The lymphatic system
advertisement
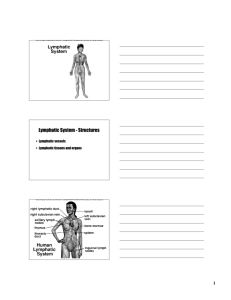
The lymphatic system The lymphatic system actually consists of two parts: (1) a network of lymphatic vessels and (2) various lymphoid tissues and organs scattered throughout the body. The lymphatic vessels transport back to the blood any fluids that have escaped from the blood vascular system. The lymphoid organs house phagocytic cells and lymphocytes, which play essential roles in the body’s defense mechanisms and its resistance to disease. lymphatic vessels • As explained before, the hydrostatic and colloid osmotic pressures operating at capillary beds force fluid out of the blood at the arterial ends of the beds and cause most of it to be reabsorbed at the venous ends . • The fluid that remains behind in the tissue spaces, as much as 3 L daily, becomes part of the interstitial fluid. This leaked fluid, plus any plasma proteins must be carried back to the blood. • This is resolved by the lymphatic vessels, or lymphatics, that collect the excess protein-containing interstitial fluid and return it to the bloodstream. Once interstitial fluid enters the lymphatics, it is called lymph (lymph = clear water). Distribution and Structure of Lymphatic Vessels: The lymphatic vessels form a one-way system in which lymph flows only toward the heart. This transport system begins in microscopic blind-ended lymphatic capillaries ,which is present between the tissue cells and blood capillaries . • lymphatic capillaries are so remarkably permeable that they were once thought to be open at one end like a straw. When fluid pressure in the interstitial space is greater than the pressure in the lymphatic capillary, a minivalve flaps gape open, allowing fluid to enter the lymphatic capillary. However, when the pressure is greater inside the lymphatic capillary, the endothelial minivalve flaps are forced closed, preventing lymph from leaking back out. • Proteins in the interstitial space enter lymphatic capillaries easily. When tissues are inflamed, lymphatic capillaries develop openings that permit uptake of even larger particles such as cell debris, pathogens and cancer cells. The pathogenic agents and cancer cells can then use the lymphatics to travel throughout the body. This threat to the body is partly resolved by the fact that through the lymph nodes it is cleansed of debris and “examined” by cells of the immune system. • Highly specialized lymphatic capillaries called lacteals (lak′te-alz) are present in the fingerlike villi of the intestinal mucosa. The lymph draining from the digestive viscera is milky white (lacte = milk) rather than clear because the lacteals play a major role in absorbing digested fats from the intestine. • The lymphatic collecting vessels have the same three tunics as veins, but the lymph vessels are thinner-walled, have more internal valves, and anastomose more. Lymph is eventually delivered to : - The right lymphatic duct drains lymph from the right upper arm and the right side of the head and thorax . -The much larger thoracic duct receives lymph from the rest of the body. As the thoracic duct runs superiorly, it receives lymphatic drainage from the left side of the thorax, left upper limb, and the head region. Each terminal duct empties its lymph into the subclavian vein on its own side of the body . Lymph Transport The lymphatic system lacks a pump. The same mechanisms that promote venous return in blood vessels act here as well— -the milking action of active skeletal muscles, -pressure changes in the thorax during breathing, - and valves to prevent backflow. Also:-pulsations of nearby arteries also promote lymph flow. - contraction of smooth muscle in the walls of the lymphatic vessels . Notice that when physical activity or passive movements increase, lymph flows much more rapidly .Hence, it is a good idea to immobilize a badly infected body part to hinder flow of inflammatory material from that region. HOMEOSTATIC IMBALANCE Anything that prevents the normal return of lymph to the blood, such as blockage of the lymphatics by tumors or removal of lymphatics during cancer surgery, results in short-term but severe localized edema (lymphedema). • Usually, however, lymphatic drainage is eventually reestablished by regrowth from the vessels remaining in the area. • To summarize lymphatic vessels functions, they (1) return excess tissue fluid to the bloodstream, (2) return leaked proteins to the blood, and (3) carry absorbed fat from the intestine to the blood (through lacteals). Lymphoid Cells 1- Lymphocytes, they arise in red bone marrow , then mature into one of the two main varieties of immunocompetent cells—T cells (T lymphocytes) or B cells (B lymphocytes)—that protect the body against antigens. • (Antigens are anything the body perceives as foreign, such as bacteria and their toxins, viruses, mismatched RBCs, or cancer cells.) 2- Macrophages play a crucial role in body protection and in the immune response by phagocytizing foreign substances and by helping to activate T cells. Lymphoid tissues and organs Lymph Nodes The principal lymphoid organs in the body are the lymph nodes, which cluster along the lymphatic vessels .Lymph nodes vary in shape and size, but most are bean shaped and less than 2.5 cm (1 inch) in length. • There are hundreds of these small organs, but because they are usually embedded in connective tissue, they are not ordinarily seen. • Large clusters of lymph nodes occur near the body surface in the inguinal, axillary, and cervical regions . • Lymph nodes have two basic functions : (1) They act as lymph “filters.” Macrophages effectively preventing pathogens from being delivered to the blood. (2) They help activate the immune system. Lymphocytes monitor the lymphatic stream for the presence of antigens and mount an attack against them. Circulation in the Lymph Nodes Lymph enters the convex side of a lymph node through a number of afferent lymphatic vessels. It then finally exits the node at its hilum (hi′lum), the indented region on the concave side, via efferent lymphatic vessels. • Because there are fewer efferent vessels draining the node than afferent vessels feeding it, the flow of lymph through the node stagnates somewhat, allowing time for the lymphocytes and macrophages to carry out their protective functions. • Lymph passes through several nodes before it is completely cleansed. HOMEOSTATIC IMBALANCE -When large numbers of pathogen are trapped in the nodes, the nodes become inflamed, swollen, and tender to the touch( swollen glands). -Lymph nodes can also become secondary cancer sites, particularly in metastasizing cancers that enter lymphatic vessels and become trapped there. The fact that cancer-infiltrated lymph nodes are swollen but usually not painful helps distinguish cancerous lymph nodes from those infected by microorganisms. Spleen The soft, blood-rich spleen is about the size of a fist and is the largest lymphoid organ. Located in the left side of the abdominal cavity just beneath the diaphragm, it curls around the anterior aspect of the stomach .It is served by the large splenic artery and vein, which enter and exit the hilum on its slightly concave anterior surface. The spleen performs four functions: 1. Its macrophages remove debris and foreign matter from blood flowing through its sinuses. 2. It stores some of the breakdown products of red blood cells for later reuse (for example, iron for making hemoglobin) and releases others to the blood for processing by the liver. 3. It is a site of erythrocyte production in the fetus (a capability that normally ceases after birth). 4. It stores blood platelets. HOMEOSTATIC IMBALANCE Because the spleen’s capsule is relatively thin, a direct blow or severe infection may cause it to rupture, spilling blood into the peritoneal cavity. Splenectomy was the standard treatment . -During the past 20 years, surgeons have discovered that, if left alone, the spleen can often repair itself so splenectomies has decreased . -If the spleen is removed, the liver and bone marrow take over most of its functions. -In children younger than 12, the spleen will regenerate if a small part of it is left in the body Thymus The bilobed thymus (thi′mus) is found in the inferior neck and extends into the superior thorax, where it partially overlies the heart deep to the sternum. - By secreting the hormones thymopoietin and the thymosins, the thymus causes T lymphocytes to become immunocompetent; that is, it enables them to function against specific pathogens in the immune response. -Prominent in newborns, the thymus continues to increase in size during the first year, when it is highly active. -After puberty, it starts to atrophy gradually and by old age it has been replaced almost entirely by fibrous and fatty tissue and is difficult to distinguish from surrounding connective tissue. Tonsils The tonsils are the simplest lymphoid organs. They form a ring of lymphatic tissue around the entrance to the pharynx (throat), where they appear as swellings of the mucosa . The tonsils are named according to location: -The paired palatine tonsils are located on either side at the posterior end of the oral cavity. These are the largest of the tonsils and the ones most often infected. - The lingual tonsil , a lumpy collection of lymphoid follicles at the base of the tongue. -The pharyngeal tonsil (referred to as the adenoids if enlarged) is in the posterior wall of the nasopharynx. -The tonsils gather and remove many of the pathogens entering the pharynx in food or in inhaled air. Aggregates of Lymphoid Follicles Peyer’s patches (pi′erz) are large isolated clusters of lymphoid follicles, structurally similar to the tonsils, that are located in the wall of the distal portion of the small intestine .Lymphoid follicles are also heavily concentrated in the wall of the appendix. • Peyer’s patches and the appendix are in an ideal position : (1) to destroy bacteria (which are present in large numbers in the intestine)and (2) to generate many “memory” lymphocytes for long-term immunity. • Peyer’s patches, the appendix, and the tonsils—all located in the digestive tract—and lymphoid follicles in the walls of the bronchi (organs of the respiratory tract) and in the mucosa of genitourinary organs, are part of the collection of small lymphoid tissues referred to as mucosa-associated lymphatic tissue (MALT). • MALT protects passages that are open to the exterior from foreign matter entering them. BODY DEFENSES Two intrinsic defense systems act both independently and cooperatively to provide resistance to disease, or immunity (immun = free).Together they are called immune system. 1. The innate (nonspecific) defense system.This system has two lines. a-The first line of defense is the external body membranes— intact skin and mucosae. b-The second line of defense ,called into action whenever the first line has been penetrated, uses antimicrobial proteins, phagocytes, and inflammation to inhibit the invaders’ spread throughout the body. 2. The adaptive (or specific) defense system provides the body’s third line of defense. This defensive response takes considerably more time to mount than the innate response. Although we consider them separately, the adaptive and innate systems always work hand in hand. PART 1: INNATE DEFENSES Are the mechanical barriers that cover body surfaces and the cells and chemicals that act on the initial internal battlefronts to face pathogens (harmful or disease-causing microorganisms) and infection. • Many times, our innate defenses alone are able to destroy pathogens • In other cases, the adaptive immune system is called into action to reinforce and enhance the innate mechanisms. • In other words , the innate defenses reduce the workload of the adaptive system by preventing the entry and spread of microorganisms in the body. The body’s first line of defense ,Skin and Mucosae -As long as the epidermis is unbroken(keratin is a physical barrier and also resistant to most weak acids and bases and to bacterial enzymes and toxins) and mucosae are intact, these physical barriers, produce a variety of protective chemicals: 1. The acidity of skin secretions (pH 3 to 5) inhibits bacterial growth, and sebum contains chemicals that are toxic to bacteria. Vaginal secretions of adult females are also very acidic. 2. The stomach mucosa secretes a concentrated hydrochloric acid solution and protein-digesting enzymes. Both kill microorganisms. 3. Saliva, which cleanses the oral cavity and teeth, 4. lacrimal fluid of the eye contain lysozyme, an enzyme that destroys bacteria. 5. Sticky mucus traps many microorganisms that enter the digestive and respiratory passageways. 6. Tiny mucus-coated hairs inside the nose trap inhaled particles, and cilia on the mucosa of the upper respiratory tract sweep dust- and bacterialaden mucus toward the mouth, preventing it from entering the lower respiratory passages. Although the surface barriers are quite effective, they are breached occasionally ,when this happens and microorganisms invade deeper tissues, the internal innate defenses come into play. Second line of defense • Phagocytes 1-macrophages (“big eaters”), the chief phagocytes which derive from white blood cells called monocytes that leave the bloodstream, enter the tissues, and develop into macrophages. Free macrophages, like the alveolar macrophages of the lungs, wander throughout the tissue spaces in search of cellular debris or “foreign invaders.” Fixed macrophages like Kupffer cells in the liver and microglia of the brain are permanent residents of particular organs. Whatever their mobility, all macrophages are similar structurally and functionally. 2- Neutrophils, the most abundant type of white blood cell, become phagocytic on encountering infectious material in the tissues. 3- Eosinophils, another type of white blood cell, are only weakly phagocytic, but they are important in defending the body against parasitic worms. • Natural Killer Cells Natural killer (NK) cells, which “police” the body in blood and lymph, are a unique group of defensive cells that can lyse and kill cancer cells and virus-infected body cells before the adaptive immune system is activated. Unlike lymphocytes of the adaptive immune system, which recognize and react only against specific virus-infected or tumor cells, NK cells are far less picky. The name “natural” killer cells reflects this nonspecificity of NK cells. NK cells are not phagocytic. They attack the target cell`s membrane and release a lytic chemical which induces the target cell to undergo apoptosis (programmed cell death). • NK cells also secrete potent chemicals that enhance the inflammatory response • Inflammation The inflammatory response is nonspecific and triggered whenever body tissues are injured by physical trauma (a blow), intense heat, irritating chemicals, or infection by viruses, fungi, or bacteria. The inflammatory response has several beneficial effects: 1. Prevents the spread of damaging agents to nearby tissues 2. Disposes of cell debris and pathogens 3. Sets the stage for repair. The four cardinal signs of short-term, or acute, inflammation are redness, heat ,swelling, and pain. -If the inflamed area is a joint, joint movement may be hampered temporarily. This forces the injured part to rest, which aids healing. -Some authorities consider impairment of function to be the fifth cardinal sign of acute inflammation. Summary of nonspecific body defenses • Fever Fever, or abnormally high body temperature, is a systemic response to invading microorganisms. Body temperature is regulated by the hypothalamus, (body’s thermostat). Normally set at approximately 37°C (98.6°F), the thermostat is reset upward in response to chemicals called pyrogens (pyro = fire), secreted by leukocytes and macrophages exposed to foreign substances in the body. -High fevers are dangerous because it denatures enzymes. -Mild or moderate fever, however, seems to benefit the body. In order to multiply, bacteria require large amounts of iron and zinc,but during a fever the liver and spleen sequester these nutrients, making them less available. Fever also increases the metabolic rate of tissue cells in general, speeding up repair processes. • Antimicrobial proteins : Complement and interpheron (see before). PART II:ADAPTIVE DEFENSES Unlike the innate system, which is always ready and able to react, the adaptive system must “meet” or be primed by an initial exposure to a specific foreign substance (antigen) before it can protect the body against that substance. Three important aspects of the adaptive immune response: 1. It is specific: It recognizes and is directed against particular pathogens or foreign substances. 2. It is systemic: Immunity is not restricted to the initial infection site. 3. It has “memory”: After an initial exposure, it recognizes and mounts even stronger attacks on the previously encountered pathogens. • Two separate but overlapping arms of adaptive immunity were recognized, each using a variety of attack mechanisms : 1-Humoral immunity (hu′mor-ul), also called antibody-mediated immunity, is provided by antibodies present in the body’s “humors,” or fluids (blood, lymph, etc.). Though they are produced by lymphocytes (or their offspring), antibodies circulate freely in the blood and lymph, where they bind primarily to bacteria, to bacterial toxins, and to free viruses, inactivating them temporarily and marking them for destruction by phagocytes or complement. 2-Cellular or cell-mediated immunity -lymphocytes(cells) themselves rather than antibodies defend the body. -Also has cellular targets—virus-infected or parasite-infected tissue cells, cancer cells, and cells of foreign grafts. The lymphocytes act against such targets either directly, by killing the foreign cells, or indirectly, by releasing chemical mediators that enhance the inflammatory response or activate other lymphocytes or macrophages. The antigens are the triggers of the activity of the cells involved in these immune responses. Antigens Antigens (an′tĭ-jenz) are substances that can mobilize the immune system and provoke an immune response. Most antigens are large, complex molecules that are not normally present in the body. Consequently, as far as our immune system is concerned, they are intruders, or nonself. An almost limitless variety of foreign molecules can act as complete antigens, including virtually all foreign proteins, many large polysaccharides, and some lipids and nucleic acids. Of these, proteins are the strongest antigens. Pollen grains and microorganisms—such as bacteria, fungi, and virus particles—are antigens because their surfaces bear many different foreign macromolecules. Incomplete Antigens or Haptens As a rule, small molecules—such as peptides, nucleotides, and many hormones—are not complete antigens. But, if they link up with the body’s own proteins, the adaptive immune system may recognize the combination as foreign and mount an attack that is harmful rather than protective. (These reactions, called hypersensitivities.) • In such cases, the troublesome small molecule is called a hapten (hap′ten; haptein = grasp) or incomplete antigen. • Besides certain drugs (particularly penicillin), chemicals that act as haptens are found in poison ivy, animal dander, detergents, cosmetics, and a number of common household and industrial products. Self-Antigens: MHC Proteins The external surfaces of all our cells are dotted with a huge variety of protein molecules. Assuming our immune system has been properly “programmed,” these self-antigens are not foreign or antigenic to us, but they are strongly antigenic to other individuals. (This is the basis of transfusion reactions and graft rejection.) Among the cell surface proteins that mark a cell as self is a group of glycoproteins called MHC proteins, the major histocompatibility complex . Because millions of combinations of these genes are possible, it is unlikely that any two people except identical twins have the same MHC proteins. Cells of the Adaptive Immune System: Three cell types : • B lymphocytes or B cells contribute to humoral immunity. • T lymphocytes or T cells are non-antibody-producing lymphocytes that constitute the cell-mediated arm of adaptive immunity. • macrophages do not respond to specific antigens but has essential roles. Lymphocytes Like all other blood cells, lymphocytes originate in red bone marrow from hematopoietic stem cells. During development, lymphocytes are “educated.” The aim of this education is twofold: 1) Each lymphocyte must become able (competent) to recognize its one specific antigen by binding to it. This ability is called immunocompetence. (2) Each lymphocyte must be unresponsive to self-antigens so that it does not attack the body’s own cells. This is called self-tolerance. -B cells become immunocompetent and selftolerant in the bone marrow. -T cells are educated in the thymus under the direction of thymic hormones. The lymphoid organs where the lymphocytes become immunocompetent (thymus and bone marrow) are called primary lymphoid organs . All other lymphoid organs are referred to as secondary lymphoid organs. Humoral (antibody-mediated)Immune Response An immunocompetent but but as yet immature B lymphocyte is activated (stimulated to complete its differentiation) when antigens bind to its surface receptors. These events trigger clonal selection ,that is, stimulate the B cell to grow and then multiply rapidly to form an army of cells all exactly like itself and bearing the same antigen-specific receptors .The resulting family of identical cells, all descended from the same ancestor cell, is called a clone and clone formation is the primary immune response. Most cells of the clone become plasma cells, the antibody-secreting effector cells of the humoral response. Although B cells secrete limited amounts of antibodies, plasma cells secrete antibodies at the unbelievable rate of about 2000 molecules per second. Each plasma cell functions for 4 to 5 days and then dies. Clone cells that do not differentiate into plasma cells become long-lived memory cells that can mount an almost immediate humoral response if they encounter the same antigen again at some future time. Memory The cellular proliferation and differentiation just described constitute the primary immune response, which occurs on first exposure to a particular antigen. • The primary response typically has a lag period of 3 to 6 days after the antigen challenge. This lag period mirrors the time required for the few B cells specific for that antigen to proliferate and for their offspring to differentiate into plasma cells. • After the mobilization period, plasma antibody levels rise, reach peak levels in about 10 days, and then decline . If (and when) someone is reexposed to the same antigen, whether it’s the second or the twenty-second time, a secondary immune response occurs. Secondary immune responses are faster, more prolonged, and more effective, because the sensitized memory cells are already in place . These memory cells provide what is commonly called immunological memory. Within hours after recognition of the “old enemy” antigen, a new army of plasma cells is being generated. Within 2 to 3 days the antibody titer (concentration) in the blood rises steeply to reach much higher levels than were achieved in the primary response. Secondary response antibodies not only bind with greater affinity (more tightly), but their blood levels remain high for weeks to months. Memory cells persist for long periods in humans and many retain their capacity to produce powerful secondary humoral responses for life. Active and Passive Humoral Immunity When your B cells encounter antigens and produce antibodies against them, you are exhibiting active humoral immunity . • Active immunity is (1) naturally acquired when you get a bacterial or viral infection, during which time you may develop symptoms of the disease and suffer a little (or a lot), and (2) artificially acquired when you receive vaccines. Indeed, once it was realized that secondary responses are so much more vigorous than primaries, the race was on to develop vaccines to “prime” the immune response by providing a first meeting with the antigen. Most vaccines contain pathogens that are dead or attenuated (living , but extremely weakened). Passive humoral immunity Instead of being made by your plasma cells, the antibodies are harvested from the serum of an immune human or animal donor. As a result, your B cells are not challenged by antigens, immunological memory does not occur, and the protection provided by these antibodies ends when they naturally degrade in the body. -Passive immunity is conferred naturally on a fetus or infant when the mother’s antibodies cross the placenta or are ingested with the mother’s milk. For several months after birth, the baby is protected from all the antigens to which the mother has been exposed. -Passive immunity is artificially conferred via a serum such as gamma globulin, which is administered after exposure to hepatitis. Other immune sera are used to treat poisonous snake bites (antivenom), botulism, rabies, and tetanus (antitoxin) because these rapidly fatal diseases would kill a person before active immunity could be established. The donated antibodies provide immediate protection, but their effect is short-lived (two to three weeks). Antibodies Antibodies, also called immunoglobulins (Igs) (im″uno-glob′u-linz), constitute the gamma globulin part of blood proteins. As mentioned earlier, antibodies are proteins secreted by activated B cells or plasma cells in response to an antigen, and they are capable of binding specifically with that antigen. They are formed in response to an incredible number of different antigens. Despite their variety, all antibodies can be grouped into one of five Ig classes, each slightly different in structure and function. Basic Antibody Structure Regardless of its class, each antibody has a basic structure consisting of four looping polypeptide chains linked together by disulfide (sulfur-to-sulfur) bonds . -Two of these chains, the heavy (H) chains, are identical to each other and contain more than 400 amino acids each. -The other two chains, the light (L) chains, are also identical to each other, but only about half as long as each H chain. The four chains combined form a molecule, called an antibody monomer (mon′o-mer), with two identical halves, each consisting of a heavy and a light chain. The molecule as a whole is T or Y shaped. • Each chain forming an antibody has a variable (V) region at one end and a much larger constant (C) region at the other end. Antibodies responding to different antigens have very different V regions, but their C regions are the same (or nearly so) in all antibodies of a given class. • The V regions of the heavy and light chains in each arm of the monomer combine to form an antigenbinding site shaped to “fit” a specific antigenic determinant. Hence, each antibody monomer has two such antigen-binding regions. Antibody Classes The five major immunoglobulin classes are designated IgM, IgA, IgD, IgG, and IgE, on the basis of the C regions in their heavy chains. (Remember the name MAGED to recall the five Ig types.) • IgD, IgG, and IgE have the same basic Y-shaped structure and thus are monomers. • IgA occurs in both monomer and dimer (two linked monomers) forms. • IgM is a huge antibody, a pentamer (penta = five) constructed from five linked monomers. • The antibodies of each class have different biological roles and locations in the body. IgM is the first antibody class released to the blood by plasma cells. IgG is the most abundant antibody in plasma and the only Ig class that crosses the placental barrier. IgA dimer, also called secretory IgA, is found primarily in mucus and other secretions that bathe body surfaces. It plays a major role in preventing pathogens from gaining entry into the body. IgE antibodies, found in minute quantities in blood, are the “troublemaker” antibodies involved in some allergies. IgD is important in activation of B cells. Cell-Mediated Immune Response Antibodies are fairly useless against intracellular pathogens (such as viruses, and the tuberculosis bacillus that quickly slip inside body cells to multiply there), fungi, malignant cells, and grafts of foreign tissue. In these cases, the cell-mediated arm of adaptive immunity comes into play . No antibodies are produced. The T cells that mediate cellular immunity are much more complex than B cells in both classification and function. There are Four populations of T cells : - CD4 cells are primarily helper T cells (TH), - CD8 cells are cytotoxic T cells (TC), whose role is to destroy any cells in the body that harbor anything foreign. - Regulatory T cells (TReg), - Memory T cells, and some fairly rare subgroups. The first step is the recognition of the foreign antigen by macrophages (antigen presenter) that present the antigen to helper T cells which become activated. • These activated helper T cells, which are antigen specific, divide many times to form memory T cells and cytotoxic (killer) T cells . • the helper T cells direct or help complete the activation of all other immune cells(B cells) so defect in T helper is very serious as it affects both T and B immunity. -The memory T cells will remember the specific foreign antigen and become active if it enters the body again. - Cytotoxic T cells are able to chemically destroy foreign antigens by disrupting cell membranes. This is how cytotoxic T cells destroy cells infected with viruses and prevent the viruses from reproducing. These T cells also produce cytokines, which are chemicals that attract macrophages to the area and activate them to phagocytize the foreign antigen and cellular Debris. -regulatory T (TReg) cells (formerly known as suppressor T cells) dampen the immune response either by direct contact or by releasing inhibitory cytokines. Organ Transplants and Prevention of Rejection Immune rejection presents a particular problem when the goal is to transplant organs from a living or recently deceased donor. Essentially, there are four major varieties of grafts: 1. Autografts are tissue grafts transplanted from one body site to another in the same person. 2. Isografts are grafts donated to a patient by a genetically identical individual, the only example being identical twins. 3. Allografts are grafts transplanted from individuals that are not genetically identical but belong to the same species. 4. Xenografts are grafts taken from another animal species, into a human being. Homeostatic Imbalances of Immunity 1-Immunodeficiencies Congenital or acquired condition that causes immune cells, to behave abnormally. The most devastating congenital conditions are a group of related disorders called severe combined immunodeficiency (SCID) syndromes, which may affect both B and T. • There are various acquired immunodeficiencies. For example, Hodgkin’s disease, cancer of the B cells, Immunosuppressive drugs and certain drugs used to treat cancer also suppress the immune system. • The most devastating of the acquired immunodeficiencies is acquired immune deficiency syndrome (AIDS), which cripples the immune system by interfering with the activity of helper T cells so produce a marked deficit of B and T cells. 2-Autoimmune Diseases Occasionally the immune system loses its ability to distinguish friend (self) from foe (foreign antigens). When this happens, the immune system, turns against itself. • The body produces antibodies (autoantibodies) and sensitized TC cells that destroy its own tissues. • This puzzling phenomenon is called autoimmunity. If a disease state results, it is referred to as autoimmune disease. 3-Hypersensitivities Result when the immune system causes tissue damage as it fights off a perceived threat (such as pollen or animal dander) that would otherwise be harmless to the body. • People rarely die of hypersensitivities; they are just miserable with them. • The different types of hypersensitivity reactions are distinguished by: (1) their time course, and (2) whether antibodies or T cells are involved. -Hypersensitivities mediated by antibodies are the immediate and subacute hypersensitivities. -T cells cause delayed hypersensitivity. Developmental Aspects of the Immune System 1. Development of the immune response occurs around the time of birth. The ability of the immune system to recognize foreign substances is genetically determined. 2. The nervous system plays an important role in regulating immune responses, possibly through common mediators. Depression impairs immune function. 3. With aging, the immune system becomes less responsive. The elderly more often suffer from immune deficiency, autoimmune diseases, and cancer.