equivalents 63