Volume regulation: Blood pressure and the kidneys (Physiology)
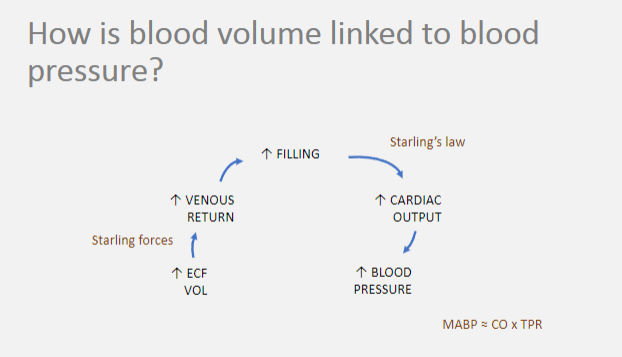
Session summary A major function of the kidney is volume regulation: regulation of the extracellular fluid volume, which includes the plasma volume, in order to maintain blood pressure. This is achieved by regulation of the amount of sodium retained in the body, since water follows sodium osmotically. This mechanism regulates blood volume (and hence pressure) over the long-term, in addition to the short-term, dynamic regulation by cardiovascular mechanisms. This lecture will integrate cardiovascular and renal physiology. To prepare, you should revise cardiovascular physiology, including the control of blood pressure, Starling's law and stroke volume, and capillary fluid exchange (Starling forces). Learning outcomes At the end of this session you will be able to: Describe the homeostatic mechanisms for maintaining sodium balance, including the factors controlling activation of RAAS Explain the relationship between total body sodium and extracellular fluid volume Explain the relationship between total body sodium and blood pressure Discuss situations in which impaired renal sodium excretion is linked to high blood pressure
-
What is osmoregulation? (1)
❀ Osmoregulation is the regulation of the amount of water in the body to maintain constant extracellular fluid (ECF) osmolarity.
-
What is volume regulation, and how is it achieved? (2)
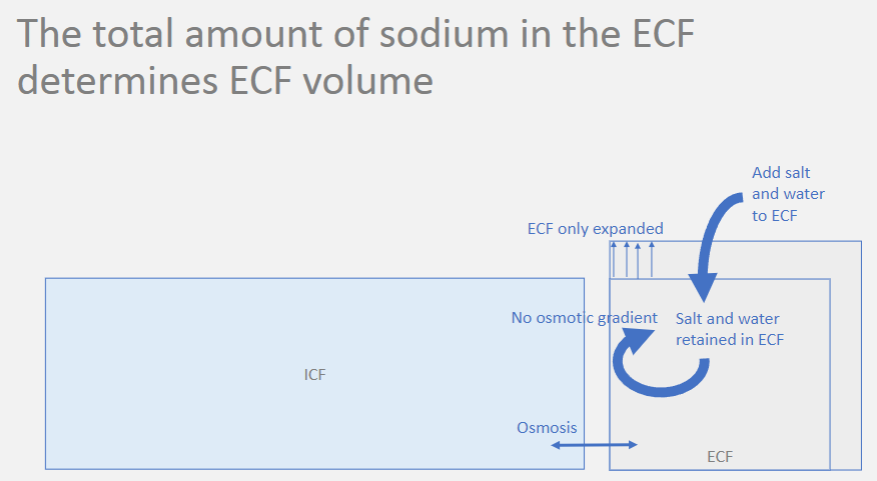
❀ Volume regulation involves regulating blood volume and pressure to ensure effective circulating volume.
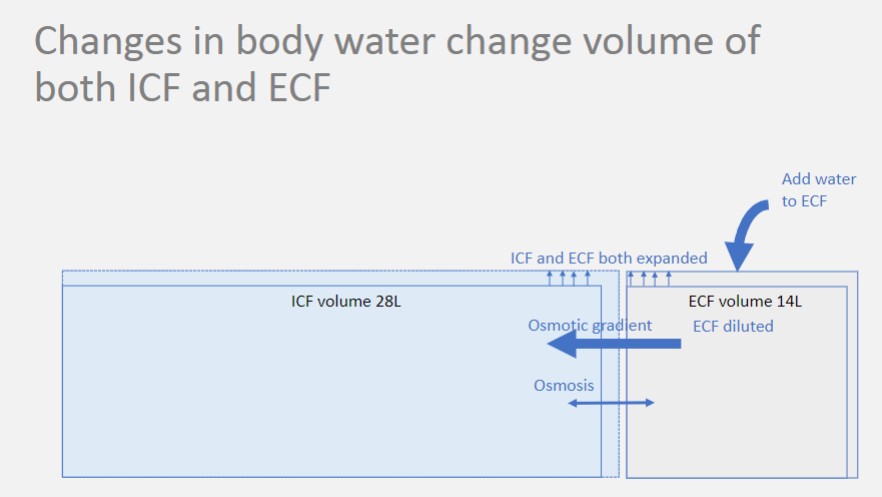
❀ This is accomplished by regulating the total amount (not concentration) of sodium in the extracellular fluid (ECF).
-
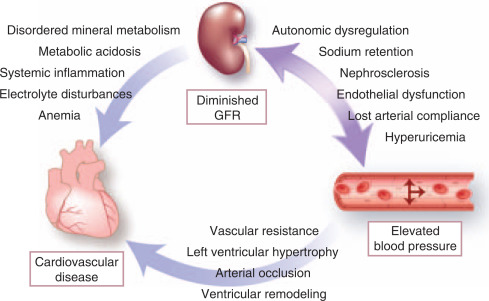
Picture demonstrating the changes in body water change (volume of both ICF and RCF):
-
Picture demonstrating the total amount of sodium in the ECF (determines ECF volume):
-
Picture demonstrating how blood volume is linked to blood pressure:
-
How is extracellular fluid (ECF) volume sensed? (1)
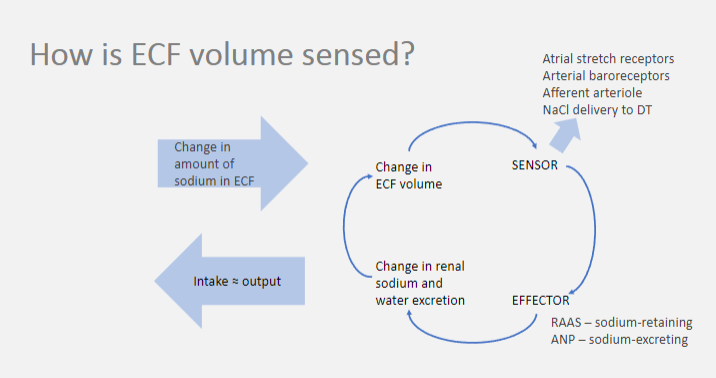
❀ Extracellular fluid volume is sensed through changes in renal sodium and water excretion.
-
What are the sensors and effectors involved in ECF volume regulation? (2)
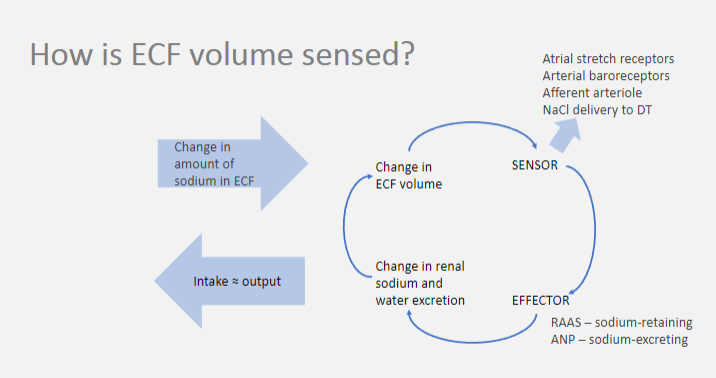
❀ Sensor: Atrial stretch receptors, arterial baroreceptors, afferent arteriole NaCl delivery to the distal tubule (DT).
❀ Effector: Renin-angiotensin-aldosterone system (RAAS) for sodium retention, atrial natriuretic peptide (ANP) for sodium excretion.
-
How does the body maintain balance between intake and output of sodium in the ECF? (1)
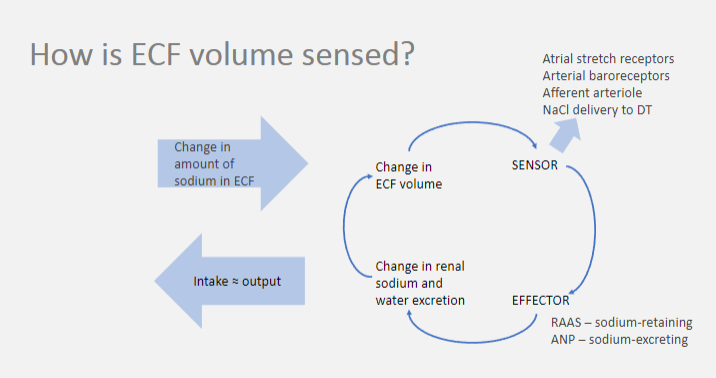
❀ The body maintains balance between intake and output of sodium in the extracellular fluid by ensuring that intake is approximately equal to output.
-
What are some mechanisms by which ECF volume is regulated? (2)
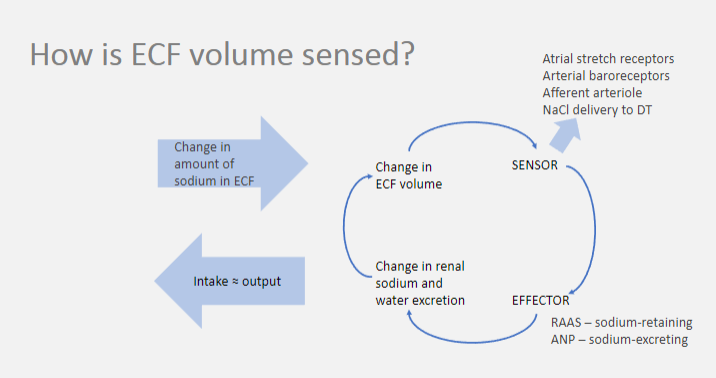
❀ Atrial stretch receptors, arterial baroreceptors, and afferent arteriole NaCl delivery to the distal tubule (DT) are involved in sensing changes in ECF volume.
❀ The renin-angiotensin-aldosterone system (RAAS) retains sodium, while atrial natriuretic peptide (ANP) promotes sodium excretion.
-
What activates the Renin-Angiotensin-Aldosterone System (RAAS)? (2)
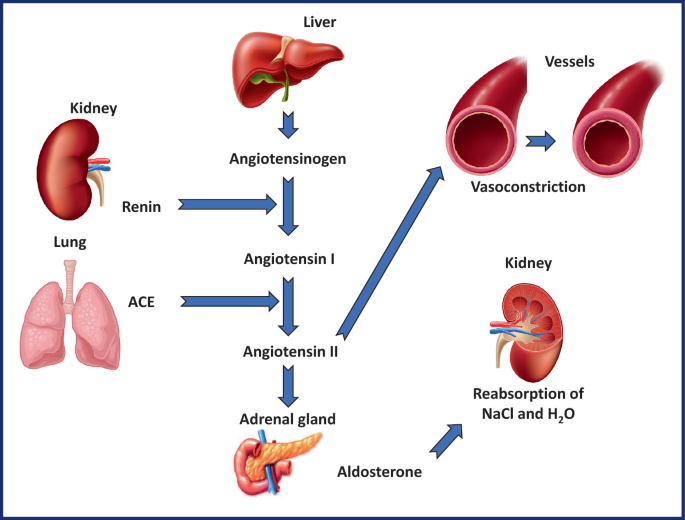
RAAS is activated by:
❀ Reduced renal perfusion
❀ Increased sympathetic activity Both are interpreted as a fall in blood volume.
-
How is aldosterone secretion increased? (2)
![Aldosterone secretion is increased by:❀ Activation of RAAS❀ Increased plasma potassium ([K+]) levels.](/flashcards/cardimage2/a566fce8/255/8255480_back.png)
Aldosterone secretion is increased by:
❀ Activation of RAAS
❀ Increased plasma potassium ([K+]) levels.
-
How is renal sodium excretion controlled? (2)
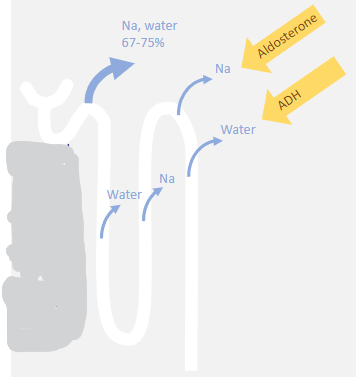
❀ Most of the filtered salt and water is reabsorbed in the proximal tubule (PT), with this fraction increasing with Renin-Angiotensin-Aldosterone System (RAAS) activity.
❀ A much smaller, variable fraction is reabsorbed from the distal tubule (DT) and collecting duct (CD).
-
What are the mechanisms of sodium reabsorption in the renal tubules? (3)
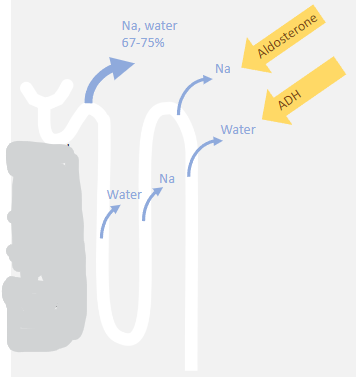
❀ Reabsorption of sodium and solute-free water are separated processes.
❀ Aldosterone-mediated sodium reabsorption increases plasma osmolarity, which is then adjusted by pure water reabsorption via the Antidiuretic Hormone (ADH) system.
❀ The result is increased sodium and water in extracellular fluid (ECF) with little or no change in plasma sodium concentration or osmolarity.
-
What is the effect of aldosterone on principal cells lining the collecting duct (CD)? (2)
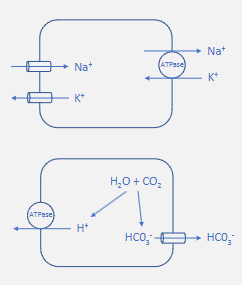
Aldosterone acts on principal cells lining the collecting duct by:
❀ Increasing Na/K ATPase activity.
❀ Increasing expression of ENaC channels on the luminal membrane.
This results in increased sodium reabsorption and increased potassium secretion.
-
How does aldosterone affect intercalated cells of the collecting duct? (2)
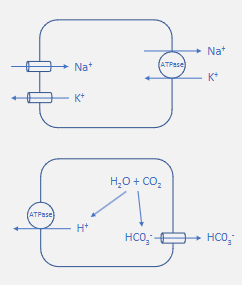
Aldosterone acts on intercalated cells of the collecting duct by:
❀ Increasing H+ ATPase activity.
This results in increased hydrogen ion secretion and increased bicarbonate reabsorption.
-

What are principal cells? (1)
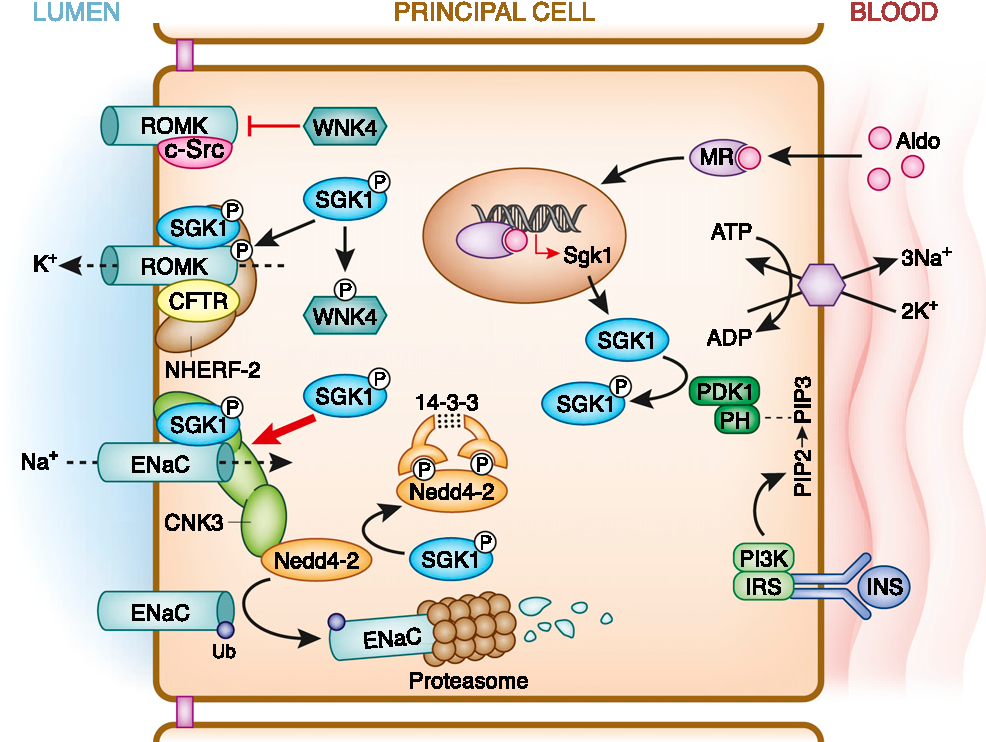
❀ Principal cells are specialized cells lining the renal tubules, particularly the collecting ducts, involved in electrolyte transport, particularly sodium and potassium.
-
What are intercalated cells? (1)
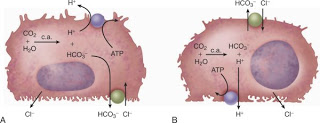
❀ Intercalated cells are specialized cells found in the renal tubules, particularly the collecting ducts, involved in acid-base regulation by secreting hydrogen ions (H+) and reabsorbing bicarbonate ions (HCO3-).
-
What does ENaC stand for? (1)
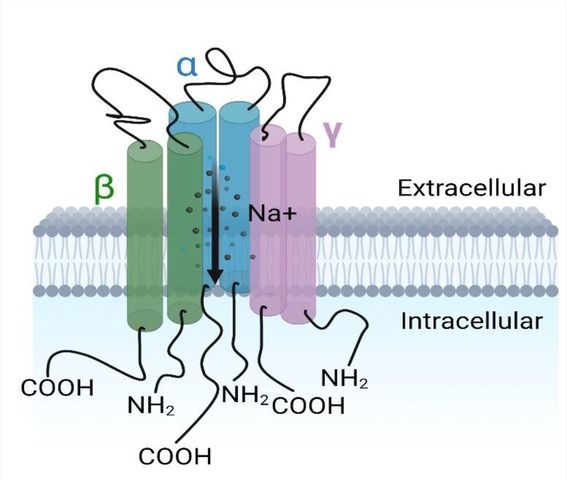
❀ ENaC stands for Epithelial Sodium Channel.
-
What is central to blood pressure homeostasis? (1)
❀ Regulation of the extracellular fluid volume (ECFV) is central to blood pressure homeostasis.
-
What is involved in the regulation of extracellular fluid volume (ECFV)? (1)
❀ Regulation of the ECFV involves control and adjustment of renal sodium excretion.
-
What is the central role of the kidney in blood pressure homeostasis? (1)
❀ The kidney plays a central role in blood pressure homeostasis by regulating extracellular fluid volume through control of renal sodium excretion.
-
What is pressure natriuresis? (1)
❀ Pressure natriuresis is a mechanism where, if blood pressure rises, renal artery pressure also increases, prompting the kidneys to respond by increasing sodium excretion, ultimately leading to a decrease in extracellular fluid volume (ECFV).
-
What is Conn's syndrome? (1)
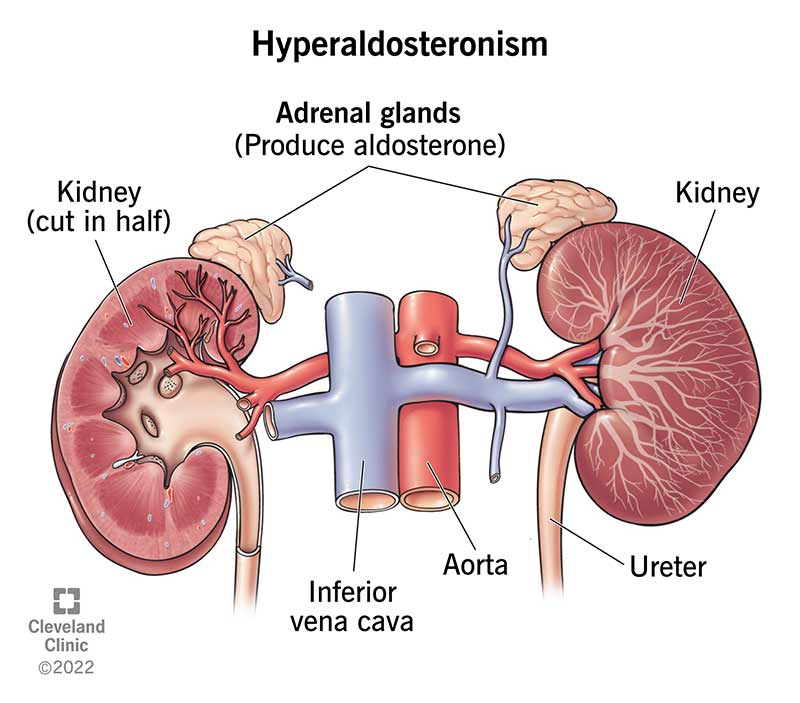
Conn's syndrome is:
❀ Primary hyperaldosteronism.
-
What are the typical causes of Conn's syndrome? (1)
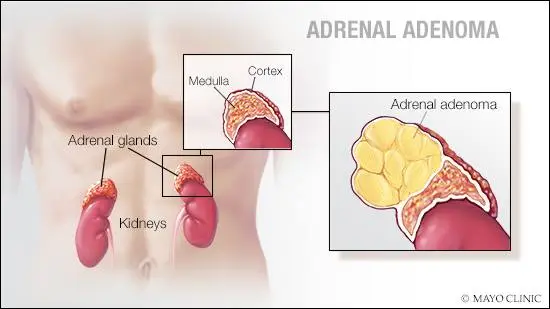
Conn's syndrome is often due to:
❀ Adenoma (tumour) of the adrenal cortex.
-
What are the effects of Conn's syndrome on renal sodium retention, extracellular fluid volume (ECFV), and blood pressure? (3)
Conn's syndrome leads to:
❀ Increased renal sodium retention.
❀ Increased reabsorption of water
❀ Increased extracellular fluid volume (ECFV).
❀ Increased blood pressure (BP).
-
What are the plasma potassium levels in Conn's syndrome? (1)
In Conn's syndrome, plasma potassium levels are:
❀ Decreased.
-
What are the levels of renin and aldosterone in Conn's syndrome? (2)
Conn's syndrome is associated with:
❀ Low renin levels.
❀ High aldosterone levels.
-
What defines hypertension? (1)
❀ Hypertension is present when systolic blood pressure is greater than 140 mmHg and/or diastolic blood pressure is greater than 90 mmHg.
-
How is hypertension classified? (2)
Hypertension is classified as:
❀ Secondary: when an identifiable cause is present, accounting for approximately 5-10% of cases.
❀ Essential: when the cause is unknown, representing over 90% of cases.
-

What is Liddle's syndrome characterized by? (1)
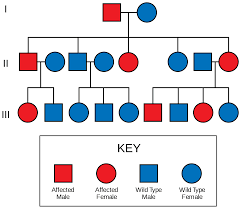
Liddle's syndrome is characterized by:
❀ A rare, genetic gain-of-function mutation in the epithelial sodium channel (ENaC).
-

What are the effects of Liddle's syndrome on renal sodium retention and blood pressure? (3)

Liddle's syndrome leads to:
❀ Increased renal sodium retention.
❀ Increased extracellular fluid volume (ECFV).
❀ Increased blood pressure (BP).
-

What are the levels of renin and aldosterone in Liddle's syndrome? (2)
Liddle's syndrome is associated with:
❀ Low renin levels.
❀ Low aldosterone levels.
-
What is renal artery stenosis? (1)
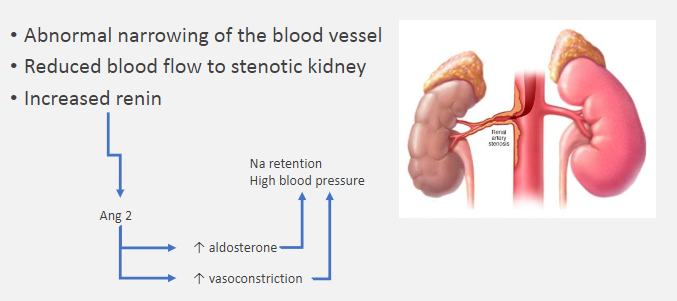
Renal artery stenosis is characterized by:
❀ Abnormal narrowing of the blood vessel supplying the kidney.
-
What are the consequences of renal artery stenosis? (1)
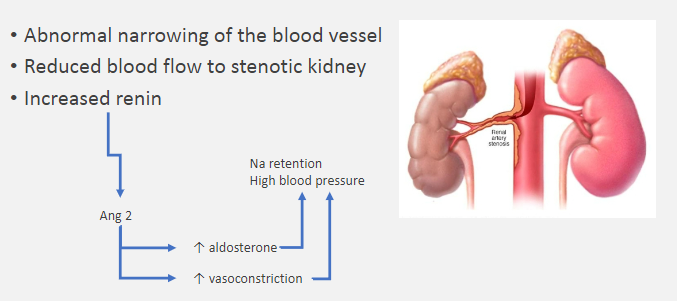
Renal artery stenosis leads to:
❀ Reduced blood flow to the stenotic kidney.
-
What is the hormonal response associated with renal artery stenosis? (1)
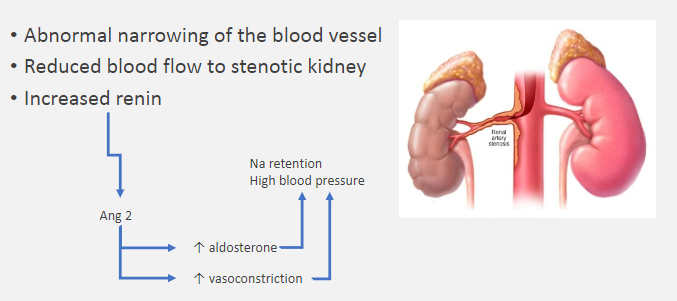
Renal artery stenosis results in:
❀ Increased renin production.
-
What characterizes Addison's disease and adrenal failure? (1)
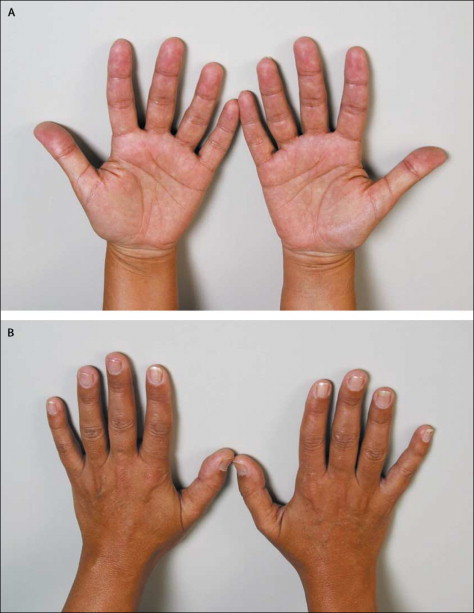
Addison's disease and adrenal failure involve:
❀ Progressive failure of the adrenal cortex, resulting in insufficient production of cortisol and aldosterone.
-
What are the consequences of untreated adrenal crisis in Addison's disease? (5)
Untreated adrenal crisis in Addison's disease can lead to:
❀ Lack of cortisol and aldosterone.
❀ Hypotension (low blood pressure).
❀ Hypovolemia (low blood volume).
❀ Hyperkalemia (high potassium levels).
❀ Hyponatremia (low sodium levels).

