Results of Total Ankle Arthroplasty Current Concepts Review 1455
advertisement
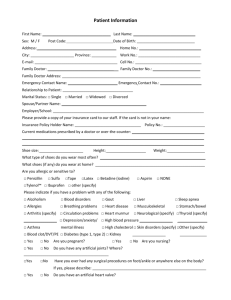
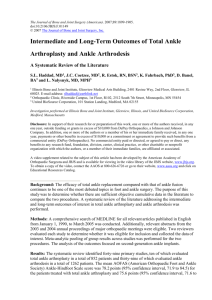
1455 C OPYRIGHT Ó 2011 BY T HE J OURNAL OF B ONE AND J OINT S URGERY, I NCORPORATED Current Concepts Review Results of Total Ankle Arthroplasty Mark E. Easley, MD, Samuel B. Adams Jr., MD, W. Chad Hembree, MD, and James K. DeOrio, MD Investigation performed at Duke University Medical Center, Durham, North Carolina ä Most published reports related to total ankle arthroplasty have a fair to poor-quality level of evidence. ä Comparative studies with a fair to good-quality level of evidence suggest that total ankle arthroplasty provides equal pain relief and possibly improved function compared with ankle arthrodesis. ä On the basis of the current literature, survivorship of total ankle arthroplasty implants, when measured as the retention of metal components, ranges from 70% to 98% at three to six years and from 80% to 95% at eight to twelve years. ä Several investigators have argued that, in the evolution of total ankle arthroplasty, some obligatory reoperation without removal of the metal implants is anticipated; examples of reoperation include relief of osseous or softtissue impingement, improvement of alignment or stability of the foot and ankle, bone-grafting for cystic lesions, and/or polyethylene exchange. ä A successful return to low-impact, recreational sporting activities is possible after total ankle arthroplasty. End-stage ankle arthritis is as debilitating as end-stage hip arthritis1, yet total joint arthroplasty has not displaced arthrodesis for end-stage ankle arthritis. Recent prospective controlled trials and meta-analyses have suggested that, for end-stage ankle arthritis, modern total ankle arthroplasty affords equivalent pain relief and perhaps better function than ankle arthrodesis2,3. In this article, we review the current results of total ankle arthroplasty and factors that may affect the interpretation of these results. Mean efficacy outcomes and patient satisfaction with the result of total ankle arthroplasty at intermediate-term followup uniformly suggest improvement from preoperative values. Pain subscores and functional outcomes are equal to and may exceed those of ankle arthrodesis. With few exceptions, implant survivorship has been reported to range from 70% to 98% at three to six years and from 80% to 95% at eight to twelve years, on the basis of the 2240 total ankle arthroplasties from multiple studies with adequate follow-up to determine implant survi- vorship4-27. Only one study, Anderson et al.28, noted a survivorship of 70%; in all other studies reviewed, the implant survivorship was >79% for three to twelve years. Some studies include longer follow-up of the same patients or implants from previous studies or represent a different analysis of the same patients9,11,17,18. The majority of the implants contributing to these survivorship curves had a satisfactory radiographic appearance. However, the radiographic appearance of some of the metal implants also included in these survivorship analyses has suggested impending failure with loosening and subsidence. For select implants, revision surgery may allow for the retention of the original metal implants. Repeat surgery in total ankle arthroplasty does not imply a failure of total ankle arthroplasty, as some repeat surgery is for relieving impingement, improving alignment, bone-grafting cysts, and/ or exchanging the polyethylene component to prolong implant survival. Confounding variables, such as a prolonged learning curve for surgeons implanting total ankle replacements Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article. J Bone Joint Surg Am. 2011;93:1455-68 d http://dx.doi.org/10.2106/JBJS.J.00126 1456 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d and the use of newer prosthetic designs and operative techniques, make it difficult to identify the reasons for success or failure. Factors to Consider in Total Ankle Arthroplasty Underlying Cause of Arthritis Degenerative, inflammatory, and posttraumatic arthritis of the ankle are the primary indications for total ankle arthroplasty (see Appendix). According to some authors, the results of total ankle arthroplasty are less favorable in patients with posttraumatic arthritis than in patients with osteoarthritis and inflammatory arthritis23,29,30. This may be because total ankle arthroplasties for posttraumatic arthritis are frequently performed in younger patients and patients who have undergone prior surgery to the ankle14,30-33. A study that analyzed data in a joint registry and a meta-analysis of studies on total ankle arthroplasty have suggested a trend of less favorable implant survivorship in patients with inflammatory arthritis compared with those with osteoarthritis 31,34. Other authors have noted that they always consider total ankle arthroplasty in patients with rheumatoid arthritis, when technically possible, and they reported identical functional outcomes after total ankle arthroplasty in patients with osteoarthritis and in those with posttraumatic arthritis35. Rippstein et al. reported better func- Fig. 1-A R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d tional outcome after total ankle arthroplasty in patients with inflammatory arthritis than in those with osteoarthritis36. Age The age of the patients receiving a total ankle arthroplasty in studies of currently available total ankle arthroplasty implants frequently has been less than fifty years; however, mean ages have consistently ranged from fifty to sixty years2,34,37. Several reports have suggested that the survivorship of implants and functional outcomes after total ankle arthroplasty are less favorable in younger patients2,15,31,32. In a study of 303 total ankle arthroplasties, Spirt et al. reported five-year implant survivorship of 74% and 89% for patients under and over the age of fifty-four years, respectively15. Those authors also calculated that patients with a median age of fifty-four years or less had a 1.45-times greater risk for reoperation and a 2.65-times greater risk of implant failure than patients over the age of fifty-four. The combination of younger age and hindfoot arthrodesis14 or osteoarthritis33 may lead to a relative increase in failure rates after total ankle arthroplasty. Nonetheless, Kofoed and Lundberg-Jensen, in a comparative study of a mobile-bearing prosthesis (Figs. 1-A through 1-D), including early-generation cemented and uncemented total ankle arthroplasty components, demonstrated that the survivorship of total ankle Fig. 1-B Figs. 1-A through 1-D A seventy-year-old man with end-stage ankle arthritis who was managed with a mobile-bearing total ankle arthroplasty. Fig. 1-A Anteroposterior weight-bearing radiograph of the ankle showing slight varus talar tilt but adequate alignment to allow consideration of a total ankle arthroplasty. Fig. 1-B Preoperative lateral radiograph showing slight anterior talar translation relative to the tibia. 1457 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d Fig. 1-C Fig. 1-D Fig. 1-C Postoperative anteroposterior weight-bearing radiograph showing satisfactory coronal plane alignment. Fig. 1-D Postoperative lateral radiograph showing satisfactory sagittal plane realignment of the ankle. arthroplasty components was comparable for patients under and over fifty years of age38. Preoperative Deformity and/or Instability The degree of ankle deformity and instability that can be adequately treated with total ankle arthroplasty continues to increase4,5,26. Despite these advances, coronal plane deformity exceeding 10° to 15° remains a relative contraindication to total ankle arthroplasty6-8,16,39,40 (Figs. 1-A, 1-C, 2-A, and 2-B). Implant survivorship typically diminishes with increasing preoperative coronal plane deformity7,16. Sagittal plane deformity, typically with relative anterior translation of the talus on the tibia, or component malrotation may also result in persistent postoperative deformity, subluxation and edge-loading of the polyethylene, osteolysis, and potential early implant failure6,7,40,41 (Figs. 1-B and 1-D). The Ankle-Subtalar Joint Complex The ankle is only one component of the ankle-hindfoot complex27,42,43, and with ankle arthritis, compensatory deformity may develop in the hindfoot. Total ankle arthroplasty occasionally requires adjunctive procedures to the hindfoot, midfoot, and forefoot in order to create a plantigrade foot on which to position the total ankle arthroplasty components4,14,17,44 (Fig. 3). Although necessary in select cases of total ankle arthro- plasty, hindfoot arthrodesis may lead to diminished survivorship of total ankle arthroplasty components in younger, higherdemand patients14. Even when patients have equal subscores for pain, the efficacy outcomes for patients who had total ankle arthroplasty with hindfoot arthrodesis will be inferior to those of patients who had isolated total ankle arthroplasty, since outcomes scoring for the ankle includes hindfoot range of motion35,44 (Figs. 4-A and 4-B). Mobile-Bearing Compared with Fixed-Bearing Implants Whereas total ankle arthroplasty implants used in patients worldwide are almost exclusively mobile-bearing three-component designs, most total ankle arthroplasty components in the United States have been fixed-bearing two-component designs. Mobilebearing devices have metal tibial and talar components articulating with an unattached polyethylene meniscus (Fig. 5); fixed-bearing prostheses have the polyethylene component secured to the metal tibial component (Fig. 6). The U.S. Food and Drug Administration (FDA) requires that three-component total ankle arthroplasty prostheses, for implantation in patients in the United States, achieve noninferiority status relative to ankle arthrodesis. The FDA’s demand was recently satisfied in a prospective controlled trial for a single three-component total ankle arthroplasty prosthesis approved for use without cement in the U.S.3. Without a similar FDA-regulated trial, other three- 1458 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d Fig. 2-A Fig. 2-B Figs. 2-A and 2-B Anteroposterior weight-bearing ankle radiographs of a seventy-three-year-old woman with end-stage ankle arthritis who had a mobilebearing total ankle arthroplasty. Fig. 2-A Preoperative radiograph demonstrating moderate-to-severe talar tilt for which total ankle arthroplasty should only be considered if the tibiotalar joint can be successfully realigned. Fig. 2-B Radiograph made a year postoperatively showing satisfactory realignment. The procedure included medial soft-tissue release. component designs may not be implanted in patients in the United States. Interpreting the Results of Total Ankle Arthroplasty Clinical Studies Published studies of total ankle arthroplasty have overwhelmingly carried a Grade-C recommendation (fair evidence or conflicting, or poor-quality, evidence, i.e., level III, IV, or V) for mobile or fixedbearing designs (Table I and Appendix). Without uniform outcome measures being applied to all studies, comparison of the results from the different case series is challenging 2,34,37. Debate remains over which outcome measures are most appropriate in the assessment of total ankle arthroplasty 2,34,37,45, and there are few comparative studies3,7,35,38,46. Recently, investigations of total ankle arthroplasty with good and fair-quality evidence3,7,35 and studies with longerterm follow-up of previous prospective case series6,9,18 have been presented or published, but there are too few to improve the recommendation for total ankle arthroplasty in the management of end-stage ankle arthritis from a Grade C to a Grade B or A. Functional outcome assessment with use of commonly applied scoring systems for total ankle arthroplasty (American Orthopaedic Foot & Ankle Society [AOFAS]47, Kofoed46, Mazur et al.48, and the New Jersey Orthopaedic Hospital system [also referred to as the Buechel-Pappas system]49) suggested uniform improvement in all studies, with follow-up scores generally ranging from 70 to 90 points (maximum, 100 points)2,34,37 (see Appendix). On the basis of data on 1888 patients in the studies reviewed that assessed patient satisfaction, the rates of patient satisfaction typically exceeded 90%, but ranged from 80% to 97%3-5,9,12,14,17-21,25-27 (see Appendix); follow-up data for patient satisfaction ratings rarely exceeded five years. On the basis of the survivorship data on 2240 implants in the studies reviewed in the present article, with the removal of a metal component or conversion to arthrodesis designated as the end point, the implant survivorship ranged from 70% to 98% at three to six years and 80% to 95% at eight to twelve years4-27 (see Appendix). Only one study, Anderson et al.28, noted the low survivorship of 70%, with six of twelve failures being attributed to technical error; for all other studies, implant survivorship was ‡79% for three to twelve years. These ranges in survivorship are supported by two recent meta-analyses34,37 (see Appendix). Meta-Analyses To our knowledge, there are three systematic reviews of total ankle arthroplasty in the literature (Table II): (1) a review of all modern (the most current version) mobile-bearing and fixed-bearing prostheses37; 1459 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d Fig. 3 Lateral weight-bearing ankle radiograph of a sixty-fiveyear-old man after total ankle arthroplasty for the treatment of end-stage ankle arthritis and hindfoot varus. Lateral displacement calcaneal osteotomy and first metatarsal dorsiflexion osteotomy were performed to treat the hindfoot varus concomitantly with a mobilebearing total ankle arthroplasty with establishment of a plantigrade foot. (2) a review of all three-component, meniscal-bearing prostheses34; and (3) a comparison of mainly second-generation total ankle arthroplasty prostheses and ankle arthrodesis2. Fig. 4-A Uniformly, the authors of the meta-analyses cautioned that most of the studies analyzed fail to meet methodological standards, lacked key data elements, and contained variability Fig. 4-B Figs. 4-A and 4-B Radiographs of a sixty-five-year-old woman, made seven years after a fixed-bearing total ankle arthroplasty for the treatment of inflammatory arthropathy. She was pain-free despite adjacent talonavicular joint arthritis that had not been addressed operatively. Fig. 4-A Lateral radiograph. Fig. 4-B Weight-bearing anteroposterior radiograph showing that the fixed-bearing total ankle arthroplasty components remained well-aligned. 1460 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d noted in Table II. The majority of reported results were for one particular design, and the authors did not identify differences in performance ratings when comparing that design against the other prostheses analyzed. Haddad et al.2, in a systematic review of both total ankle arthroplasty and ankle arthrodesis, included ten studies with 852 total ankle arthroplasties, with both mobile and fixedbearing designs, and thirty-nine studies with 1262 ankle arthrodeses (Table II). The mean AOFAS scores were 78.2 points and 75.6 points for total ankle arthroplasty and ankle arthrodesis, respectively, and the mean subscores for pain, function, and alignment for total ankle arthroplasty were 34.5, 37.4, and 9.4 points, respectively. In the review of total ankle arthroplasty studies by Haddad et al.2, the meta-analytic mean results were excellent for 38% of the patients, good for 30.5%, fair for 5.5%, and poor for 24%. When these percentages were also calculated as a ratio of the number of patients with a particular outcome divided by the total of ninety-two patients reporting the outcome, fortyeight patients (52.2%) had an excellent result; twenty-eight (30.4%), a good result; four (4.3%), a fair result; and twelve (13%), a poor result. In studies lacking such detail for total ankle arthroplasty, good results were noted for 388 (80.5%) of the 482 patients and poor results were observed in ninety-four Fig. 5 A mobile-bearing, three-component total ankle replacement. Note that the polyethylene is independent of the tibial component. in operative procedures, evaluation tools, and reporting of outcomes. Therefore, generalizations about total ankle arthroplasty outcomes derived from meta-analyses of the existing body of literature for total ankle arthroplasty are difficult to make in a reliable manner. Several recent investigations of total ankle arthroplasty have better evidence and longer follow-up periods and, if they were included, may have improved the conclusions that could be drawn from these meta-analyses3,7,9,18,26. Gougoulias et al.37 identified thirteen eligible studies comprising 801 mobile-bearing and 304 fixed-bearing prostheses (Table II). Including only the results of current total ankle arthroplasty designs, the authors noted that functional outcome scores improved in all studies and no one prosthesis demonstrated superiority over another. Residual pain was common after total ankle arthroplasty, with pain reported in 27% to 60% of the ankles. Some patients had clinically and radiographically acceptable implants but unexplained pain that prompted conversion to arthrodesis in select patients18,25. Stengel et al. 34 identified eighteen eligible studies of mobile-bearing total ankle arthroplasty with a mean follow-up period of 44.2 months (range, 35.9 to 52.4 months). The efficacy outcome for the ten eligible studies (497 patients) that used 100-point scales (Kofoed46 or AOFAS47) and the survivorship rates for the six studies that provided such data are Fig. 6 A fixed-bearing, two-component total ankle replacement. Note that the polyethylene is fixed to the tibial component. 1461 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d TABLE I Recommendations for Care: Grades of Recommendation for Treatment of End-Stage Ankle Arthritis with Total Ankle Arthroplasty Grade of Recommendation* Type of implant Mobile-bearing total ankle arthroplasty Fixed-bearing total ankle arthroplasty Etiology of ankle arthritis Total ankle arthroplasty for osteoarthritis Total ankle arthroplasty for posttraumatic arthritis Total ankle arthroplasty for inflammatory arthritis Other factors Coronal plane alignment <10° to 15° varus or valgus >10° to 15° varus or valgus Patient age R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d C C C C C C I C *C = conflicting or poor-quality evidence (Level-IV or V studies) not allowing a recommendation for or against intervention and I = insufficient evidence to make a recommendation. patients (19.5%). With respect to the low rate of patient satisfaction, their analysis included the results of one study of a fixed-bearing two-component prosthesis50 that were inferior to those in most studies of total ankle arthroplasty, including other studies of the same prosthesis8,51. The implant survival rates in the meta-analysis by Haddad et al.2 were lower than those for the other meta-analyses. The mean survivorship in this meta-analysis was diminished by the poor implant survival rates reported in the case series by Anderson et al.28 and a comparative study by Kofoed and Lundberg-Jensen38. With five-year survivorship of 70%, Anderson et al.28 acknowledged that their results and survivorship were negatively influenced by a so-called learning curve and an incomplete inventory of talar component sizes for their initial cases. Furthermore, the prosthesis they used did not consistently have the titanium spray that is currently used on this mobilebearing prosthesis. Likewise, the comparative study by Kofoed and Lundberg-Jensen included the early cemented and uncemented versions of the mobile-bearing prosthesis that are now abandoned38. Joint Registries The apparent advantages offered by joint registries (see Appendix) are that (1) data on a large number of operative procedures are available for analysis; (2) outcomes are not limited to procedures performed in centers of excellence; (3) surgeon, hospital, and region-specific trends in practices can be studied; and (4) uniform evaluation tools are used to facilitate comparisons31,32,52,53. In 2007, eighteen surgeons from eighteen hospitals reported their results extracted from New Zealand’s National Joint Registry53. Only two surgeons had performed more than twenty-five total ankle arthroplasties. New Zealand’s registry included 202 total ankle arthroplasties performed in 183 patients, with 7% that had failed at a mean follow-up of twenty-eight months. Implant selection by all of the surgeons participating in the registry consisted of only two prostheses with meaningful follow-up data for study: one two-component, fixed-bearing implant (58%) and one three-component, mobilebearing implant (22%). The overall five-year survival rate was 86%, and most failures were due to aseptic loosening. A patientbased questionnaire, extrapolated from the Oxford twelve-item hip-scoring system54 and completed at six months by 74% of the patients in the registry who had a total ankle arthroplasty, was described as a useful audit tool, with five-year failure-free rates of 95% for the patients with so-called good scores and 65% for those with poor scores. Sweden’s national joint registry included 531 primary mobile-bearing total ankle arthroplasties (492 patients) reported between 1993 and 200532 (see Appendix). Seventy-three percent of the total ankle arthroplasties had been performed by three surgeons in four hospitals. The reported revision rate of 19% in this patient cohort was subject to a learning curve, with the busiest three surgeons noting an improvement in implant survivorship of 70% for the first thirty total ankle arthroplasties and 86% for the subsequent 132 total ankle arthroplasties. As the surgeons gained experience with the procedure, and the design of the implants and the instruments used to make the bone cuts for the prostheses improved, the unacceptable rate of technical errors was lessened32,52. The published analysis of total ankle arthroplasties included in the Norwegian Arthroplasty Register includes 257 primary total ankle arthroplasties in 245 patients (mean age, fifty-eight years) with an average follow-up of four years31 (see Appendix). Meaningful data from this database are given for an early version of one mobile-bearing prosthetic design (1996 to 2002) and a modern version of the same prosthesis (2000 to 2005). Fewer revisions due to aseptic loosening of the tibial component were performed in patients with the modern prosthesis than in those with the earlier design32,40,55. The authors reported a five-year and ten-year survivorship of 89% and 76%, respectively. These calculations include the outdated cemented two-component versions of a mobile-bearing prosthetic design that is no longer used. A total of twenty-one revisions were performed in 216 mobile-bearing implants. Six revisions were done for aseptic loosening; five involved the early design whereas only one involved the modern design. Those authors defined revision as reoperation and did not designate removal of a metal component or conversion to arthrodesis as the end point for their overall survivorship analysis as is commonly reported in other studies3,7,14,37. Recalculation of this registry’s survivorship without the six polyethylene exchanges and the three other reoperations without removal of the metal components would make this study’s survivorship 1462 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d ä TABLE II Meta-Analyses No. of Eligible Studies No. of Ankles Type of Prostheses Analyzed Mean Age (yr) 13 1105 Mobile and fixed bearing 58.9 34 18 1107 Mobile bearing only 2 10 852 Mobile and fixed bearing Study 37 Gougoulias et al. (2010) Stengel et al. (2005) Haddad et al. (2007) Cause of Ankle Arthritis (% of ankles) Trauma Idiopathic Autoimmune Other 34 24.20 31.20 1 56.2 27.7 24.6 37.5 10.2 58 27.1 32.1 38.9 1.9 *Reported as good, excellent, satisfied, or satisfied with minimal reservation; percentage is based on number of patients who responded (may differ from number of implants). †Based on only six studies reporting survivorship data. §NR = not distinguished from reoperation rate. data consistent with those from other studies of modern total ankle arthroplasty. The outcomes of 515 primary mobile-bearing total ankle arthroplasties included in the Finnish Arthroplasty Register were published in 201052. Three centers each performed 100 total ankle arthroplasties or more, four centers performed between ten and fifty total ankle arthroplasties, and ten centers accounted for less than ten total ankle arthroplasties each. The five-year survival rate was 83%, with any reason for revision surgery as the end point, and 95%, with only aseptic loosening as the end point. Their analysis of the results failed to show a measurable difference in implant survival rates between high and low-volume hospitals. Despite the fact that the metal implants were well-fixed to bone, several total ankle arthroplasties showed ligamentous instability, which the authors attributed to the learning curve for total ankle arthroplasty and persistent ligament attenuation secondary to preoperative deformity. Alternative Approaches for the Assessment of Functional Outcome Gait Analysis with and without Functional Assessment Ankle arthritis causes considerable reduction in functional assessment scores, and successful total ankle arthroplasty typically improves function and gait characteristics56-59. On the basis of a prospective comparative analysis of preoperative and postoperative gait analysis, mobile-bearing total ankle replacements were found to improve locomotion function and decrease energy expenditure57. Similarly, a nearly normal gait pattern was observed in a comparative analysis of ten patients with a mobile-bearing total ankle replacement and ten healthy, control subjects56,60. Valderrabano et al.59 showed that patients with ankle arthritis had significantly worse AOFAS and Short Form-36 (SF-36) scores compared with subjects with physiologically normal ankles. At twelve months after total ankle arthroplasty, these same patients demonstrated no differences in spatiotemporal variables of gait analysis compared with the same subjects with healthy ankles59. Although successful ankle arthrodesis reliably relieves pain, the functional outcome and gait are different from those of healthy unaffected ankles61. Proprioception and Muscle Rehabilitation Conti et al.62 demonstrated no difference in the results of proprioceptive testing between arthritic ankles managed with total ankle arthroplasty and unaffected, contralateral ankles. Valderrabano et al.63 noted that muscle function in patients with osteoarthritic ankles improved after total ankle arthroplasty compared with the preoperative finding, but the improvement did not reach the level of the healthy, contralateral leg. Activity Levels and Sporting Activity Three recent articles evaluated participation in sports following total ankle arthroplasty20,29,35. In addition to the AOFAS and visual analog scale scores, the authors used the Foot and Ankle Ability Measure64, Foot Function Index65, University of California at Los Angeles (UCLA) activity scale66, the Activities Rating Scale67, and the International Physical Activity Questionnaire68. The authors’ objective was not to decide what sports may be recommended after total ankle arthroplasty but to determine what activities patients chose to perform following total ankle arthroplasty35. Naal et al.29, in a study of 155 total ankle arthroplasties with two mobile-bearing implant designs in 137 patients (average age, 59.8 years), with short to intermediate-term followup, determined activity levels with use of the UCLA activity scale66 and the Activities Rating Scale67. While 65% of the patients reported that total ankle arthroplasty had improved their sports ability, no differences were found with regard to preoperative and postoperative participation in sports, number of different sports, or frequency of weekly sporting activity. Most commonly, patients participated in swimming, cycling, and fitness and/or weight-training. Using the International Physical Activity Questionnaire, the authors also calculated that 79% of the patients met current guidelines for health-enhancing physical activity. The authors noted that neither sports participation nor activity levels were associated with radiographic lucencies, although they acknowledged that longer follow-up was needed. Valderrabano et al.20 evaluated 152 mobile-bearing total ankle arthroplasties in 147 patients (average age, 59.6 years) clinically and by questionnaire at the time of early follow-up. Of the 76% of the patients who underwent total ankle arthroplasty 1463 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d TABLE II (continued) Outcome and/or Patient Satisfaction* Survivorship (%) Revision Rate (%) Arthrodesis (%) Functional outcome of 70-92 points, based on 100-point scale; satisfaction rates of 79%-97% at 2 yr 90 (58-100) at 5 yr 6 (2.9-6.6 yr) 3.5 Mean improvement of 45.2 points (range,37-82 points), based on 100-point scale at a mean of 44.2 mo 90.6 at 5yr† NR§ 6.3 Mean postop. AOFAS score of 78.2; 78% good to excellent results 78.3 at 5 yr; 77 at 10 yr 7.2 4.9 for posttraumatic ankle arthritis, 83% reported good-to-excellent results, with the mean AOFAS score improving from 36 to 84 points. The patients who were active in sports preoperatively tended to be active in sports after total ankle arthroplasty. Most commonly, patients participated in hiking, biking, and swimming. Bonnin et al.35 evaluated 179 mobile-bearing total ankle arthroplasties in 170 patients (average age, 60.9 years) clinically and with a self-administered questionnaire at a mean follow-up interval of 53.8 months. The AOFAS ankle-hindfoot scores47 were extracted from the patient charts; the questionnaire included the Foot Function Index65 and the Foot and Ankle Ability Measure64 scoring methods. An evaluation of sporting activities was performed only for the ninety-eight patients with osteoarthritis. In this retrospective case-controlled study, the authors compared the functional outcomes of their patients who had total ankle arthroplasty with those of patients who had total knee arthroplasty. On the basis of an 82% response rate to the questionnaire, which showed that 76% of the patients rated their ankle as normal or nearly normal, the authors concluded that a return to light recreational activities and a nonimpact sport is generally possible, but that impact sports or strenuous recreational activities are rarely possible. Methods of Assessing Outcomes After Total Ankle Arthroplasty Physician-Based and Patient-Derived Outcomes Many of the currently used outcome instruments lack validity, reliability, responsiveness, and effectiveness for the assessment of outcomes after total ankle arthroplasty45,64,68,69. The trend in determining efficacy outcomes for total ankle arthroplasty is toward patient-based rather than physician-derived methodology19,20,29,35,45,70-72, with the anticipation of garnering a meaningful understanding of patients’ pain relief and improved function2,13,29,34,35,37,45,59,70. While the clinician-based region-specific AOFAS47, Kofoed46, and Mazur48 scoring systems are the most widely used outcome tools for total ankle arthroplasty, evidence suggests that their use in total ankle arthroplasty is limited45,73-75, with a poor correlation to the patient-derived SF-3671. Several authors favor the SF-36 in evaluating the foot and ankle1,13,20,22,34,59,76. SooHoo et al., in two different articles, suggested that the weak correlation between the SF-36 and AOFAS assessment tools indi- Other Residual pain in 27%-60% Results compared with ankle arthrodesis cates that the AOFAS scoring system is subject to poor construct validity71,72. A criticism of several patient-generated outcome tools, including the SF-36 and Health Assessment Questionnaire, is that they cannot adequately determine the region-specific health state of patients with ankle arthritis, with or without total ankle arthroplasty45. Likewise, the visual analog scale, while self-reported, is not region-specific13,45. Recent patient-derived outcomes used in total ankle arthroplasty include the Foot Function Index and Ankle Osteoarthritis Score45,65,70,77, with the Foot Function Index being considered a reasonable, validated outcomes tool70,72,78. Pain Scores and Functional Outcome In the majority of studies of modern total ankle arthroplasty, mean pain scores consistently improve following total ankle arthroplasty 37, with pain relief being at least as good as that after arthrodesis3. However, several studies have acknowledged that a considerable number of patients are not pain-free following total ankle arthroplasty4,6,7,9,12,14,18-22,37. Even though physician-derived outcome assessments may suggest good-to-excellent function in regular activities, they often lack the sensitivity to identify a less favorable outcome with strenuous activities4,29,35. Moreover, equal pain relief is reported by patients after total ankle arthroplasty with or without triple arthrodesis, thus suggesting equal outcomes on the basis of the isolated pain score. However, when physicianderived functional outcome measures are used, patients with the combined procedure of triple arthrodesis and total ankle arthroplasty immediately have lower functional scores than those undergoing isolated total ankle arthroplasty, because of the loss of hindfoot motion that occurs with hindfoot arthrodesis. Functional outcome measures typically include ankle range of motion. In the present review, analysis of the studies that described ankle range of motion before and after total ankle arthroplasty suggested only marginal improvements, with the mean increase in the sagittal plane motion arc ranging from 3° to 14°2,4,6,7,12,14,18,26,34,37,40. Range of motion is probably best assessed with use of radiographic analysis4,17,25,36,79, although some authors have demonstrated a satisfactory association between clinical and radiographic assessment of range of motion after total ankle arthroplasty21. 1464 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d Survivorship Tables Numerous surgeons have opined that reoperation for any reason other than revision arthroplasty or removal of any metal component, conversion to arthrodesis, or amputation does not constitute implant failure3,5-7,10,11,14,18,25,26. Examples of such reoperations include relief of osseous or soft-tissue impingement, improvement of alignment or stability of the foot or ankle, bone-grafting for cystic lesions, and/or polyethylene exchange3,14,15,17,18,22,26,34,37. Several investigators have argued that, in the evolution of total ankle arthroplasty, some obligatory reoperation without removal of the metal implants is anticipated9,14,15,18. In our opinion, the literature frequently presents an underestimation of reported survivorship of total ankle replacements because of the use of all reoperations as the end point15,31 and the influence of the so-called surgeon’s learning curve7,28,32,33,40,52,80-82. Bonnin et al.18 presented eleven-year survivorship estimates of their mobile-bearing prostheses for all reoperations (65%) and revision of the metal components or conversion to arthrodesis (85%). Radiographic Outcomes Alignment Alignment is typically assessed as one component of the functional score in most physician-based efficacy outcome assessments, with a high variability in methodology even when a goniometer is used. Several investigators have included more accurate radiographic assessments of alignment; however, the methodology of radiographic measurements is not uniform3,6,7,14,18,19,23-26,36,39,40,70 (Fig. 4-B). Subsidence and/or Migration and Radiolucencies Several studies have described implant migration, subsidence, or radiolucencies on the basis of serial radiographs4,7,9,14,18,25,26,29,55. Not all changes in position or radiolucencies portend diminished implant survivorship3,6,7,18,25,26,36. Progressive lucencies or cysts may be bone-grafted with successful implant retention, provided the implant is well-fixed at the time of reoperation2,6,7,14,18,36,45. Several investigators have explained that a minor amount of desirable settling in the first six to twelve months, typically in the talar component, allows the prosthesis to find its optimal position3,12,23,26,36,40,83. Fig. 7 Anteroposterior radiograph of the ankle of a seventy-six-year-old woman, made four years after a fixed-bearing total ankle arthroplasty for the treatment of incongruent varus talar tilt. Despite persistent varus deformity and osteolysis in the distal aspect of the tibia, the patient was able to function well with minimal symptoms. She had favorable results on the physician and patient-based outcome measures, satisfaction scores, and survivorship analysis despite radiographic findings concerning for impending failure. The extent of radiographic lucencies or cysts is often difficult to assess on radiographs and may be obscured by the prosthesis, particularly one that caps the talar dome6,7,20,26. Computed tomography is more sensitive than radiography in delineating cystic lesions84. Impending Failure or Threatened Prosthesis Multiple studies have described favorable survivorship of some total ankle replacements despite radiographic evidence of socalled impending or threatening failure due to progressive radiolucency or to component migration or subsidence12,22,28,40 (Fig. 7). Simply reporting survivorship at five to ten years as retention of the original metal components with disregard for radiographic findings may lead to a decline in longer-term survivorship analysis as these prostheses fail. Few studies reflect the best-case and worst-case scenarios in their survivorship analyses to account for these radiographic findings4,18,28. Probably most appropriately, Rippstein et al. include pending metal component exchange or conversion to arthrodesis in their survivorship estimations36. Progression of Adjacent Joint Arthritis Several studies have described the development or progression of subtalar or talonavicular arthritis after total ankle arthroplasty6,17,85, while others have noted no subtalar arthritis14,86, although at shorter follow-up intervals. Wood et al.6, in evaluating 167 total ankle arthroplasties in 156 patients with a minimum follow-up of five years, noted that seventy-two ankles (43%) were associated with preexisting end-stage subtalar arthritis, seventy (42%) demonstrated no radiographic change in subtalar arthritis, and twenty-five (15%) showed worsening subtalar arthritis. Knecht et al.17, in reviewing 117 fixed-bearing total ankle replacements with a minimum follow-up of two years, noted that twenty-two (19%) had progressive subtalar 1465 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d arthritis and seventeen (15%) had progressive talonavicular arthritis. Mann et al. observed no radiographic progression of hindfoot arthritis at an average follow-up of ten years for forty-five (88%) of fifty-five mobile-bearing total ankle arthroplasties; none of the remaining patients with progression of hindfoot arthritis was symptomatic26. SooHoo et al.85, using California’s hospital discharge database, identified 480 total ankle arthroplasties over a ten-year study period and suggested that the subtalar arthrodesis rate at five years after total ankle arthroplasty was 0.7%. These studies suggest that total ankle arthroplasty does not fully protect the adjacent hindfoot from the development or progression of arthritis. Arthroplasty Compared with Arthrodesis The evaluation of outcomes after total ankle arthroplasty is subject to comparison, either directly or indirectly, with those after arthrodesis2,3,85,87. While the database review by SooHoo et al. identified a higher complication rate for total ankle arthroplasty than for ankle arthrodesis85, the meta-analysis by Haddad et al. suggested similar intermediate-term outcomes for total ankle arthroplasty and arthrodesis2. Findings of similar functional outcomes for total ankle arthroplasty and ankle arthrodesis with a higher complication rate are corroborated by the comparative analyses by Krause et al. with use of validated outcome measures87. A recently published prospective comparison of a mobile-bearing prosthesis with ankle arthrodesis suggested that pain relief is equal and functional outcome is better after total ankle arthroplasty, on the basis of physicianbased and patient-based efficacy outcomes3. However, functional outcome by traditional scoring methodology immediately sets ankle arthrodesis at a disadvantage because of the loss of ankle range of motion. The current literature suggests that gait and range of motion are better after total ankle arthroplasty, perhaps accounting for diminished rates of adjacent subtalar or talonavicular joint arthritis after total ankle arthroplasty compared with those after arthrodesis6,7,17,61,86,88,89. Long-term outcomes after ankle arthrodesis have demonstrated high rates of functional disability88,89, and recent reports by Greisberg et al.90 and Hintermann et al.91 supported conversion of ankle arthrodesis to total ankle arthroplasty in select patients. Influence of Prosthetic Design, Instrumentation, and Technique Several implant design changes that have improved outcomes in total ankle arthroplasty include uncemented components5,31,51, augmented titanium plasma spray and hydroxyapatite coating on the backside of the metal components for one mobile-bearing design28,31,32,40,55, conversion of a shallow sulcus to a deep sulcus on another mobile-bearing total ankle arthroplasty design7,10,11, addition of a hydroxyapatite coating to the medial aspect of a third type of mobile-bearing design4,18, increased inventory of component sizes16,28,32,33, and the use of intraoperative fluoroscopy to improve component alignment70. Other studies have confirmed improved fixation with double-over single-coating porous ingrowth surface for that same mobile-bearing implant28,32. Improvement in instru- mentation, while rarely mentioned in total ankle arthroplasty outcome studies, most likely allows greater precision and reproducibility in performing total ankle arthroplasty26,32,52. Survivorship is typically diminished when optimal total ankle arthroplasty alignment is not achieved4,6,7,15,16,32,33,38,52,70,92. Several authors have described soft-tissue balancing and adjunctive procedures for the ankle and hindfoot to allow for the correction of deformity in the coronal plane5,15,18,26,36,44,92. Reproducible techniques in total knee arthroplasty to correct deformity have been extrapolated to deformity correction in total ankle arthroplasty93,94. Kofoed5 described a technique of intra-articular correction to realign severe valgus of the ankle with total ankle arthroplasty that is similar to an intra-articular correction of the knee for severe genu valgum95. Bonnin et al.4 described correction of severe varus malalignment with a comprehensive medial soft-tissue release similar to that performed for genu varum96,97. The authors added that the medial release technique typically obviates the need for lateral ligament reconstruction, a technique frequently described for total ankle arthroplasty in ankles with varus malalignment3. Alternatively, a sliding medial malleolar osteotomy has been described in select patients with varus malalignment92. Mild-to-moderate preoperative anterior translation of the talus within the ankle mortise appears to correct well with total ankle arthroplasty, even with mobile-bearing designs7. Developing Proficiency in Total Ankle Arthroplasty The literature on outcomes after total ankle arthroplasty has suggested that there is a period during which surgeons gain experience and expertise before they are proficient at performing total ankle arthroplasty3,14,18,28,32,33,36,37,40, with several investigations that have directly studied this issue80-82,98. Saltzman et al.81 suggested that this so-called learning curve exists irrespective of particular training in total ankle arthroplasty and showed, in a multicenter study, that complication rates are essentially halved as a surgeon gains experience3. Survivorship and outcomes reported by the inventor of a prosthesis may exceed those reported by other surgeons5,11,17,37; indeed, implant survivals of 95% at six years (based on 132 total ankle arthroplasties in 126 patients) for one fixed-bearing design17, 95% at twelve years (based on twenty-five total ankle arthroplasties in twentyfive patients) for one mobile-bearing prosthesis5, and 92% at twelve years (based on seventy-five total ankle arthroplasties in seventy-four patients) for another mobile-bearing design11 have not been consistently reproduced7,15,28,33,70. The results reported by Wood et al.7 suggested that, after a so-called learning curve has been established with one prosthesis, that experience may reduce or even eliminate the so-called learning curve with another, a finding supported in the Swedish Ankle Arthroplasty Register32. Complications and Their Salvage Several investigators have directly studied the complications of total ankle arthroplasty15,76,85,87,98, and systematic reviews have offered dedicated analysis of complication rates in total ankle arthroplasty2,34,37,76,85,98. Some authors’ methodology for reporting complications may be far more sensitive than that of others, 1466 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d leading to disproportionately high complication rates when their implant survivorship is not significantly different from those in other studies14,87. The systematic review of the effect of complications on outcome after total ankle arthroplasty by Glazebrook et al.76 was based on 2386 total ankle arthroplasties from twenty studies that met the authors’ inclusion criteria. High-grade complications of implant failure, aseptic loosening, and deep infection were associated with high failure rates for total ankle arthroplasty. Medium-grade complications of technical error, subsidence, and postoperative fracture were associated with moderate failure rates. Low-grade complications of intraoperative fracture and problems with wound-healing demonstrated negligible failure rates. This method of categorizing complications has been utilized by other authors26. On the basis of the available literature of current total ankle arthroplasty prostheses, salvage of a failed total ankle replacement does not require arthrodesis in most patients. In the meta-analysis by Gougoulias et al.37, implant failure was reported for 108 (9.8%) of 1105 total ankle arthroplasties at an average of 5.2 years, with sixty-seven (62%) of the failed implants managed with revision and thirty-nine (36%), with conversion to arthrodesis. In that review, a single patient who had failure of a total ankle replacement (<1%) had a transtibial amputation37, slightly less than the eight (2.6%) of 306 patients reported in a different study that considered total ankle arthroplasty as salvage in patients who were already considering amputation15. The meta-analyses by Stengel et al.34 and Haddad et al.2 described conversion of total ankle replacement to arthrodesis in forty-nine of 1086 patients (a pooled estimate of 6.3%) and twenty-nine of 572 (5.1%), respectively. Not all conversions of total ankle replacement to arthrodesis are due to implant failure; several authors have reported intractable, unexplained pain despite satisfactory clinical and radiographic findings as the reason for conversion to arthrodesis2,18,31,37. In general, authors have suggested that successful revision or conversion to arthrodesis with structural bone graft is possible2,5,11,14,18,34,37. Some authors who reported the results of investigations dedi- cated to repeat surgery for failed total ankle replacement99-101 found conversion to arthrodesis was favored over revision28,99, and the rate of union in patients with osteoarthritis was higher than that in patients with inflammatory arthritis99. Overview Despite the primarily weak evidence that does not allow a high grade of recommendation and the high variability in outcomes measures for total ankle arthroplasty, the intermediate-term efficacy outcomes, patient satisfaction, and implant survivorship are favorable. Improved operative technique, greater familiarity with the procedure on the part of surgeons, and advances in implant and instrumentation design may allow enhanced implant survivorship, an improved learning curve, and a decreased need for reoperation and revision. Appendix Tables showing patient demographic information, functional outcomes and patient satisfaction, implant survival and reoperations, radiographic loosening, and registry data from studies of total ankle arthroplasty are available with the online version of this article at jbjs.org. n NOTE: The authors thank the teams of Haddad et al.2, Stengel et al.34, and Gougoulias et al.37 for their extensive reviews of the total ankle arthroplasty literature. Mark E. Easley, MD James K. DeOrio, MD Department of Orthopaedic Surgery, Duke University Medical Center, Box 2950, Trent Drive, Durham, NC 27710. E-mail address for M.E. Easley: mark.e.easley@duke.edu Samuel B. Adams Jr., MD W. Chad Hembree, MD Box 3000, DUMC, Trent Drive, Durham, NC 27710 References 1. Glazebrook M, Daniels T, Younger A, Foote CJ, Penner M, Wing K, Lau J, Leighton R, Dunbar M. Comparison of health-related quality of life between patients with endstage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90:499-505. 2. Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89: 1899-905. 3. Saltzman CL, Mann RA, Ahrens JE, Amendola A, Anderson RB, Berlet GC, Brodsky JW, Chou LB, Clanton TO, Deland JT, Deorio JK, Horton GA, Lee TH, Mann JA, Nunley JA, Thordarson DB, Walling AK, Wapner KL, Coughlin MJ. Prospective controlled trial of STAR total ankle replacement versus ankle fusion: initial results. Foot Ankle Int. 2009;30:579-96. 4. Bonnin M, Judet T, Colombier JA, Buscayret F, Graveleau N, Piriou P. Midterm results of the Salto Total Ankle Prosthesis. Clin Orthop Relat Res. 2004;424: 6-18. 5. Kofoed H. Scandinavian Total Ankle Replacement (STAR). Clin Orthop Relat Res. 2004;424:73-9. 6. Wood PL, Prem H, Sutton C. Total ankle replacement: medium-term results in 200 Scandinavian total ankle replacements. J Bone Joint Surg Br. 2008;90: 605-9. 7. Wood PL, Sutton C, Mishra V, Suneja R. A randomised, controlled trial of two mobile-bearing total ankle replacements. J Bone Joint Surg Br. 2009;91:69-74. 8. Takakura Y, Tanaka Y, Kumai T, Sugimoto K, Ohgushi H. Ankle arthroplasty using three generations of metal and ceramic prostheses. Clin Orthop Relat Res. 2004; 424:130-6. 9. Hintermann B, Barg A. Mid-to-long-term survivorship of the HINTEGRA total ankle. Read at the American Orthopaedic Foot & Ankle Society 26th Annual Summer Meeting; 2010 Jul 7-10; National Harbor, MD. 10. Buechel FF Sr, Buechel FF Jr, Pappas MJ. Ten-year evaluation of cementless Buechel-Pappas meniscal bearing total ankle replacement. Foot Ankle Int. 2003; 24:462-72. 11. Buechel FF Sr, Buechel FF Jr, Pappas MJ. Twenty-year evaluation of cementless mobile-bearing total ankle replacements. Clin Orthop Relat Res. 2004;424:19-26. 12. San Giovanni TP, Keblish DJ, Thomas WH, Wilson MG. Eight-year results of a minimally constrained total ankle arthroplasty. Foot Ankle Int. 2006;27:418-26. 13. Nunley JA, Caputo A, Easley ME, Cook C. Mid to long-term outcomes of the STAR total ankle replacement: the patients’ perspective. J Bone Joint Surg Am. In press. 14. Valderrabano V, Hintermann B, Dick W. Scandinavian total ankle replacement: a 3.7-year average followup of 65 patients. Clin Orthop Relat Res. 2004;424: 47-56. 1467 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d 15. Spirt AA, Assal M, Hansen ST Jr. Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am. 2004;86:1172-8. 16. Doets HC, Brand R, Nelissen RG. Total ankle arthroplasty in inflammatory joint disease with use of two mobile-bearing designs. J Bone Joint Surg Am. 2006;88: 1272-84. 17. Knecht SI, Estin M, Callaghan JJ, Zimmerman MB, Alliman KJ, Alvine FG, Saltzman CL. The Agility total ankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86:1161-71. 18. Bonnin M, Gaudot F, Laurent JR, Ellis S, Colombier JA, Judet T. The Salto total ankle arthroplasty: survivorship and analysis of failures at 7 to 11 years. Clin Orthop Relat Res. 2011;469:225-36. 19. Besse JL, Brito N, Lienhart C. Clinical evaluation and radiographic assessment of bone lysis of the AES total ankle replacement. Foot Ankle Int. 2009;30:964-75. 20. Valderrabano V, Pagenstert G, Horisberger M, Knupp M, Hintermann B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med. 2006;34:993-9. 21. Ali MS, Higgins GA, Mohamed M. Intermediate results of Buechel Pappas unconstrained uncemented total ankle replacement for osteoarthritis. J Foot Ankle Surg. 2007;46:16-20. 22. Kopp FJ, Patel MM, Deland JT, O’Malley MJ. Total ankle arthroplasty with the Agility prosthesis: clinical and radiographic evaluation. Foot Ankle Int. 2006;27: 97-103. 23. Pyevich MT, Saltzman CL, Callaghan JJ, Alvine FG. Total ankle arthroplasty: a unique design. Two to twelve-year follow-up. J Bone Joint Surg Am. 1998;80:1410-20. 24. Karantana A, Hobson S, Dhar S. The Scandinavian total ankle replacement: survivorship at 5 and 8 years comparable to other series. Clin Orthop Rel Res. 2010;468:951-7 25. Wood PL, Karski MT, Watmough P. Total ankle replacement: the results of 100 mobility total ankle replacements. J Bone Joint Surg Br. 2010;92:958-62. 26. Mann J, Mann R, Horton E. STAR ankle: long-term results. Foot Ankle Int. 2011;32:473-84. 27. Giannini S, Romagnoli M, O’Connor JJ, Malerba F, Leardini A. Total ankle replacement compatible with ligament function produces mobility, good clinical scores, and low complication rates. Clin Orthop Rel Res. 2010; 468:2746-53. 28. Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg Am. 2003;85:1321-9. 29. Naal FD, Impellizzeri FM, Loibl M, Huber M, Rippstein PF. Habitual physical activity and sports participation after total ankle arthroplasty. Am J Sports Med. 2009;37:95-102. 30. Bai L-B, Lee K-B, Song EK, Yoon TR, Seon JK. Total ankle arthroplasty outcome comparison for post-traumatic and primary osteoarthritis. Foot Ankle Int. 2010;31: 1048-56. 31. Fevang BT, Lie SA, Havelin LI, Brun JG, Skredderstuen A, Furnes O. 257 ankle arthroplasties performed in Norway between 1994 and 2005. Acta Orthop. 2007; 78:575-83. 32. Henricson A, Skoog A, Carlsson A. The Swedish Ankle Arthroplasty Register: an analysis of 531 arthroplasties between 1993 and 2005. Acta Orthop. 2007;78: 569-74. 33. Hurowitz EJ, Gould JS, Fleisig GS, Fowler R. Outcome analysis of agility total ankle replacement with prior adjunctive procedures: two to six year followup. Foot Ankle Int. 2007;28:308-12. 34. Stengel D, Bauwens K, Ekkernkamp A, Cramer J. Efficacy of total ankle replacement with meniscal-bearing devices: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2005;125:109-19. 35. Bonnin MP, Laurent JR, Casillas M. Ankle function and sports activity after total ankle arthroplasty. Foot Ankle Int. 2009;30:933-44. 36. Rippstein PF, Huber M, Coetzee JC, Naal FD. Total Ankle Replacement With Use of a New Three-Component Implant. J Bone Joint Surg Am. In press. 37. Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res. 2010; 468:199-208. 38. Kofoed H, Lundberg-Jensen A. Ankle arthroplasty in patients younger and older than 50 years: a prospective series with long-term follow-up. Foot Ankle Int. 1999; 20:501-6. 39. Haskell A, Mann RA. Ankle arthroplasty with preoperative coronal plane deformity: short-term results. Clin Orthop Relat Res. 2004;424:98-103. 40. Wood PL, Deakin S. Total ankle replacement. The results in 200 ankles. J Bone Joint Surg Br. 2003;85:334-41. 41. Espinosa N, Walti M, Favre P, Snedeker JG. Misalignment of total ankle components can induce high joint contact pressures. J Bone Joint Surg Am. 2010; 92:1179-81. 42. Leardini A, O’Connor JJ, Catani F, Giannini S. A geometric model of the human ankle joint. J Biomech. 1999;32:585-91. 43. Leardini A, O’Connor JJ, Catani F, Giannini S. Mobility of the human ankle and the design of total ankle replacement. Clin Orthop Relat Res. 2004;424:39-46. 44. Kim BS, Knupp M, Zwicky L, Lee JW, Hintermann B. Total ankle replacement in association with hindfoot fusion: outcome and complications. J Bone Joint Surg Br. 2010;92:1540-7. 45. Naal FD, Impellizzeri FM, Rippstein PF. Which are the most frequently used outcome instruments in studies on total ankle arthroplasty? Clin Orthop Relat Res. 2010;468:815-26. 46. Kofoed H. Cylindrical cemented ankle arthroplasty: a prospective series with long-term follow-up. Foot Ankle Int. 1995;16:474-9. 47. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-53. 48. Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg Am. 1979;61:964-75. 49. Buechel FF, Pappas MJ, Iorio LJ. New Jersey low contact stress total ankle replacement: biomechanical rationale and review of 23 cementless cases. Foot Ankle. 1988;8:279-90. 50. Nishikawa M, Tomita T, Fujii M, Watanabe T, Hashimoto J, Sugamoto K, Ochi T, Yoshikawa H. Total ankle replacement in rheumatoid arthritis. Int Orthop. 2004;28:123-6. 51. Takakura Y, Tanaka Y, Kumai T, Sugimoto K, Ohgushi H. Ankle arthroplasty using three generations of metal and ceramic prostheses. Clin Orthop Relat Res. 2004;424:130-6. 52. Skyttä ET, Koivu H, Eskelinen A, Ikävalko M, Paavolainen P, Remes V. Total ankle replacement: a population-based study of 515 cases from the Finnish Arthroplasty Register. Acta Orthop. 2010;81:114-8. 53. Hosman AH, Mason RB, Hobbs T, Rothwell AG. A New Zealand national joint registry review of 202 total ankle replacements followed for up to 6 years. Acta Orthop. 2007;78:584-91. 54. Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185-90. 55. Carlsson A. [Single- and double-coated STAR total ankle replacements: a clinical and radiographic follow-up study of 109 cases]. Orthopade. 2006;35:527-32. German. 56. Doets HC, van Middelkoop M, Houdijk H, Nelissen RG, Veeger HE. Gait analysis after successful mobile bearing total ankle replacement. Foot Ankle Int. 2007; 28:313-22. 57. Detrembleur C, Leemrijse T. The effects of total ankle replacement on gait disability: analysis of energetic and mechanical variables. Gait Posture. 2009;29: 270-4. 58. Dyrby C, Chou LB, Andriacchi TP, Mann RA. Functional evaluation of the Scandinavian Total Ankle Replacement. Foot Ankle Int. 2004;25:377-81. 59. Valderrabano V, Nigg BM, von Tscharner V, Stefanyshyn DJ, Goepfert B, Hintermann B. Gait analysis in ankle osteoarthritis and total ankle replacement. Clin Biomech (Bristol, Avon). 2007;22:894-904. 60. Houdijk H, Doets HC, van Middelkoop M, Dirkjan Veeger HE. Joint stiffness of the ankle during walking after successful mobile-bearing total ankle replacement. Gait posture. 2008;27:115-9. 61. Thomas R, Daniels TR, Parker K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J Bone Joint Surg Am. 2006; 88:526-35. 62. Conti SF, Dazen D, Stewart G, Green A, Martin R, Kuxhaus L, Carl Miller M. Proprioception after total ankle arthroplasty. Foot Ankle Int. 2008;29:1069-73. 63. Valderrabano V, Nigg BM, von Tscharner V, Frank CB, Hintermann B. Total ankle replacement in ankle osteoarthritis: an analysis of muscle rehabilitation. Foot Ankle Int. 2007;28:281-91. 64. Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26: 968-83. 65. Budiman-Mak E, Conrad K, Stuck R, Matters M. Theoretical model and Rasch analysis to develop a revised Foot Function Index. Foot Ankle Int. 2006;27:519-27. 66. Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890-5. 67. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213-8. 68. Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int. 2004; 25:521-5. 69. Parker Nester CJ, Long AF, Barrie J. The problem with measuring patient perceptions of outcome with existing outcome measures in foot and ankle surgery. Foot Ankle Int. 2003;24:56-60. 70. Schutte BG, Louwerens JW. Short-term results of our first 49 Scandinavian total ankle replacements (STAR). Foot Ankle Int. 2008;29:124-7. 71. SooHoo NF, Shuler M, Fleming LL; American Orthopaedic Foot Ankle Society. Evaluation of the validity of the AOFAS Clinical Rating Systems by correlation to the SF-36. Foot Ankle Int. 2003;24:50-5. 1468 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O L U M E 93-A N U M B E R 15 A U G U S T 3, 2 011 d d R E S U LT S OF T O TA L A N K L E A R T H R O P L A S T Y d 72. SooHoo NF, Vyas R, Samimi D. Responsiveness of the foot function index, AOFAS clinical rating systems, and SF-36 after foot and ankle surgery. Foot Ankle Int. 2006;27:930-4. 73. Guyton GP. Theoretical limitations of the AOFAS scoring systems: an analysis using Monte Carlo modeling. Foot Ankle Int. 2001;22:779-87. 74. Pena F, Agel J, Coetzee JC. Comparison of the MFA to the AOFAS outcome tool in a population undergoing total ankle replacement. Foot Ankle Int. 2007;28:788-93. 75. Toolan BC, Wright Quinones VJ, Cunningham BJ, Brage ME. An evaluation of the use of retrospectively acquired preoperative AOFAS clinical rating scores to assess surgical outcome after elective foot and ankle surgery. Foot Ankle Int. 2001;22:775-8. 76. Glazebrook MA, Arsenault K, Dunbar M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int. 2009;30:945-9. 77. Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998;19: 466-71. 78. Agel J, Beskin JL, Brage M, Guyton GP, Kadel NJ, Saltzman CL, Sands AK, Sangeorzan BJ, SooHoo NF, Stroud CC, Thordarson DB. Reliability of the Foot Function Index: a report of the AOFAS Outcomes Committee. Foot Ankle Int. 2005; 26:962-7. 79. Coetzee JC, Castro MD. Accurate measurement of ankle range of motion after total ankle arthroplasty. Clin Orthop Relat Res. 2004;424:27-31. 80. Myerson MS, Mroczek K. Perioperative complications of total ankle arthroplasty. Foot Ankle Int. 2003;24:17-21. 81. Saltzman CL, Amendola A, Anderson R, Coetzee JC, Gall RJ, Haddad SL, Herbst S, Lian G, Sanders RW, Scioli M, Younger AS. Surgeon training and complications in total ankle arthroplasty. Foot Ankle Int. 2003;24:514-8. 82. Haskell A, Mann RA. Perioperative complication rate of total ankle replacement is reduced by surgeon experience. Foot Ankle Int. 2004;25:283-9. 83. Nelissen RG, Doets HC, Valstar ER. Early migration of the tibial component of the Buechel-Pappas total ankle prosthesis. Clin Orthop Relat Res. 2006;448:146-51. 84. Hanna RS, Haddad SL, Lazarus ML. Evaluation of periprosthetic lucency after total ankle arthroplasty: helical CT versus conventional radiography. Foot Ankle Int. 2007;28:921-6. 85. SooHoo NF, Zingmond DS, Ko CY. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg Am. 2007;89: 2143-9. 86. Kofoed H, Stürup J. Comparison of ankle arthroplasty and arthrodesis. A prospective series with long-term follow-up. Foot. 1994;4:6-9. 87. Krause FG, Windolf M, Bora B, Penner MJ, Wing KJ, Younger AS. Impact of complications in total ankle replacement and ankle arthrodesis analyzed with a validated outcome measurement. J Bone Joint Surg Am.2011;93:830-9. 88. Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83: 219-28. 89. Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J Bone Joint Surg Br. 2003; 85:994-8. 90. Greisberg J, Assal M, Flueckiger G, Hansen ST Jr. Takedown of ankle fusion and conversion to total ankle replacement. Clin Orthop Relat Res. 2004;424:80-8. 91. Hintermann B, Barg A, Knupp M, Valderrabano V. Conversion of painful ankle arthrodesis to total ankle arthroplasty. J Bone Joint Surg Am. 2009;91:850-8. 92. Cornelis Doets H, van der Plaat LW, Klein JP. Medial malleolar osteotomy for the correction of varus deformity during total ankle arthroplasty: results in 15 ankles. Foot Ankle Int. 2008;29:171-7. 93. Laskin R. The Insall Award. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop Relat Res. 1996;331:29-34. 94. Miyasaka KC, Ranawat CS, Mullaji A. 10- to 20-year followup of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res. 1997;345:29-37. 95. Easley ME, Insall JN, Scuderi GR, Bullek DD. Primary constrained condylar knee arthroplasty for the arthritic valgus knee. Clin Orthop Relat Res. 2000;380: 58-64. 96. Whiteside LA, Saeki K, Mihalko WM. Functional medial ligament balancing in total knee arthroplasty. Clin Orthop Relat Res. 2000;380:45-57. 97. Whiteside LA. Soft tissue balancing: the knee. J Arthroplasty. 2002;17(4 Suppl 1): 23-7. 98. McGarvey WC, Clanton TO, Lunz D. Malleolar fracture after total ankle arthroplasty: a comparison of two designs. Clin Orthop Relat Res. 2004;424:104-10. 99. Culpan P, Le Strat V, Piriou P, Judet T. Arthrodesis after failed total ankle replacement. J Bone Joint Surg Br. 2007;89:1178-83. 100. Kotnis R, Pasapula C, Anwar F, Cooke PH, Sharp RJ. The management of failed ankle replacement. J Bone Joint Surg Br. 2006;88:1039-47. 101. Berkowitz MJ, Clare MP, Walling AK, Sanders R. Salvage of failed total ankle arthroplasty with fusion using structural allograft and internal fixation. Foot Ankle Int. 2011;32:493-502.