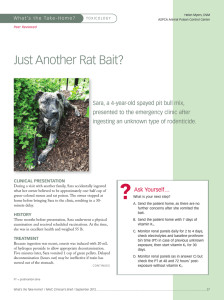
pediatric toxicology
advertisement

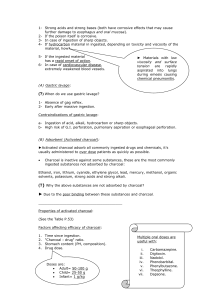
Badrinath Narayan, PEM Fellow Pediatric AHD, Aug 5th 2014 PEDIATRIC TOXICOLOGY Objectives Provide a general approach to the poisoned patient History, physical, investigations Introduce types of decontamination with indications/complications List “Pills that Kill” Poisoning Poisoning One of the most common medical emergencies Exploratory behaviour Child abuse Environmental exposures Suicide attempts In utero toxicants Pediatricians have a role in advocacy Modes of exposure: Ingestion, ocular exposure, topical exposure, envenomation, inhalation and transplacental exposure. Approach Brief window of opportunity to make critical diagnostic and management decisions Prioritize critical assessment and simultaneous management interventions 14 year old female found unconscious in a park by friends The patient is brought into the trauma bay at BCCH ED What would you do? Primary Survey ABCDEFG Apply monitors - O2, HR, RR, cycling BP Obtain vitals: HR, RR, BP, O2 sat A – Maintain patency, assess reflexes, note GCS, have airway equipment ready B - Apply O2, consider ETCO2, ABG C – Assess perfusion, Get two large bore Ivs Disability (GCS, pupil size and reactivity), ? Signs of trauma Decontamination Drug Treatment – dextrose, oxygen, narcan Bedside Glucose Primary Survey Pay special attention to: Evidence of impaired airway protective reflexes Many poisoned patients will vomit Elective endotracheal intubation may be indicated at a lower threshold Anticipate imminent respiratory failure Cyanosis/apnea are late findings Case The patient has been stabilized What would you ask? History – known intoxicant Take standard AMPLE history plus: What was ingested, How much, When, Why? Obtain prescription bottles when possible, and be sure that bottles contain med listed Talk to patient’s family and friends in ED/contact home Ensure belongings are looked at to identify paraphernalia In a toddler think single pills, in an adolescent think co-ingestions!! When to suspect? Suspected but unknown intoxicant: Acute onset of illness Pica-prone age (1-5) History of pica, ingestions Current household “stress” Significantly altered mental status Family medications/recent illnesses Social: grandparents visiting, holiday parties, other events Case On exam what things might you see to suggest a toxicological cause for the child’s presentation? Physical Vitals GCS/mental status Pupils, EOM, fundi Mouth: corrosive lesions, odors, secretions Respiratory: rate, chest excursion, air entry CVS: rate, rhythm, perfusion GI: motility, corrosive effects Skin colour, burns, diaphorsis, piloerection, track marks Bladder size Odours Removal of toxic substance Decontamination: Removal of a substance prior to entry into the circulation Elimination: Removal of a substance by enhanced excretion once it has entered the circulation Approach to decontamination Get help -- Poison control centre 24-hour Line: 604-682-5050 or 1-800567-8911 Healthcare professionals only line: 604-707-2787 or 1-866-298-5909 (outside the Lower Mainland) Monday to Friday from 9 am - 4 pm Forms of Decontamination Topical flush aggressively (ocular or skin), remove contaminated clothing Dilution Ipecac (no longer recommended; AAP statement against it) Activated Charcoal Gastric Lavage – also fallen out of favour Whole Bowel Irrigation Dilution Indicated if toxin produces only simple irritation Controversial for caustic agents May be used in first few minutes NOT for drugs – may increase absorption Not if upper airway compromise Water or milk E.g. dish soap Activated Charcoal “Activation” increases surface area of particles Toxins adsorb to activated charcoal decreasing amount adsorbed by the body Some toxins are not well adsorbed – most small molecules Iron, the alcohols, lithium, strong acids and alkali, sodium, chloride. Dose: 10:1 charcoal to drug ratio. For unknown ingestions dosing is based on ability to tolerate the agent: Children - 1 gram/kg of body weight. Activated Charcoal Timing If not contraindicated there does not seem to be a reasonable time that is too late to give AC, especially with SR or DR products Dogma used to be an hour but studies with respect to delayed gastric emptying have challenged this data Multiple-dose activated charcoal sustained-release products useful with drugs with low Vd, low protein binding, long half-life Activated Charcoal Activated charcoal not useful with: P esticides H ydrocarbons A cids, Alkali, Alcohols I ron L ithium, Liquids S olvents Activated Charcoal Contraindications absent gut motility or perforation if endoscopic visualization is required (e.g. caustic ingestions) loss of protective airway reflexes Complications fatal aspiration small bowel obstruction Gastric Lavage Orogastric lavage with a large bore tube (36-40 F for adult; no smaller than 22-24 F for children) RARELY recommended – not been demonstrated to improve outcome, several risks Might be considered: VERY early or after very dangerous ingestions (colchicine, arsenic) Ensure airway protected Place patient in left lateral decubitus position with the head down Have suction available for secretions Place tube (tragus-nose-xyphoid) and confirm position Lavage until fluids clear Whole Bowel Irrigation Whole bowel irrigation of the entire GI tract by instillation of large volumes of fluid Usually takes hours Has been used safely in children Most useful for substances with delayed absorption ( i.e. extended release ), not amenable to activated charcoal and with body stuffers/packers Whole Bowel Irrigation Accomplished by orally taking (or through NG) large volumes of Nulytely (approved for children and adults), Colyte, or Golytely Adolescents: mininum of 1.5-2 L/hour Children: 25 mL/kg/h Give until rectal effluent is clear. Whole Bowel Irrigation Contraindications: absent bowel sounds bowel obstruction or perforation unprotected compromised airway hemodynamic instability Forms of Elimination Urine alkalinization - promotes excretion of salicylate, enhances clearance of some drugs Dialysis Charcoal Hemoperfusion Dialysis Consider nephrology consult with dialysis if: S alicylates T heophylline U remia M ethanol B arbiturates L ithium E thylene Glycol Antidotes Poison Antidote Acetaminophen N-acetylcysteine Anticholinergics Physostigmine Cholinergics Atropine Benzodiazepines Flumazenil Carbon monoxide Oxygen Cyanide Amyl nitrite, sodium nitrite, sodium thiosulfate, hydroxycobalamin Digoxin Ethylene glycol Digoxin-specific Antibodies Ethanol/fomepizole, thiamine and pyridoxine Poison Antidote Heavy metals Dimercaprol (BAL), EDTA, penicillamine Hypoglycemic agents Dextrose, sucrose, octreotide Iron Deferoxamine mesylate Isoniazid Pyridoxine Methanol Ethanol/fomepiz ole, folic acid Methemoglobin Methylene blue emia Opioids Naloxone Organophospha Atropine, tes pralidoxamine Avoid physostigmine if TCA ingestion present - has potential to worsen ventricular conduction defects and to lower seizure threshold. Investigations Select tests only Help confirm diagnosis Help monitor Help identify “silent” killers Tox screens not useful in acute management Investigations All symptomatic patients with unknown ingestion should get electrolytes, glucose, osmolarity, acetaminophen/ASA levels, blood gas, EKG All suicidal patients should get acetaminophen level (~1:500 patients without a history of APAP ingestion will have a potentially toxic blood level - NYPCC) and ASA level Other tests based on history, physical, level of suspicion CBC Specific drug levels Urinanalysis BHCG Calcium, liver function panel Increased anion gap metabolic acidosis (Na – (Cl + HCO3) M ethanol (hx of alcohol abuse, methanol level), metformin U remia (BUN) D KA, AKA, SKA (hx; urine ketones) P araldehyde (distinctive odor) I soniazid (seizure; lactate level) L actic acidosis E thylene glycol (level) S alicylates/solvents (level) Increased Osmolar gap (serum – calculated) “Two salts and a sticky BUN” M annitol A lcohols D ye G lycerol A cetone S orbitol Pitfalls of osmolar gap Cannot distinguish between type of toxic alcohol Insensitive in late presentations Not sufficiently sensitive to exclude small ingestion Cannot rule out ingestion based on a normal OG Radio-opaque drugs Chloral Hydrate Opioid packets (latex) Iron and other heavy metals Neuroleptics Sustained release tablets/Salicylates ECG Findings include: Toxicologic tachcyardia/bradycardia QRS widening Prolonged QT (www.qtdrugs.org) Findings can develop late so obtain serial ECGs Case A 2 year old girl is found playing with his grandmother’s pill box. Some pills may be missing and a powder residue is found in the child’s mouth. What medications would most concern you if this child ate “just one pill”? ONE PILL KILLERS Small dose toxins Substance Major symptom Symptom onset Beta-adrenergic antagonists(sustained release) Bradycardia, hypotension Delayed, up to 24 hours Buproprion(sustained release) Seizure, cardiovascular collapse Delayed up to 24 hours CCB (sustained release) Bradycardia, hypotension dElayed, up to 24 hours Clonidine Apnea, bradycardia, hypotension 1-2 hours Lomotil (Diphenoxylate/Atropine) Apnea Delayed, up to 24 hours Methylsalicylate (oil of wintergreen) Metabolic acidosis, pulmonary/cerebral edema 1-6 hours Opioids: extended release preparations Apnea Delayed, up to 24 hours Medications Methadone 1 – 2 hours Sulfonylureas Hypoglycemia Delayed, up to 24 hours Theophylline Seizure, hypotension Delayed, up to 24 hours Camphor Seizure Minutes to hours Pesticides SLUDGE Minutes to hours Toxic alcohols Blindness, renal failure, metabolic acidosis 3 – 8 hours (ethylene glycol) 3 – 18 hours( methanol) Other agents Case A 3 yo male presents to the ED comatose with a GCS of 6. He was found on the bathroom floor. Following stabilization, what is the most immediate course of action? A. Head CT B. ECG C. Tox screen D. Broad spectrum Abx