Thyroid gland (Physiology)
Thyroid gland - Dr Peter Skorupski Session Summary Thyroid hormone is essential for normal growth and development in humans and throughout the vertebrates. It functions as an important metabolic regulator in adults. We will explore synthesis and action of thyroid hormone and its regulation by the hypothalamic-pituitary axis. We will conclude with a brief description of common disorders of thyroid function. Learning outcomes At the end of this session you will be able to: Provide an overview of thyroid function Identify the thyroid hormones and describe their synthesis and action Classify and describe thyroid hormone receptors Explain negative feedback control of thyroid hormone by the hypothalamic-pituitary axis Explain common disorders of hyper- and hypothyroidism Session resources Lecture slidesDownload Lecture slides Session activities Lecture recording part 1 Lecture recording part 2 Additional resources For some optional extra reading you could check this account of a case of hyperthyroidism in Vander's Human PhysiologyLinks to an external site.. Chapter 19 Medical Physiology: Integration Using Clinical Cases. See section A: Case Study of a Woman with Palpitations and Heat Intolerance Session conclusion Thyroid hormones have a very wide range of functions, essential for growth and development, and normal metabolic and physiological function in adults. Thyroid hormone disorders are not usually life threatening emergencies, but can still make one's life pretty miserable. Having said that, extreme thyrotoxicosis (a thyroid storm) is a medical emergency in adults, and uncorrected congenital deficiencies will lead to irreversible mental and physical developmental defects. Questions to think about Screening for primary hypothyroidism typically measures TSH rather than TH levels. Explain. Iodine deficiency, Hashimoto's disease and Graves disease can all lead to goitre. Explain
-
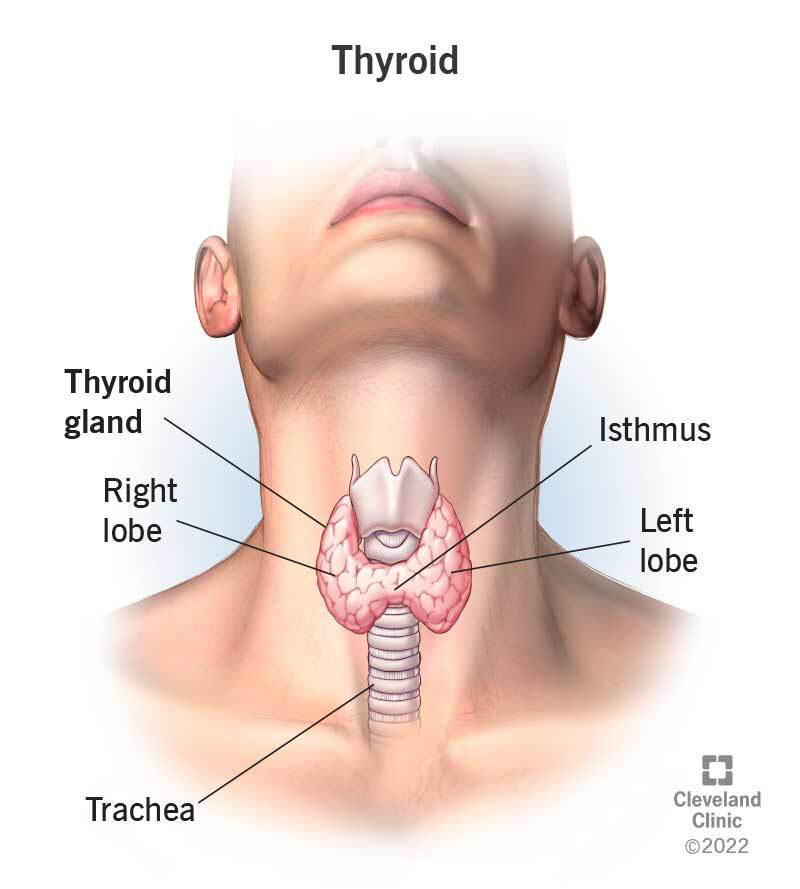
How does the blood supply to the thyroid gland compare to that of the kidney?
The thyroid gland has a rich blood supply, with more blood per unit weight than the kidney.
-
What artery supplies the thyroid gland from the subclavian artery?
The inferior thyroid artery supplies the thyroid gland from the subclavian artery.
-
What artery supplies the thyroid gland from the carotid artery?
The superior thyroid artery supplies the thyroid gland from the carotid artery.
-
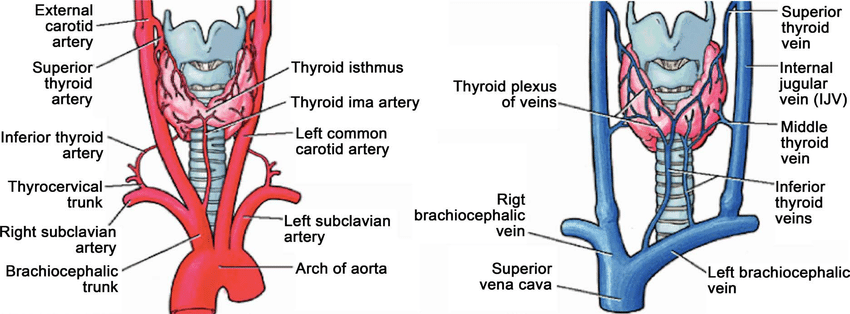
Picture demonstrating the histology of the thyroid gland:
-
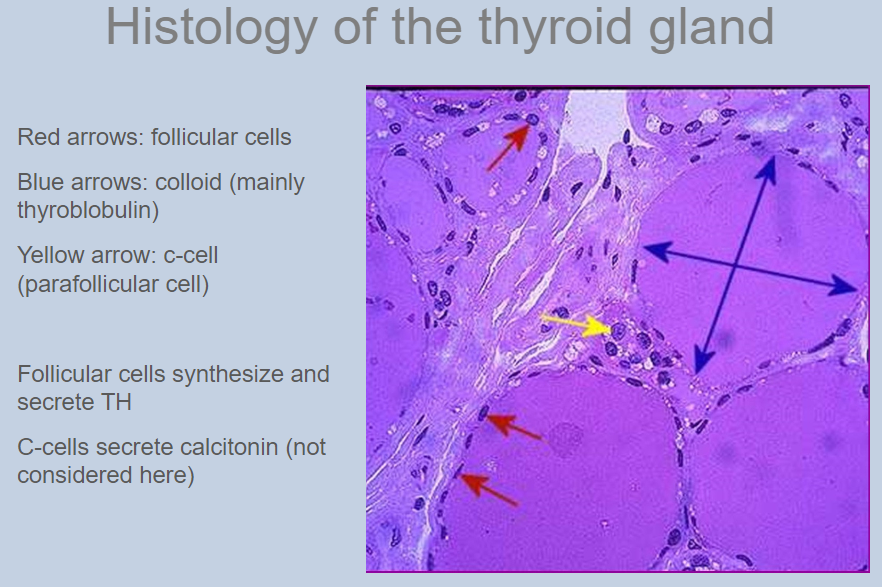
What are thyroid hormones derived from?
Thyroid hormones are derived from two iodinated tyrosine molecules, T3 and T4.
-
What is T4, and what is its role?
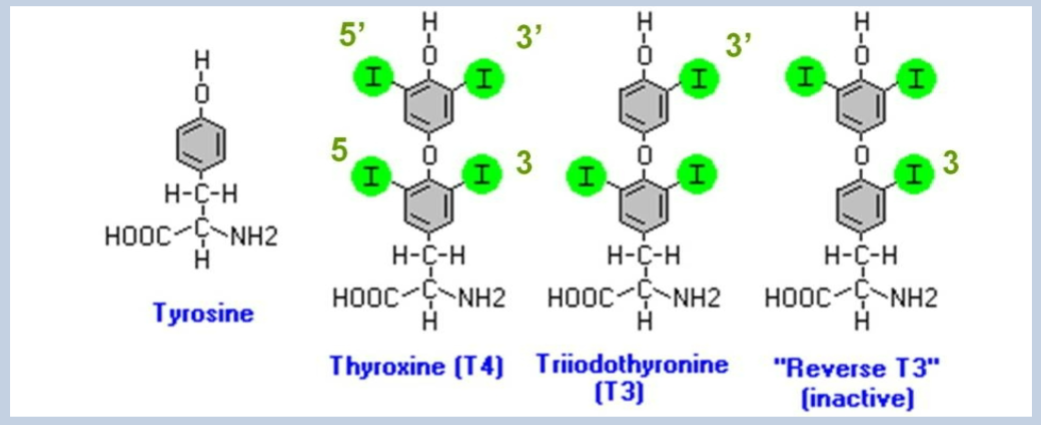
T4, or thyroxine, is the major form of thyroid hormone released into the blood and acts as a prohormone, being less active than T3.
-
What is T3, and what is its role?
T3, or triiodothyronine, is the active form of thyroid hormone that is converted from T4 in target cells.
-
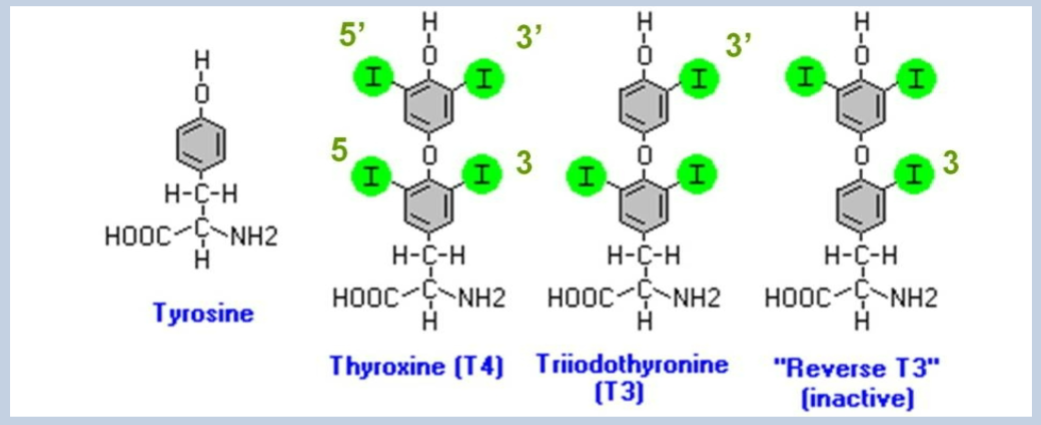
Picture demonstrating TH synthesis and release:
-
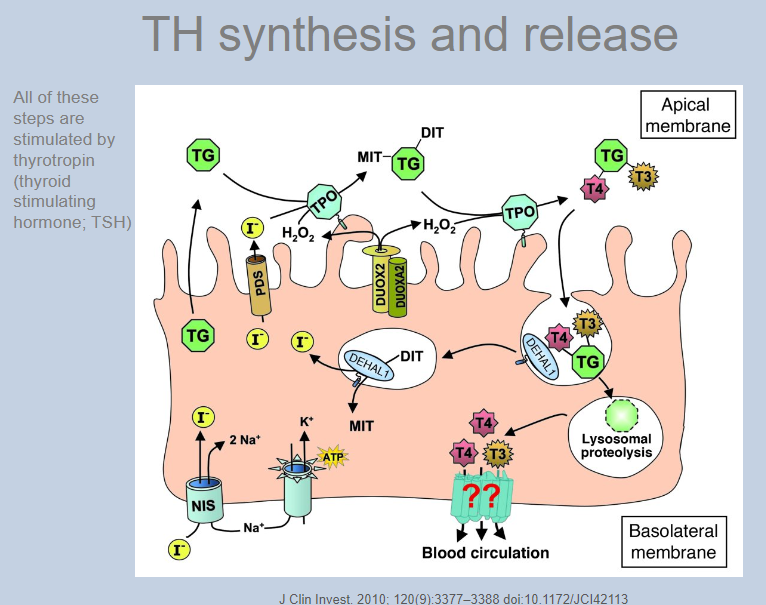
What is the first step in thyroid hormone synthesis?
The active uptake of iodide (I-) across the basolateral membrane, against its concentration and electrical gradient, by the Na/I symporter (NIS). This process is stimulated by thyroid-stimulating hormone (TSH).
-
What happens to iodide after it is taken up by the Na/I symporter?
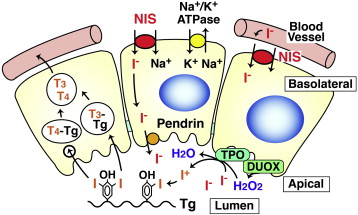
Iodide effluxes (diffuses) across the apical membrane via an exchanger known as pendrin (PDS).
-
How is iodide oxidized, and what enzyme catalyzes this reaction?
At the extracellular apical membrane of the thyroid gland, iodide is oxidized by hydrogen peroxide (H2O2) to iodine, catalyzed by thyroid peroxidase (TPO).
-
To what is iodine covalently bound during thyroid hormone synthesis?
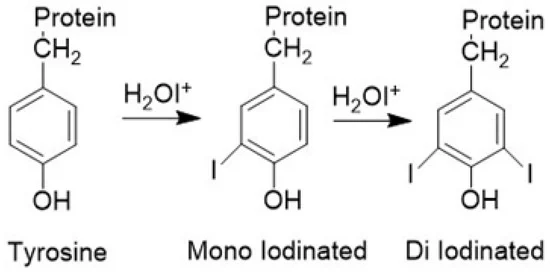
Iodine is covalently bound to tyrosine residues within the thyroglobulin (TG) macromolecule.
-
What triggers the uptake of colloid droplets into follicular cells?
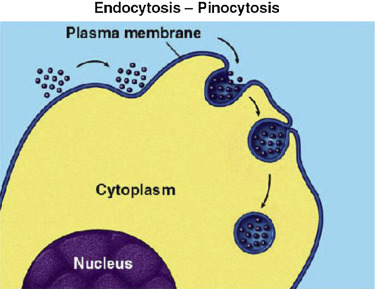
Thyroid-stimulating hormone (TSH) triggers the uptake of colloid droplets, which consist of thyroid hormones within thyroglobulin molecules, into the follicular cells by pinocytosis.
-
What occurs after colloid droplets are taken up into follicular cells?
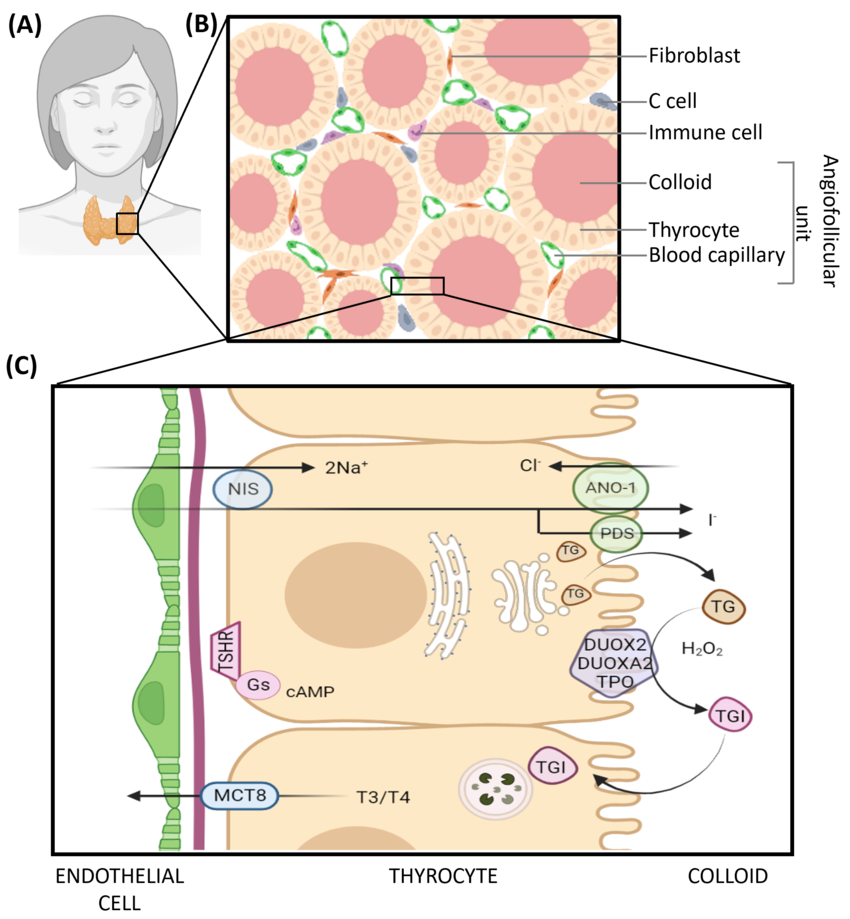
The colloid droplets fuse with lysosomes, causing hydrolysis of thyroglobulin and release of T3 and T4.
-
What percentage of T4 is converted to T3 before secretion, and what happens to the released iodide?
About 10% of T4 undergoes mono-deiodination to T3 before it is secreted, and the released iodide is reutilized.
-
How much thyroid hormone is secreted per day, and in what proportions?
Approximately 100 μg of thyroid hormone is secreted per day, with about 90% being T4 and 10% being T3.
-
What process is critical for thyroid hormone secretion?
Secretion of thyroid hormones relies on a membrane transporter.
-
What percentage of circulating thyroid hormones are bound to plasma proteins?
Over 99% of circulating thyroid hormones are bound to plasma proteins.
-
What is the main plasma protein that binds thyroid hormones, and what percentage does it bind?
The main plasma protein that binds thyroid hormones is thyroid-binding globulin (TBG), which binds approximately 70% of thyroid hormones.
-
Which other plasma proteins bind thyroid hormones, and what are their respective binding percentages?
Transthyretin (also known as prealbumin) and albumin both bind thyroid hormones, each accounting for 10-20% of the binding.
-
What are the serum concentrations of total T4 and T3?
The serum concentration of total T4 is approximately 100 nmol/L, and total T3 is approximately 2 nmol/L.
-
What are the serum concentrations of free T4 and free T3?
The serum concentration of free T4 is approximately 20 pmol/L (0.02% of total T4), and free T3 is approximately 5 pmol/L (0.4% of total T3).
-
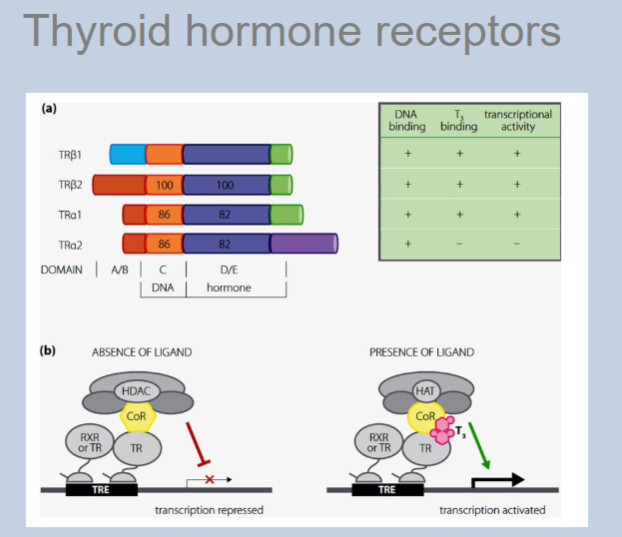
What type of receptors do thyroid hormones act on in target tissues?
Thyroid hormones act on thyroid hormone receptors (TRs), which belong to the nuclear receptor superfamily.
-
What is the primary function of thyroid hormone receptors (TRs)?
TRs function as ligand-activated transcription factors.
-
Which thyroid hormone has a high affinity for thyroid hormone receptors (TRs)?
T3 (triiodothyronine) has a high affinity for thyroid hormone receptors.
-
What is required for the activation of thyroid hormone receptors?
Activation of thyroid hormone receptors to thyroid hormone response elements (TREs) in the promoter regions of target genes, requires dimerization with another TR or with a retinoid X receptor (RXR).
-
How many genes encode thyroid hormone receptors, and what are they?
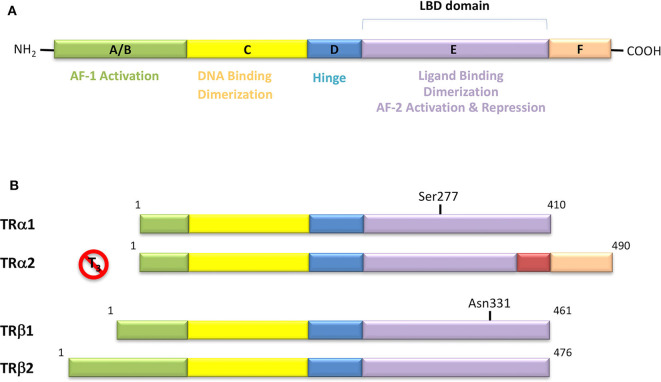
Thyroid hormone receptors are encoded by two genes: TR alpha and TR beta.
-
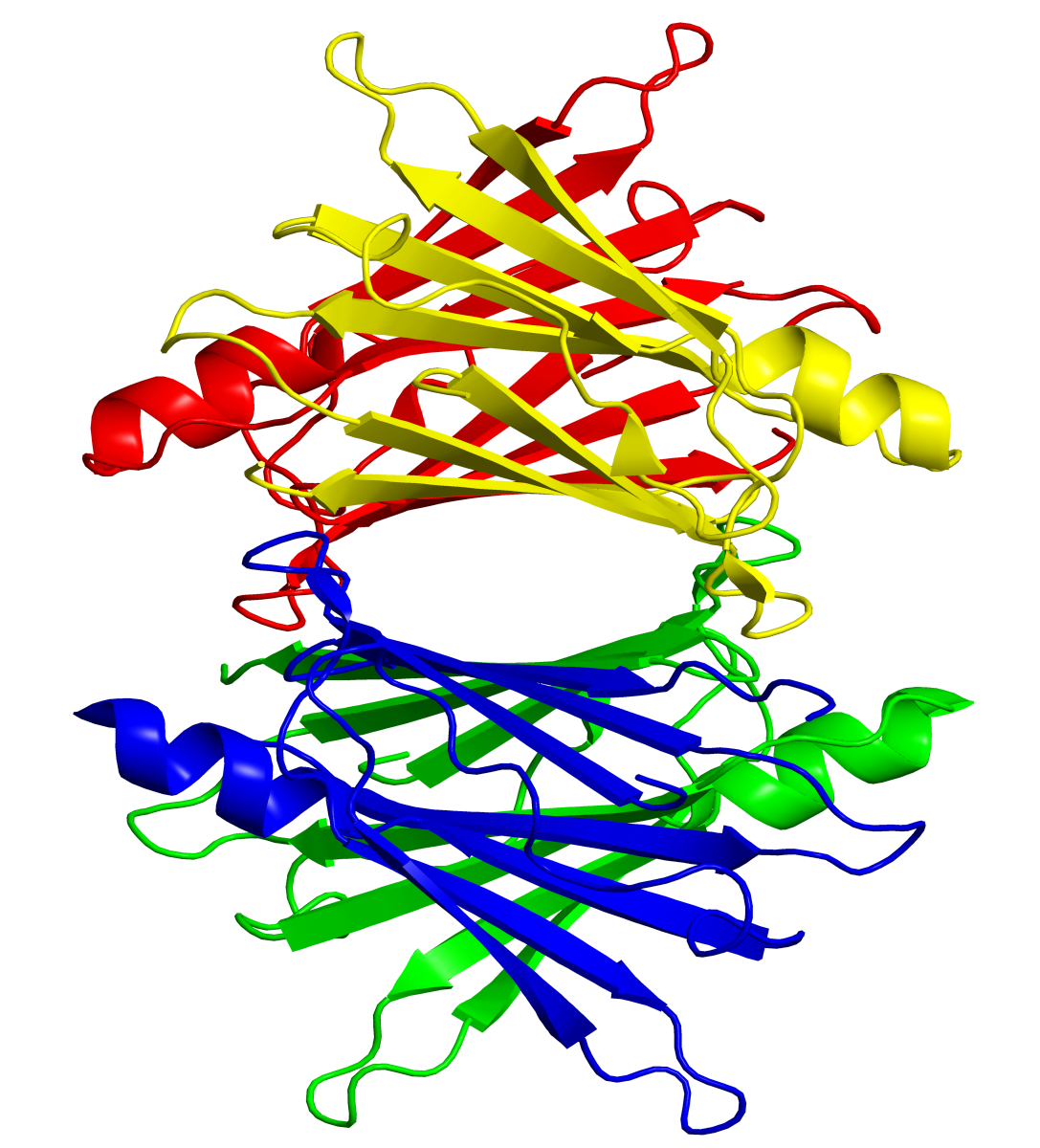
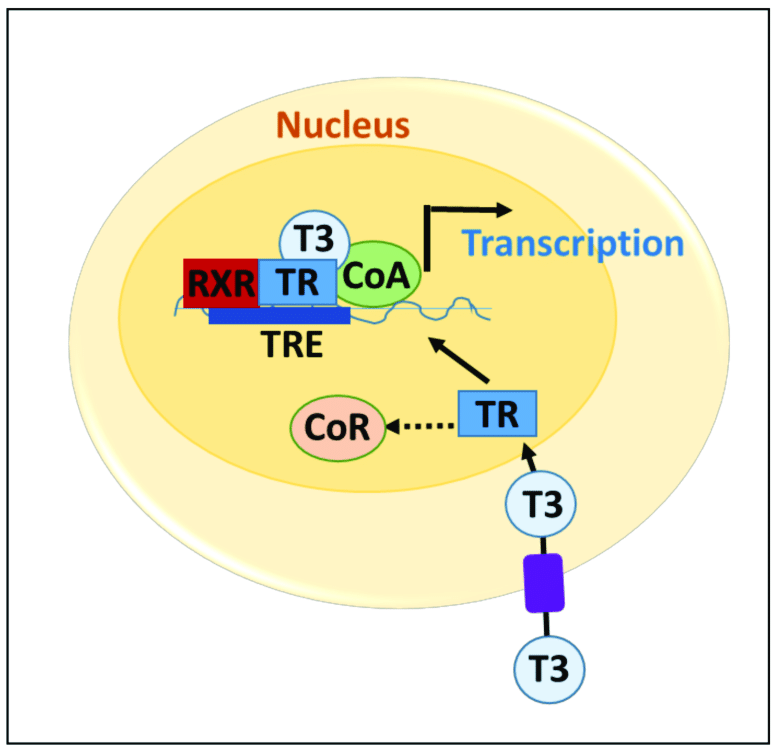
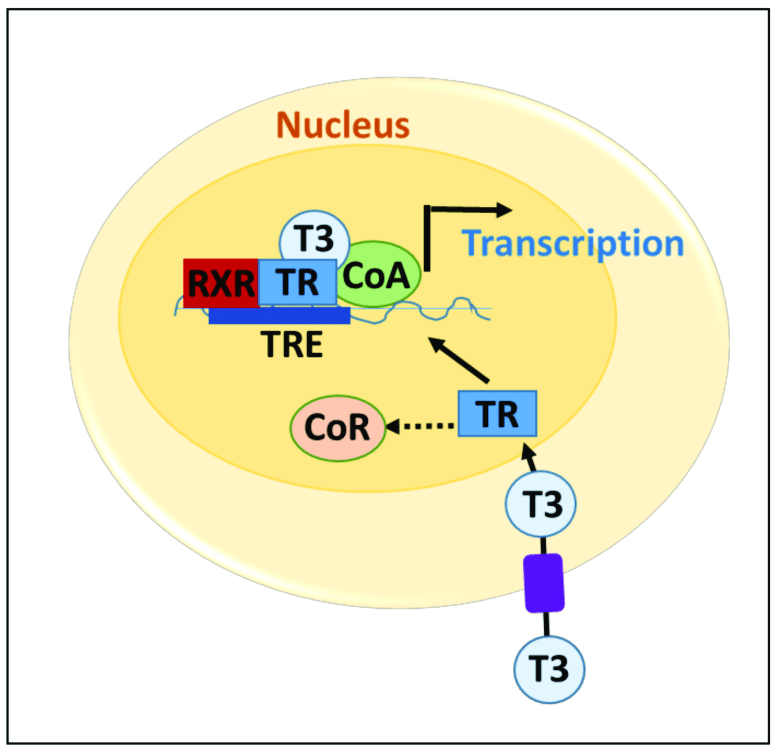
Picture demonstrating thyroid hormone receptors:
-
How are the relative levels of T3, T4, and inactive forms controlled in target tissues?
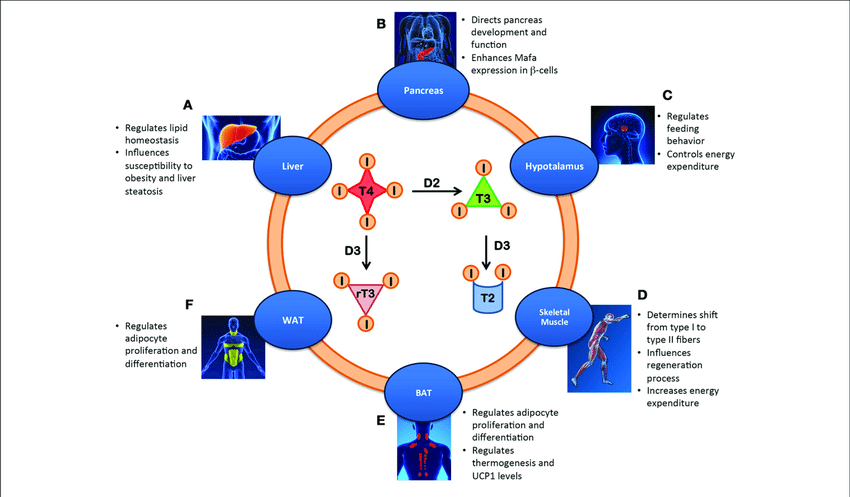
The relative levels of T3, T4, and inactive forms are controlled by three iodothyronine selenodeiodinases (D1, D2, and D3).
-
Why is selenium essential in the diet for thyroid hormone metabolism?
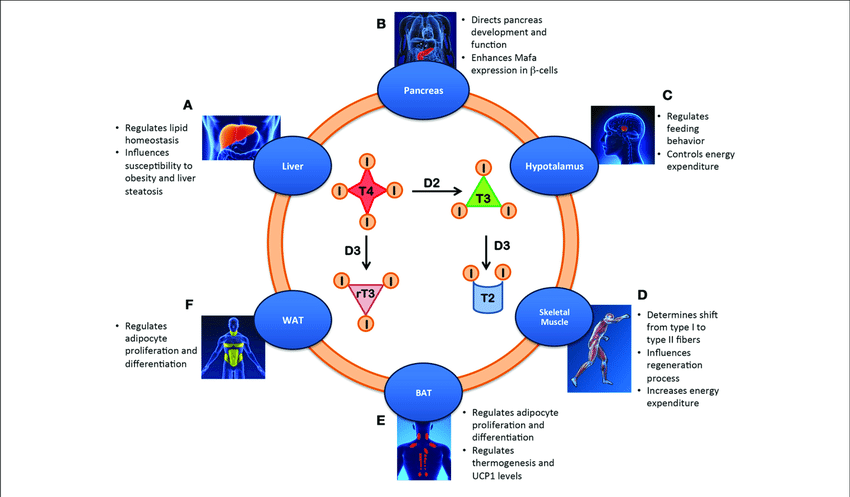
Selenium is a trace element essential in the diet because it is a component of the iodothyronine selenodeiodinases that regulate thyroid hormone metabolism.
-
What is the role of iodothyronine selenodeiodinases in thyroid hormone regulation?
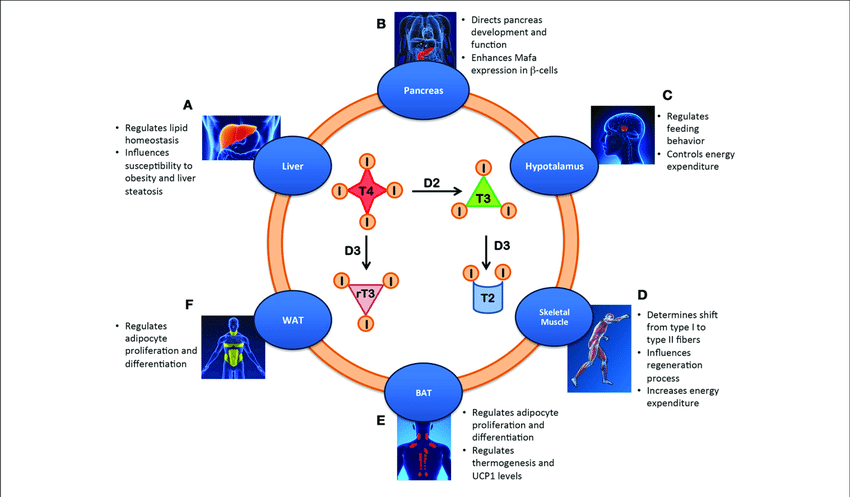
Iodothyronine selenodeiodinases regulate the amount of T3 actually available to bind with thyroid hormone receptors in target tissues.
-
How is the expression of iodothyronine selenodeiodinases characterized?
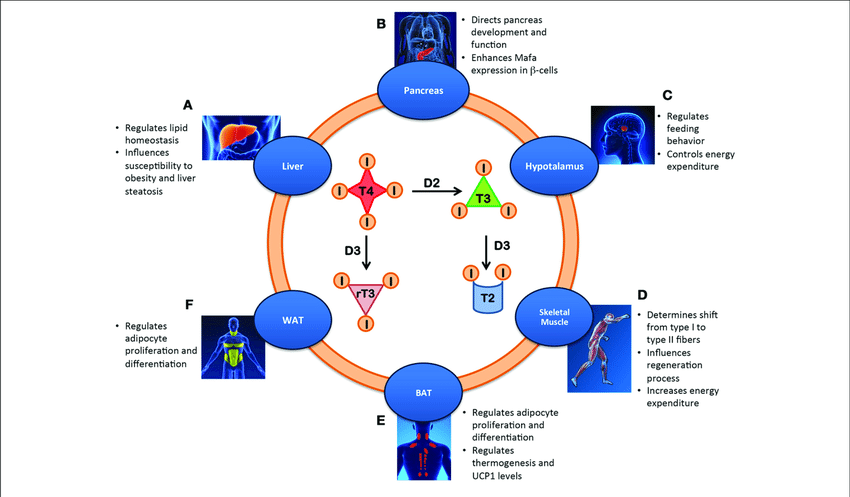
The expression of iodothyronine selenodeiodinases is tissue-specific.
-
What are T2 and rT3?
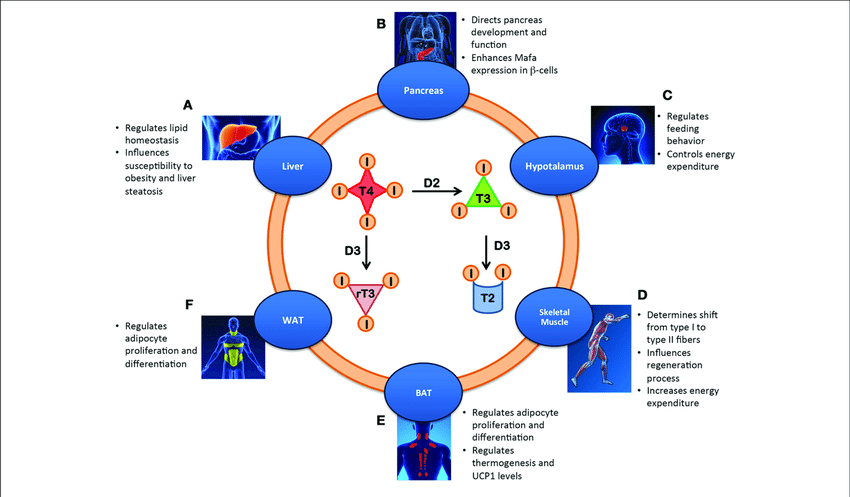
T2 and rT3 (reverse T3) are inactive metabolites of T3 and T4.
-
What was previously believed about the diffusion of thyroid hormones (TH) across the cell membrane?
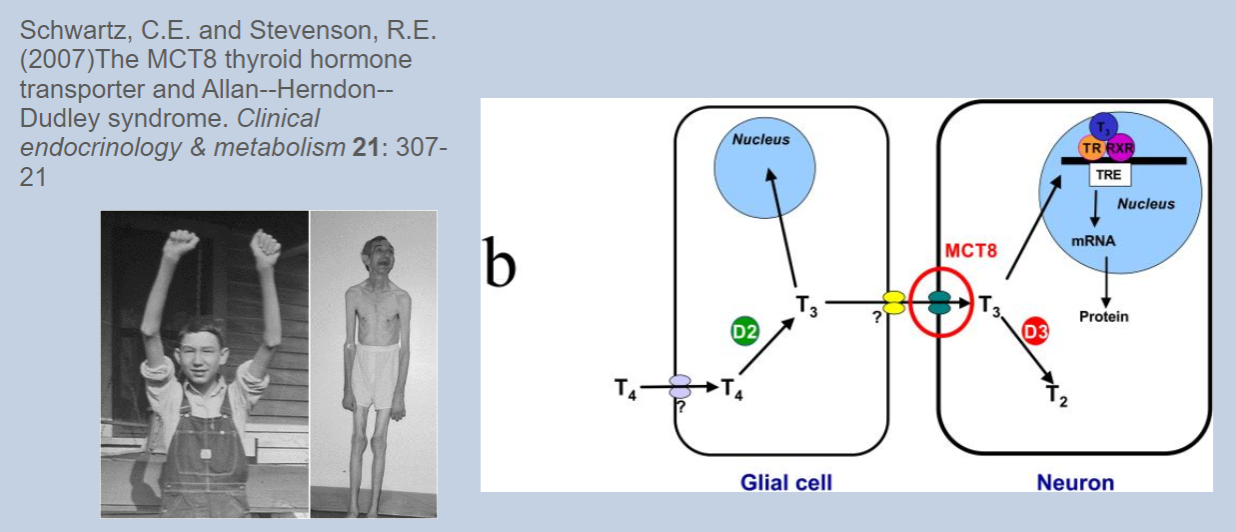
It was previously thought that thyroid hormones could freely diffuse across the cell membrane.
-
What is now known about the transport of thyroid hormones across the cell membrane?
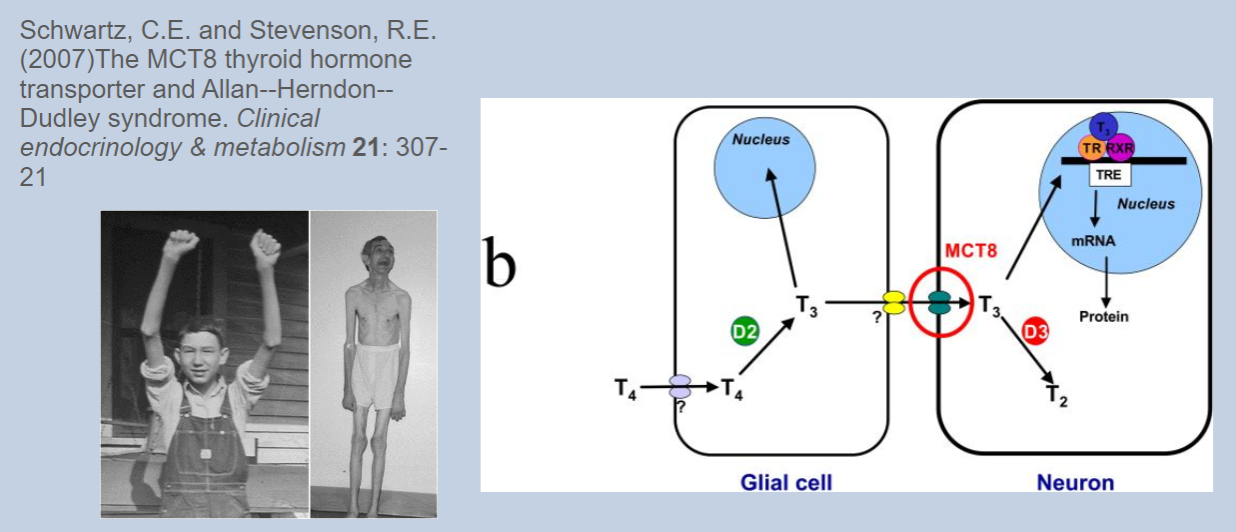
It is now known that transporters are required for thyroid hormones to cross the cell membrane.
-
Name two recently identified thyroid hormone transporters.
Two recently identified thyroid hormone transporters are MCT8 (monocarboxylate transporter 8) and OATP1C1 (organic anion transporting polypeptide 1C1).
-
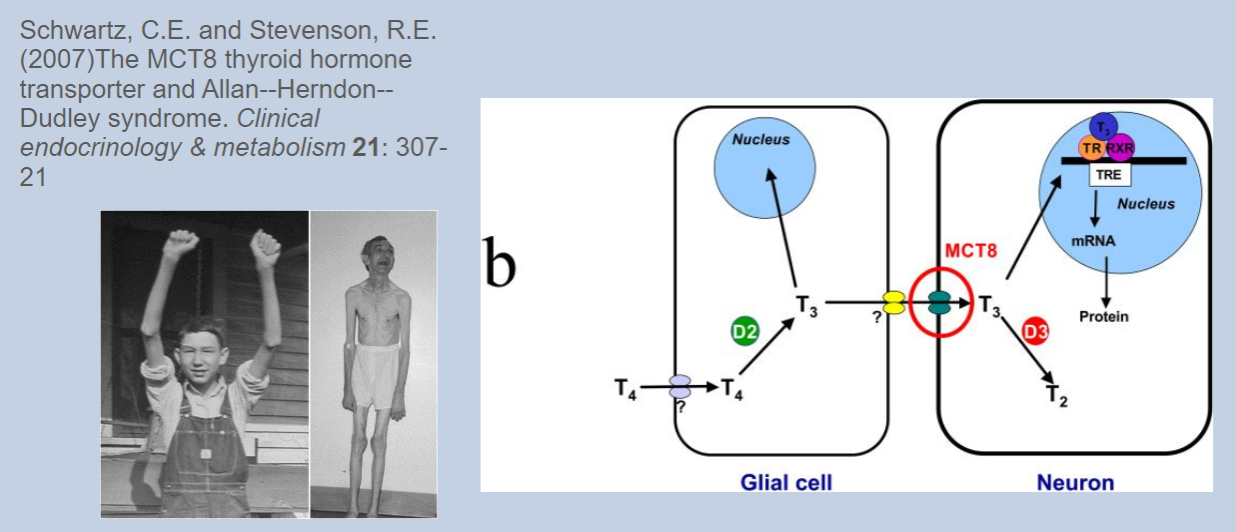
What condition is associated with mutations in the MCT8 gene?
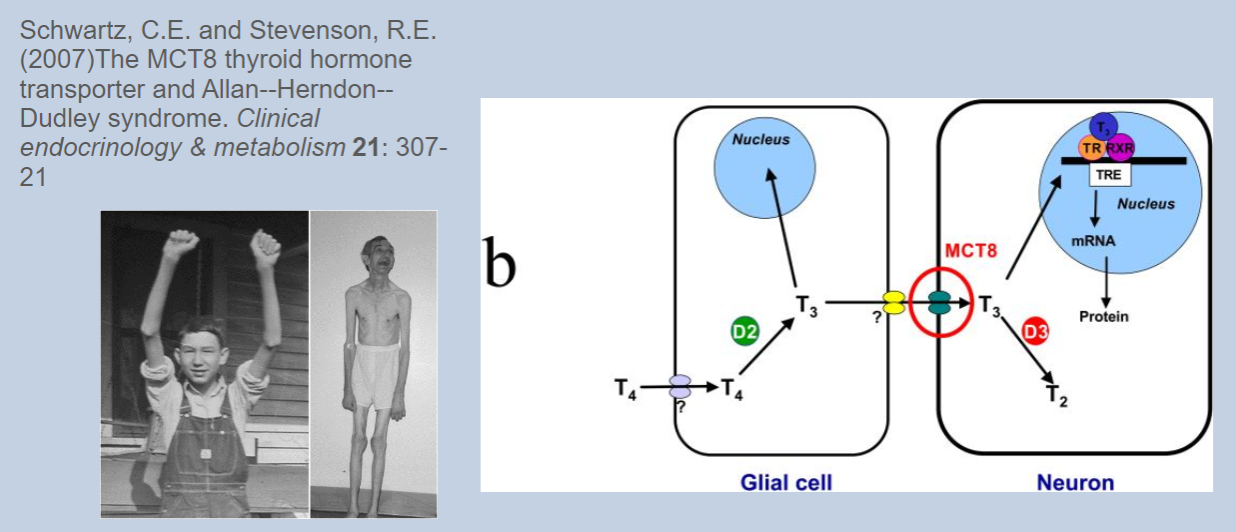
Mutations in the MCT8 gene are associated with Allan-Herndon-Dudley syndrome, an X-linked condition.
-
What are the symptoms of Allan-Herndon-Dudley syndrome?
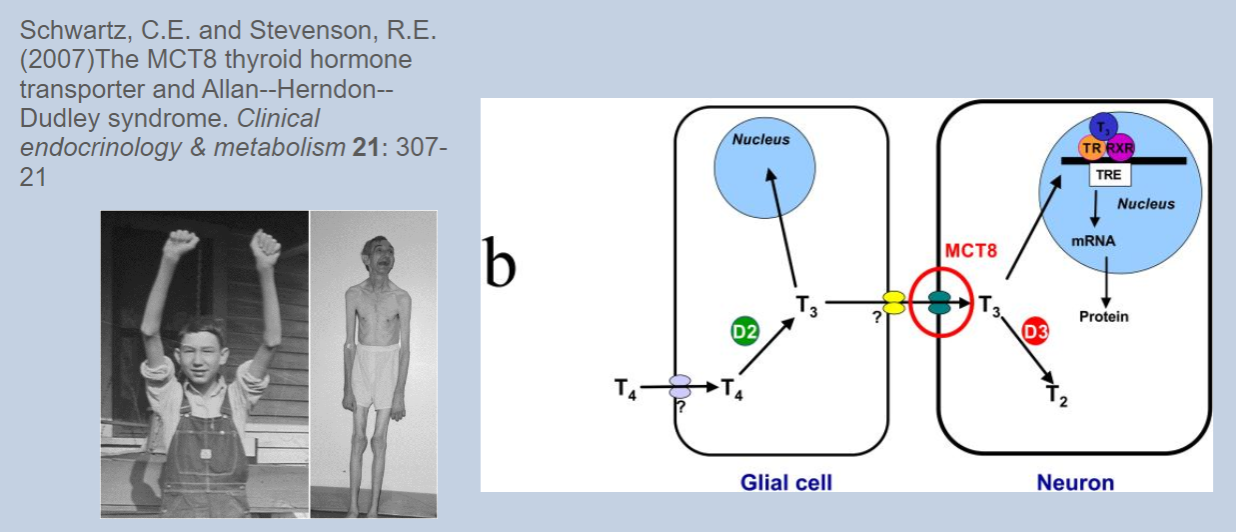
Allan-Herndon-Dudley syndrome is associated with psychomotor retardation.
-
How do thyroid hormones affect the metabolic rate?
Thyroid hormones increase the metabolic rate.
-
What cellular components are affected by thyroid hormones to increase metabolic rate?
Thyroid hormones increase the number and size of mitochondria, the activity of enzymes in the metabolic chain, and Na/K ATPase activity.
-
What effects do thyroid hormones have on the heart?
Thyroid hormones have positive inotropic (increasing force of contraction) and chronotropic (increasing heart rate) effects on the heart.
-
How do thyroid hormones interact with the sympathetic nervous system?
Thyroid hormones synergize with the sympathetic nervous system.
-
What role do thyroid hormones play in energy metabolism?
Thyroid hormones partially antagonize insulin signalling and promote gluconeogenesis and lipolysis.
-
What are the general developmental roles of thyroid hormones?
Thyroid hormones are essential for growth and development.
-
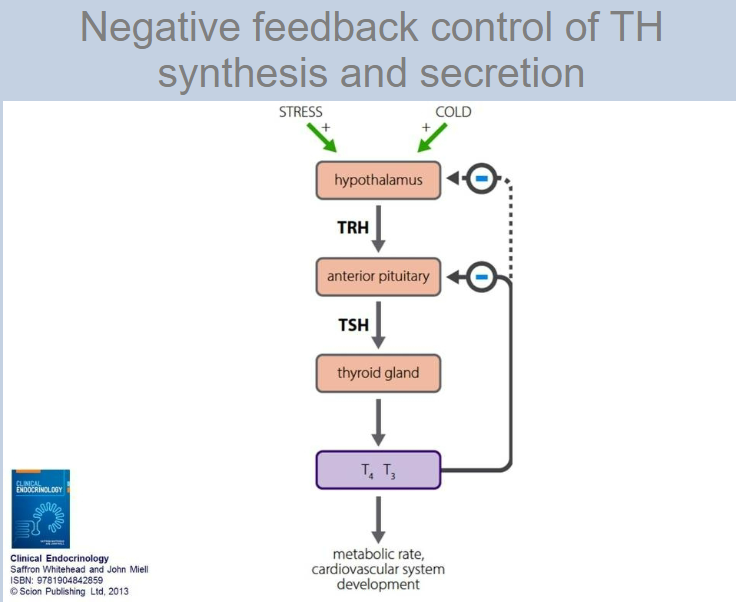
What type of control regulates thyroid hormone synthesis and secretion?
Negative feedback control regulates thyroid hormone synthesis and secretion via the hypothalamic-pituitary axis.
-
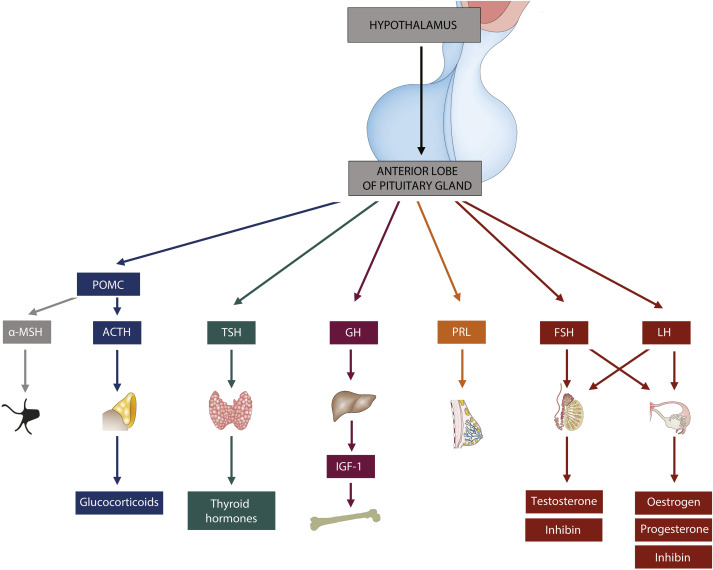
What do hypothalamic neurosecretory cells release to regulate thyroid hormone synthesis?
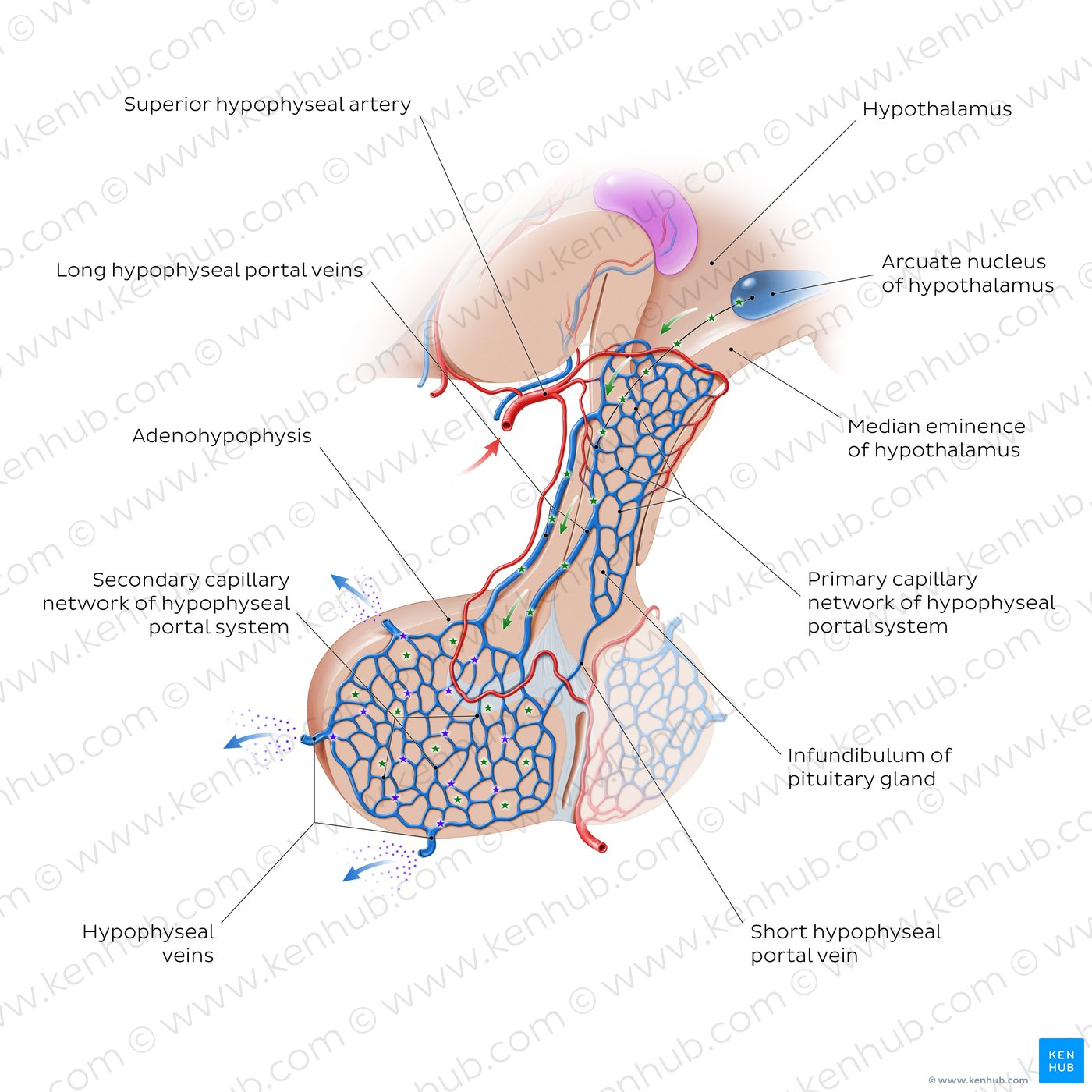
Hypothalamic neurosecretory cells release thyrotropin-releasing hormone (TRH) into the portal capillaries.
-
What effect does thyrotropin-releasing hormone (TRH) have on the anterior pituitary?
TRH stimulates thyrotrophs in the anterior pituitary to secrete thyroid-stimulating hormone (TSH).
-
What hormone does the anterior pituitary secrete in response to TRH, and what is its target?
The anterior pituitary secretes thyroid-stimulating hormone (TSH) in response to TRH, and its target is the thyroid gland.
-
How does negative feedback operate in the hypothalamic-pituitary-thyroid axis?
Increased levels of thyroid hormones (T3 and T4) inhibit the release of TRH from the hypothalamus and TSH from the anterior pituitary, reducing thyroid hormone production.
-
Picture demonstrating Negative feedback control of TH synthesis and secretion:
-
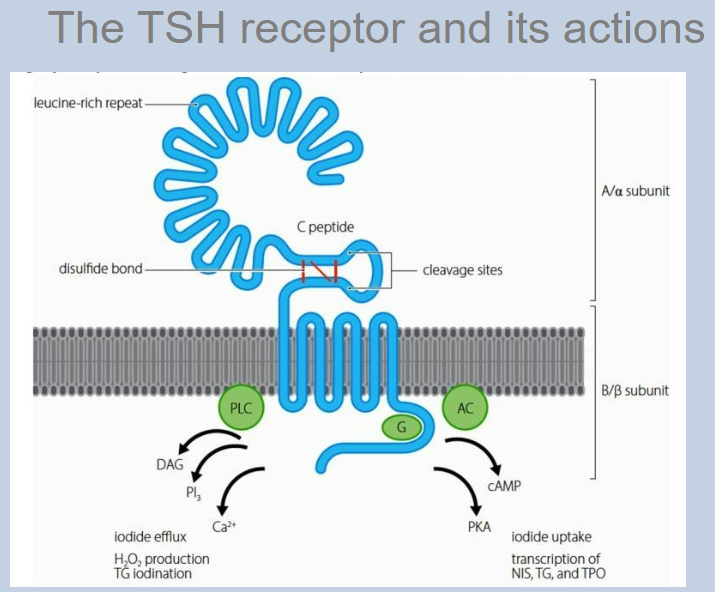
Picture demonstrating The TSH receptor and its actions:
-
What effect does TSH have on iodine uptake?
TSH increases iodine uptake by the thyroid gland.
-
How does TSH influence thyroid hormone synthesis?
TSH stimulates reactions involved in thyroid hormone synthesis, including the activity of thyroid peroxidase (TPO).
-
What is the role of TSH in relation to colloid in the thyroid gland?
TSH stimulates the uptake of colloid into the thyroid follicular cells.
-
How does TSH affect the growth of the thyroid gland?
TSH induces the growth of the thyroid gland, which can lead to the development of a goitre if overstimulated.
-
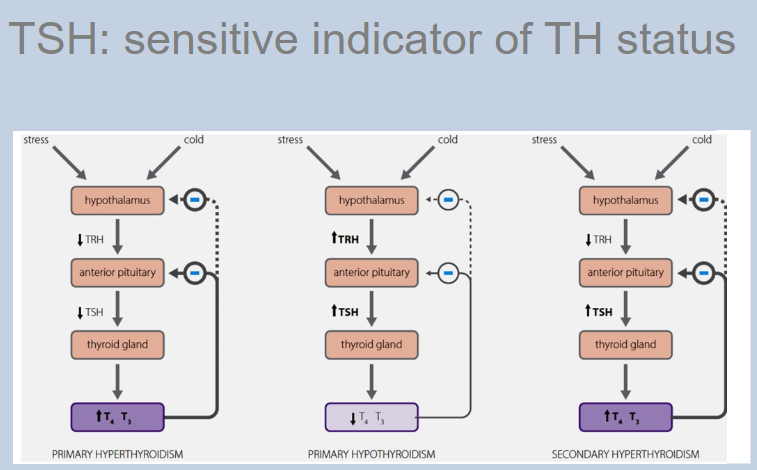
What does euthyroid mean?
Euthyroid refers to normal thyroid function.
-
What is hyperthyroidism?
Hyperthyroidism is the condition of having an excess of thyroid hormones (TH).
-
What is the primary cause of hyperthyroidism?
Primary hyperthyroidism is caused by a problem in the thyroid gland itself.
-
What is the secondary cause of hyperthyroidism?
Secondary hyperthyroidism is caused by a problem in the pituitary regulation of the thyroid gland.
-
What is hypothyroidism?
Hypothyroidism is the condition of having a deficiency of thyroid hormones (TH).
-
Picture demonstrating TSH: sensitive indicator of TH status:
-
What type of condition is Grave's disease?
Grave's disease is an autoimmune condition.
-
What are the levels of thyroid hormones (TH) and thyroid-stimulating hormone (TSH) in Grave's disease?
In Grave's disease, there are high circulating levels of thyroid hormones (TH) and low levels of thyroid-stimulating hormone (TSH).
-
What are some common symptoms of Grave's disease?
Common symptoms of Grave's disease include weight loss, tachycardia, and fatigue.
-
What physical sign is associated with Grave's disease due to TSH receptor stimulation?
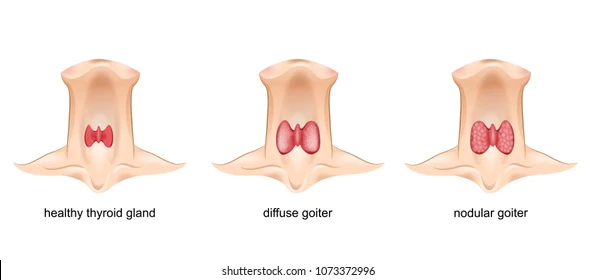
A diffuse goitre is associated with Grave's disease due to TSH receptor stimulation.
-
What is ophthalmopathy in the context of Grave's disease?
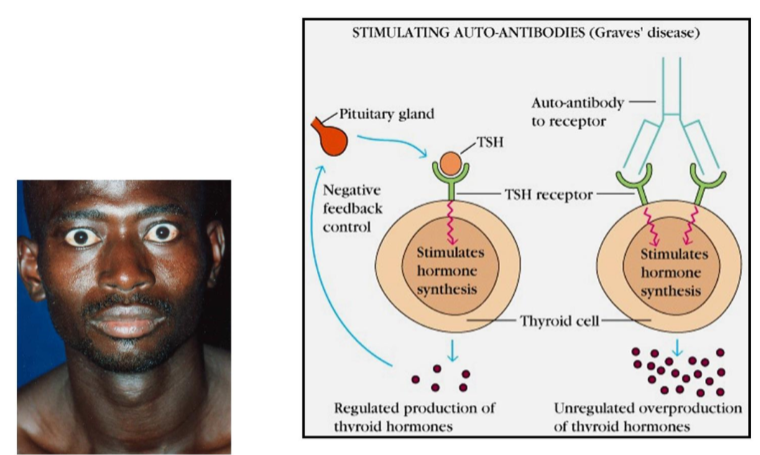
Ophthalmopathy in the context of Grave's disease refers to eye-related symptoms such as bulging eyes (exophthalmos) and other ocular abnormalities.
-
What type of condition is Hashimoto’s disease?

Hashimoto’s disease is an autoimmune condition.
-
What are the levels of thyroid hormones (TH) and thyroid-stimulating hormone (TSH) in Hashimoto’s disease?
In Hashimoto’s disease, there are low circulating levels of thyroid hormones (TH) and high levels of thyroid-stimulating hormone (TSH).
-
What are some common symptoms of Hashimoto’s disease?
Common symptoms of Hashimoto’s disease include lethargy, intolerance to cold, and lack of growth and development.
-
What physical sign is associated with Hashimoto’s disease?
A diffuse goitre is associated with Hashimoto’s disease.
-
How does Hashimoto’s disease affect growth and development?
Hashimoto’s disease can lead to a lack of growth and development due to thyroid hormone deficiency.

