Uterus, Uterine Tubes & the Cervix (Physiology 2)
Uterus, uterine tubes & cervix - Dr David Gillott Session introduction This lecture looks at the basic functional anatomy of uterus, uterine tubes and the cervix. The regulation and co-ordination of these by the menstrual cycle is explored. Investigations of tubal patency are described. Learning outcomes At the end of this lecture unit, you will be able to: Describe the functional anatomy of the uterus, tubes and cervix Understand the physiological changes in these structures during the menstrual cycle Explain the principles of testing for tubal patency Review the phases of the menstrual cycle
-
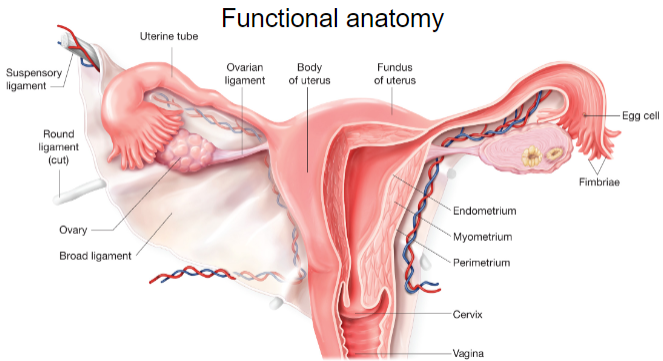
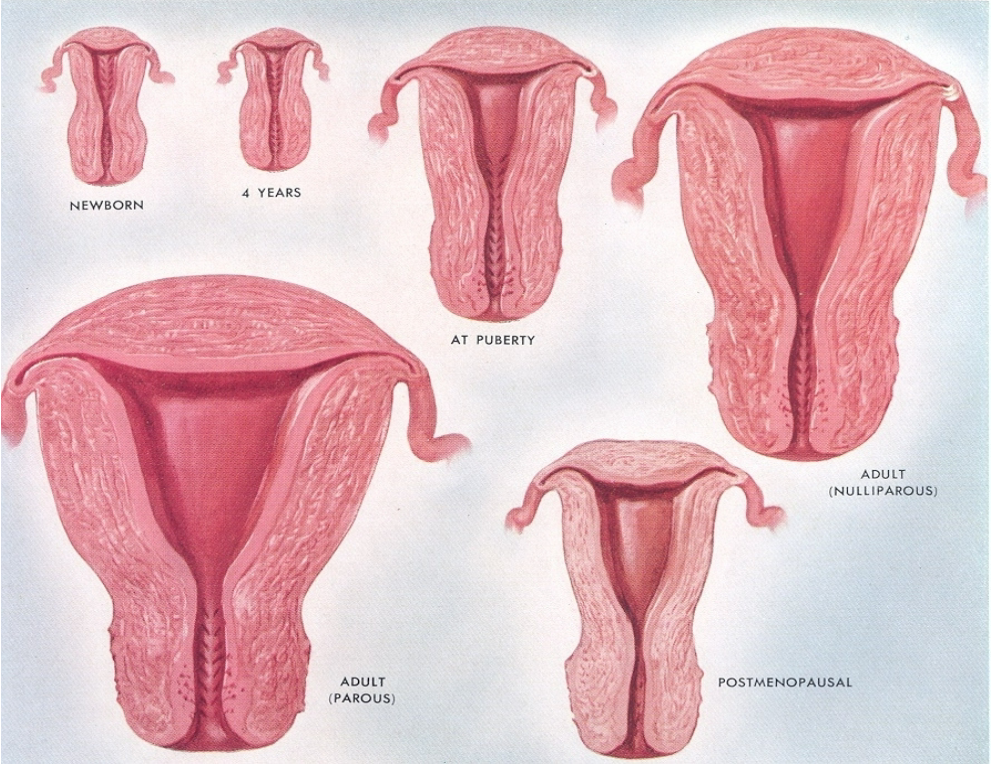
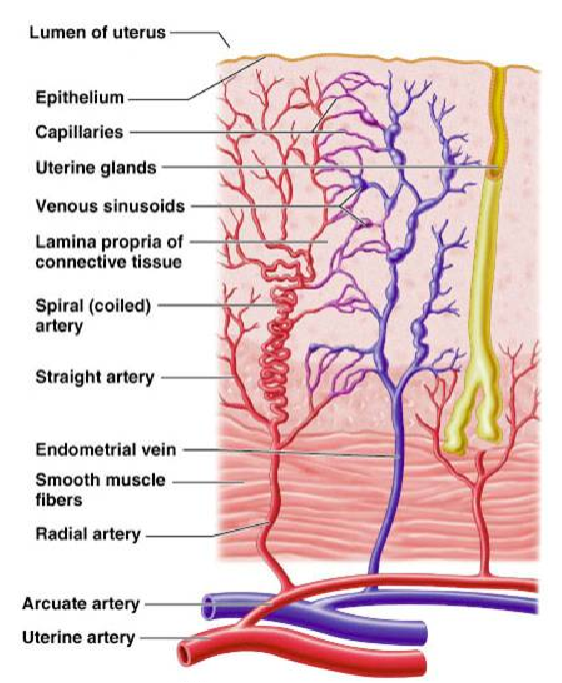
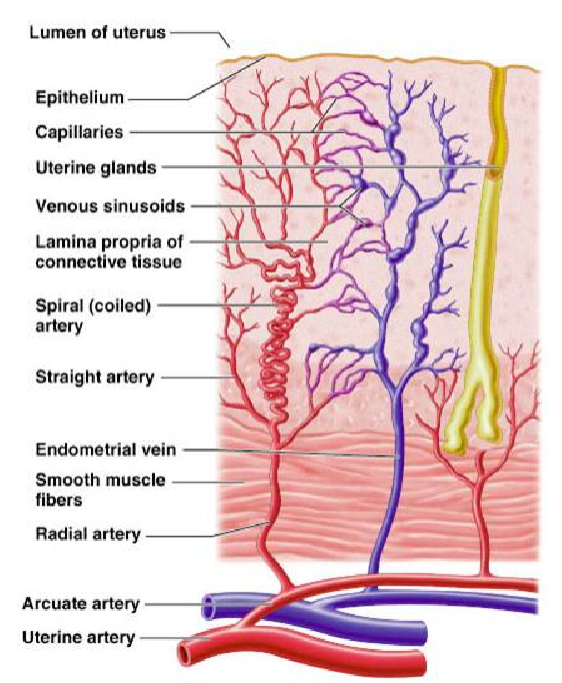
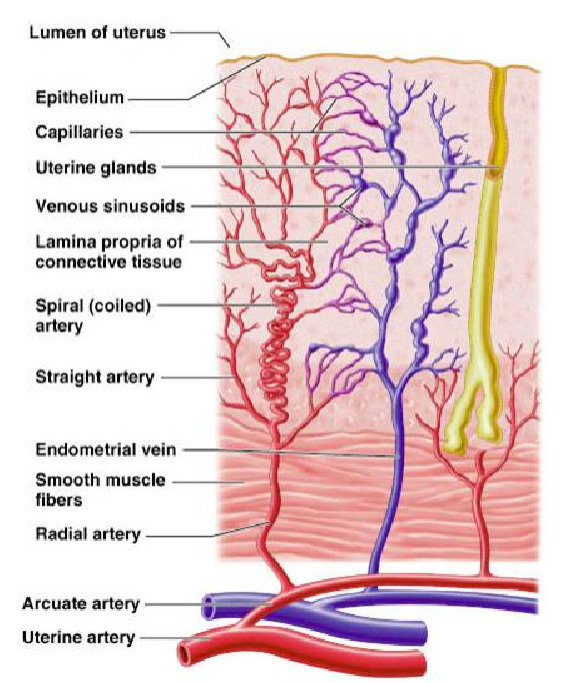
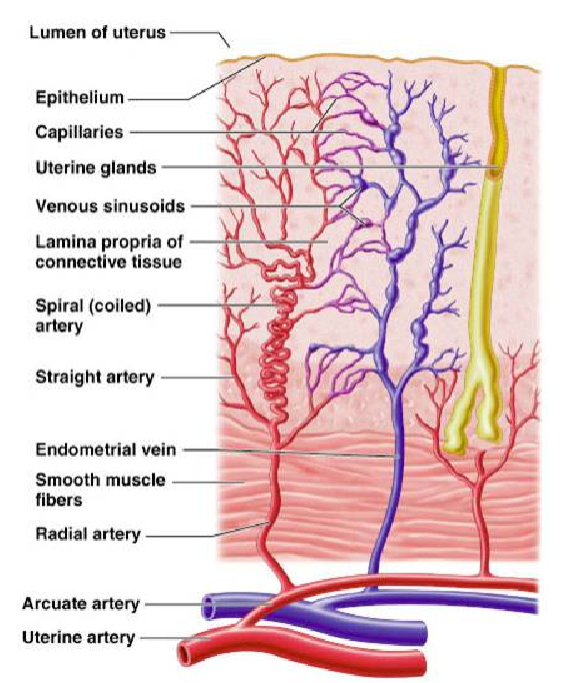
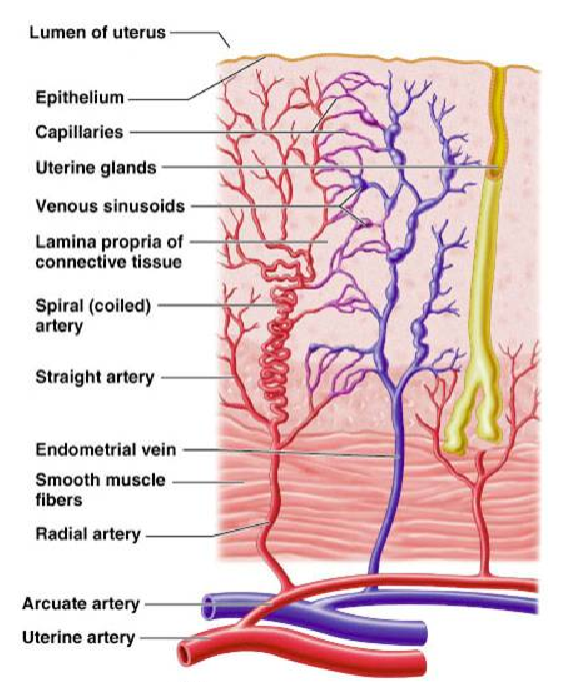
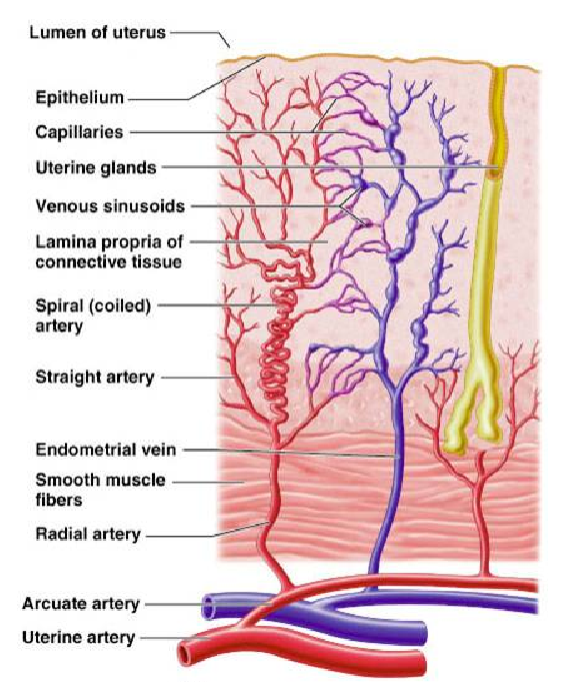
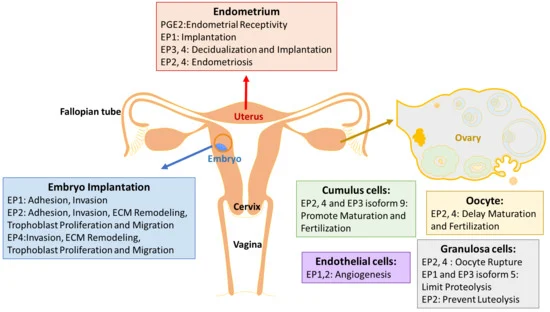
Picture demonstrating the functional anatomy of the female reproductive system:
-
How do maternal steroids influence the uterus in newborns? (2)
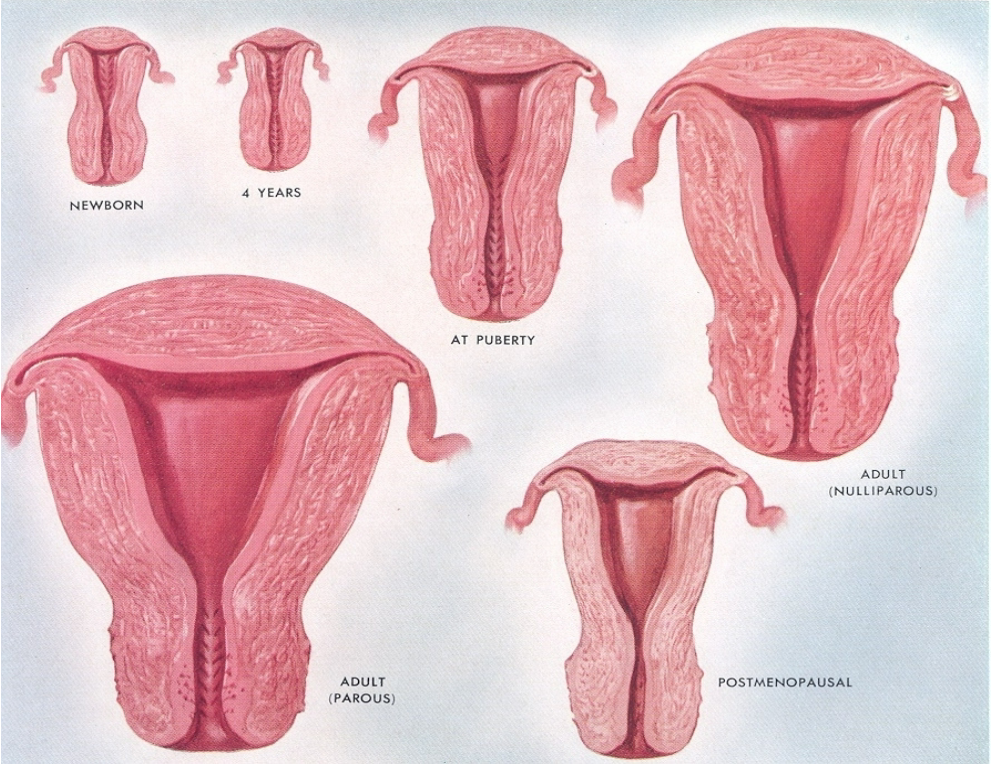
Maternal steroids increase the size of the newborn’s uterus.
This effect results from exposure to maternal hormones during fetal development.
-
How does the uterus change during infancy? (2)
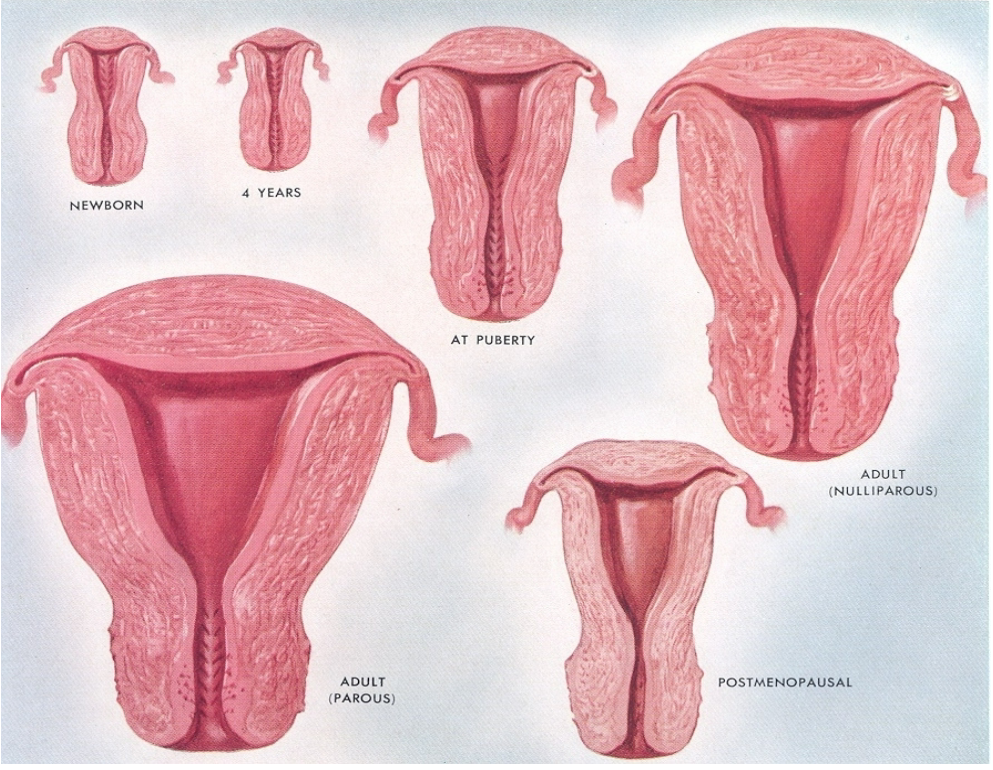
The uterus continues to grow in size along with the child’s height.
This growth reflects a gradual development that aligns with overall body growth during infancy.
-
What hormone influences the development of the myometrium, and how? (2)
Estradiol Dependency: The myometrium (muscle layer of the uterus) depends on estradiol for growth and development.
Estradiol stimulates cellular proliferation and growth within the myometrium.
-
How does the growth of the uterus corpus compare to the cervix? (2)
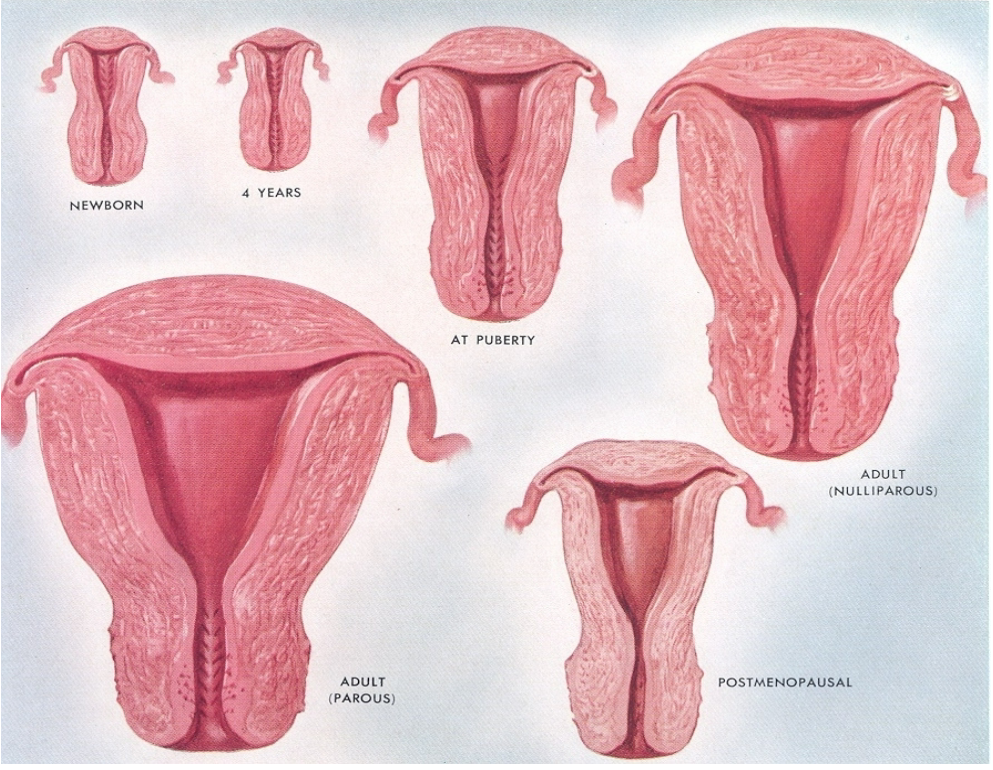
The corpus of the uterus undergoes a greater increase in size than the cervix.
This differential growth results in a larger and more developed uterine body compared to the cervical area.
-
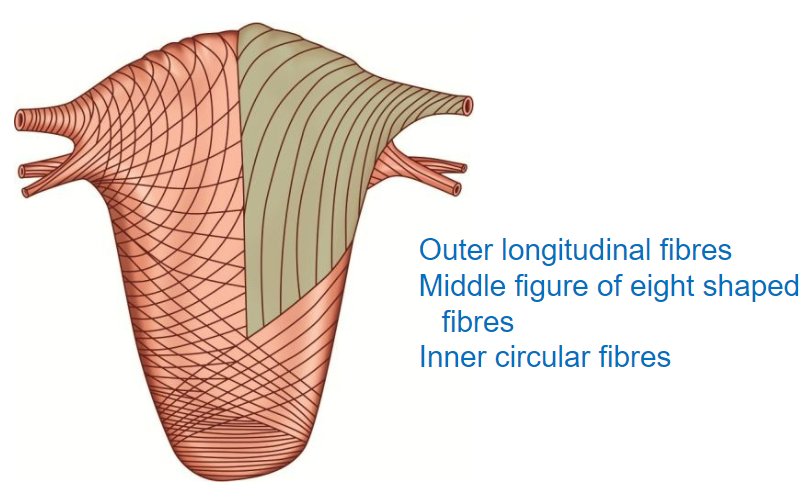
What is the myometrium, and how is it structured? (2)
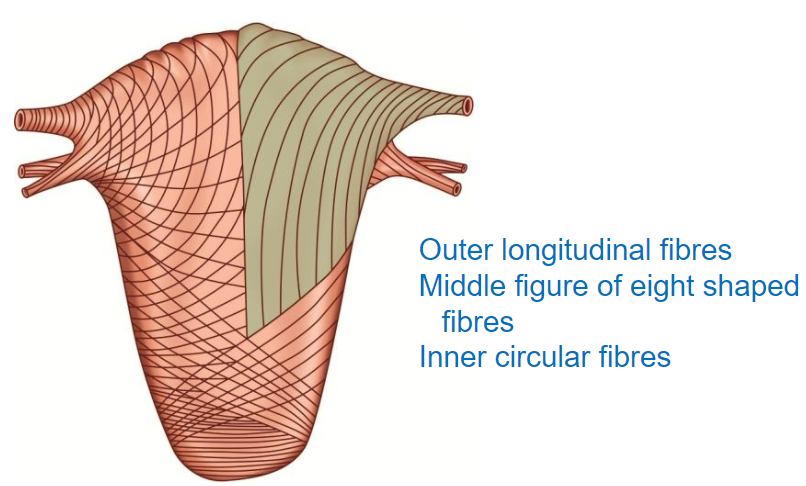
The myometrium is the muscular layer of the uterus, composed of three layers of smooth muscle.
These layers are organized to facilitate contraction, increasing uterine pressure to direct contents toward the cervix.
-
What function does the myometrium serve in relation to blood loss? (2)
The myometrium acts as a natural ligature, helping to prevent blood loss.
Its contraction compresses blood vessels within the uterine wall, reducing bleeding risk.
-
What are the three layers of the myometrium, and how are they arranged? (3)
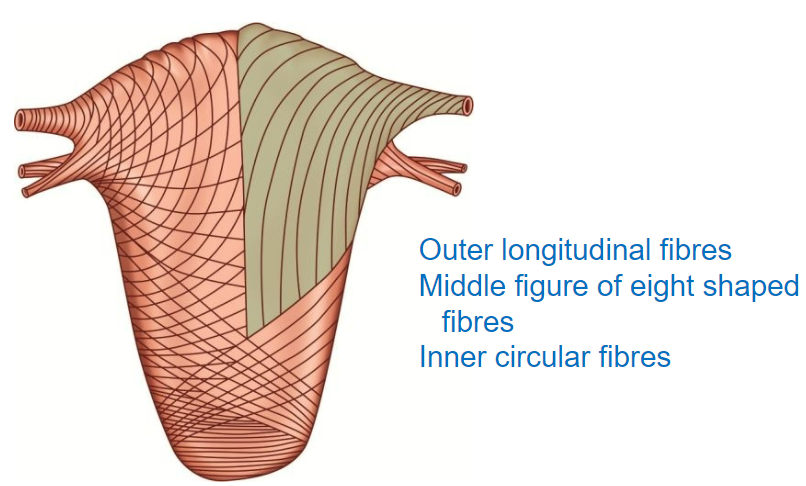
Outer Layer: Longitudinal fibers that run along the length of the uterus.
Middle Layer: Figure-of-eight shaped fibers, aiding in effective contraction.
Inner Layer: Circular fibers, providing structural integrity and assisting with contraction.
-
What layers surround the myometrium? (2)
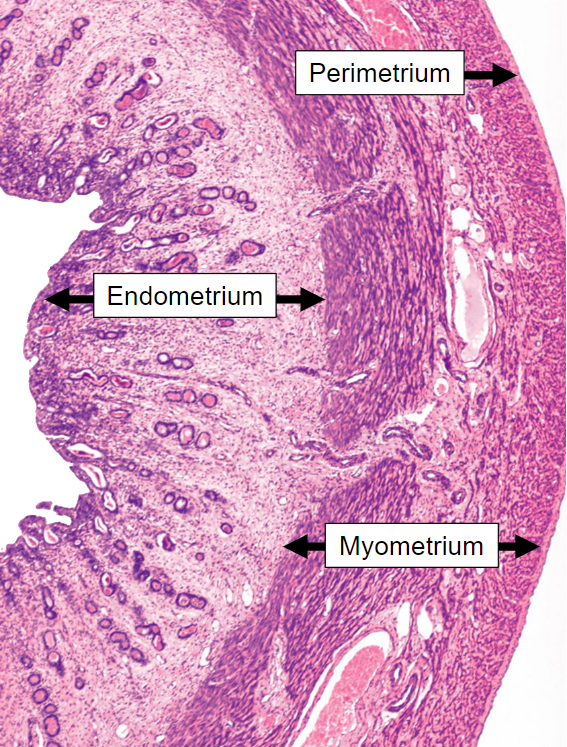
Perimetrium: The outermost layer of the uterus.
Endometrium: The innermost layer, lining the uterine cavity.
-
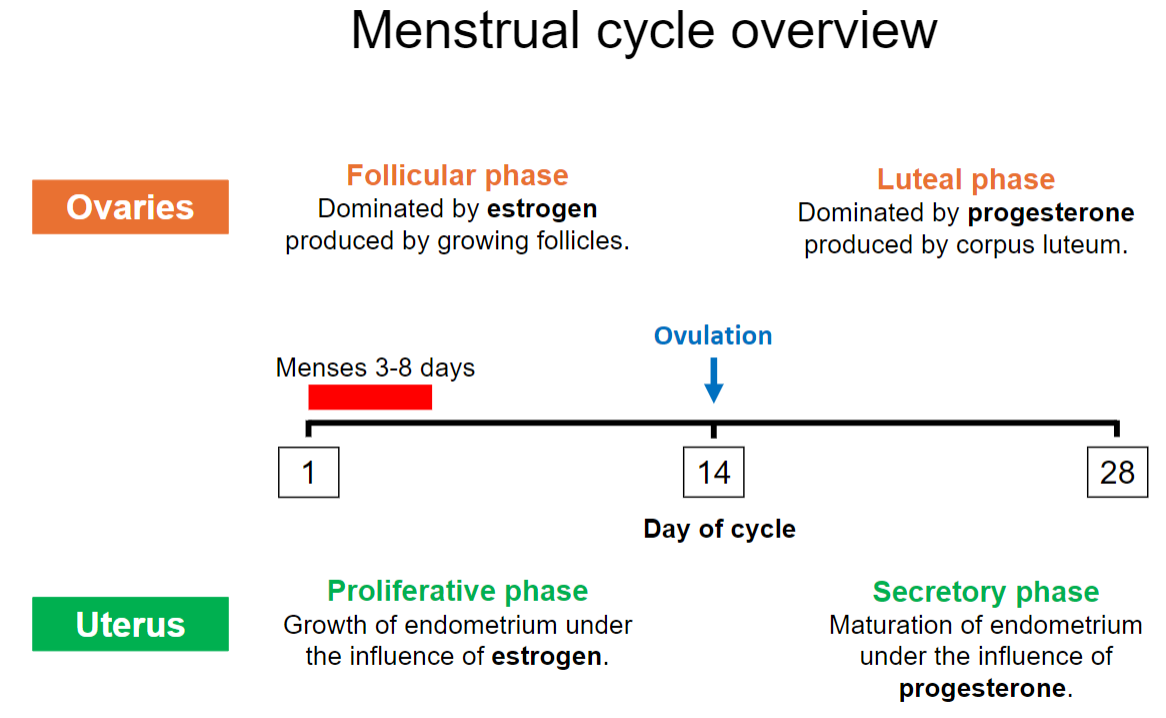
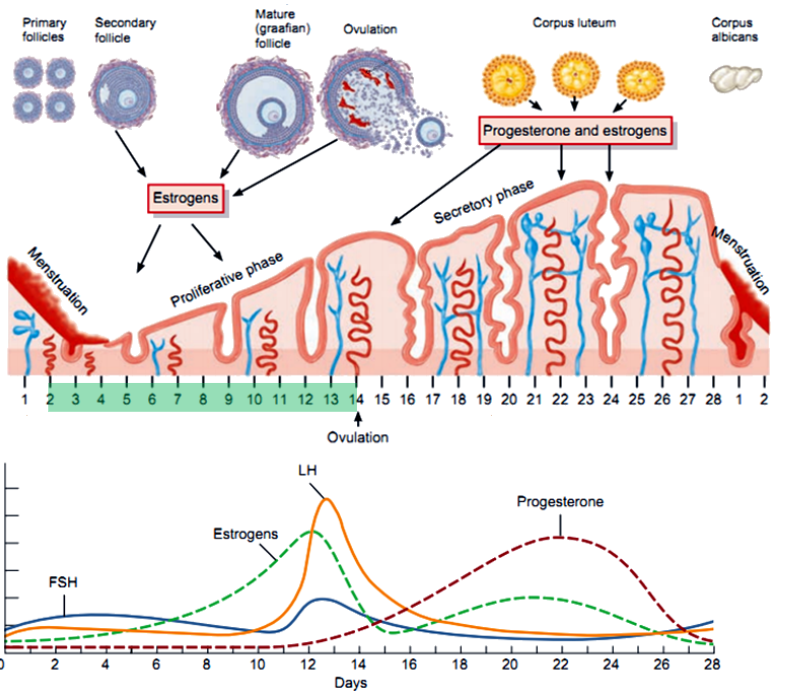
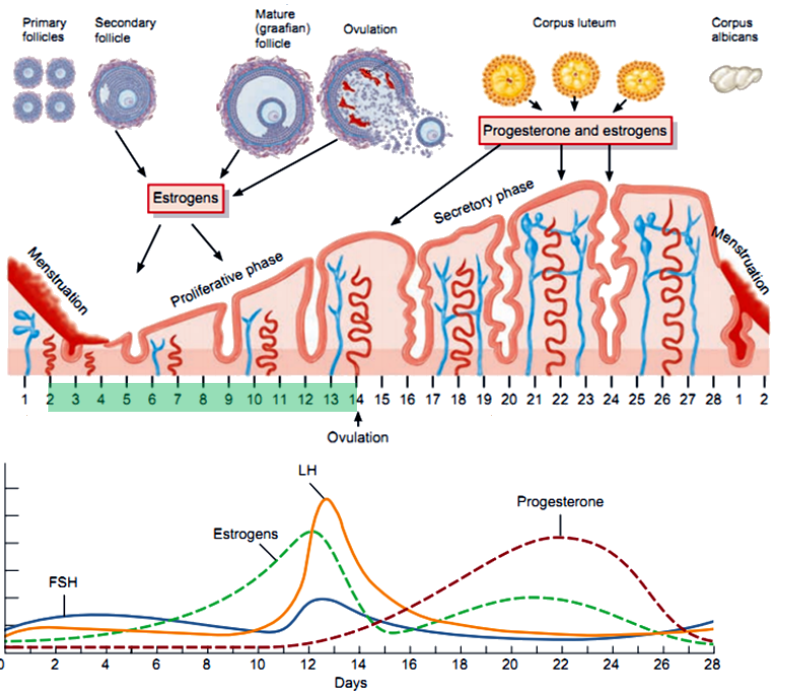
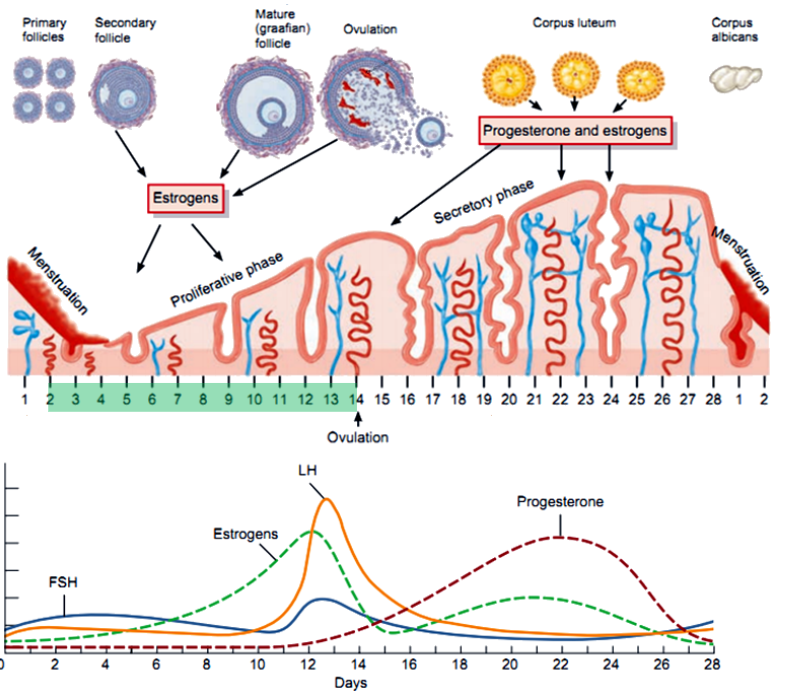
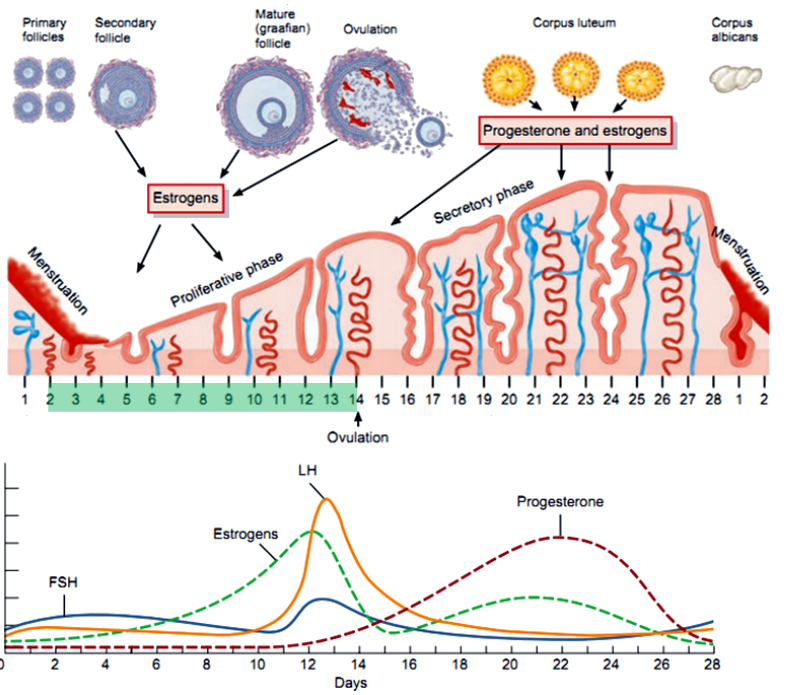
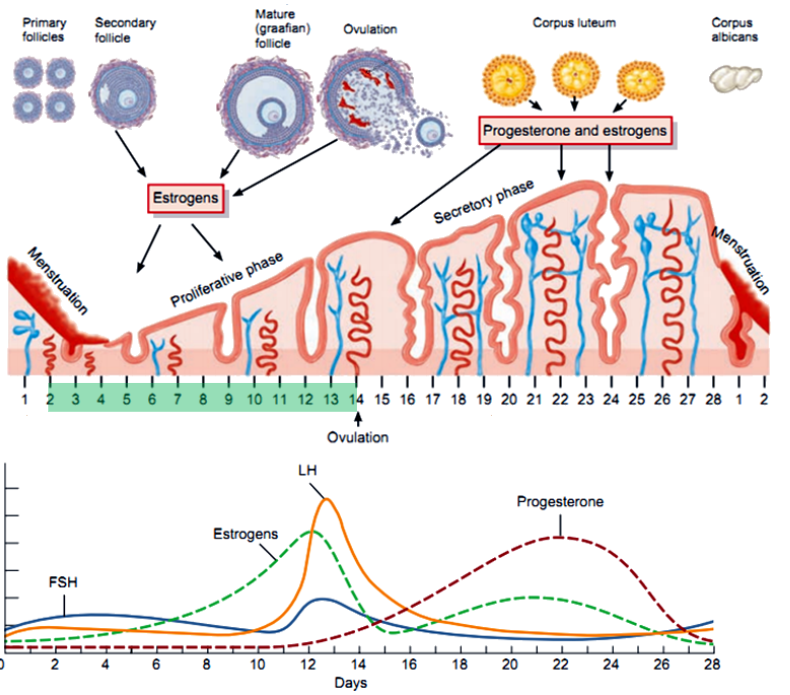
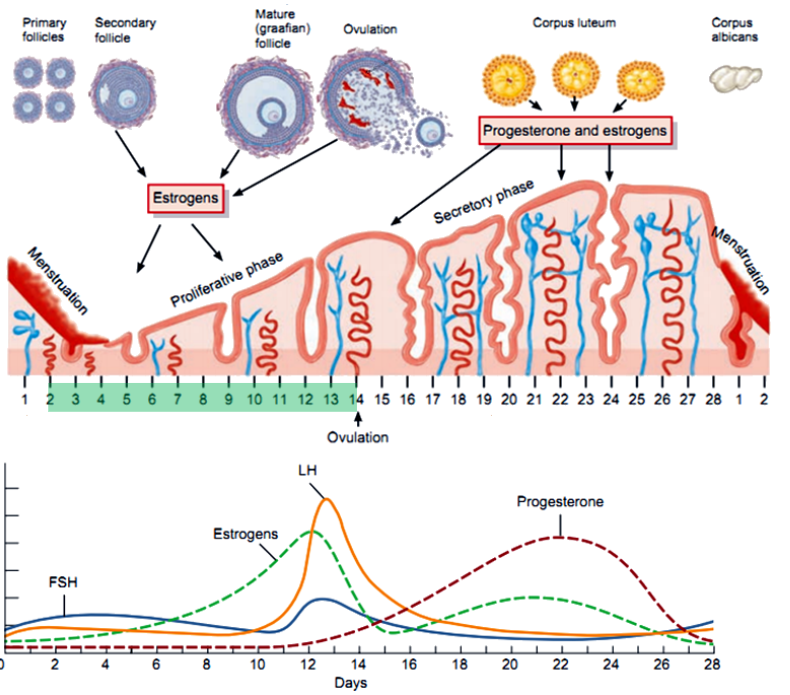
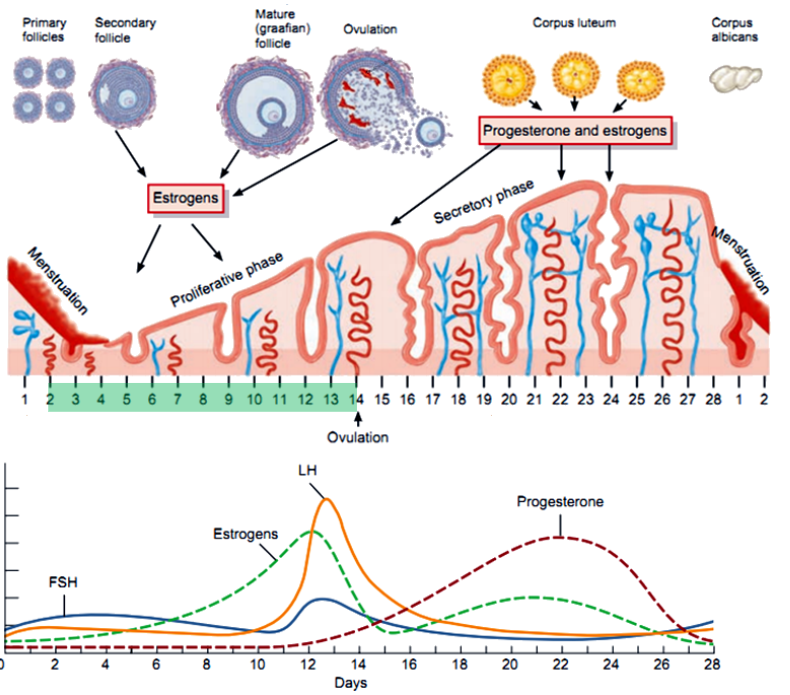
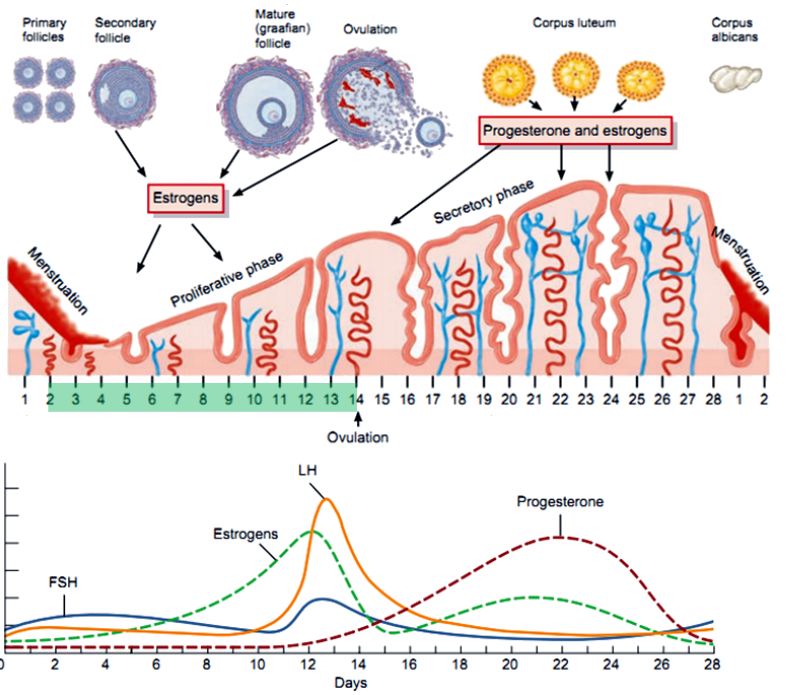
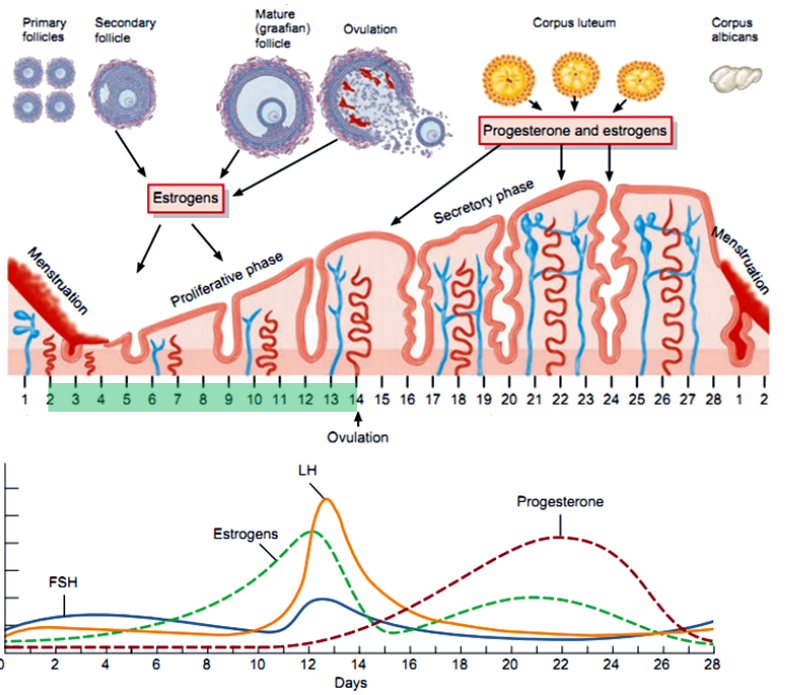
What are the main phases of the menstrual cycle, and what days do they typically occur on? (3)
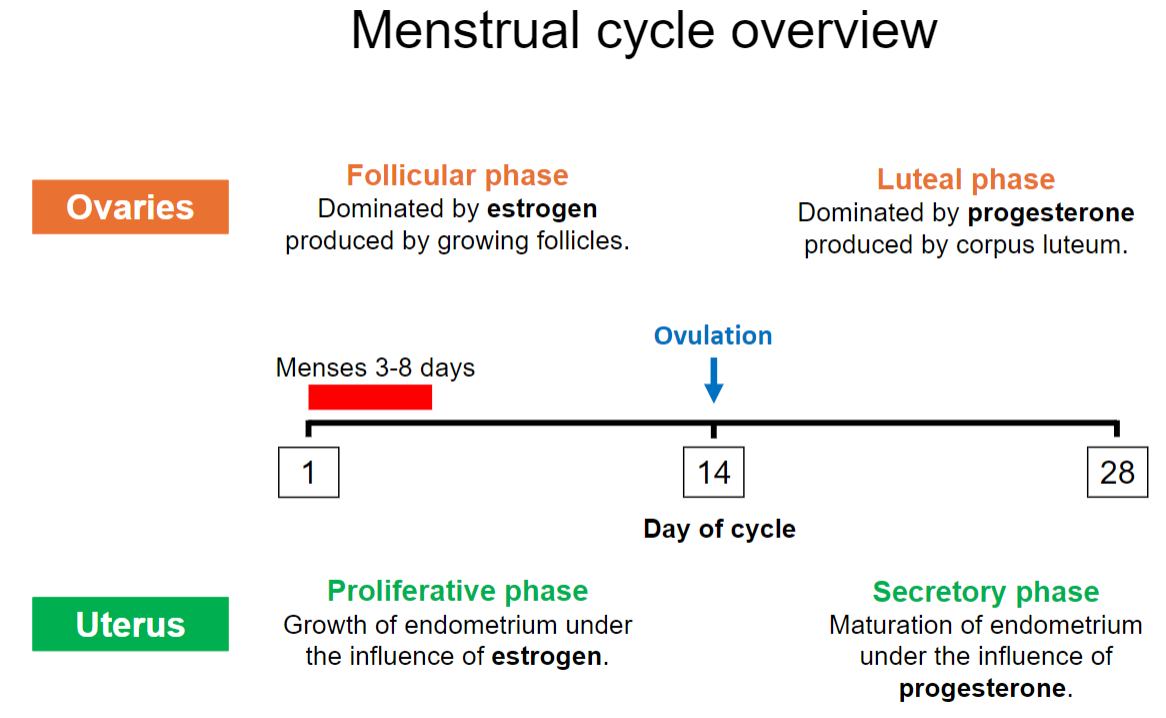
Follicular Phase: Begins on day 1, dominated by estrogen.
Ovulation: Around day 14.
Luteal Phase: Days 15-28, dominated by progesterone.
-
What occurs during the follicular phase in terms of hormone production? (6)
FSH Stimulates Follicle Growth: FSH promotes the growth and development of follicles in the ovary.
Estrogen Production Begins: Granulosa cells produce estrogen by converting androgens from the theca cells using the enzyme aromatase.
Two-Cell, Two-Gonadotropin Interaction: LH stimulates theca cells to produce androgens, while FSH stimulates granulosa cells to convert these androgens into estrogen.
Rising Estrogen Levels: Estrogen increases as the dominant follicle grows, exerting negative feedback on FSH and LH secretion initially.
Estrogen Positive Feedback: Toward the end of the phase, high estrogen levels trigger a positive feedback loop, causing the LH surge.
Low Progesterone: Progesterone levels remain low as the corpus luteum has not yet formed.
-
What is the role of the proliferative phase in the menstrual cycle? (2)
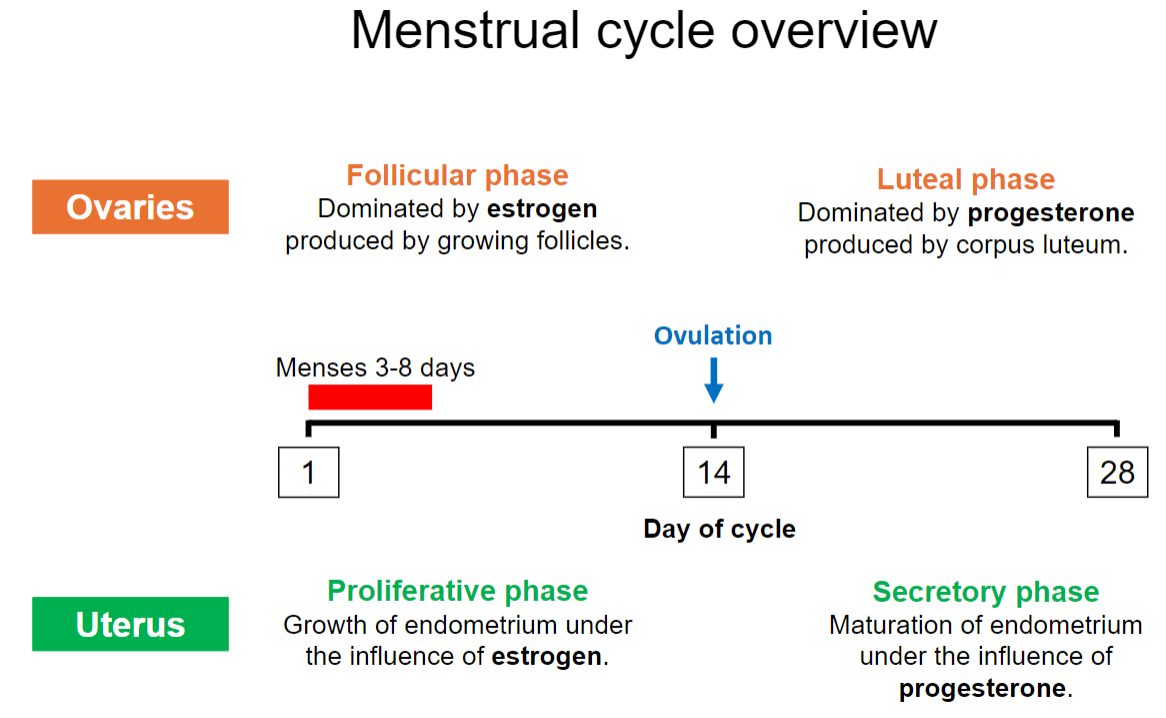
The endometrium grows and thickens under the influence of estrogen.
Prepares the uterus for potential implantation.
-
What hormone dominates the luteal phase, and what structure produces it? (2)
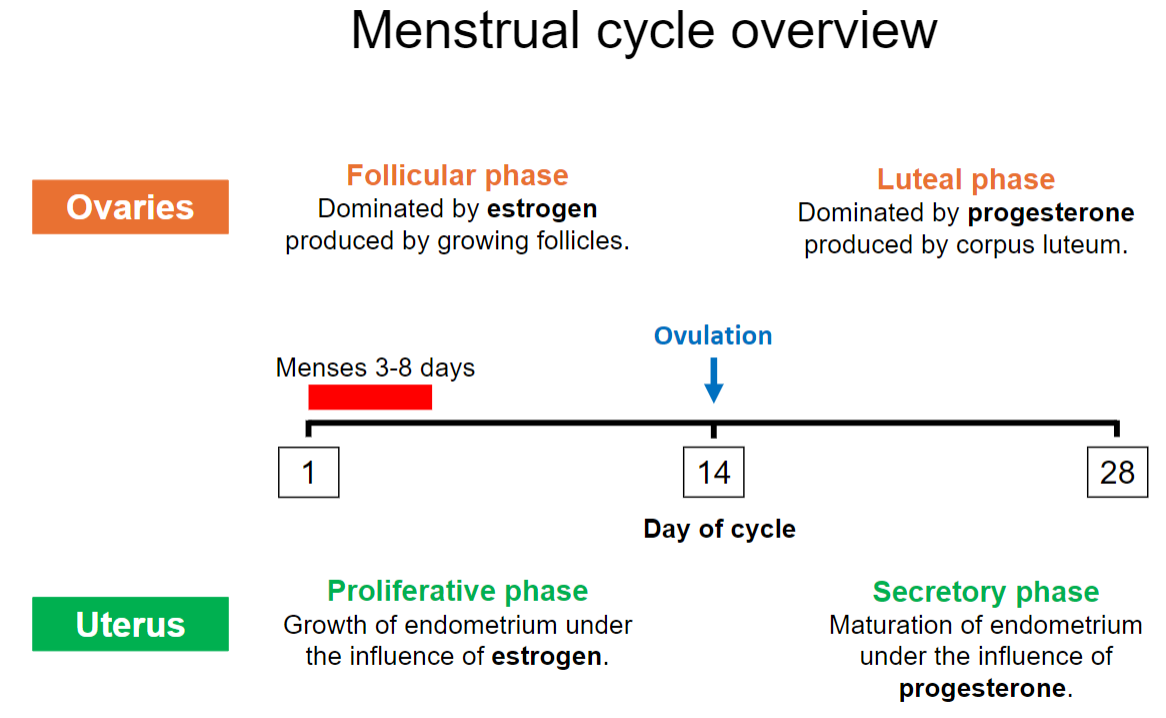
Progesterone is the dominant hormone in the luteal phase.
It is produced by the corpus luteum.
-
What is the secretory phase, and what influences it? (2)
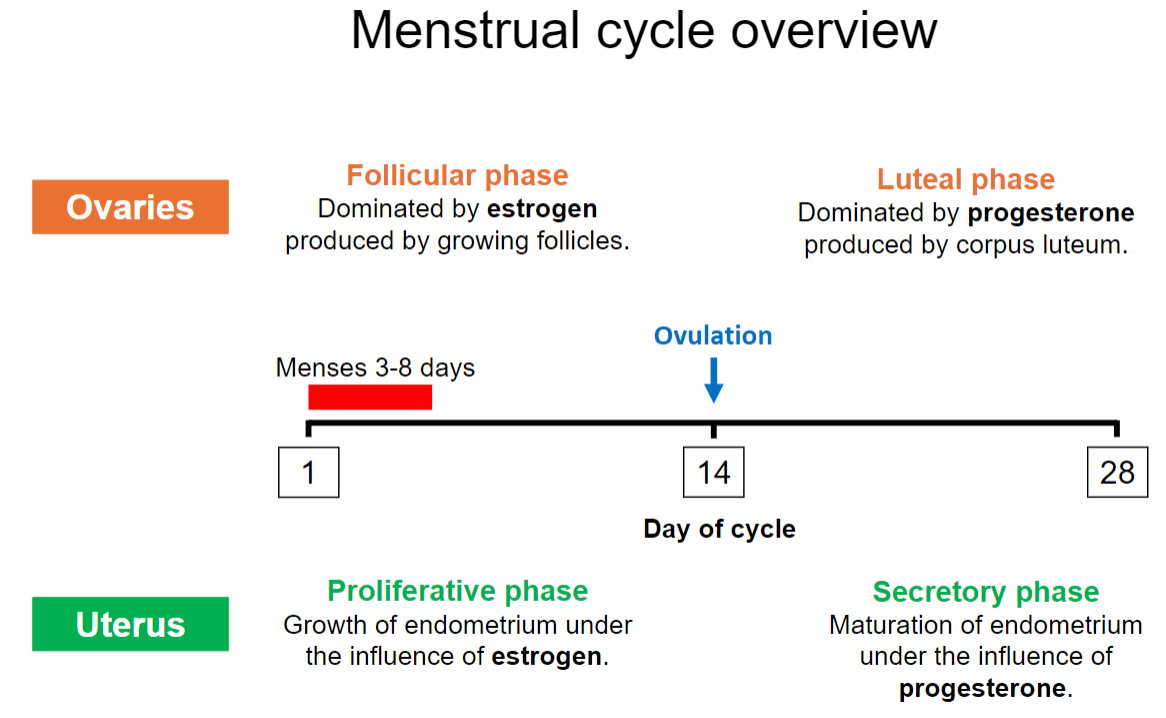
The endometrium matures to prepare for potential embryo implantation.
This phase is influenced by progesterone.
-
How long does the menstrual phase (menses) typically last? (1)
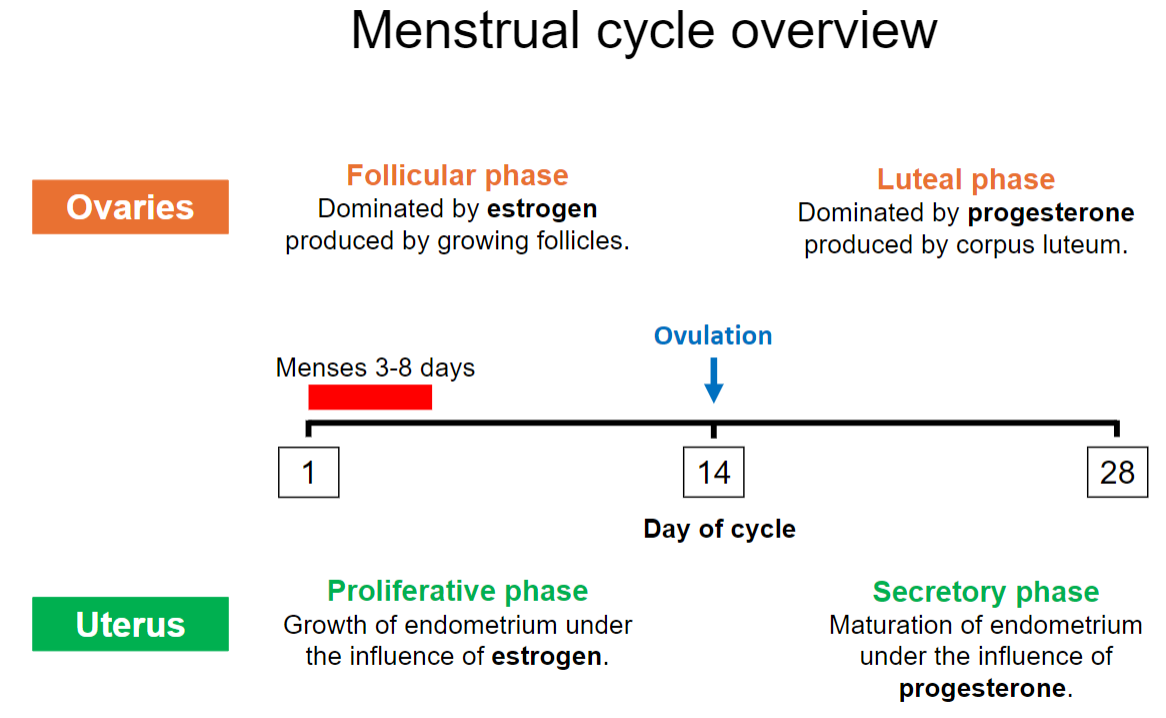
The menstrual phase typically lasts 3-8 days.
-
How does the endometrium respond cyclically to steroid hormones? (2)
Dependent on estrogen and progesterone levels.
Undergoes cyclic changes in response to these hormones.
-
What effect does estrogen have on the endometrium during the proliferative phase? (1)
Estrogen stimulates growth of the endometrium.
-
How thick can the endometrium typically appear on an ultrasound during the secretory phase? (1)
Between 7-16 mm.
-
What role does progesterone play in the endometrium during the secretory phase? (2)
Progesterone transforms the endometrium from a growing (proliferative) state to a functional state by causing the cells to specialize (differentiate).
It prevents further thickening of the endometrium by stopping estrogen-driven growth.
-
What happens to the endometrium at menstruation? (1)
Most of the endometrium is lost due to a drop in progesterone as the corpus luteum degenerates.
-
What remains of the endometrium after menstruation? (2)
A 2-3 mm thick stromal matrix.
Contains small columnar cells and straight glandular extensions
-
What hormone stimulates the growth of the endometrium in the proliferative phase? (1)
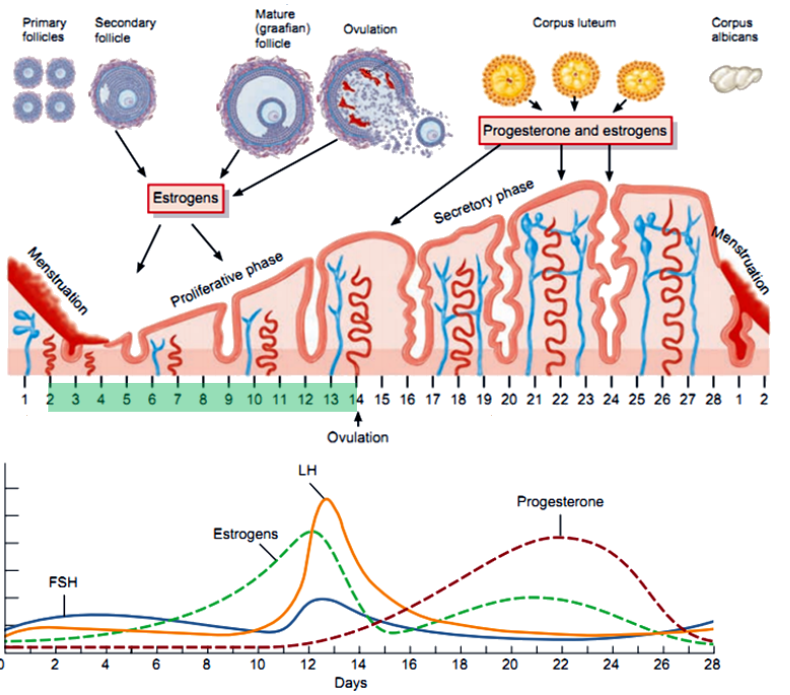
Estrogen from the growing follicle.
-
What key features mark the proliferative phase in the endometrium? (3)
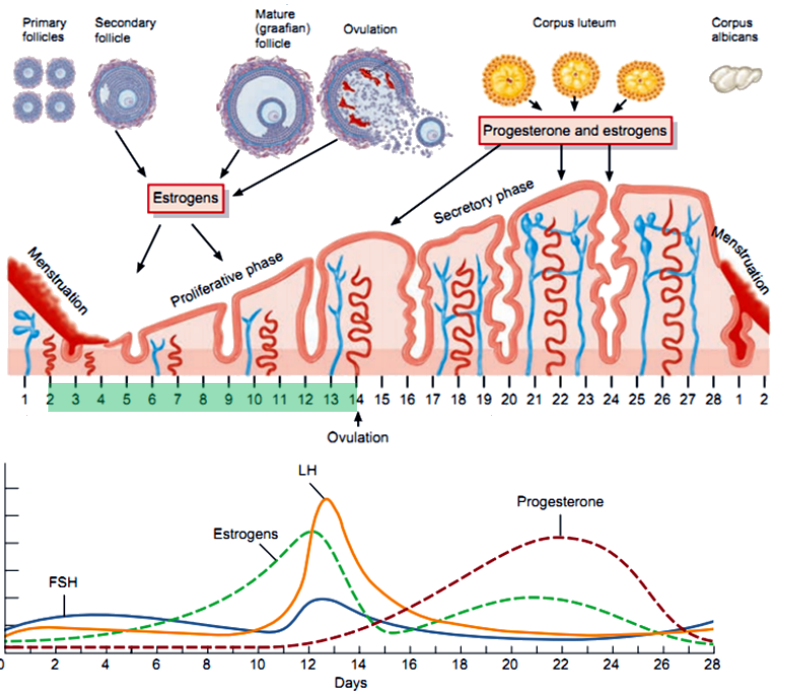
Stromal cell division (stroma is the connective tissue that supports the endometrial glands and vessels).
Ciliated surface formation (ciliated cells help move the fertilized egg towards the uterus after fertilization by the sperm).
Glands expand and become tortuous (twisted to increase surface area).
-
What changes in vascularity occur during the proliferative phase? (2)
Increased vascularity.
Neoangiogenesis peaks with maximal cell division by days 12-14.
-
When Are Progesterone Receptors Induced, and What Other Event Occurs? (2)
Progesterone receptors are induced in the endometrium when its thickness exceeds 4 mm, typically during the proliferative phase (mid-cycle).
This is accompanied by small muscular contractions of the myometrium, which help improve blood flow to the endometrium and assist sperm transport through the uterus toward the uterine tubes.
-
When does the endometrial secretory phase begin, and what hormone influences it? (2)
Begins 2-3 days after ovulation.
Gradual rise in progesterone reduces cell division.
-
What changes occur in the glands during the secretory phase? (2)
Endometrial glands become more twisted and enlarged (increase in tortuosity and distension).
They start secreting glycoproteins and lipids to nourish a potential embryo.
-
What are the effects of oedema and vascular changes in the secretory phase? (3)
Increased vascular permeability.
Arterioles contract and grow tightly wound, increasing surface area.
Enhanced blood supply.
-
How does the myometrium respond during the secretory phase? (2)
The myometrial smooth muscle cells enlarge, and uterine contractions are suppressed (to prevent disruption to the developing endometrium).
Blood supply to the myometrium increases to support the endometrial changes.
-
What happens to the corpus luteum (CL) if fertilization does not occur? (2)
The CL has a lifespan of 14 days and then regresses.
This regression leads to a fall in progesterone levels, causing the endometrium to be lost (menses).
-
How does the regression of the corpus luteum affect FSH levels? (2)
The drop in progesterone removes its negative feedback on the pituitary gland.
This allows an inter-cycle rise in FSH, preparing for a new cycle.
-
How is the corpus luteum maintained during pregnancy? (2)
hCG from the embryo binds to the LH receptors on the CL.
This "rescues" the CL, allowing it to continue producing progesterone and maintain the endometrium.
-
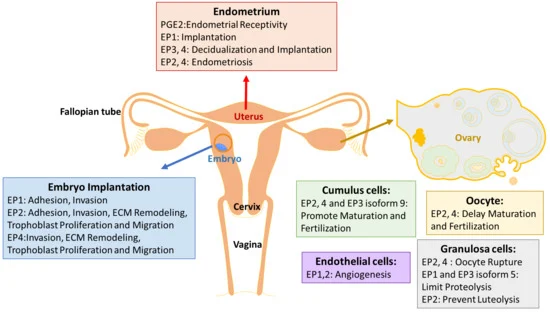
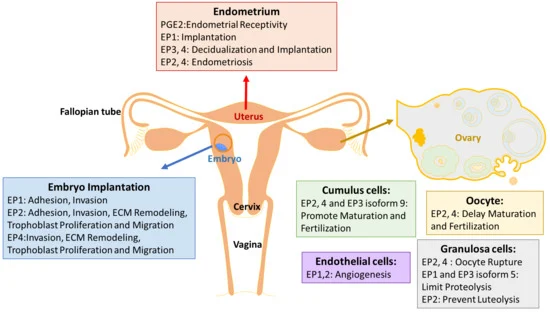
What triggers the start of menstruation? (2)
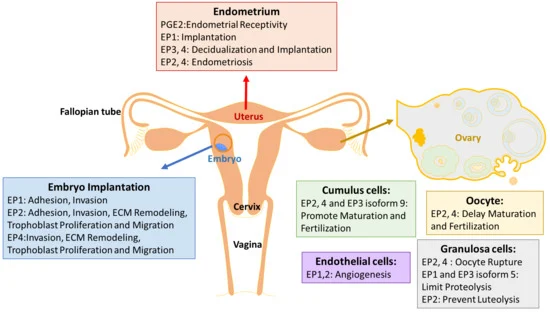
A decline in progesterone levels causes endometrial cells to secrete prostaglandins (PGF2α & PGE2).
These prostaglandins cause blood vessel constriction in the endometrium, leading to ischaemia and necrosis.
-
What happens to blood vessels and tissue during menstruation? (3)
Proteolytic enzymes are released from dying tissue, breaking down cells.
Blood vessels dilate, leading to bleeding as the outer endometrial layer is shed.
Approximately 50% of the endometrium is lost within 24 hours, with up to 80ml blood loss considered normal.
-
How long does menstrual bleeding typically last, and what causes menstrual cramps? (2)
Menstrual bleeding normally lasts for 4 or more days.
Prostaglandins induce uterine muscle contractions, which help shed the endometrial lining and cause menstrual cramps.
-
What role does the basal layer of the endometrium play post-menstruation? (2)
The basal layer remains intact after the outer endometrium is shed.
Estrogen from the next follicular phase stimulates endometrial proliferation, beginning the cycle anew.
-
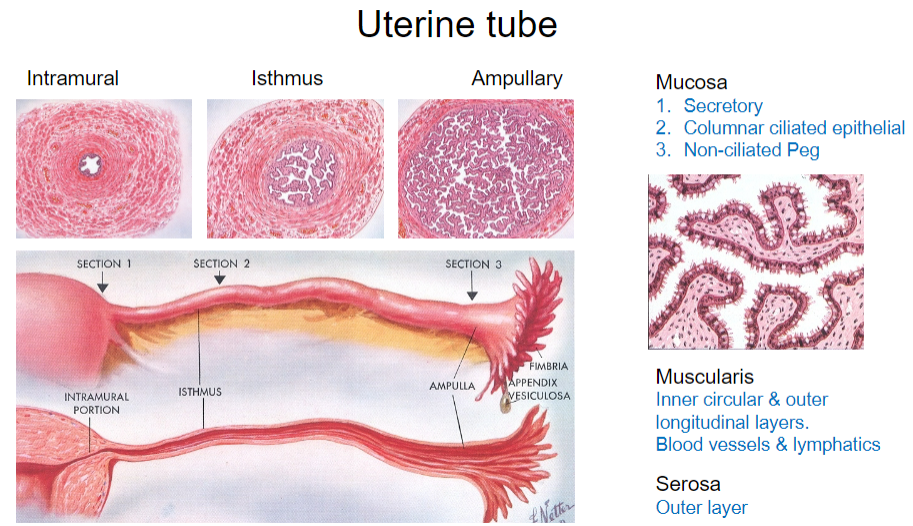
What are the parts of the uterine tube? (4)
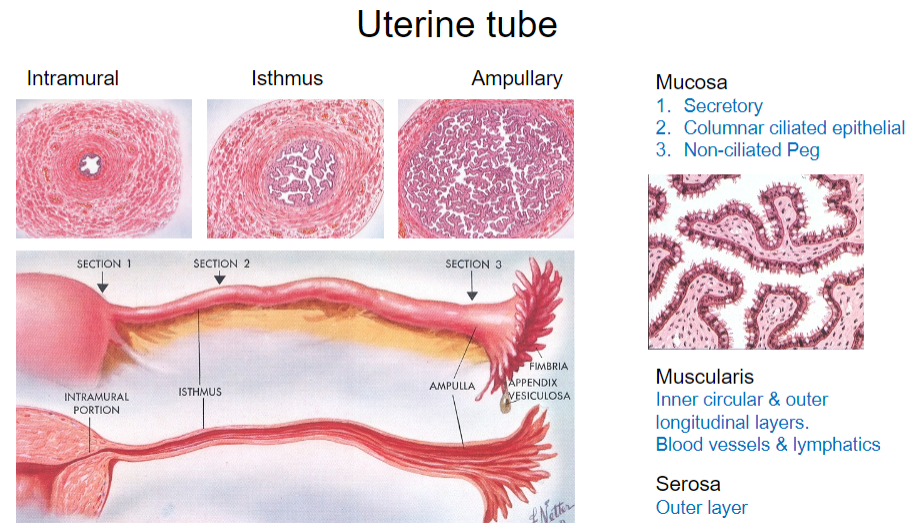
Intramural
Isthmus
Ampullary
Mucosa
-
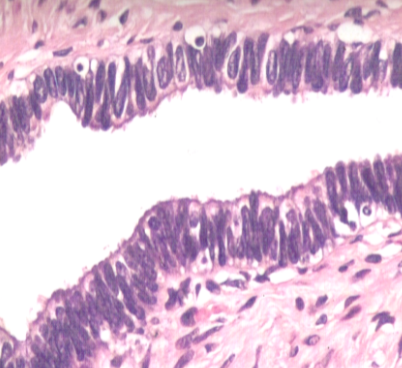
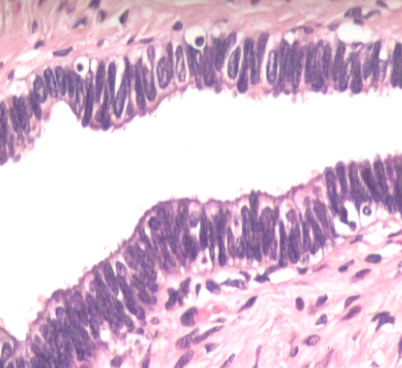
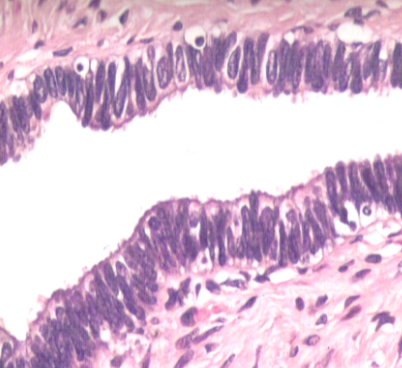
What are the types of epithelial cells found in the mucosa of the uterine tube? (3)
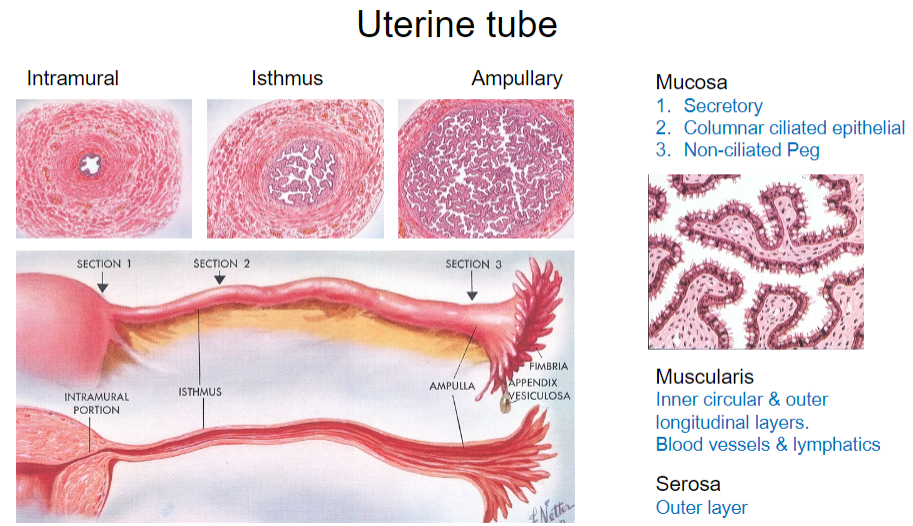
Secretory cells
Columnar ciliated epithelial cells
Non-ciliated peg cells
-
What is the structure of the muscularis layer in the uterine tube? (2)
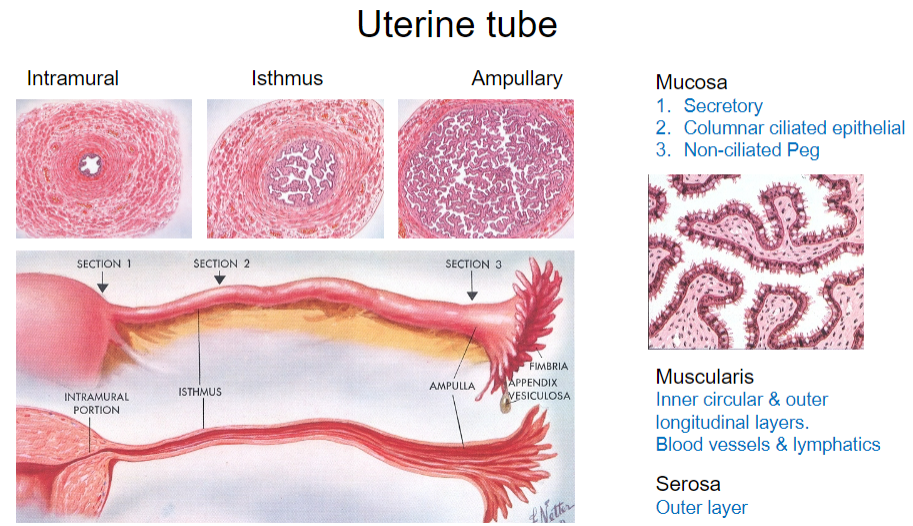
Inner circular layer
Outer longitudinal layer
-
What are the functions of the blood vessels and lymphatics in the uterine tube? (1)
They provide nutrients and remove waste from the uterine tube.
-
What is the outermost layer of the uterine tube? (1)
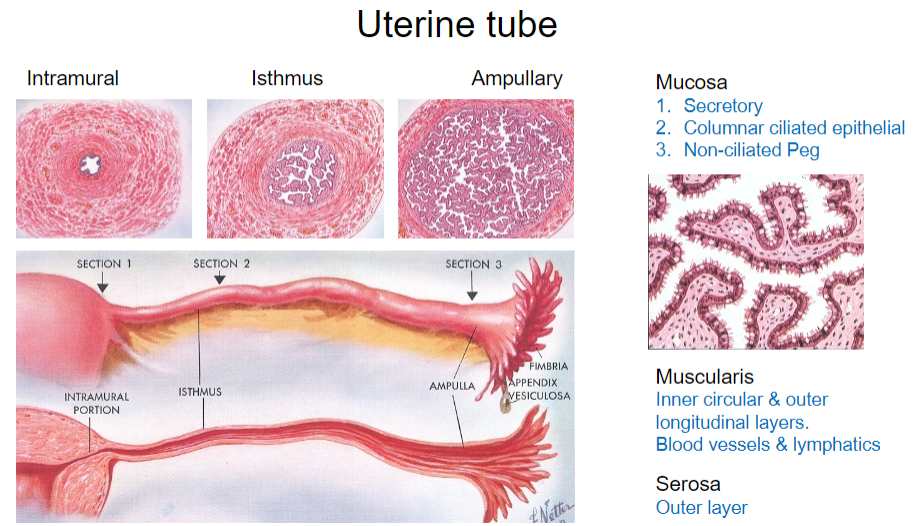
Serosa
-
When can the oocyte pass down the uterine tube, and what processes facilitate this? (2)
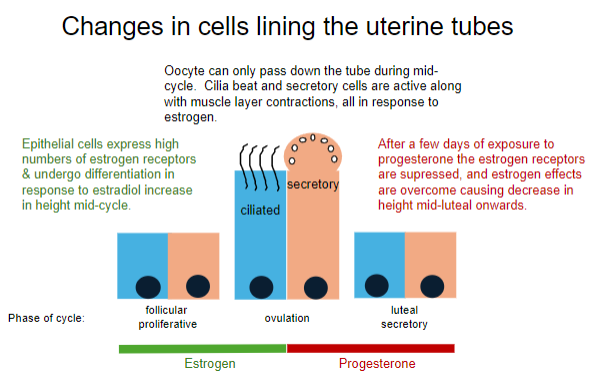
The oocyte can pass down the tube during mid-cycle (ovulation).
Cilia beat, secretory cells are active, and muscle layer contractions occur, all in response to estrogen.
-
How do epithelial cells in the uterine tube respond to estrogen during the follicular phase? (2)
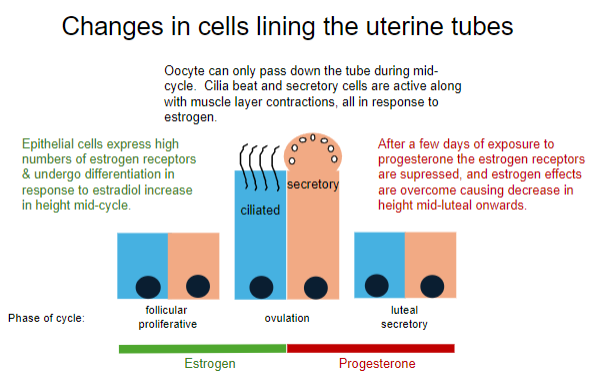
Epithelial cells express high numbers of estrogen receptors.
They undergo differentiation, increasing in height in response to an increase in estradiol.
-
What happens to the uterine tube epithelial cells after exposure to progesterone during the luteal phase? (2)
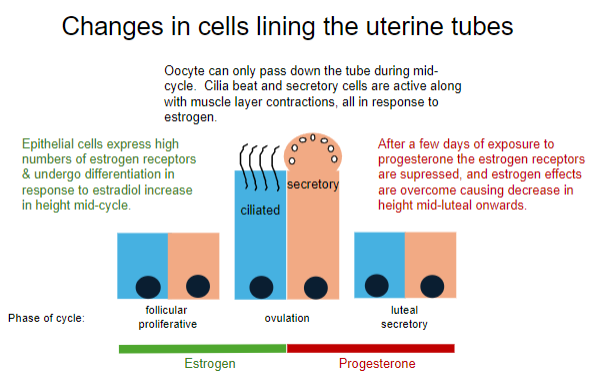
Estrogen receptors are suppressed.
Estrogen effects are overcome, causing a decrease in cell height during the mid-luteal phase onwards.
-
What hormones dominate the different phases of the menstrual cycle? (5)
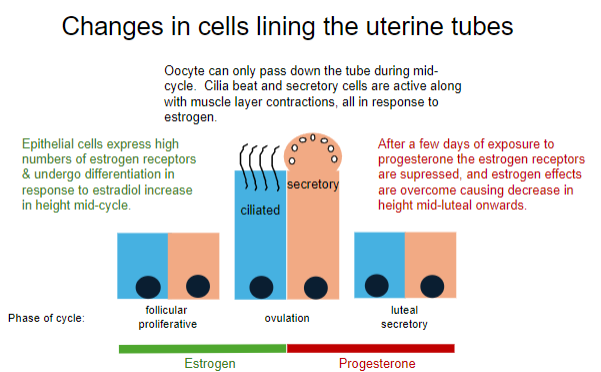
Follicular phase: Estrogen (Days 1-14)
Proliferative phase: Estrogen (Days 5-14)
Ovulation: Estrogen (Day 14)
Luteal phase: Progesterone (Days 15-28)
Secretory phase: Progesterone (Days 15-28)
-
What is the biggest cell in the body? (1)
The egg (100um in diameter, red blood cell is around 7-8um)
-
How long does the egg remain in the uterine tube before fertilization? (1)
The egg remains in the tube for approximately 5 days.
-
Where does fertilization occur in the female reproductive system? (1)
Fertilization occurs in the ampulla of the uterine tube.
-
What are the potential consequences of damage to the uterine tube lining? (3)
Pain
Infertility
Ectopic pregnancy
-
What is laparoscopy, and what is it used for? (2)
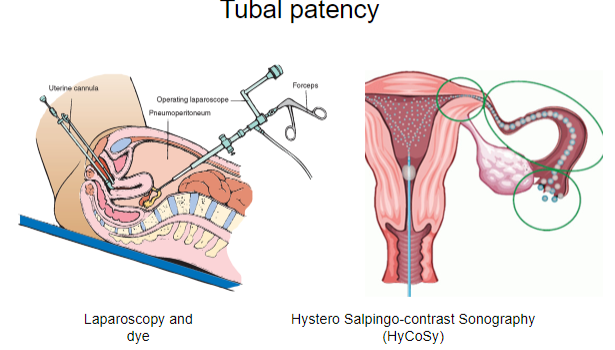
Laparoscopy is a minimally invasive surgical procedure that involves inserting a small camera (laparoscope) through small incisions in the abdomen to examine the internal organs, such as the uterus, ovaries, and fallopian tubes.
It is commonly used for diagnosing and treating conditions like infertility, endometriosis, pelvic pain, and tubal blockages.
-
What is Hystero Salpingo-contrast Sonography (HyCoSy) and what does it assess? (2)
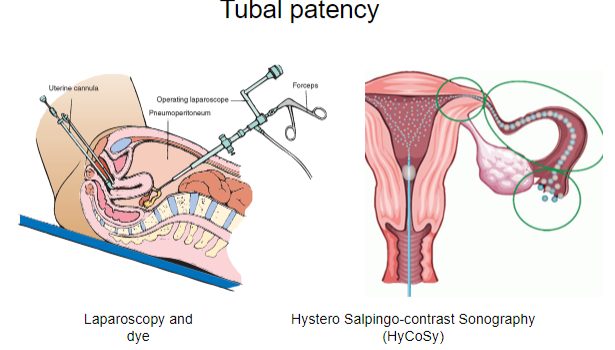
HyCoSy is a diagnostic procedure used to assess tubal patency (openness) and uterine conditions.
It involves injecting a contrast medium into the uterus and fallopian tubes and using ultrasound to visualize the flow of the contrast, checking for blockages or abnormalities.
-
What are the key structural features and functions of the cervix? (4)
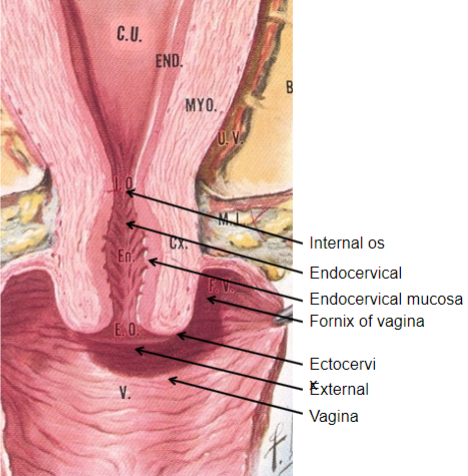
Muscular structure: The cervix is a muscular organ capable of significant expansion during childbirth.
Endocervical mucosa: About 3mm thick, it is lined with columnar mucous cells and contains numerous tubular mucous glands that secrete viscous, alkaline mucus into the lumen, providing a protective barrier against infections.
Function as a barrier: The mucus prevents pathogens from entering the uterus but still allows passage of motile sperm.
Ectocervix: Covered with nonkeratinized stratified squamous epithelium, similar to the vaginal lining, providing further protection.
-
What changes occur in the cervix during the follicular phase of the menstrual cycle, and how do these changes support fertilization? (5)

Vascularity and edema: Estrogen increases vascularity in the cervix and causes edema (swelling), preparing the cervix for potential fertilization.
Mucous changes: Estrogen causes the cervical mucus to become less viscous, which facilitates sperm passage.
Composition of mucus: The mucus composition changes to contain glycoproteins.
Microscopic channels: These glycoproteins align to form microscopic channels within the mucus.
Sperm transport: The aligned channels allow sperm to swim up the cervix towards the uterus, aiding fertilization.
-
What changes occur in the cervix during the luteal phase of the menstrual cycle, and how do these changes impact fertility? (4)

Reduced mucus secretion: Progesterone reduces the secretion of cervical mucus.
Increased viscosity: The mucus becomes more viscous with reduced water content.
Mesh-like structure: The glycoproteins in the mucus form a mesh-like structure that acts as a barrier.
Barrier to sperm and microorganisms: This mucus structure prevents sperm from passing through and helps protect against infection, reducing the chance of fertilization.
-
What are the structural features and functions of the vagina? (5)
Structure:
Thick-walled tube approximately 10cm long.
Lined with specialized squamous epithelial cells.
Environment:
Warm, damp, and contains glycoproteins, creating an environment conducive to reproduction.
Infection prevention:
The acidic secretions provide antimicrobial protection, preventing infections.
Layers of epithelial cells are constantly shed and flow downward, aiding in cleaning.
Secretions:
Secretions are produced by the cervix and vaginal epithelium (transudation).
Secretions change throughout the menstrual cycle.
Bartholin’s glands:
Located near the vaginal opening, they secrete mucus to lubricate the vagina.
Homologous to the bulbourethral glands in males.
-
What are the effects of estrogen and progesterone on the endometrium? (4)
Estrogen:
Stimulates the growth and proliferation of the endometrial lining during the proliferative phase.
Increases the number of progesterone receptors in the endometrial cells.
Progesterone:
Induces differentiation of the endometrium during the secretory phase, preparing it for potential implantation.
Reduces cell division and promotes the secretion of glycogen and lipids in the endometrial glands.
Opposes the estrogenic effects, halting further proliferation.
-
What is the major role of the uterine tube? (2)
Transport of the ovum from the ovary to the uterus.
Site of fertilization, typically occurring in the ampullary region of the tube.
-
How does cervical mucus change throughout the menstrual cycle and why is this important? (4)
Follicular phase (Estrogen dominant):
Cervical mucus becomes thin, clear, and watery, facilitating sperm movement through the cervix.
Ovulation:
Mucus reaches peak clarity and stretchability, providing the ideal environment for sperm survival and motility.
Luteal phase (Progesterone dominant):
Mucus becomes thick and viscous, creating a barrier to sperm and microorganisms.
Importance:
These changes optimize the chances of fertilization during the fertile window and protect the reproductive tract at other times.
-
The first half of the menstrual cycle is dominated by estrogen, what are the different effects of this hormone on the uterine tube and cervical mucus? (4)
Uterine tube:
Estrogen increases the activity of the ciliated epithelial cells, enhancing the transport of the egg towards the uterus.
Stimulates secretory activity, aiding in creating an environment that supports the ovum and sperm.
Cervical mucus:
Estrogen causes the mucus to become clear, thin, and stretchy, which facilitates sperm passage into the uterus and fallopian tubes.
-
The second half of the menstrual cycle is dominated by progesterone, what are the different effects of this on the uterine tube and cervical mucus? (4)
Uterine tube:
Progesterone reduces cilia activity and secretory function, preparing the tube for possible implantation by creating a less hospitable environment for sperm and egg transport.
Cervical mucus:
Mucus becomes thick, opaque, and sticky, acting as a barrier to sperm and pathogens.
-
Uterine tube secretory and cilia activity is at a maximum around the time of ovulation and for the next 5 or so days, what is the significance of this? (3)
Significance:
Enhances the environment for sperm survival and movement towards the egg.
Facilitates the capture and transport of the egg towards the uterus.
Ensures optimal conditions for fertilization and early embryo development.
-
How might the progesterone-only pill affect the progress of sperm and fertilisation? (3)
Effects on cervical mucus:
The progesterone-only pill thickens cervical mucus, making it more difficult for sperm to enter the uterus.
Effects on uterine lining:
It prevents the endometrium from thickening, making implantation less likely.
Impact on ovulation:
In some cases, it may suppress ovulation, reducing the chances of fertilization altogether.

