-
Where are the ovaries?
located in pelvic cavity on lateral sides of uterus and connected to body wall by ligaments that are continuous with the peritoneum
-
What is the histology of the ovaries?
- 4 layers (from superficial to deep): surface (germinal) epithelium, tunica albuginea, ovarian cortex, ovarian medulla
-
What is the surface (germinal) epithelium layer of the ovaries?
layer of cuboidal epithelial cells (modified visceral peritoneum lacking connective tissue)
-
What is the histology of tunica albuginea?
– dense connective tissue
-
What does the ovarian cortex contain?
contains ovarian follicles and connective tissue
o follicle = layer(s) of cells surrounding each developing oocyte that supports and protects it through its development
-
What does the ovarian medulla contain?
contains blood and lymph vessels, nerves, and connective tissue
-
What are the 3 sections of the uterine (fallopian) tubes?
- infundibulum
- ampulla = middle: site where fertilization usually occurs
- isthmus: connects to uterus
-
What is the infundibulum?
- a section of the fallopian tube
- suspended over each ovary,
- opening of uterine tube into peritoneal cavity,
- has finger-like projections called fimbriae that cover the ovary during ovulation. They help capture and move the oocyte into the uterine tube
-
What is the histology of the uterus?
- mucosa: simple columnar epithelium (two cells types)
- muscularis externa: smooth muscle (contraction helps move oocyte/cell mass along the tube)
- serosa: visceral peritoneum
-
What are the two kinds of cells in the simple columnar epithelium mucosa in the fallopian tubes?
- ciliated cells: help move oocyte/zygote/morula along the tube
- non-ciliated secretory cells with microvilli: secretes fluid that provides nutrients to oocyte/cell mass
-
What is the Uterus (womb) anatomically?
- Hollow, muscular organ located superior to bladder
- 3 parts:
- fundus: superior to isthmus of uterine tubes
- body: main portion, space within = uterine cavity, site where most embryo implantation and growth occur
- cervix: inferior, narrow passageway that opens into vagina
-
What is the histology of the uterus?
- it has 3 layers: endometrium, myometrium (muscularis externa), and perimetrium (serosa)
-
What is the histology of the myometrium of the uterus?
- smooth muscle
-
What is the histology of the perimetrium of the uterus?
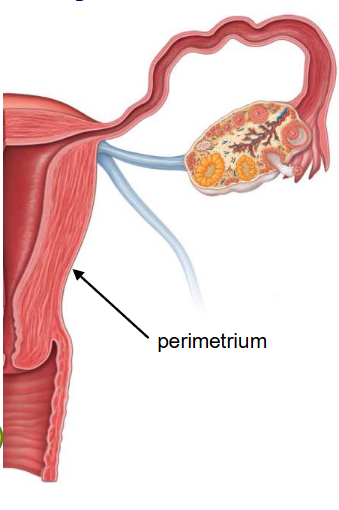
- outer layer
- visceral peritoneum
-
What is the histology of the endometrium of the uterus?
- mucous membrane composed of a simple columnar epithelium that lines the inner surface of the uterus
- specialized lamina propria that consists of 2 highly vascularized layers: Functional layer (stratum functionalis) and Basal layer (stratum basalis)
-
What is the histology of the Basal layer (stratum basalis) of the endometrium of the uterus?
permanent layer attached to myometrium
undergoes mitosis to replace the stratum functionalis and the simple columnar epithelium
-
What is the histology of the Functional layer (stratum functionalis) of the endometrium of the uterus?
superficial layer
develops at puberty and is shed monthly (menstruation) along with the simple columnar epithelium
contains endometrial glands (epithelial tissue) that secrete a nutritive fluid for the embryo prior to formation of the umbilical cord
-
What is the vagina (birth canal) anatomically?
connects uterus to external genitalia
female organ of copulation
-
What is the histology of the vagina?
- mucosa: thick stratified squamous epithelium, has rugae
- muscularis externa: smooth muscle
- adventitia: fibroelastic connective tissue
-
What are the reproductive structures that lie external to the vagina e.i. are part of the vulva?
mons pubis, labia majora/minora, clitoris, a vestibule (vagina and external urethral orifice) and greater vestibular glands
-
What is the mons pubis anatomically?
adipose tissue that overlies and cushions pubic symphysis
-
What is the labia majora/minora anatomically?
the labia majora are two large skin folds that surround the labia minora
the labia minora are small inner folds of skin that surround the vestibule
-
What are the greater vestibular glands of the vulva do?
secrete mucus to lubricate the vestibule
-
What is the clitoris anatomically?
mainly internal, with small external portion at anterior junction of labia minora
contains erectile tissue
derived from the same embryonic tissue as the penis
-
What is oogenesis?

-
What does 1 primary (1 degree) oocyte form?
forms 1 ovum and 2 or 3 polar bodies
-
What are polar bodies?
discarded nuclear material
-
What are oogonia?
- diploid stem cells that multiply by mitosis during fetal development
- differentiate into primary oocytes
-
How many primary oocytes (2n) are there at birth, what are they doing?
- ~ 1 million in ovaries at birth
- enter meiosis I before birth, but arrested in prophase I
- at puberty less than half of oocytes remain
-
What happens with secondary (2 degree) oocyte (n)?
o begins meiosis II and arrests in metaphase II
o this is ovulated (usually 1/month)
o ~ 500 ovulated from puberty to menopause
-
What do germ cells in the ovarian follicles do during the Late Embryonic and Fetal period (before birth)?
migrate to the developing gonads where they differentiate into oogonia
-
What do oogonia in the ovarian follicles do during the Late Embryonic and Fetal period (before birth)?
Oogonia begin to proliferate in the embryonic period until several million are formed, at which point proliferation ends
Oogonia begin to differentiate into primary oocytes during the early fetal period: Meiosis I begins, but stops in prophase I, Meiotic arrest continues until puberty
-
What do primordial follicles do in the ovarian follicles do during the Late Embryonic and Fetal period (before birth)?
- they form, Primary oocytes become surrounded by a single layer of flat pre-granulosa (follicular) cells
- Most primordial follicles with primary oocytes begin to degenerate over time, such that there are fewer at birth.
-
How do the ovaries develop during childhood? ( although mostly inactive)
some of the primordial follicles develop into primary follicles: the single layer of flat pre-granulosa cells becomes cuboidal – now called granulosa cells
however, in the absence of reproductive hormones, primordial and primary follicles also continue to degenerate such that there is less than half a million primary oocytes are left at puberty
-
How do the ovaries develop during puberty?
- Each month, primary follicles continue to form and reproductive hormones selectively stimulate some of these follicles to continue their development in the ovarian cortex.
- They pass through one or more of the following stages: secondary follicle, vesicular (antral) follicle, preovulatory (graafian) follicle, corpus luteum, corpus albicans
-
What is the secondary follicle?
- one of the follicles the primary follicles can stimulate to develop each month
- during the transition from primary to secondary follicle, hormone secreting theca cells form from surrounding connective tissue cells
- granulosa cells proliferate (become stratified) and start to secrete fluid and estrogen
- fluid-filled spaces between granulosa cells start to develop as fluid accumulates
-
What is the vesicular (antral) follicle?
- one of the follicles the primary follicles can stimulate to develop each month
the fluid filled spaces unite into a single large antrum
granulosa cells that still surround oocyte = corona radiata
usually, only one dominant vesicular follicle will continue development from this point per ovarian cycle
-
What is the preovulatory (graafian) follicle?
- one of the follicles the primary follicles can stimulate to develop each month
the follicle grows significantly in size and protrudes from the surface of ovary
-
What do rising hormone levels cause in the preovulatory (graafian) follicle?
- formation of a secondary oocyte – completion of Meiosis I; enters Meiosis II and arrests in Metaphase II
- ovulation: release of secondary oocyte (surrounded by corona radiata) from follicle into peritoneal cavity (follicle remains in ovary)
-
What is penetrated if fertilization occurs?
if fertilization occurs, the acrosome of a single sperm will penetrate the corona radiata
-
What is the corpus luteum?
- one of the follicles the primary follicles can stimulate to develop each month
follicle that remains after ovulation
produces high levels of hormones that support fetal development
if there is no pregnancy, it degenerates into the corpus albicans
-
What is the corpus albicans?
- one of the follicles the primary follicles can stimulate to develop each month
- scar-like structure on surface of ovary
- does not release any hormones
-
What is tubal ligation?
surgical procedure on the uterine tube that prevents passage of gametes through the uterine tube (does not affect ovarian/menstrual cycles)
-
What is a vasectomy?
- relatively minor procedure that prevents sperm passage through the vas deferens (ejaculation still occurs, but the semen does not contain sperm or testicular fluid)
-
What is an ectopic pregnancy?
complication of pregnancy in which the embryo implants outside of the body of the uterus (mostly in the uterine tube, and to a lesser extent in the peritoneal cavity, cervix, ovarian surface)
in most cases the developing fetus is unable to survive
can lead to rupture of uterine tube (which can be life-threatening) and impaired fertility in future

