burgess-observation-status - NY Statewide Senior Action Council
advertisement

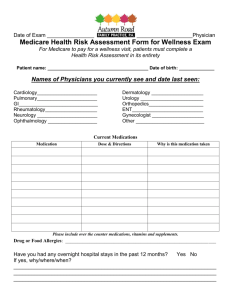
Medicare Patients Rights and Better Care Transitions Michael Burgess New York StateWide Senior Action Council, September 13, 2012 Nothing Short of a Revolution and Change in Culture of Health Care • Health Care is Quickly Moving from a Fee-forService World to a Coordinated Care Model with a Bundled Payments to Providers • Concerns about Quality of Care and Cost of Care are leading to changes in the delivery of care with heavy focus on care transitions, coaching, primary care, prevention • Shorter Stays in Hospitals are leading to the need for greater community support And yet, • “Patients and family caregivers are not adequately prepared to manage their conditions during the transition between care settings in the absence of health care professionals, leading to symptom exacerbation, an increased likelihood of crisis, inappropriate health care utilization and readmission to the hospital.” - Tompkins County Rural Community Based Care Transition Program Problem situation “Observation Status” • Hospital admissions and re-admissions practices have changed with an increase of over 20% in “observation status” classification • Beneficiaries impacted because status effects Part A and Part B Medicare payments and full out of pocket costs for nursing home rehab without 3 day admission • Little education and outreach regarding shift Patient Centered Care and Community Outreach and Services • New Models are Based on Need for Patients and Caregivers to Be More involved in care • Education and Community Outreach to patients though has not kept up with changes • Hospitals are now becoming more involved with community projects for intensive care transitions involving nurses, coaches, to assist in post hospital care Local Innovative Approaches • • • • • Care Transitions Demonstration with CMS Community Supports Navigator Health Coaches Medical Homes Target High Need Chronically Ill with Intensive support • Enhanced Prevention Efforts • NY Connects Targeting High Risk Patients • Providing intensive support and monitoring of high risk patients with serious chronic conditions to make sure that they are getting primary care, medications and support services • Focus is on patients with congestive heart failure, COPD, pneumonia, diabetes CMS Strategies to Improve Quality and Reduce Costs • • • • • • • • • Accountable Care Organizations Health Homes Financial Incentives to Reduce Re-Admissions Wellness and Prevention Initiatives Partnership for Patients Care Transitions Grants Community First Choice Independent Living Patient Safety, Reduce Medical Errors Reduce Medicare Fraud Medicare Beneficiary Feedback (IPRO) Communication/Care Coordination • Option for short term rehab was never provided by hospital • Did not receive discharge planning while in hospital • Discharged from hospital with no instructions • Insurance pressure to discharge too soon • Did not involve caregiver in discharge plan • Cared for by many physicians in the hospital, none of which were the primary; gave conflicting information • Poor communication between providers, patient and caregiver • Sent home alone, was afraid did not know what to do Medicare Beneficiary Feedback Medication Reconciliation • Too many medications to track and manage • Medication not explained or did not understand • Primary care physician changed dosages after I purchased medications at discharge • Insurance plan did not allow medications prescribed at discharge • Did not know I was being discharged with new medications • Medication name was different on discharge summary that what pharmacy dispensed • Hospital gave prescription for same medication I was taking at home but with different name and I took both • Difficulty getting to pharmacy Medicare Beneficiary Feedback Follow-up Physician Visits • Realized that more questions should have been asked in hospital • Having to wait several weeks to get appointment • Did not have transportation to appointment • Difficulty getting a live person on the phone to schedule appointment with doctor • Confusion about which physicians to follow up with: primary or specialists or all Medicare Beneficiary Feedback Caregiver Perceptions • Lack of time for health workers to talk to patient and caregiver • Assumption that caregiver knows everything and has no questions • Assumption patient has caregiver at home who is able to provide needed care • Caregiver does not realize they are caregiver • Power of attorney not honored • Difficulty advocating for patient with Alzheimers Community Collaboration – Health and Aging Networks • Formalize Relationships in the community between health and aging networks • “Care Transitions” Coalition to Bring Together Hospitals, Health Providers and Aging Network • Problem solving to discuss difficult cases • Joint advocacy on health issues, i.e. observation status