1. RESPIRATORY SYSTEM

STRUCTURE AND FUNCTION
Lecture—1
Dr.Zahoor Ali Shaikh
1
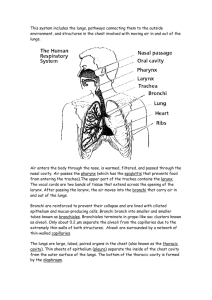
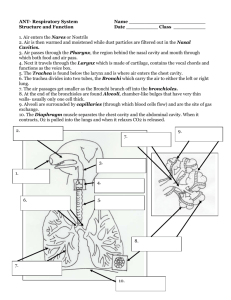
Nasal passages (Nose)
Pharynx (Throat )
Larynx (Voice box)
Trachea –Divides into Right main bronchus and
Left main bronchus
Bronchi
Bronchioles—large and small
Terminal Bronchioles
Respiratory Bronchioles
Alveolar Duct
Alveoli
2
3
4
Trachea divides into Right and Left Bronchi which enter Right and Left Lungs
Within each lung, bronchi continue to branch into narrow (small diameter),shorter and more numerous airways like branching of a tree.
Small braches are known as Bronchioleslastly Terminal bronchioles
5
At the end of Terminal Bronchioles, are
Respiratory Bronchioles , Alveolar duct,
Alveoli.
Tiny sacs(Alveoli) where gas exchange takes place between alveolar air and blood capillaries
6
Trachea and large bronchi have cartilaginous rings that prevent these from compressing
Very small bronchioles have no cartilage to hold them open. Their wall has smooth muscle
This smooth muscle is innervated by
Autonomic Nervous System, and is also sensitive to some hormones and local chemicals, which affect the air flow in small bronchioles
7
1- Breathing Oxygen in, and breathing out
Carbon dioxide
Helps in regulation of pH of blood (Acid –base balance) , by adjusting the rate of removal of
CO
2
.
8
-- Cellular Respiration ( Internal Respiration)
--External Respiration
Cellular Respiration
It refers to intracellular metabolic process in the Mitochondria, which uses O produces CO
2
2 and and energy ATP from food.
9
CELLULAR
RESPIRATION
10
On a mixed diet ( Carbohydrate, Fat, Protein ) O used is 250 ml/min and CO ml/min.
2 produced is 200
We use the Term Respiratory Quotient (RQ) produced = 200
2
RQ=
CO
2
O
2 used = 250
- On a mixed diet RQ = O.8
-- RQ depends on the type of food used
-- when Carbohydrate is used RQ= 1
-- when Fat is used RQ= 0.7
-- when Protein used RQ=0.8
11
Exchange of O
2 and CO
2 between External environment and cells of body. It has 4 steps.
1 – Gas exchange between the atmosphere and alveoli.
2- Exchange of O
2 and CO
2 between air in the alveoli and blood in pulmonary capillaries.
Transport of O
2 tissues. and CO
4 – Exchange of O
2
2 by the blood to the and CO capillaries and tissue cells
2 between system
12
13
It is route for water loss and heat elimination.
Inspired air is humidified and warmed by the respiratory airways before it is expired .
Respiratory pump – helps in venous return.
Helps in regulation of PH of blood.
It enables speech, singing .
It defends against inhaled foreign material.
14
Prostaglandins are inactivated in the lungs.
Conversion of angiotensinI to angiotensinII hormone, by ACE ( angiotensin converting enzyme ).
Nose– part of respiratory system , organ of smell.
15
O
2 and CO
2 diffuse through alveoli.
Rate of diffusion depends on thickness of alveolar membrane, surface area and partial pressure of O
2 and CO alveolar cells [type 1].
2
.
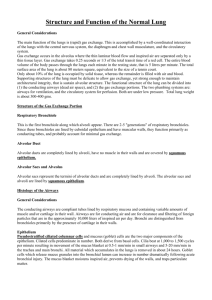
Alveolar wall consists of single layer of
16
Each alveolus is surrounded by a network of pulmonary capillaries, which is also single layer .
The interstitial space between an alveolus and capillary is very thin 0.5 µm which facilitates gas exchange.
Respiratory Membrane [Alveolar wall and
Capillary wall].
17
Lungs contain about 500 million alveoli, each about 300 µm in diameter [surface area exposed between alveolar air and pulmonary capillary blood is about 75 m 2 , size of tennis court].
In alveoli, there are Type II alveolar cells .
They secrete Pulmonary Surfactant.
Pulmonary Surfactant is a phospholipoprotein complex that helps in lung expansion.
18
19
Also in alveolar lumen, present are alveolar macrophages which help in defense
[Phagocytosis].
Pore of Kohn – are present between adjacent alveoli. Their presence permits air flow between adjacent alveoli. This process is called Collateral Ventilation.
20
Two lungs
- Right lung is divided into 3 lobes [upper, middle, lower] by oblique and transverse fissure.
- Left lung is divided into 2 lobes [upper, lower and has lingula] by oblique fissure.
Lung – has alveoli, blood vessels and large quantities of elastic connective tissues.
Changes in lung volume and alveolar volume are brought about through changes in dimensions of thoracic cavity.
21
The outer chest [Thorax] is formed by 12 pairs of curved ribs, which join the sternum anteriorly and thoracic vertebrae posteriorly.
Diaphragm – forms floor of thoracic cavity.
Diaphragm is sheet of skeletal muscle that separates thoracic cavity from abdominal cavity. It is penetrated by esophagus and blood vessels.
In the lung and chest wall, there is considerable amount of elastic connective tissue.
22
Pleura – separates each lung from the thoracic wall.
Pleura which surround each lung has two layers –
Visceral Pleura [inner layer] which surrounds the lung and Parietal Pleura [outer layer] which is under thorax.
Interior of pleural sac(space between parietal and visceral pleura) is known as Pleural Cavity.
Surfaces of pleura secrete intrapleural fluid which lubricates surfaces as they slide on each other during respiratory movements.
Clinical application – pleurisy – [inflammation of pleura]. It causes pain during inspiration and expiration, and friction rub.
23
24
Ventilation - air flow into and out of lungs.
We will consider
1. Atmospheric [barometric] pressure
2. Intra-alveolar pressure or Intra-pulmonary pressure
3. Intra-pleural pressure
25
It is pressure exerted by weight of air in the atmosphere on objects on Earth, as Earth surface.
At sea level, atmospheric pressure is
760mmHg.
Atmospheric [Barometric] pressure decreases at high altitude as layers of air decrease in thickness.
26
It is pressure within alveoli. It is 760mmHg. It decreases slightly during inspiration and increases during expiration.
Intra-Pleural Pressure or Intra-thoracic Pressure
It is pressure within pleural sac.
It is pressure exerted from outside the lungs within thoracic cavity.
Intra-pleural pressure is -4 mmHg [756mmHg which is 4mmHg less than atmospheric pressure of 760mmHg]
27
28
Flow of air into and out off lung occurs due to cyclic changes in intra-alveolar pressure.
Intra-alveolar pressure is less than atmospheric pressure during inspiration.
Intra-alveolar pressure is greater than atmospheric pressure during expiration.
29
30
When thorax expands, the lungs also expand that is lungs follow the movements of chest wall.
Transmural Pressure Gradient
It is the pressure difference between alveolar pressure and intra-pleural pressure in the lungs.
Intra-alveolar pressure equals to atmospheric pressure of 760mmHg.
Intra-pleural pressure is 756mmHg.
So there is greater pressure in the lungs as compared to pleura.
This Transmural pressure of +4mmHg causes stretching or opening of alveoli ,therefore lungs are always forced to expand.
31
Pneumothorax – air in the pleural cavity.
If there is chest injury, air rushes into the pleural cavity from high atmospheric pressure when chest is punctured e.g. broken rib or stab wound.
In Pneumothorax, pressure in the pleural cavity increases and causes the collapses of the lung.
Pleural Effusion – Abnormal collection fluid in the pleural cavity e.g. Tuberculosis
32
Functional Anatomy of Respiratory System
Functions of Respiratory System
External and Cellular Respiration
Non-respiratory functions of respiratory system
Gas Exchange between alveoli and pulmonary capillaries
Respiratory membrane (Alveolar wall & capillary wall)
Lungs and Thoracic Cavity
Visceral, Parietal Pleura and Pleura Cavity
Atmospheric pressure, Intra-alveolar pressure and
Intra-pleural pressure
Transmural Pressure and its importance
Applied Aspects – Pleurisy, Pneumothorax, pleuraleffusion
33
THANK YOU
34