DRUGS AFFECTING CLOT FORMATION
advertisement
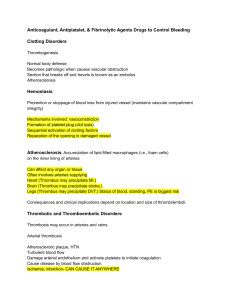
Blood coagulation is a complex process that involves vasoconstriction, platelet clumping or aggregation, and a cascade of clotting factors produced in the liver that eventually react to break down fibrinogen (a protein also produced in the liver) into insoluble fi brin threads. 2 Damaged vessel endothelium is a stimulus to circulating platelets, causing platelet adhesion. B. Platelets release mediators, and platelet aggregation results. 3 4 Drugs that affect clot formation include: - antiplatelet drugs, which alter platelet aggregation and the formation of the platelet plug; - anticoagulants, which interfere with the clotting cascade and thrombin formation; and - thrombolytic agents, which break down the thrombus or clot that has been formed by stimulating the plasmin system. 5 Antiplatelet agents decrease the formation of the platelet plug by decreasing the responsiveness of the platelets to stimuli that would cause them to stick and aggregate on a vessel wall. Antiplatelet agents available for use Include: abciximab (ReoPro), anagrelide (Agrylin), aspirin, cilostazol (Pletal), clopidogrel (Plavix), dipyridamole (Persantine), eptifibatide (Integrilin), ticlopidine (Ticlid), ticagrelor (Brilinta), and tirofiban (Aggrastat 6 - Abciximab, eptifi batide, and tirofi ban are administered intravenously (IV). - Antiplatelet agents that are administered orally include anagrelide, aspirin, cilostazol, clopidogrel,ticagrelor, and ticlopidine. - Dipyridamole is used orally or as an IV agent. These drugs are generally well absorbed and highly bound to plasma proteins. They are metabolized in the liver and excreted in urine, and they tend to enter breast milk . 7 - Antiplatelet agents are contraindicated in the presence of allergy to the specific drug. - Caution should be used in the following conditions: the presence of any known bleeding disorder because of the risk of excessive blood loss; recent surgery because of the risk of increased bleeding in unhealed vessels;and closed head injuries because of the risk of bleeding from the injured vessels in the brain 8 Although there are no adequate studies of these drugs in pregnancy, they are contraindicated with pregnancy because of the potential for increased bleeding (see Adverse Effects); they should be used during pregnancy only if the benefi ts to the mother clearly outweigh the potential risks to the fetus. These drugs are also contraindicated during lactation because of the potential adverse effects on the fetus or neonate; if they are needed by a breast-feeding mother, she should fi nd another method of feeding the baby. 9 Platelet levels should be checked regularly to monitor for thrombocytopenia if a patient is on this drug. 10 headache, dizziness, and weakness Nausea and gastrointestinal (GI) distress may occur because of direct irritating effects of the oral drug on the GI tract. Skin rash, another common effect, may be related to direct drug effects on the dermis. 11 Anticoagulants are drugs that interfere with the normal coagulation process by interfering with the clotting cascade and thrombin formation. Drugs in this class include: antithrombin III (Thrombate III), argatroban (Acova), bivalirudin (Angiomax), desirudin (Iprivask), fondaparinux (Arixtra), heparin (generic), and warfarin (Coumadin) and the two newest oral anticoagulants dabigatran (Pradaxa) and rivaroxaban (Xarelto). 12 Pharmacokinetics Heparin is injected IV or subcutaneously and has an almost immediate onset of action. It is excreted in urine. Warfarin, dabigatran, and rivaroxaban are used orally. 13 Warfarin is readily absorbed through the GI tract, metabolized in the liver, and excreted in urine and feces. Warfarin’s onset of action is about 3 days; its effects last for 4 to 5 days. Because of the time delay, warfarin is not the drug of choice in an acute situation, but it is convenient and useful for prolonged effects. 14 The most commonly encountered adverse effect of the anticoagulants is bleeding, ranging from bleeding gums with tooth brushing to severe internal hemorrhage. Warfarin has been associated with alopecia and dermatitis, as well as bone marrow depression. 15 - The anticoagulants are contraindicated in the presence of known allergy to the drugs. - They also should not be used with any conditions that could be compromised by increased bleeding tendencies, including hemorrhagic disorders, recent trauma, spinal puncture, GI ulcers, recent surgery, intrauterine device placement, tuberculosis, presence of indwelling catheters, and threatened abortion. 16 - Warfarin is contraindicated in pregnancy because fetal injury and death have occurred; in lactation, because of the potential risk to the baby; and in renal or hepatic disease. - heparin does not enter breast milk, and so it is the anticoagulant of choice if one is needed during lactation. 17 Evaluate for therapeutic effects of warfarin— prothrombin time (PT) 1.5 to 2.5 times the control value or ratio of PT to International Normalized Ratio (INR) of 2 to 3— to evaluate the effectiveness of the drug dose. ■ Evaluate for therapeutic effects of heparin—whole blood clotting time (WBCT) 2.5 to 3 times control or activated partial thromboplastin time (APTT) 1.5 to 3 times the control value—to evaluate the effectiveness of the drug dose. 18 ■ Evaluate the patient regularly for any sign of blood loss (petechiae, bleeding gums, bruises, dark-colored stools, dark-colored urine) . 19 ■ Establish safety precautions to protect the patient from injury. ■ Provide safety measures, such as use of an electric razor and avoidance of contact sports, to decrease the risk of bleeding. ■ Provide increased precautions against bleeding during invasive procedures; use pressure dressings; avoid intramuscular injections; and do not rub subcutaneous injection sites because the state of anticoagulation increases the risk of blood loss. 20 ■ Mark the chart of any patient receiving this drug to alert the medical staff that there is a potential for increased bleeding. ■ Maintain antidotes on standby (protamine sulfate for heparin, vitamin K for warfarin) in case of overdose. ■ Monitor the patient carefully when any drug is added because of the risk of drug–drug interactions that would change the effectiveness of the anticoagulant. 21 THROMBOLYTIC AGENTS 22