PPTX, 3.71MB - National Aboriginal Community Controlled Health
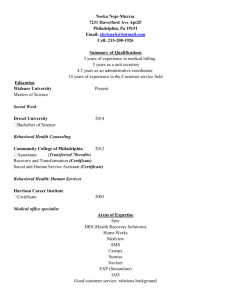
advertisement

Orientation Workshop The presenters acknowledge the Traditional Owners of the land on which we meet. Acknowledgements The Australian College of Remote and Rural Medicine (ACCRM) Department of Health and Aging NACCHO Telehealth Working Group Telehealth Working Group NACCHO’s GOAL To have all 150 member services in Australia Telehealth enabled by end of 2015 – work with affiliates How? Information, on-line training module, templates, needs analysis, technical support, funding support, business case analysis tool, on-line chat forum Government advocacy – particularly for funding for investment in technology Your choice as to whether to undertake this new technology… The stethoscope “… That it will ever come into general use, notwithstanding its value, I am extremely doubtful; because its beneficial application requires much time, and gives a good deal of trouble both to the patient and the practitioner; and because its whole hue and character is foreign, and opposed to all our habits and associations. ..” John Forbes M.D., Physician to the Penzance Dispensary and Secretary of the Royal Geological Society of Cornwall. NACCHO’s Telehealth Information Workshops Starting point To provide information and resources that will allow you to plan for and set up your service for the implementation of Telehealth consultations NACCHO’s current projects and team 1. Telehealth Support Project 2. Telehealth Delivery Project Roy Monaghan and Suzanne Jenkins Telehealth Support Project Education resources and guidelines Telehealth Orientation Workshops – 1 or 2 per state Online training module Online chat forum Development of a long term strategy Telehealth Delivery Project Needs analysis – Technology and other needs Training and other activities to meet needs Business case analysis tool for services Small grants for infrastructure Technical support and advice What is Telehealth? Telehealth is the use of information & communication to deliver health care at a distance (video conferencing) 1928. Alfred Traeger demonstrating his first pedal radio. Photo John Flynn. 1970’s -trials of video communication began By mid 1990’s several small scale video consultation services to rural areas established state health departments, universities. Expensive. July 2011 – Medicare item numbers expanded What do you use? Normal desktop or laptop computer Special purpose built systems iPads, tablets, smartphones Generally available or special computer software programs Why Telehealth? Patient Give the patient more treatment options No travel outside the community Cost savings Quicker access to specialists - faster diagnosis Better continuity of care – ability to see the specialist more frequently Culturally “safer” – consultation occurs in familiar place Less disruption to patient’s family, home, community and work life Greater equity with city communities Why Telehealth? (continued) Clinician Able to provide better and quicker care Wider referral networks Stronger relationships with specialist Access to specialist advice in an emergency Better access to information and training – sense of being better supported Why Telehealth? (continued) Service Medicare support – generous support at present in the form of incentives and rebates Ability to offer a better service to patients Allows better integration of care Get your patient seen quicker Specialist Potentially better relationship with patient and referring doctor Ability to talk with patient and clinician together Reduced travel time so more time for follow up Why Telehealth? (continued) Government Less cost – patient travel and support Better outcomes for remote and rural people Better outcomes for Aboriginal and Islander people What the research says Are Telehealth consultations any good? For dermatology, psychiatry, psycho-geriatrics, neurology, minor injuries in the emergency department, and rheumatology, there was consistently good to excellent diagnostic agreement when video consultation was compared to traditional in-person consultation. (Martin-Kahn et al., 2011) For clinical oncology and clinical genetics video consulting is effective, and comparable to in-person consultations. (Kitimura et al., 2010; Hilgart et al., 2012) What the research says (continued) Mental health This is the most researched area of Telehealth. It has been found that video consulting is: As accurate as in-person consultation for psychiatric diagnosis. (Hyler et al., 2005) Produces similar outcomes in psychotherapy treatment including cognitive behavior therapy for conditions such as post traumatic stress disorder, other anxiety disorders, anorexia, and mood disorder. (Backhaus et al., 2012) Equivalent for assessing and treating psychosis; does not trigger symptomatology in patients with schizophrenia.(Sharp et al., 2011) Effective in treating children and adolescents. (Slone & Reese, 2012) What the research says (continued) How do the patents feel about Telehealth? Patients generally report very high rates of satisfaction with video consultations. How do the clinicians feel about Telehealth? Clinicians’ rates of satisfaction are adequate, but not as high as patients. Conclusion re benefits of Telehealth Works pretty well in many clinical situations What doesn’t work so well? Physical examinations – need for the specialist to rely on the patient end clinician’s examination Evaluation of overall physical appearance – for example pallor, fine tremor, lack of affect, and a range of other things might not be easily determined remotely. Conveying or receiving emotions through body language of facial expressions Clarity on responsibilities between clinician and specialist The sense of a close healing relationship that can be achieved by in-person meetings What is the uptake of Telehealth? At the end of September 2012 the Department of Human Services had processed 42,568 Telehealth services • 26, 680 by specialists • 15,832 by GPs • 74 by Nurse Practitioners/Midwives • For 21,000 patients • By 6500 practitioners. What is the spread between states? Patient Services in each State as at 31 May 2012 35.00% 30.00% 25.00% 20.00% 15.00% 10.00% 5.00% 0.00% NSW VIC QLD SA WA TAS NT ACT Number of Services by Providers Number of services & number of providers by provider type – May 2012 8,000 Number of services 7,000 Number of providers 6,000 5,000 4,000 3,000 2,000 1,000 0 Consultant physician Psychiatry Specialist GP/ Nurse Practitioner/Midwife Eligibility Outside RA 1 areas (major cities) All patients of AMS’s Patients of Aged Care Facilities Starting Telehealth in your service What do you need? Patient (who has agreed) Room Technology Attendant clinician Specialist Workflow that works! The Patient Selecting patients for telehealth Telehealth is beneficial for patients who: Can’t readily travel (elderly, frail, physically disabled, home, cultural or work responsibilities) Will benefit from accessing specialist services in a timely manner Do not need a physical examination from the specialist, or if they do, where the attending Telehealth clinician can adequately undertake this. The Patient (continued) Patients who might have a problem with Telehealth include patients who: Are very deaf Have minimal English proficiency Have restless children in attendance. Those with personal or cultural concerns re technological based consultations Note: Current research indicates that Aboriginal patients are generally very accepting of and happy with Telehealth consultations – Source: Dr Victoria Wade, PhD student, Adelaide University. Patient Consent Your patient must agree to a Telehealth consultation based on a good understanding of what it entails Give a clear verbal explanation and a patient information sheet – test their understanding They need to know: • Why they are having a Telehealth consultation • Other options for their care if not comfortable with Telehealth. • The role of each person participating: both in the room and on the computer interface. • Out-of pocket charges and how the Telehealth session compares to other available options. • Who to give feedback to and who to complain to if any problems. • The level of security and privacy. Patient Consent (continued) The 3 Principles of Informed Consent 1. The patient needs to be given the information in a culturally appropriate manner. 2. The patient needs to understand the information. It must be in a suitable form and the patient needs time to think about it plus talk with an appropriate person which might be a family member at home. 3. The patient needs to make a choice. This choice can be revisited by the patient at any time. Patient Consent Form The Room Availability? (on-time appointments) Comfortable and culturally appropriate? Enough space? (camera view, room for family) Light? Private? (sound proof) Does it allow the equipment to function properly? Access to medical equipment? Access to other resources? The Technology Attendant Clinician There are Medicare rebates for the following types of staff to be present with the patient during the video consultation GP or other medical practitioner Aboriginal/Islander Health Worker Practice nurse Nurse Practitioner Midwife Which staff member should attend the Telehealth consultation? Complex or difficult issues about which the doctor would like advice from the specialist on diagnosis or management - attendance by referring doctor Uncomplicated (e.g. follow up) – attendance by health worker or nurse Attendant Clinician (continued) Training is essential in : Using the technology The workflow processes Making the patient comfortable Resources: Printed materials – NACCHO and others Online training module –NACCHO/ACRRM Videos Clinicians already using Telehealth The Specialist Doing Telehealth are around: 515 Consultant physicians 215 Psychiatrists 325 Specialists How do you find them? ACRRM Provider Directory (Australian College of Remote and Rural Medicine) on the eHealth section of their website Advisable to use existing referral pathways The specialist’s location mightn’t be important if you are seeking only a second opinion or if it is a one-off consultation. If the patient is likely to need to see the specialist in person – better to use someone relatively close. . ACRRM’s Specialist Provider Directory Workflow There will need to be some changes to workflow for Telehealth consultations How will you organise this? Flowchart developed by Practice Manager: Prashiba Thavarajadeva Montague Farm Medical Centre (Adelaide) Bookings and Administration Bookings Administration staff will need to know with consultations are by Telehealth and can coordinate booking the room, equipment, clinician with the patient, and the distant clinician as a single event. Allocation of Time Add a bit of extra time to begin (to check the technology and patient position. Patient to arrive about 10 minutes early. Running on Time It is essential to run on time – Have a back-up staff member available to begin the consultation if the designated person may run late. Billing Telehealth is unique - two clinicians can receive a MBS rebate for seeing the patient at the same time. The Patient-end Bill the patient in the same way as for any other service There are unique item numbers for Telehealth which attract a higher rebate than for an equivalent in-person consultation Until June 30 2014 there 3 additional incentive payments as well Billing (continued) The Distant Specialist Can send the patient a bill by post, which the patient can pay and then obtain a rebate. Alternatively, if the specialist wishes to bulk bill: The clinician with the patient can complete the assignment of benefit form on the specialist’s behalf, have the patient to sign it, and then send it to Medicare. The specialist sends the assignment of benefit form to the patient, who signs it and forwards it to Medicare. The specialist can obtain an email agreement: the specialist sends an email to the patient with details of the service and charge, and the patient replies by email agreeing to assign the benefit. The Business Case It is ideal to do an analysis of the costs and benefits of Telehealth in terms of money, time and patient care benefits. NACCHO will be embedding a business case analysis tool in our training module – It will be available separately as well Others are available as well. Workflow planning and training Lots to consider! As a first step create a flow chart or map that can be used as a focus of team discussion to define roles and processes You will need to: Make a service based decision about starting Telehealth Get a commitment to make the appropriate changes Ensure processes and roles are clear – discuss and document Make time for staff training Workflow planning (continued) Include Telehealth in your quality improvement programs At suitable time intervals (3-6 monthly) it is important to evaluate Telehealth services and their usefulness, and to discuss how processes can be improved and made more effective. Check on insurance and professional indemnity Designate a person in your service to take a coordinating role to deal with Telehealth related issues Do your first consultation! Don’t worry if there are a few things that don’t work. Fix them next time. Questions and discussion