Living Kidney Donation: Settling Psychosocial Barriers
advertisement
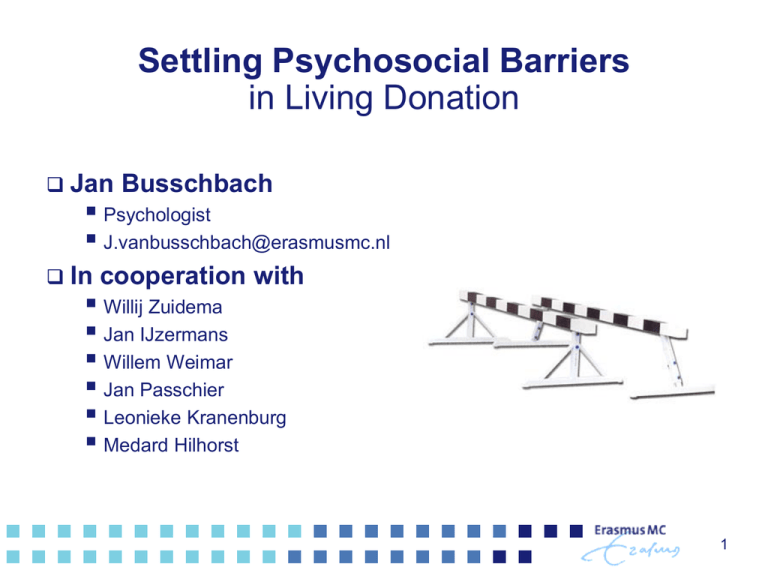
Settling Psychosocial Barriers in Living Donation Jan Busschbach Psychologist J.vanbusschbach@erasmusmc.nl In cooperation with Willij Zuidema Jan IJzermans Willem Weimar Jan Passchier Leonieke Kranenburg Medard Hilhorst 1 Living donor transplantation: are the outcomes good enough? Advantages Reduces the waiting list Increases craft survival Are the outcomes good enough? Should we pursue living donation? Are the better outcomes worth the costs? • Are the outcomes more valuable than the cost to overcome the barriers From a descriptive point of view… The answer is might be no… Living donation is not widely pursued The effects do not outweighed the cost to overcome the barriers 2 Barriers What are the barriers? Sometimes hard medical issues… But most often soft issues Legal Cultural Organizational Psychological 3 Psychological barriers Negative emotions towards living donation Inappropriate emotions Issues that related to inappropriate emotions … Information Wrong information Risk perception Wrong risk perception Communication between patient and donor Blocked communication * Kranenburg LW, Zuidema WC, Weimar W, Hilhorst MT, IJzermans JN, Passchier J, Busschbach JJ. Psychological barriers for living kidney donation: how to inform the potential donors? Transplantation. 2007 Oct 27;84(8):965-71 4 What can we do? How can we change… Wrong information Wrong risk perception Blocked communication Talking with the potential donor and patient Rational Information Interpretation Emotion More and better information… Gives more appropriate emotions 6 Not so rational,.. but reality Emotion Interpretation Information Better (more appropriate) emotion Better interpretation of information 7 Most likely model… Interpretation Emotion Information Interpretation Need to work on both information and emotion Next question: how? Talking with the patient and the potential donor But there is not yet a ‘evidence based’ way… 8 Looking for the best psychotherapy.. Not much difference between psychotherapies Many very different therapies seem to work equally well Research into non-specific factors Success factors in counseling Most important non-specific factors Therapeutic alliance Therapy adherence System involvement • Family • Friends Therapeutic alliance Biggest generic success factor Sexton & Wiston (1992) “…research has confirmed [that] the success of any therapeutic endeavor depends on the participants establishing an open, trusting, collaborative relationship or alliance.” • http://personcentered.com/research.html Control of emotion Safe environment How do we establish such alliance Listening and talking… Is it so simple? Counter-transference Our own ‘psychological schemes’ interfere Alternatively: Use theoretical scheme It does not matter much which… Behavioral therapy Cognitive therapy Schema focus Mentalisation Reduces influence of own ‘psychological schemes’ Helps to build a “…open, trusting, collaborative relationship or alliance.” In order to control emotions Treatment adherence Treatment adherence is fatal It does not matter which therapy As long as one use ONE therapy Created a consistent… Framework Language In a confusing world Thus consistency is important In time Within the team Protocols: adherence Involve system Patient part of ‘system’ System Family Friends College's Neighborhood System is strong Involve system when necessary In living donation, the system is important Obviously…the donor is part of the system 3 success factors 1. 2. 3. Therapeutic alliance Adherence to ‘a’ therapy Involve system What stops us? Fear for pressure on the potential donor But we put pressure on patients on a routine basis “If you don’t take the medicine you will become sick” Not the medical domain The donor is not a patient It is not ethical… to talk to the potential donor 15 Not the medical domain? Potential donor is not a patient Excludes caregivers Exclude prevention Suggests that patients are independent subjects, and not part of a system The potential donor is in the medical domain 16 Not ethical? In spoken language: good or bad In science: consistent set of rules Rules that are valid Rules we agree on… Is talking with the potential donor and patient ethical? Is there a consistent set of rules? • Rules that are valid • Rules we agree on… That forbid or allow such interference 17 Forbid interference Non-directivity and value neutrality Talking with the potential donor is directive But there is no such thing as non-directivity and value neutrality in counselling in general • This rule can not applied validly anywhere One should not change personal beliefs Assumes that beliefs are stable,… which they are not • Personal beliefs have formed… • There is no reason to believe they are completed Assumes that beliefs are always right… which they are not Assumes that it possible not to interfere… No consistent sets of rules.. 18 Allow interference in beliefs Stephen Toulmin Beliefs are a model of logical arguments Arguments are not fixed, but dynamic, Interferences can refine the model of arguments Rawls Beliefs are a model of reflective equilibrium Beliefs represents a network of idea’s and facts Interferences can help to keep communication within the network open 19 It is ethical to talk to the donor* Ethics is a consistent set of rules Rules we would like to endorse Set of rules that hold back interventions Set of roles that allow interventions Seems to be inconsistent Consistent Outcome in terms of process variables * Hilhorst MT, Kranenburg LW, Busschbach JJ. Should health care professionals encourage living kidney donation? Med Health Care Philos. 2007;10(1):81-90 Existing interventions Most standard Physician talks with patient • Information • Emotion regulation Patient talks with potential donor • Patients brings donor to the physician More active towards donor…. (Rotterdam) Information meetings For both patients and relatives (perhaps the donor) “semi targeted” information towards donor 21 Norwegian approach Dr. Anders Hartmann The physician communicates directly with the potential donor Physician discusses system with patient Physician asks permission from patient And calls the donor No motivation of any refusal is given: “donor is not suitable” 22 Norwegian approach will be appreciated 60 50 40 Positive Mixed Negative 30 20 10 0 Patients "Donors" 23 James Rodrique Activates communication in family (systems) “Very local” information meeting Especially in minorities RCT results: Increase in knowledge Willingness to discuss living donation Decrease concerns Outcome in terms of better model of arguments Toulmin, Ralws Rodrigue et al. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. Am J Transplant 2007;7:394-401. 24 Illustration of a theoretical framework MST: MultiSystemic Therapy Crime prevention in youth Involving the whole system Blueprint therapy evidence-based Practical “Whatever it takes” But what about Own psychological schemes? Treatment adherence? Treatment adherence MST Conclusions There are psychosocial barriers In living donation It is ethical to interfere Outcomes define in process variable These barriers can be overcome Building a constructive alliance • Controlling emotions Treatment adherences Involve system 27