Treatment of Hypertension (Physiology)
Session summary High blood pressure is a significant risk factor for cardiovascular disease and numerous other pathologies. The main focus of this session will be on the principles of renal and cardiovascular physiology that are exploited in pharmacological treatment of hypertension. We are not introducing new material in this session but rather integrating material previously covered in cardiovascular physiology and pharmacology and renal physiology. Learning outcomes At the end of this session you will be able to: Explain the control of blood pressure over the short and long terms Define hypertension and its associated risks Describe the risk factors for hypertension, and lifestyle modifications that may prevent it Explain pharmacological treatment of hypertension and its physiological basis
-
What is blood pressure? (1)
✩ Blood pressure is the pressure exerted by blood on blood vessels.
-
What are the mechanisms involved in short-term regulation of blood pressure? (2)
Short-term regulation involves:
✩ Baroreceptors, which sense changes in blood pressure and signal to the nervous system.
✩ Sympathetic and parasympathetic outflow, which adjust heart rate, contractility, and vascular tone.
-
What are the mechanisms involved in long-term regulation of blood pressure? (2)
✩ Long-term regulation involves hormonal control of total body sodium, which affects blood volume and extracellular fluid volume (ECFV).
✩ It also involves the degree of vasoconstriction, which influences total peripheral resistance (TPR).
-
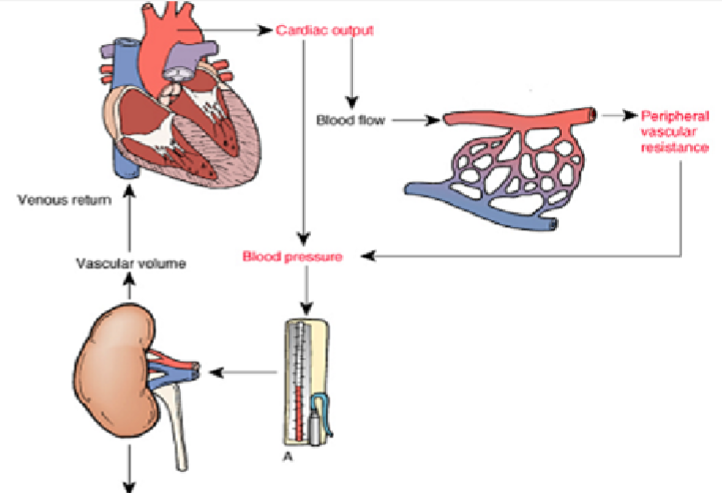
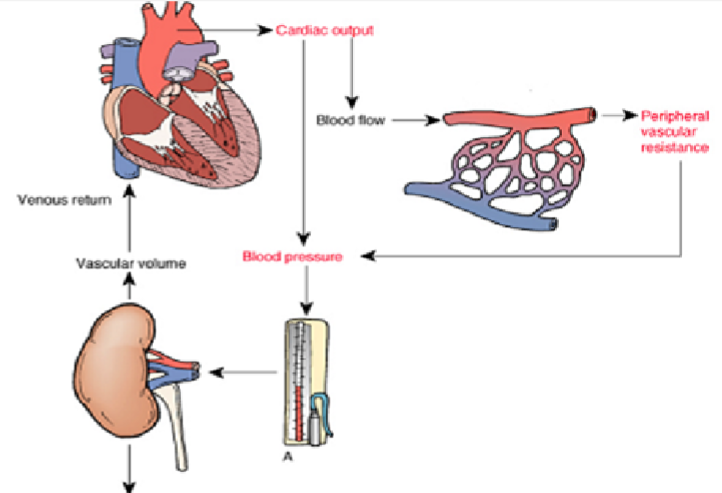
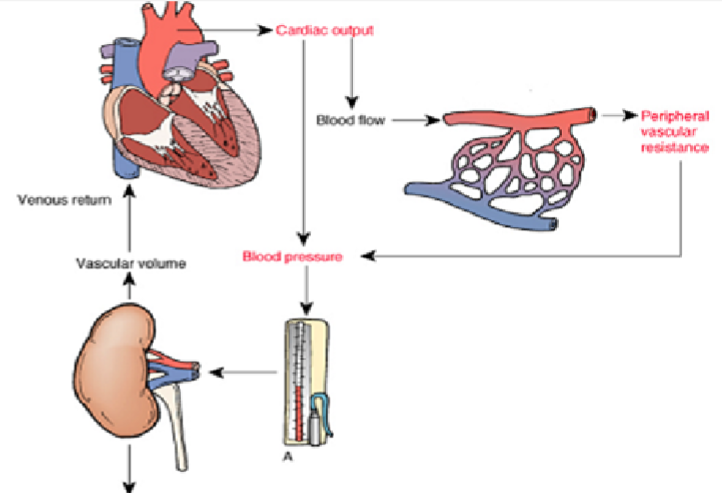
What is the equation for mean arterial blood pressure (MABP)? (1)
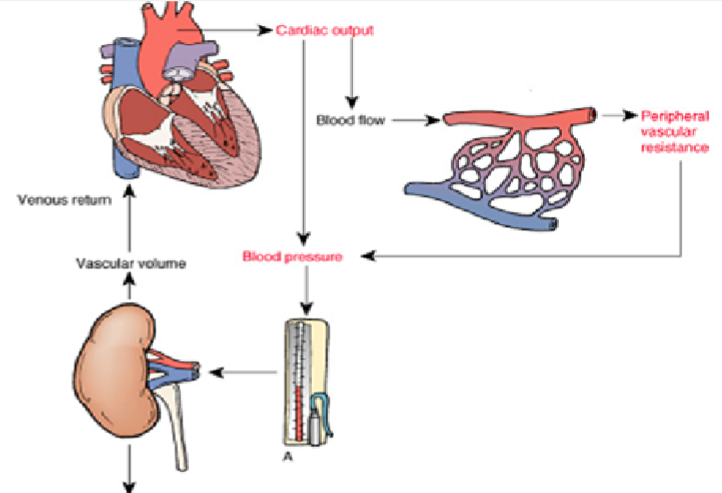
MABP ≈ CO x TPR
MABP: mean arterial blood pressure
CO: cardiac output
TPR: total peripheral resistance
-
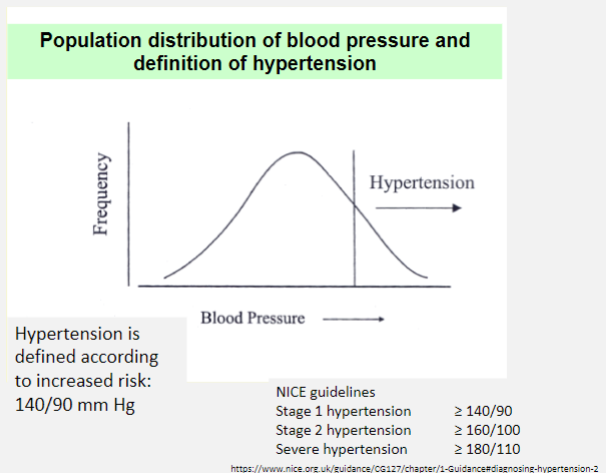
Picture demonstrating population distribution of blood pressure and definition of hypertension:
-
How are criteria for hypertension defined? (1)
✩ Hypertension is typically defined based on blood pressure measurements. According to current guidelines, hypertension is diagnosed when systolic blood pressure (SBP) is consistently ≥ 140 mmHg and/or diastolic blood pressure (DBP) is consistently ≥ 90 mmHg.
-
What are the health risks associated with hypertension? (5)
Hypertension is a significant risk factor for various health conditions, including:
✩ Stroke
✩ Ischemic heart disease
✩ Left ventricular hypertrophy and heart failure
✩ Renal failure
✩ Retinopathy
-
What are the causes of secondary hypertension? (4)
Secondary hypertension refers to cases where an identifiable cause can be found and accounts for less than 10% of all hypertension cases. Causes include:
✩ Renal disease
✩ Vascular conditions such as renal artery stenosis
✩ Hormonal disorders such as Conn’s syndrome or Cushing’s syndrome
✩ Monogenic genetic diseases like Liddle’s syndrome
-
What are the causes of primary or essential hypertension? (2)
✩ Primary or essential hypertension accounts for over 90% of all cases. It is characterized by elevated blood pressure without an identifiable cause.
✩ Proposed mechanisms include a combination of genetic predisposition and environmental factors.
-
What are the possible mechanisms and risk factors for essential hypertension? (9)
Possible mechanisms and risk factors for essential hypertension include:
✩ Increased sympathetic nervous system (SNS) activity
✩ Increased activity of the renin-angiotensin-aldosterone system (RAAS)
✩ Endothelial dysfunction
✩ Defects in vascular smooth muscle contraction
✩ Abnormalities in renal sodium handling, often exacerbated by increased salt intake
✩ Obesity and insulin resistance
✩ Advancing age, as hypertension becomes more prevalent with age
✩ Ethnicity, with higher rates observed in certain ethnic groups such as Afro-Caribbean populations
✩ Family history of hypertension/genetic predisposition
-
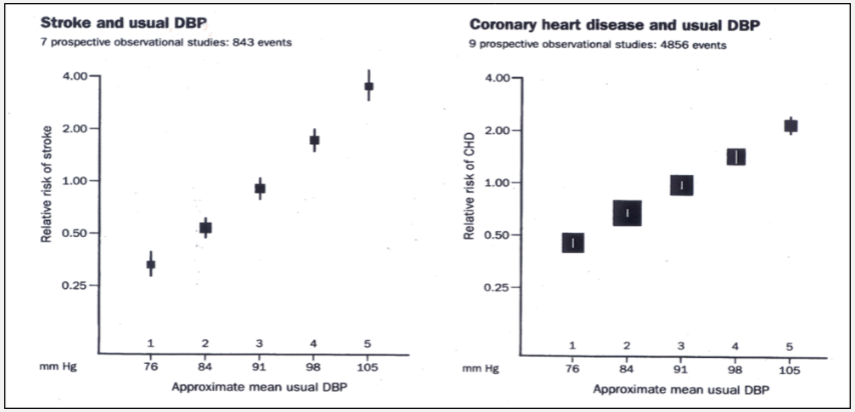
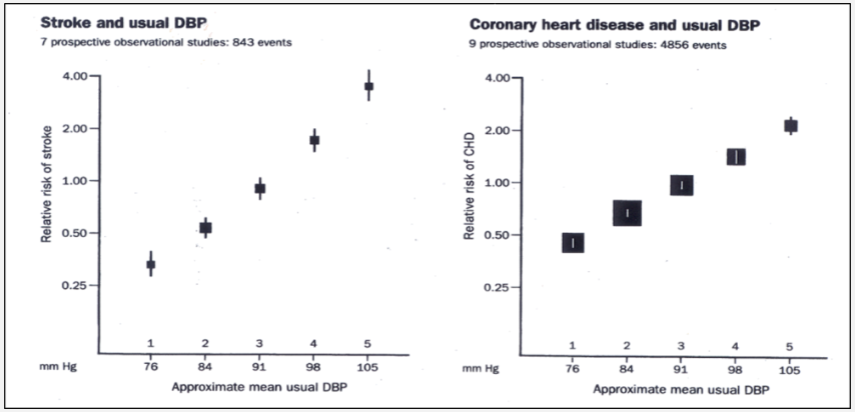
Why treat hypertension? (1)
Hypertension treatment is crucial due to its associated risks. For instance:
✩ Reduction of 5 mm Hg in diastolic blood pressure over 5 years can lead to significant risk reduction:
✩ Decrease in strokes by 42%
✩ Decrease in heart attacks by 16%
✩ Decrease in vascular mortality by 21%
-
What are the goals of anti-hypertensive treatment? (3)
The goals of anti-hypertensive treatment include:
✩ Achieving adequate blood pressure control, typically defined as < 140/90 mmHg, to alter relative risk of cardiovascular events.
✩ Prevention of target organ damage.
✩ Controlling other cardiovascular risk factors.
-
What are the treatment pathways for hypertension? (3)
Treatment pathways for hypertension include:
✩ Non-pharmacological approaches such as lifestyle modifications.
✩ Pharmacological treatment with medications.
✩ Surgical interventions, particularly if there's a known underlying cause such as Conn’s syndrome.
-
What lifestyle modifications can help manage hypertension? (6)
Lifestyle modifications that can help manage hypertension include:
✩ Quitting smoking
✩ Weight control
✩ Reducing salt intake
✩ Engaging in regular exercise
✩ Reducing alcohol intake
✩ Considering behavioral therapies such as cognitive-behavioral therapy (CBT)
-
What are the major classes of antihypertensive drugs? (5)
The major classes of antihypertensive drugs include:
✩ ACE inhibitors (Angiotensin-Converting Enzyme inhibitors)
✩ Angiotensin II receptor blockers (ARBs)
✩ Diuretics
✩ Drugs acting on the Sympathetic Nervous System
✩ Vasodilators
-
What are the side effects of ACE inhibitors? (2)

Side effects of ACE inhibitors include:
✩ Cough, which is common and occurs due to a decrease in bradykinin breakdown.
✩ Angioedema, which is rare but serious.
-
What side effect is common to both ACE inhibitors and AT1 receptor blockers? (1)
✩ Both ACE inhibitors and AT1 receptor blockers can lead to hyperkalemia, an elevated level of potassium in the blood.
-
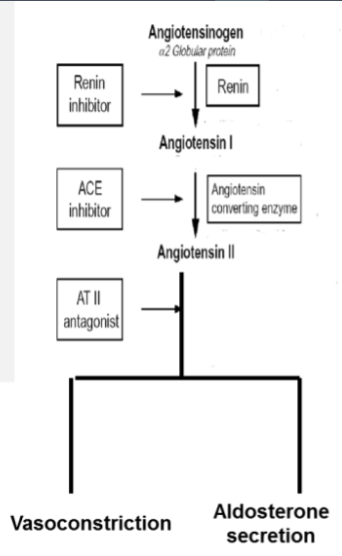
What is the mechanism of action of ACE inhibitors and AT1 receptor blockers? (1)
✩ Both ACE inhibitors and AT1 receptor blockers decrease vasoconstriction and aldosterone secretion to reduce blood pressure.
-
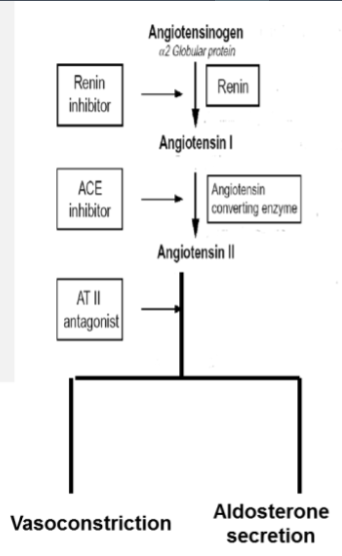
What is the mechanism of action of diuretics? (2)
✩ Diuretics increase sodium and water excretion, leading to a reduction in blood volume.
✩ As blood volume decreases, cardiac output (CO) is reduced, ultimately resulting in a decrease in blood pressure (BP), as per the equation BP ≈ CO x TPR (total peripheral resistance).
-
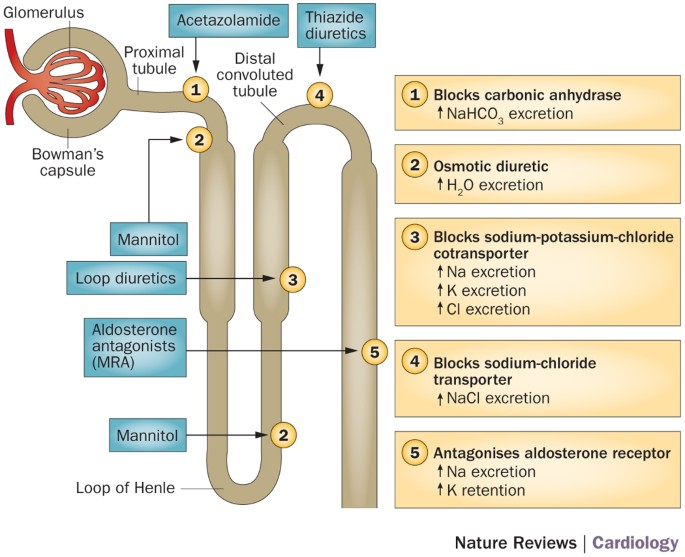
What are the effects of β1 receptors on the cardiovascular system? (2)
Activation of β1 receptors leads to:
✩ Increased heart rate (HR) and contractility, resulting in increased cardiac output (CO).
✩ Vasoconstriction, ultimately increasing total peripheral resistance (TPR) and blood pressure (BP).
-
How do beta blockers (β1 blockers) affect the cardiovascular system? (2)
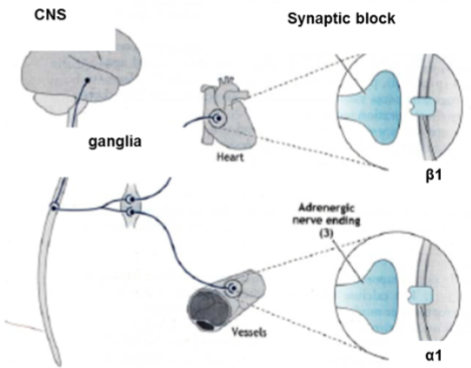
Beta blockers such as atenolol block β1 receptors, leading to:
✩ Reduction in heart rate (HR) and contractility, resulting in decreased cardiac output (CO).
✩ Inhibition of renin release.
-
How do potassium channel openers act as vasodilators? (3)
![Potassium channel openers act on arterioles by:✩ Increasing outward potassium (K+) current, leading to hyperpolarization of smooth muscle cells.✩ Reducing voltage-gated calcium channel (VGCC) activity and intracellular calcium concentration ([Ca]i).✩ Decreasing myosin light chain kinase (MLCK) activity, which results in increased relaxation and vasodilation of arterioles.](/flashcards/cardimage2/3926c975/258/8258268_back.png)
Potassium channel openers act on arterioles by:
✩ Increasing outward potassium (K+) current, leading to hyperpolarization of smooth muscle cells.
✩ Reducing voltage-gated calcium channel (VGCC) activity and intracellular calcium concentration ([Ca]i).
✩ Decreasing myosin light chain kinase (MLCK) activity, which results in increased relaxation and vasodilation of arterioles.
-
What are examples of potassium channel openers? (1)
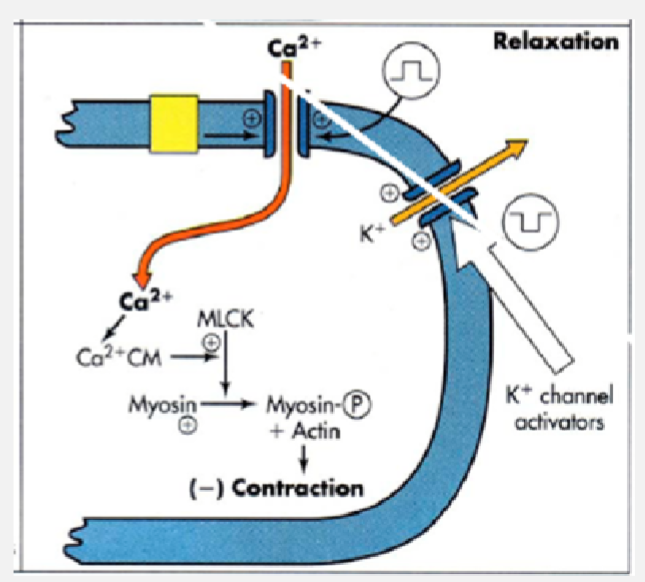
✩ Examples of potassium channel openers include minoxidil and diazoxide.
-
How do voltage-dependent calcium channel blockers act as vasodilators? (2)
![Voltage-dependent calcium channel blockers act on arterioles by:✩ Blocking voltage-gated calcium channel (VGCC) activity in vascular smooth muscle cells (VSMCs), leading to reduced intracellular calcium concentration ([Ca]i).✩ Decreasing myosin light chain kinase (MLCK) activity, which results in increased relaxation and vasodilation of arterioles.](/flashcards/cardimage2/3926c975/258/8258270_back.png)
Voltage-dependent calcium channel blockers act on arterioles by:
✩ Blocking voltage-gated calcium channel (VGCC) activity in vascular smooth muscle cells (VSMCs), leading to reduced intracellular calcium concentration ([Ca]i).
✩ Decreasing myosin light chain kinase (MLCK) activity, which results in increased relaxation and vasodilation of arterioles.
-
What is an example of a voltage-dependent calcium channel blocker? (1)
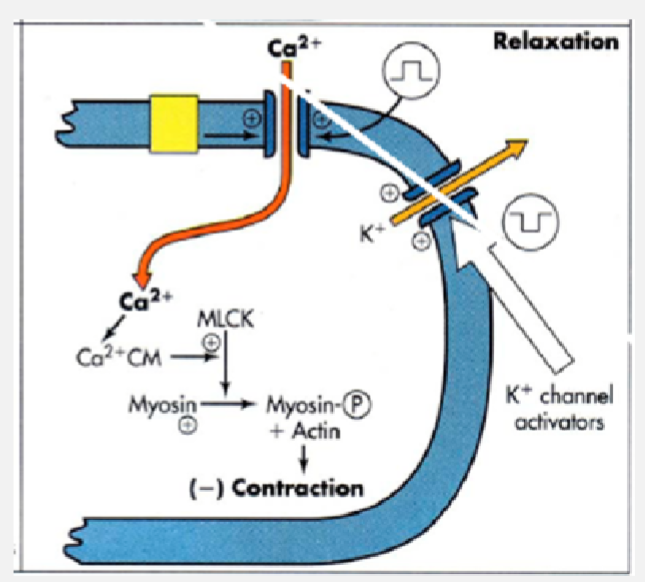
✩ An example of a voltage-dependent calcium channel blocker is nifedipine.
-
What are the key issues to consider in selecting drug therapy for hypertension? (6)
Key issues to consider include:
✩ Determining whether the hypertension is primary (also known as essential) or secondary.
✩ Reviewing evidence of efficacy of the chosen drug.
✩ Assessing potential side effects and drug interactions.
✩ Considering individual demographics and co-existing diseases.
✩ Evaluating the impact on quality of life and economic considerations.
✩ Guidelines from organizations like NICE (National Institute for Health and Clinical Excellence) can help navigate these complexities.
-
What is pressure natriuresis and its importance in long-term regulation of blood pressure? (3)
✩ Pressure natriuresis refers to the phenomenon where an increase in blood pressure leads to an increase in sodium excretion by the kidneys over time.
✩ This mechanism plays a crucial role in the long-term regulation of blood pressure by helping to maintain sodium balance in the body.
✩ As blood pressure rises, the kidneys respond by increasing sodium excretion, which helps to lower blood volume and subsequently decrease blood pressure.
-
Can you explain the mechanism of pressure natriuresis? (2)
✩ Pressure natriuresis is mediated by the kidneys' ability to adjust sodium excretion in response to changes in blood pressure. When blood pressure increases, there is an increase in renal artery pressure, which stimulates the kidneys to excrete more sodium.
✩ This increased sodium excretion leads to a reduction in extracellular fluid volume (ECFV), which helps to lower blood pressure back towards normal levels.

