Document 11129531
advertisement
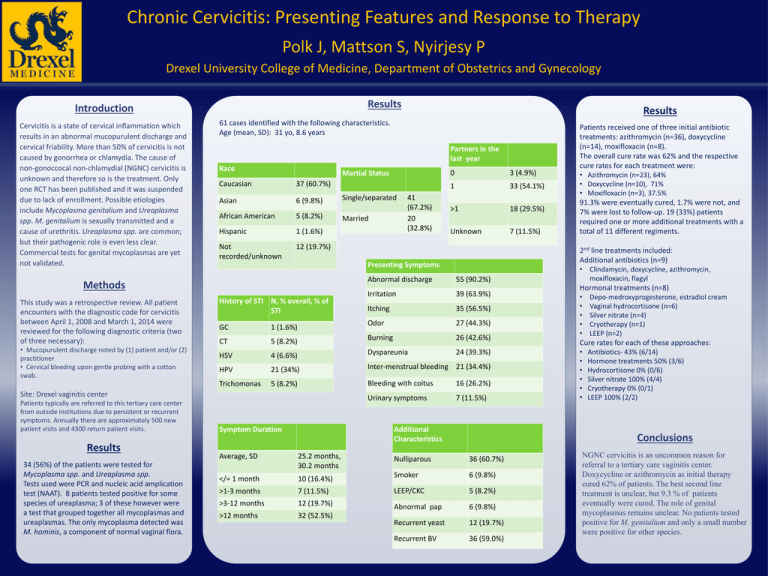
Chronic Cervicitis: Presenting Features and Response to Therapy Polk J, Mattson S, Nyirjesy P Drexel University College of Medicine, Department of Obstetrics and Gynecology Results Introduction Cervicitis is a state of cervical inflammation which results in an abnormal mucopurulent discharge and cervical friability. More than 50% of cervicitis is not caused by gonorrhea or chlamydia. The cause of non-gonoccocal non-chlamydial (NGNC) cervicitis is unknown and therefore so is the treatment. Only one RCT has been published and it was suspended due to lack of enrollment. Possible etiologies include Mycoplasma genitalium and Ureaplasma spp. M. genitalium is sexually transmitted and a cause of urethritis. Ureaplasma spp. are common; but their pathogenic role is even less clear. Commercial tests for genital mycoplasmas are yet not validated. 61 cases identified with the following characteristics. Age (mean, SD): 31 yo, 8.6 years Partners in the last year Race Martial Status Caucasian 37 (60.7%) Asian 6 (9.8%) African American 5 (8.2%) Hispanic 1 (1.6%) Not recorded/unknown 12 (19.7%) • Mucopurulent discharge noted by (1) patient and/or (2) practitioner • Cervical bleeding upon gentle probing with a cotton swab. Results 34 (56%) of the patients were tested for Mycoplasma spp. and Ureaplasma spp. Tests used were PCR and nucleic acid amplication test (NAAT). 8 patients tested positive for some species of ureaplasma; 3 of these however were a test that grouped together all mycoplasmas and ureaplasmas. The only mycoplasma detected was M. hominis, a component of normal vaginal flora. Married 41 (67.2%) 20 (32.8%) Abnormal discharge 3 (4.9%) 1 33 (54.1%) >1 18 (29.5%) Unknown 7 (11.5%) 55 (90.2%) 39 (63.9%) Itching 35 (56.5%) Odor 27 (44.3%) 5 (8.2%) Burning 26 (42.6%) HSV 4 (6.6%) Dyspareunia 24 (39.3%) HPV 21 (34%) Inter-menstrual bleeding 21 (34.4%) Trichomonas 5 (8.2%) Bleeding with coitus 16 (26.2%) Urinary symptoms 7 (11.5%) History of STI N, % overall, % of STI GC CT 1 (1.6%) Symptom Duration Average, SD Patients received one of three initial antibiotic treatments: azithromycin (n=36), doxycycline (n=14), moxifloxacin (n=8). The overall cure rate was 62% and the respective cure rates for each treatment were: • Azithromycin (n=23), 64% • Doxycycline (n=10), 71% • Moxifloxacin (n=3), 37.5% 91.3% were eventually cured, 1.7% were not, and 7% were lost to follow-up. 19 (33%) patients required one or more additional treatments with a total of 11 different regiments. 2nd line treatments included: Additional antibiotics (n=9) Irritation Site: Drexel vaginitis center Patients typically are referred to this tertiary care center from outside institutions due to persistent or recurrent symptoms. Annually there are approximately 500 new patient visits and 4300 return patient visits. Single/separated 0 Presenting Symptoms Methods This study was a retrospective review. All patient encounters with the diagnostic code for cervicitis between April 1, 2008 and March 1, 2014 were reviewed for the following diagnostic criteria (two of three necessary): Results Additional Characteristics • Clindamycin, doxycycline, azithromycin, moxifloxacin, flagyl Hormonal treatments (n=8) • • • • • Depo-medroxyprogesterone, estradiol cream Vaginal hydrocortisone (n=6) Silver nitrate (n=4) Cryotherapy (n=1) LEEP (n=2) Cure rates for each of these approaches: • • • • • • Antibiotics- 43% (6/14) Hormone treatments 50% (3/6) Hydrocortisone 0% (0/6) Silver nitrate 100% (4/4) Cryotherapy 0% (0/1) LEEP 100% (2/2) Conclusions 25.2 months, 30.2 months Nulliparous 36 (60.7%) </= 1 month 10 (16.4%) Smoker 6 (9.8%) >1-3 months 7 (11.5%) LEEP/CKC 5 (8.2%) >3-12 months 12 (19.7%) Abnormal pap 6 (9.8%) >12 months 32 (52.5%) Recurrent yeast 12 (19.7%) Recurrent BV 36 (59.0%) NGNC cervicitis is an uncommon reason for referral to a tertiary care vaginitis center. Doxycycline or azithromycin as initial therapy cured 62% of patients. The best second line treatment is unclear, but 9.3 % of patients eventually were cured. The role of genital mycoplasmas remains unclear. No patients tested positive for M. genitalium and only a small number were positive for other species.