Femoral Acetabular Impingement - MUSC Musculoskeletal Radiology
advertisement

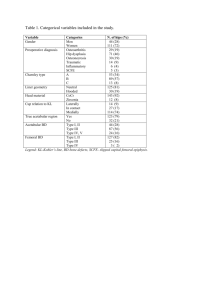
Femoral Acetabular Impingement: excerpt from “New Developments in Hip Imaging” Reto Sutter, Marco Zanetti, and Christian W. A. Pfirrmann. Radiology, September 2012 (264) p651-667. Femoroacetabular Impingement Background Early-onset osteoarthritis of the nondysplastic hip is commonly caused by FAI (74). FAI is further divided into cam-type impingement with deformities of the femoral head and neck, pincer-type impingement with focal or general overcoverage of the acetabulum, and mixed-type FAI with both cam- and pincer-type features (75,76). Typically, Patients with FAI become symptomatic in early adulthood (77). There is some debate whether cam-type and pincer-type impingement constitute strictly separate entities, or whether most cases of FAI involve a mixed origin. While the Bernese group reported that 61%–86% of patients have a combination of both forms of impingement (78,79), other authors insist that cam and pincer are distinct entities (80) or report an intermediate value of 42% of patients with cam-type morphology who also have a pincer deformity (76). The initial imaging of patients suspected of having FAI should be performed by using radiography. Some of the geometric abnormalities are very subtle and require a highly standardized radiographic technique. Rotation and tilting of the pelvis will lead to false-positive or false-negative findings. For the anteroposterior view of the pelvis, the patient lies on the examination table and the central beam is directed to the midpoint between a line connecting both anterosuperior iliac spines and the superior border of the symphysis (81,82). In a correct anteroposterior view the distance between the sacrococcygeal joint and the pubic symphysis is an average of 32 mm in men and 47 mm in women (81). The pelvis exhibits a normal rotation if the middle of the sacrococcygeal joint and the pubic symphysis are aligned (82). Acetabular Retroversion Acetabular retroversion may lead to pincer-type FAI due to an anterolateral focal overcoverage of the acetabulum (83). Three signs are indicative of acetabular retroversion on radiographs: the crossover sign, the posterior wall sign, and the ischial spine sign (Fig 6). In the crossover sign, also called the “figure of 8” sign, the anterior wall of the acetabulum crosses over the posterior wall to the lateral side, whereas in the normally oriented acetabulum the anterior wall is strictly medial to the posterior wall (84,85). The posterior wall sign is present if the center of the femoral head is located lateral to the posterior acetabular wall, whereas it is located medial to the posterior wall in the normally oriented acetabulum (84). And finally, the ischial spine sign is positive if the projected shape of the ischial spine protrudes and is visible medial to the pelvic rim (86). The ischial spine sign carries a sensitivity of 90% and a specificity of 71% on clinical radiographs for diagnosing acetabular retroversion even when the pelvis is tilted or rotated (87). The crossover and posterior wall signs seem to be associated with progression of osteoarthritis of the hip (88). All three signs are subject to intra- and interindividual error, as a recent report has confirmed (89): Only the posterior wall sign had a substantial interindividual agreement with a κ value of 0.633. The crossover sign had the least intra- and interobserver reliability. Furthermore, correct assessment of acetabular retroversion was related to the observer’s individual experience in identifying these signs on radiographs, rather than years of clinical practice (89). View larger version: In this page In a new window Download as PowerPoint Slide Figure 6: Schematic of left hip as seen on anteroposterior views of pelvis demonstrate radiographic signs of (a, b) general overcoverage of the acetabulum or (c–e) focal overcoverage of the acetabulum due to acetabular retroversion. (a) Coxa profunda with floor of acetabular fossa (red line) overlapping ilioischial line (dashed line). (b) Protrusio acetabuli with medial aspect of femoral head (red line) overlapping ilioischial line (dashed line). (c) Crossover sign, also known as “figure of eight” sign. Superior aspect (solid green line) of anterior acetabular wall (dashed green line) crosses over posterior wall to the lateral side. (d) Posterior wall sign with center of femoral head (red dot) located lateral to posterior acetabular wall (red line). (e) Ischial spine sign with shape of ischial spine protruding medial of pelvic rim. Acetabular Depth An increased acetabular depth refers to the general overcoverage of the acetabulum (Fig 6, 6b), rather than only focal overcoverage, and is associated with pincer-type FAI (77). A coxa profunda can be diagnosed on a correctly positioned anteroposterior radiograph of the pelvis, if the floor of the acetabular fossa touches or overlaps the ilioischial line medially (90). If the acetabular overcoverage is even more pronounced and the femoral head can be seen overlapping the ilioischial line medially, the condition is called protrusio acetabuli (91). An alternative method for determining general overcoverage is the center-edge angle (the Wiberg angle), which is the angle between a straight vertical line and a line through the acetabular edge, with both crossing at the center of the femoral head: An angle of 39°–44° represents coxa profunda, and an angle greater than 44° represents protrusio acetabuli (92). In a study with 46 patients, a center-edge angle of more than 40° was reported to be a useful sign for diagnosing pincer-type FAI, with a specificity of 100% but only a moderate sensitivity of 84% (93). While the precise diagnosis of focal overcoverage of the acetabulum has received considerable attention in the past few years, general overcoverage of the acetabulum has been less debated. A long-term (at least 10 years) follow-up study has shown that coxa profunda is associated with the progression of osteoarthritis; however, an even stronger association has been found between coxa vara and osteoarthritis progression (88). Geometric Deformities of the Femoral Head and Neck Initial assessment of deformities of the proximal femur that contribute to cam-type FAI is performed with radiographs, and deformities can be detected on both the anteroposterior view and the crosstable lateral view. Recent studies have shown limited reliability when assessing the anterior headneck junction deformity by using the alpha angle on radiographs: Correlation between the frog-leg view and CT images was low, with an intraclass correlation coefficient of 0.08 (94), but the Dunn view seems to be more useful, with a Pearson correlation coefficient of 0.7 and an accuracy of 90%, when compared with MR imaging (95). One needs to be aware that radiographic evaluation of the head-neck junction has limited reliability for assessing the exact extent of cam-type deformities, with a low interobserver agreement (κ = 0.19–0.24 for different radiographic projections) and low to moderate intraobserver agreement (κ = 0.30–0.55) (96). Furthermore, normal findings on radiographs do not exclude cam-type impingement, as has been shown in a retrospective analysis of 58 patients (79). Assessment of Cam-Type Deformities While radiography plays an important role as a baseline examination in the evaluation of patients in whom osteochondroplasty of the femoral head-neck junction is planned, MR imaging with radial images enables more accurate assessment of the extent of the deformities (79). The alpha angle was originally introduced by Nötzli et al (97) on oblique axial gradient-echo MR images obtained parallel to the axis of the femoral neck, to quantify the cam-type deformity. The authors of the initial study reported interobserver differences of plus or minus 7% for the alpha angle (97). However, validation of the measurement of the alpha angle produced only moderate results after repeated assessments by the same reader (98) and interobserver differences of up to 30% (99). Initially, the alpha angle was only measured anteriorly at the 9 o’clock position (97). Later, radial plane images rather than oblique axial plane images have been used for the measurement of the alpha angle, to assess not only the anterior head-neck junction but also the whole circumference (75). The maximum cam-type deformity of the femoral neck is commonly located at the anterosuperior position (Fig 7) (75). As a result, the classic anterior alpha angle on MR images or the anterior or lateral alpha angle on radiographs will not demonstrate the maximum deformity (22,95,100). Measurement of the alpha angle on radiographs is incomplete and neither facilitates a reliable decision whether surgery is necessary nor allows for adequate preoperative planning (100). View larger version: Figure 7: Cam-type FAI of left hip in a 38-year-old man. (a) Sagittal 3D double-echo steady-state MR arthrographic image (25/9) demonstrates labral detachment (arrowhead). ○ = center of femoral head. Dashed line represents plane of (b) radial reconstruction from transverse 3D true fast imaging with steady-stage precession MR study (12/6). Abnormal alpha angle α of 65° in the anterosuperior portion of femoral head-neck junction is due to cam-type deformity. The anterosuperior labral detachment can also be seen (arrowhead). Alpha angle is measured between axis of femoral neck and line from center of femoral head to the point where distance from center to peripheral contour of femoral head exceeds radius of the femoral head. Axis of femoral neck is defined as a line that passes through center of femoral head and center of femoral neck at its narrowest point. d/2 = half of femoral neck diameter. Three-dimensional CT data can be used to assess cam-type deformities by means of an automated multiple radial plane analysis (101). Preoperative 3D CT in patients with FAI was found to be of only moderate value for predicting arthroscopic findings, with κ values of 0.48 for cam-type FAI and 0.16 for pincer-type FAI (102). In addition, 3D CT data can be used for kinematic analysis of the hip joint with simulations of the range of motion before and after surgical treatment for FAI (103,104). Sonographic evaluation of cam-type FAI has also been utilized. Sonography is able to depict camtype deformities of the anterior and anterosuperior regions of the femoral head-neck junction (Fig 8) with a sensitivity of 89%–93%, albeit with a low specificity of 14%–36% (105). The same technique was unreliable in the calculation of the alpha angle in the anterior and anterosuperior regions: Receiver operating characteristic analysis demonstrated an area under the curve of 0.581–0.688 (105). It should be noted that evaluation of many intraarticular pathologic conditions cannot be performed with sonography. As an example, a possible mixed-type impingement would be missed at sonography, because only the osseous contours of the femoral head-neck junction can be depicted. Figure 8: Correlation of cam-type deformity of left femur at sonography and MR imaging in a 45-year-old woman with hip pain and clinical findings of FAI. (a) Transverse sonographic image shows cam-type deformity (arrowhead) at anterior portion of the femoral head-neck junction. (b) Radial reconstruction of 3D transverse oblique true fast imaging with steady-state precession MR study (12/6) at the same level as a confirms cam-type deformity (arrowhead). r = Radius of femoral head. Threshold Dilemma for the Alpha Angle Regarding the threshold of the normal alpha angle, there are currently several schools of thought that use either a 50° or a 55° cutoff. While the 50° (or 50.5°) cutoff value is mainly used in the orthopedic literature (95,106–108), the 55° cutoff value is used both in the radiologic and the orthopedic literature and is the threshold that is used more often (22,75,98–100,109). Interestingly, all of these groups cite the original Nötzli et al (97) study with 39 patients and 35 asymptomatic volunteers as a basis for their choice. Nötzli et al reported a minimal alpha angle of 55° for the patient group and a maximum alpha angle of 48° for the volunteer group, but they also proposed a value of 50° as a potential threshold in the anterior position. To date, no conclusive data are available for determining an ideal cutoff value for the alpha angle, to our knowledge. The decision to perform surgery in a patient is not based on the alpha angle alone but rather on the combination of radiologic and clinical findings. Furthermore, the morphology of the acetabulum could also play a role in the development of pain and in the progression of joint degeneration in patients with FAI. Neumann et al (110) advocate that an alpha angle of 43° should be considered a sufficient postoperative result. They analyzed 45 patients who underwent osteochondroplasty for FAI and found that the alpha angle was reduced by 23° on average, resulting in a mean postoperative alpha angle of 43°. New Insights from Asymptomatic Volunteer Studies Several additional facts have become known about FAI in the past several years. Radiologic evidence of FAI is quite common in young active patients with hip complaints: At least one radiologic finding of FAI was detected in 87% of patients with symptoms in the hip, groin, or pelvis (111). In a retrospective analysis of 200 patients who underwent CT for reasons not related to the hip joint, the alpha angle was significantly larger in asymptomatic patients with herniation pits (55.2° ± 11.9) than in asymptomatic patients without herniation pits (49.8° ± 9.3), although there was a substantial overlap in the range of alpha angles between the two groups (112). Notably, several studies involved groups of asymptomatic volunteers: Cam-type deformities were detected in every fourth young asymptomatic male volunteer and in every second young male with decreased internal rotation (107,113,114). In several of these studies with volunteers, alpha angles that were previously considered abnormal have been found in many asymptomatic individuals (115), with anterosuperior angles greater than 50.5° in 53% of subjects and greater than 55° in 33.5% (107). Laborie et al (116) recently reported a large number of radiographic findings of pincer-type FAI in a large cohort study of young adults, with a prevalence of 11%–23% for the posterior wall sign and 46%–51% for the crossover sign on anteroposterior radiographs. While the authors stated that the very high prevalence of the crossover sign in their cohort might be due to differences in pelvic positioning and definitions used for a positive crossover sign compared with those used in other studies (116), it is notable that signs of acetabular overcoverage seem to be quite frequent in the general population. In a long-term follow-up study with 96 asymptomatic individuals with radiographic features of FAI, 17.7% developed osteoarthritis during a period of 19 years, while 82.3% remained free of osteoarthritis (117). Therefore, a substantial portion of hips with radiographic signs of FAI may not develop osteoarthritis in the long term (117). These studies with volunteers show that minor cam- and pincer-type deformities are relatively common in asymptomatic individuals; moreover, in the preceding section we discussed the lack of an ideal cutoff value for the alpha angle. If in daily radiologic routine a minor cam- or pincer-type deformity is found in a patient without other clinical and imaging features of FAI, it should be regarded as a normal variant or as a predisposing factor for the development of FAI and not as clear-cut proof of FAI. New Ways out of the Controversy? In light of the controversy surrounding the alpha angle, several other measurement methods have been used to assess cam-type deformities of the femoral head such as the femoral head-neck offset (95,97), the offset ratio (118), the beta angle in open-chamber MR imaging (119), or the anterior femoral distance (99), but so far none of these new parameters has met widespread acclaim. Also, although the origin of the cam-type deformity is not yet clear, a recent report links highactivity sports participation during childhood and adolescence with cam-type impingement in highactivity basketball players, when compared with an age-matched group who did not perform highactivity sports during childhood and adolescence (109). Although this study sheds some light on the development of cam-type FAI in a highly active population, it remains to be seen whether activity levels also influence the development of cam-type deformities in the general population (109). Decreased internal rotation of the hip in FAI is not dependent only on the cam-type deformity. An analysis of collision models based on CT data from 20 patients showed that femoral torsion and acetabular coverage also have to be assessed in patients suspected of having FAI (120). A decreased femoral antetorsion increases the risk of early femoroacetabular collision during normal movements and sports (120,121). A study with 126 individuals showed that femoral antetorsion was reduced in patients with cam-type FAI (mean, 10.0° ± 9.1 [standard deviation]) and increased in patients with pincer-type FAI (18.3° ± 9.8), when compared with asymptomatic volunteers (12.7° ± 10.0) (121). Consequently, in patients with cam-type FAI and substantially reduced femoral antetorsion, a rotational osteotomy of the femur might be performed in addition to femoral osteochondroplasty and acetabular rim resection (122). New attention has focused on genetic predisposition in the development of FAI. Pollard et al (123) found that siblings of patients with cam-type FAI had a relative risk of 2.8 of having a cam-type deformity, and siblings of patients with pincer-type deformities had a relative risk of 2.0 of having the same deformity, due to abnormal joint morphology.