The Menstrual Cycle (Physiology 2)
The Menstrual Cycle - Dr Suman Rice Lecture outline The menstrual cycle impacts on the lives of women on a daily basis and its normal functioning is essential for fertility. The normal physiology of the menstrual cycle involves integration and understanding of folliculogenesis and the HPG axis i.e. the production of sex steroid hormones, which feedback onto the hypothalamus and pituitary to alter production and secretion of GnRH and the gonadotrophins, to ultimately control the growth, development and ovulation of a mature oocyte capable of being fertilized. This lecture will also cover the formation of the corpus luteum which is necessary to support any eventual pregnancy. Desired Learning Outcomes By the end of this lecture unit, students should be able to: Describe the phases of the cycle and integrate folliculogenesis and oogenesis with these phases Understand the cyclical secretion of steroid hormones and how they control hypothalamic and pituitary hormone secretion by positive and negative feedback feed back Explain ovulation of the dominant follicle and reduction in and reduction in chromosome numbers to form a haploid egg ready for fertilization Discuss the formation of the corpus luteum and how its secretions prepares the uterus and tubes to receive a fertilized egg. Understand the demise of the corpus luteum and reinstatement of the next menstrual cycle. Analyse how the physiological features of the menstrual cycle can be used to predict ovulation for either family planning or contraception Session resources Download Download Downloadthe lecture slides. Session Activities Panopto recording (available after the session) Optional Additional Resources This is a clear summary of the menstrual cycleLinks to an external site. See below a 3D model of the female reproductive system Female Reproductive Organs-X SectionLinks to an external site. by Interactive ArtLinks to an external site. on SketchfabLinks to an external site. Essential Reproduction (2018) by Johnson M.H. 8th edition: Wiley-Blackwell (Links to an external site.) Glossary Follicular phase – the phase of the menstrual cycle associated with growth of the follicles and selection of the dominant follicle. It is characterised by oestrogen production. Ovulation – the release of a mature haploid oocyte from the dominant follicle in response to a surge in LH Luteal phase – the phase of the menstrual cycle associated with formation the corpus luteum after ovulation. It is characterised by progesterone production Dominant follicle – the follicle that is selected from the growing cohort of antral follicles to become the pre-ovulatory follicle and release a mature egg at ovulation Corpus luteum – the structure formed from the granulosa and theca cells of the follicle after ovulation, which is triggered by the surge in LH and causes luteinisation of the granulosa and theca cells. Menses – the shedding of the endometrial tissue lining along with blood Polar body – the small structure contains half the chromosomes after the completion of meiosis I.
-
What is the purpose of selecting a single oocyte during the menstrual cycle (2)?
The menstrual cycle selects one oocyte (egg) for ovulation, ensuring only one egg is released each cycle to optimize fertilization chances.
Follicles begin to develop, but only the dominant follicle continues to mature and releases the egg.
-
Why is it important for eggs to have the correct number of chromosomes (haploid) (2)?
The egg undergoes meiosis to reduce its chromosome number by half, ensuring it is haploid (23 chromosomes).
Upon fertilization, the egg combines with the sperm (haploid), creating a diploid zygote (46 chromosomes), restoring the full chromosome count.
-
What is the significance of regular spontaneous ovulation in the menstrual cycle (2)?
Ovulation must occur at the correct time to ensure it coincides with fertilization, improving the chances of pregnancy.
Regular ovulation ensures a predictable cycle and contributes to overall fertility.
-
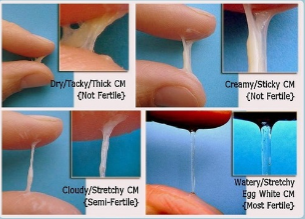
How do the vagina, cervix, and fallopian tubes undergo cyclical changes during the menstrual cycle (2)?
Vagina: Changes in secretions (usually acidic but during ovulation, the pH of vaginal secretions shifts to become more alkaline) to help sperm survival and motility.
Cervix: Cervical mucus becomes thinner and more slippery during ovulation, aiding sperm entry.
Fallopian Tubes: Become more active in capturing and transporting the egg for fertilization.
-
How does the uterus prepare for possible implantation of a fertilized egg (2)?
The endometrium (uterine lining) thickens in preparation for implantation.
Estrogen and progesterone work together to enhance blood flow, secretion, and nutrient supply to support a developing embryo.
-
How does the uterus support the fertilized and dividing egg after fertilization (2)?
The uterine lining provides nutrients, oxygen, and waste removal to support the growing embryo.
Early stages of pregnancy are supported by the corpus luteum, which secretes progesterone until the placenta forms and takes over.
-
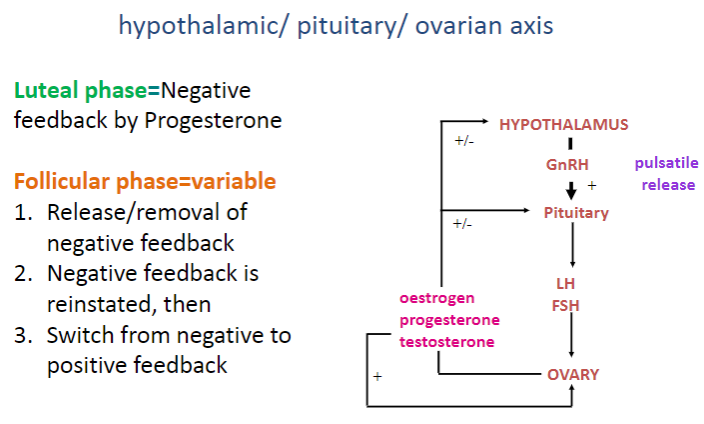
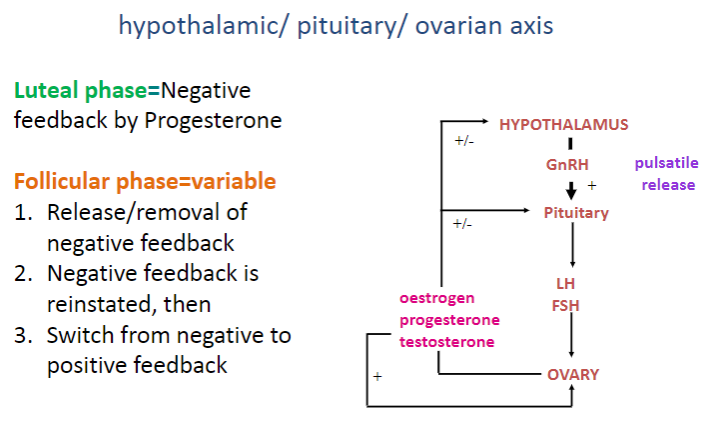
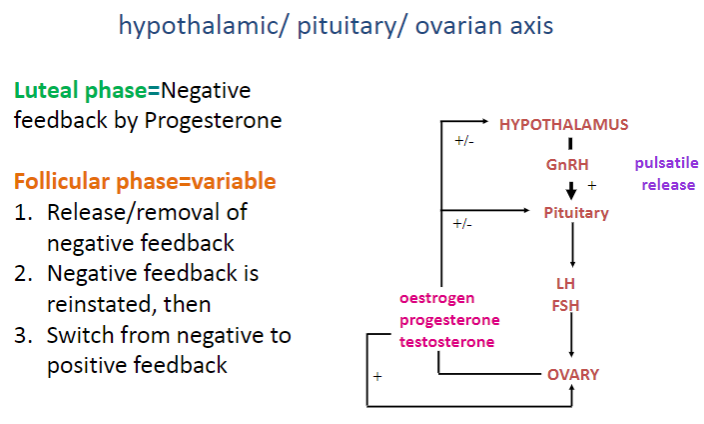
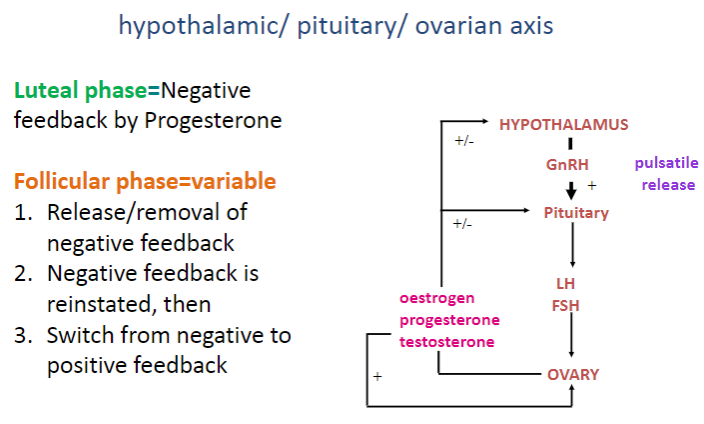
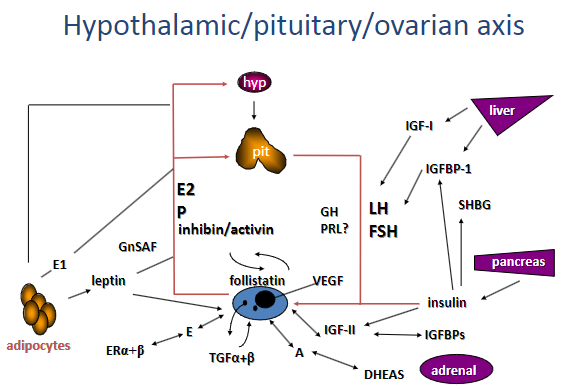
What is the role of the hypothalamus, anterior pituitary, and ovaries in controlling the menstrual cycle (3)?
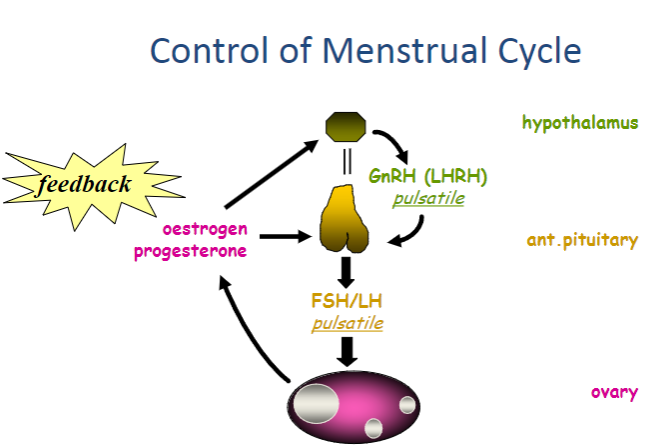
The hypothalamus releases GnRH (Gonadotropin-Releasing Hormone) in a pulsatile manner, which stimulates the anterior pituitary to release FSH and LH.
The anterior pituitary releases FSH and LH in response to GnRH, which regulate the growth of follicles and ovulation.
The ovaries produce oestrogen and progesterone, which influence the endometrium and provide feedback to regulate GnRH, FSH, and LH release.
-
How do GnRH, FSH, and LH work together to regulate the menstrual cycle (3)?
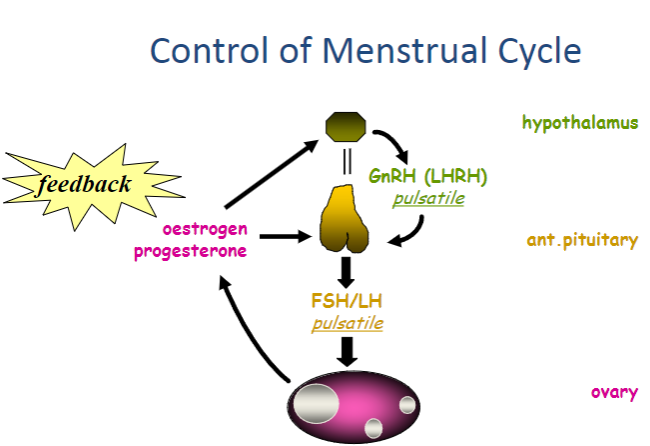
GnRH is released pulsatile from the hypothalamus, stimulating the anterior pituitary to release FSH and LH.
FSH promotes the maturation of follicles in the ovaries, while LH triggers ovulation, releasing the egg.
The pulsatile release of GnRH ensures the correct timing for FSH and LH secretion, crucial for follicle maturation and ovulation.
-
What is the role of oestrogen and progesterone in the menstrual cycle and how do feedback mechanisms affect the cycle (3)?
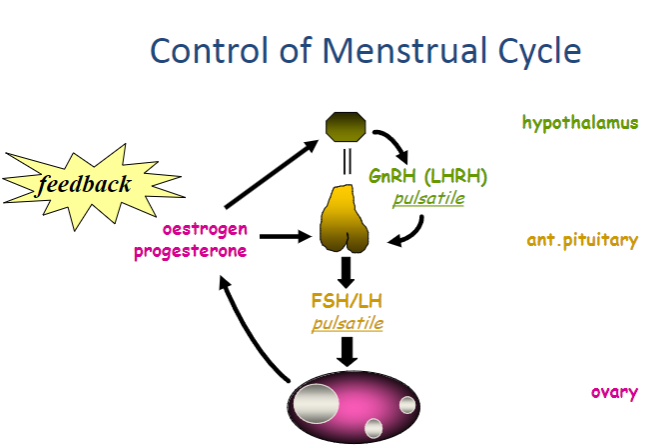
Oestrogen stimulates the growth of the endometrial lining and helps regulate FSH and LH release through feedback.
Progesterone prepares the endometrium for implantation and maintains the early stages of pregnancy if fertilization occurs.
Both oestrogen and progesterone provide feedback to the hypothalamus and anterior pituitary, controlling the release of GnRH, FSH, and LH to ensure the cycle progresses correctly.
-
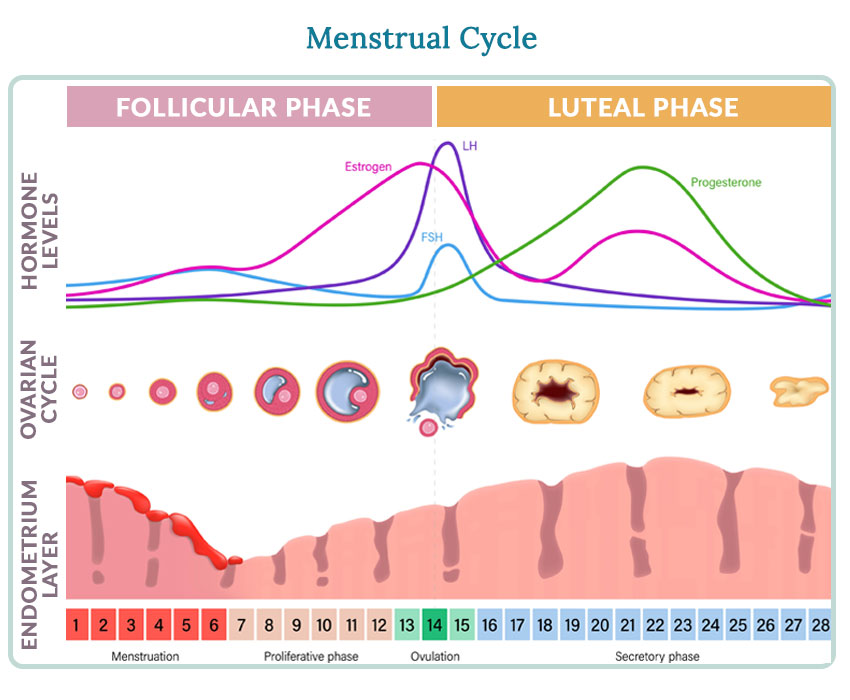
What happens during the follicular phase of the menstrual cycle (3)?
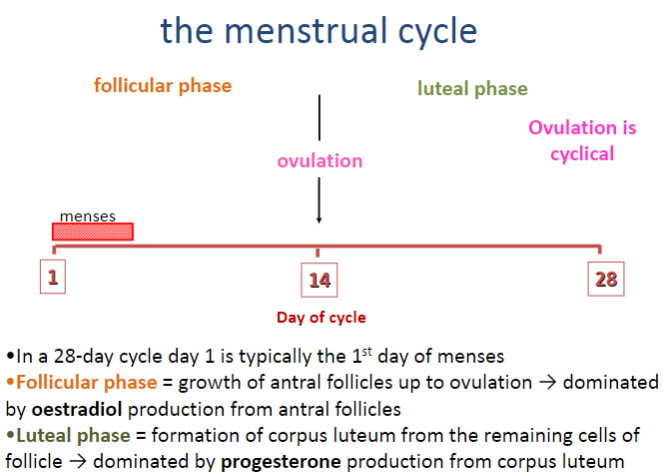
The follicular phase involves the growth of antral follicles up to ovulation.
It is dominated by the production of oestradiol from the antral follicles.
This phase begins on day 1 of the cycle (first day of menses) and continues until ovulation.
-
What occurs during the luteal phase of the menstrual cycle (3)?
The luteal phase begins after ovulation and involves the formation of the corpus luteum from the remaining cells of the follicle.
It is dominated by progesterone production from the corpus luteum.
This phase prepares the uterus for possible implantation and supports early pregnancy if fertilization occurs.
-
What is ovulation and how does it relate to the menstrual cycle (2)?
Ovulation is the release of the mature egg from the dominant follicle, occurring around the middle of the menstrual cycle.
It is a cyclical process, typically occurring around day 14 in a 28-day cycle, marking the transition between the follicular and luteal phases.
-
What are the two phases of the menstrual cycle and how are they separated (2)?
The menstrual cycle has two phases: the follicular phase and the luteal phase.
Ovulation occurs between these phases, marking the transition from follicular to luteal.
-
What happens on day 1 of the menstrual cycle and during the follicular phase (3)?
Day 1 of the menstrual cycle is the first day of bleeding (menses).
The next 14 days are the follicular phase, during which antral follicles grow and mature.
This phase is dominated by the production of oestradiol from the developing follicles.
-
What occurs during ovulation and the transition to the luteal phase (3)?
Ovulation occurs at the end of the follicular phase (around the middle of the cycle), releasing the mature egg.
After ovulation, the remnant of the follicle becomes the corpus luteum.
The luteal phase, lasting the next 14 days, is dominated by progesterone production from the corpus luteum.
-
What happens at the end of the luteal phase if there is no pregnancy (2)?
If pregnancy does not occur, menstruation follows at the end of the luteal phase.
The corpus luteum degenerates, leading to a drop in progesterone levels, which triggers the shedding of the endometrial lining.
-
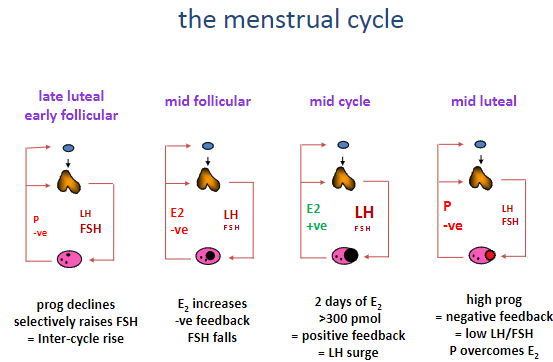
Picture demonstrating the menstrual cycle:
-
What is the inter-cycle rise in FSH and why is it important? (2)
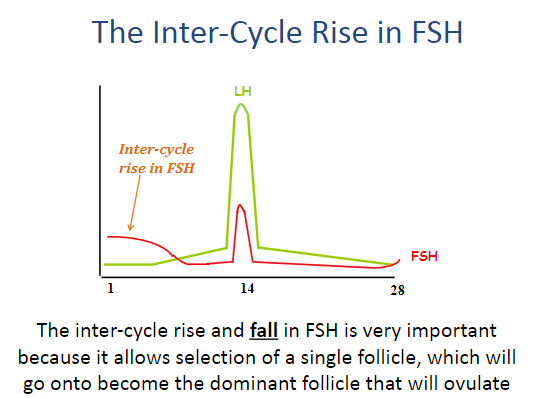
The inter-cycle rise and fall in FSH is crucial for the selection of a single follicle.
This follicle will go on to become the dominant follicle that will ovulate.
-
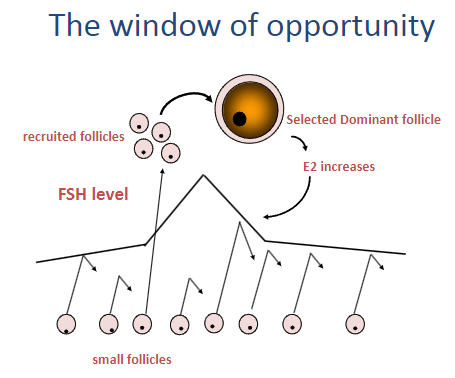
What happens during the selection of the dominant follicle? (3)
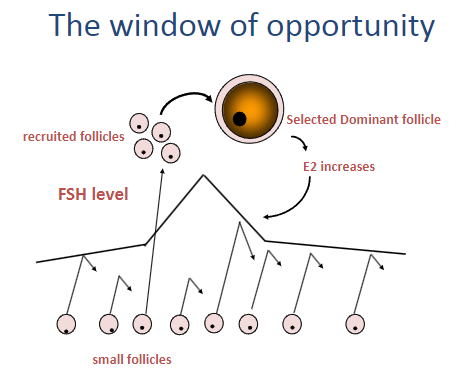
A group of recruited follicles begin to grow, but only one becomes the dominant follicle.
As the dominant follicle develops, estrogen (E2) levels increase.
The increase in E2 helps create a "window of opportunity" where the dominant follicle is selected, while smaller follicles are inhibited by low FSH levels.
-
How does the dominant follicle survive the fall in FSH levels? (2)
The dominant follicle has acquired enough sensitivity to FSH that it can continue growing even as FSH levels decline.
The rising levels of oestradiol from the dominant follicle help maintain its growth and survival, despite the reduced FSH.
-
What is the process of follicle selection and how does it occur? (4)
Raised FSH levels create a "window" of opportunity to recruit antral follicles that are at the appropriate stage for further growth.
According to the FSH threshold hypothesis, one follicle from the group of antral follicles is at the right stage to survive the decline in FSH.
This follicle becomes the dominant follicle (DF) and will eventually ovulate.
Oestradiol levels rise from the dominant follicle, which reinstates negative feedback at the pituitary, causing FSH levels to fall and preventing further follicle growth.
-
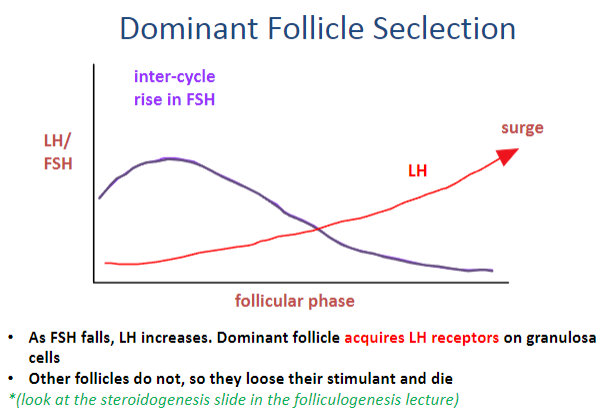
How does the dominant follicle survive and become selected during the menstrual cycle? (4)
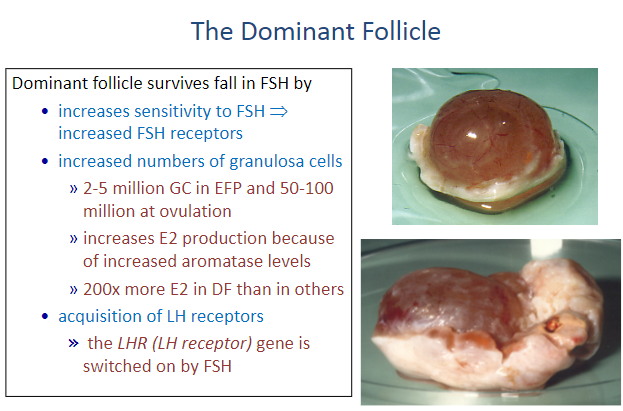
During the inter-cycle, there is an initial rise in FSH, followed by a surge in LH, which plays a key role in follicle selection.
As FSH levels fall, LH levels increase.
The dominant follicle acquires LH receptors on its granulosa cells, enabling it to continue growing.
Other follicles that do not acquire LH receptors lose their stimulatory signal and undergo atresia (cell death).
-
How does the dominant follicle survive the fall in FSH and continue to develop? (4)
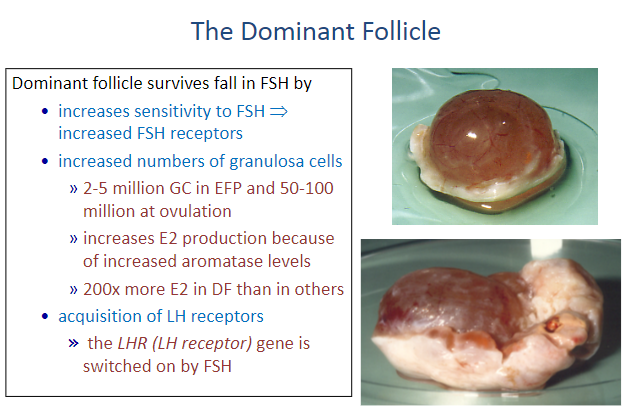
The dominant follicle increases its sensitivity to FSH by upregulating FSH receptors on granulosa cells.
It also increases the number of granulosa cells, from 2-5 million at early follicular phase (EFP) to 50-100 million at ovulation.
The increase in granulosa cells results in a higher production of estradiol (E2) due to elevated aromatase levels, making the dominant follicle produce 200x more E2 than other follicles.
The dominant follicle acquires LH receptors, which are activated by FSH, enabling it to respond to the upcoming LH surge.
-
What is the steroidogenesis pathway in the dominant follicle (DF)? (5)
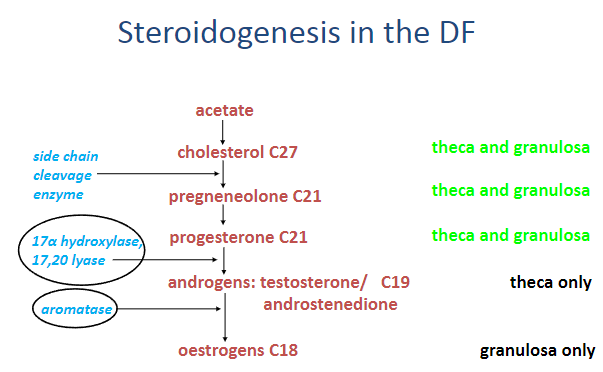
Acetate is the precursor molecule used to produce cholesterol (C27).
Cholesterol (C27) is converted to pregnenolone (C21).
Pregnenolone (C21) is then converted to progesterone (C21).
In the theca cells, androgens such as testosterone (C19) and androstenedione (C19) are produced.
In the granulosa cells, estrogens (C18) are synthesized, primarily through the conversion of androgens.
-
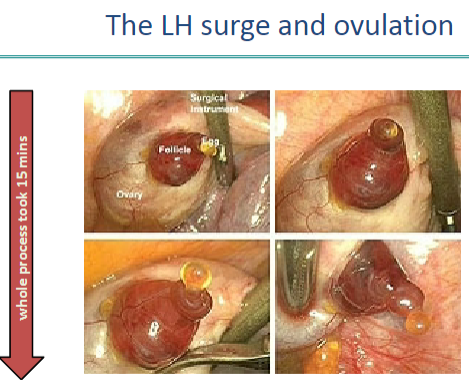
What triggers the LH surge and what are its effects? (5)
E2 feedback switches from negative to positive after 48 hours of elevated E2 levels (>300pM).
Causes a massive release of LH from the pituitary with an exponential rise in LH serum levels.
Triggers ovulation cascade, leading to the release of the egg.
Induces luteinisation, forming the corpus luteum (composed of luteinised granulosa and theca cells).
Results in a fall in E2 production but stimulates progesterone (P) production, which dominates.
-
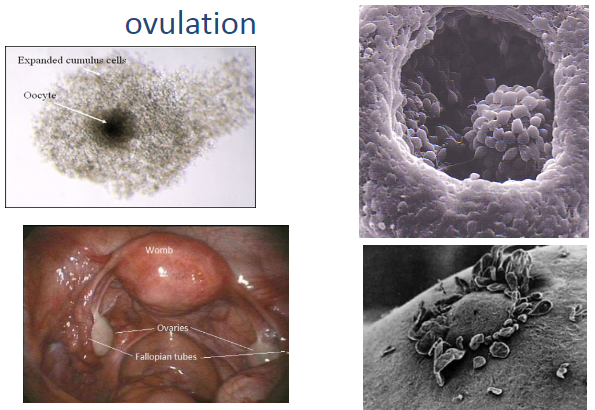
What occurs during ovulation? (4)
Blood flow to the follicle increases, forming an apex or stigma on the ovary wall.
Proteases and inflammatory mediators are locally released.
Enzymatic breakdown of the ovary wall proteins occurs.
12-18 hours after the LH peak, the follicle wall is digested, and the cumulus-oocyte complex (COC) is released.
-
What happens to the oocyte during and after ovulation? (4)
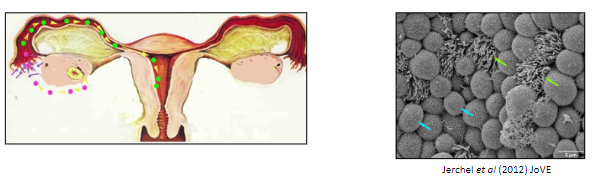
The oocyte with cumulus cells is extruded from the ovary.
Follicular fluid may flow into the Pouch of Douglas.
The egg is collected by the fimbriae of the uterine (Fallopian) tube.
The egg progresses down the tube via peristalsis and the action of cilia.
-
Picture demonstrating the process of ovulation:
-
Picture demonstrating the LH surge and ovulation:
-
What occurs during meiosis and extrusion of the polar body in the oocyte? (5)

LH surge triggers the nucleus of the oocyte in the dominant follicle to complete the first meiotic division.
Half of the chromosomes are packaged into the first polar body, a small structure within the egg.
The egg, retaining most of the cytoplasm, becomes a secondary oocyte.
The first polar body does not divide further and has no further role in the process.
The oocyte begins the second meiotic division but arrests again.
-
What are the key features of the secondary oocyte? (4)
Only one oocyte is produced, unlike multiple sperm.
The largest cell in the body (sperm are the smallest but fastest).
Must support early embryonic divisions until the embryo attaches to the placenta.
Spends 2-3 days in the uterine tube, potentially encountering sperm.
-
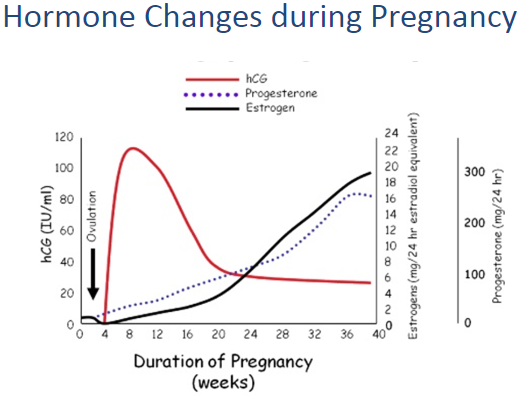
How is the corpus luteum formed, and what is its function? (5)
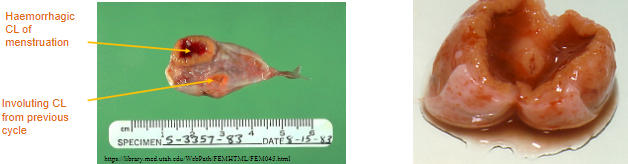
After ovulation, the follicle collapses, forming the corpus luteum ("yellow body").
Progesterone production increases significantly, along with some estradiol (E2).
The corpus luteum contains numerous LH receptors, allowing it to function even with low LH levels.
If pregnancy occurs, hCG from the syncytiotrophoblast binds to LH receptors to maintain the corpus luteum.
The corpus luteum is essential for early pregnancy support through hormone production.
-
Picture demonstrating hormone changes during pregnancy:
-
What are the secretions of the corpus luteum and their functions? (5)
Progesterone:
Supports the oocyte during its journey.
Maintains the corpus luteum.
Prepares the endometrium for potential implantation.
Controls cellular activity in the Fallopian tubes.
Alters cervical secretions.
Estradiol (E2):
Essential for maintaining the endometrium.
-
What happens if fertilization does not occur? (5)
The corpus luteum has a finite lifespan of 14 days.
Its removal is necessary to initiate a new cycle.
Cell death occurs, leading to the breakdown of vasculature.
The corpus luteum shrinks during this process.
The mechanism for the corpus luteum's demise is not well understood.
-
What is the role of feedback mechanisms in hormonal regulation? (3)
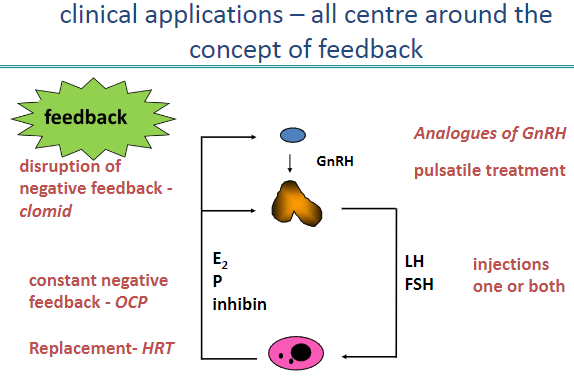
Feedback involves regulation of hormone levels such as E2 (oestradiol), P (progesterone), inhibin, LH, FSH, and GnRH.
It is central to controlling the menstrual cycle and fertility.
Clinical applications often target these feedback loops for therapeutic purposes.
-
How do GnRH analogues function in clinical treatments? (2)
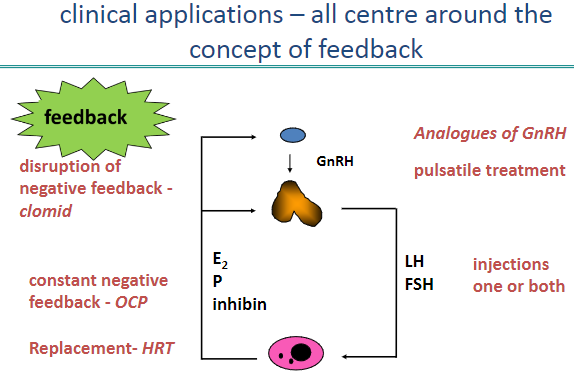
GnRH analogues can be used in two ways: pulsatile treatment or constant suppression.
Pulsatile treatment stimulates LH and FSH production, aiding in infertility treatment.
-
What are some clinical applications involving the disruption of negative feedback? (3)
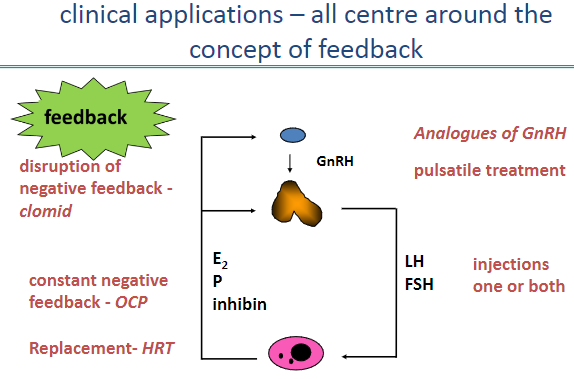
Clomiphene (Clomid) disrupts negative feedback, increasing GnRH secretion to stimulate ovulation.
Constant suppression of feedback, as with oral contraceptive pills (OCP), prevents ovulation.
Negative feedback control can be tailored to either stimulate or suppress hormone production.
-
What is the purpose of hormone replacement therapy (HRT)? (2)
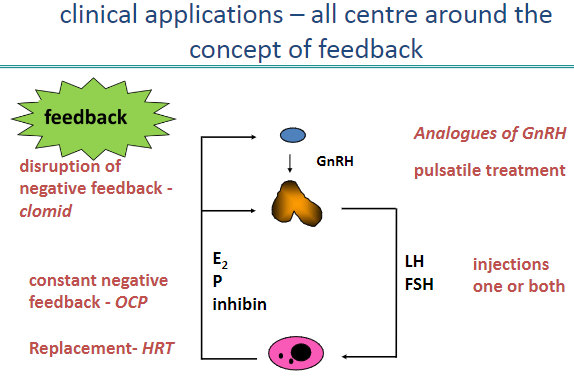
HRT replaces hormones like E2 and P to alleviate symptoms of menopause.
It can also support the endometrium in women with hormonal deficiencies.
-
Picture demonstrating hypothalamic/pituitary/ovarian axis:
-
What are the two phases of the menstrual cycle, and how do their durations differ? (2)
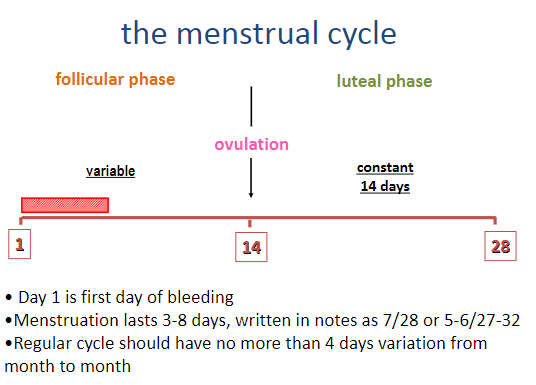
Follicular phase: Variable in length.
Luteal phase: Constant, lasting 14 days.
-
What marks the start of the menstrual cycle, and how long does menstruation last? (3)
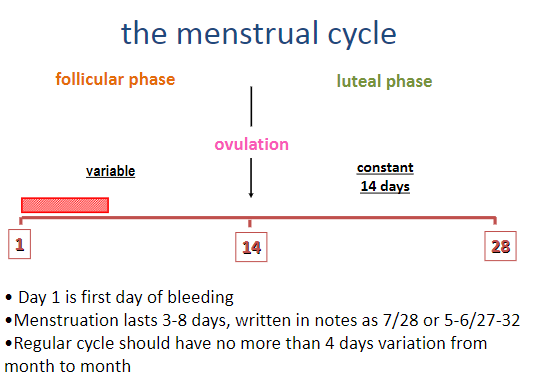
Day 1 is the first day of bleeding.
Menstruation lasts 3–8 days.
Written in notes as 7/28 or 5–6/27–32.
-
How is a regular menstrual cycle characterized in terms of variation? (1)
Regular cycles should have no more than 4 days of variation from month to month.
-
How can a patient determine when they are going to ovulate if their cycles are regular? (1)
It is easy to predict ovulation with regular cycles.
-
How can a patient determine when they are going to ovulate if their cycles are irregular? (3)
Tracking ovulation with ultrasound monitoring: This method can be used to observe follicle development and predict ovulation, especially when undergoing ovulation induction.
Using ovulation predictor kits (OPKs): These kits detect hormone surges (like LH), which typically precede ovulation.
Having regular intercourse: Engaging in intercourse three times per week ensures sperm will be present around the time of ovulation, even if it's not precisely predicted.
-
If a woman has a 32-day cycle, on what day will she ovulate? (1)
She will ovulate on Day 18.
-
What are the signs of ovulation? (5)
A slight rise in basal body temperature, typically 0.5 to 1 degree
Tender breasts
Abdominal bloating
Light spotting
Changes in cervical mucus
-
What is the purpose of tracking basal body temperature for ovulation? (2)
To identify the slight rise in temperature (0.5 to 1 degree)
To track ovulation from day 1 of the last menstrual period (LMP)
-
What might cause slight pain or ache on one side of the abdomen during ovulation? (1)
Ovulation-related discomfort, often due to the release of an egg from the ovary
-
What is the fertile period and what factors affect it? (4)
The fertile period spans 6 days.
Lifespan of the egg: Up to 24 hours after ovulation.
Lifespan of sperm: Median survival is 1.5 days, but sperm can survive up to 5 days in sperm-supportive mucus.
Sperm survival is dependent on the type and quantity of cervical mucus, and the quality of the sperm.
-
What is E3G and how does it relate to ovulation prediction? (2)
E3G is a urinary metabolite of oestradiol.
It allows women to identify days of high fertility leading up to ovulation.
-
What is the cost and quantity of ovulation prediction kits? (1)
£25 for 20 tests.
-
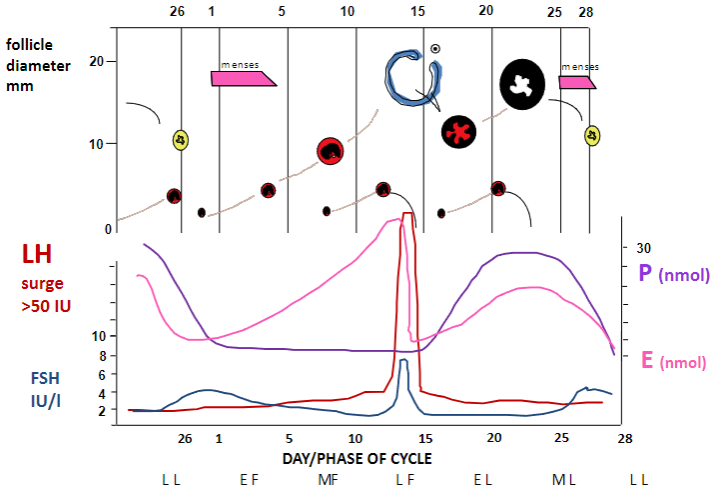
Picture demonstrating follicle diameter and the days of the cycle:
-
What are the key points to remember about hormone changes during the menstrual cycle? (4)
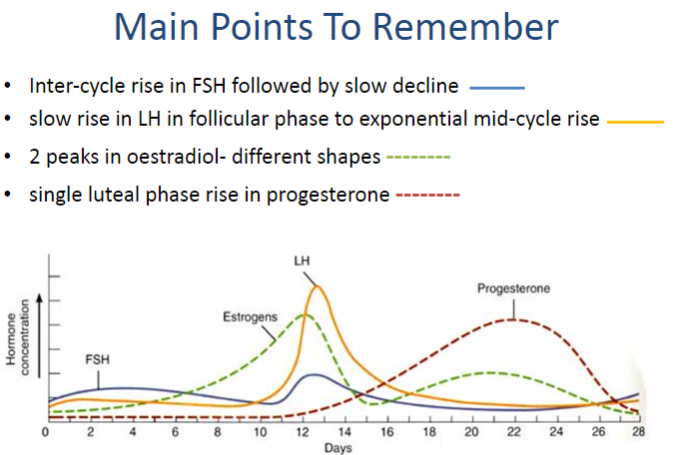
Inter-cycle rise in FSH followed by slow decline.
Slow rise in LH during the follicular phase, followed by an exponential mid-cycle rise.
Two peaks in oestradiol with different shapes.
Single luteal phase rise in progesterone.
-
What is the follicular phase of the menstrual cycle? (2)
The follicular phase is associated with the growth of follicles and the selection of the dominant follicle.
It is characterized by oestrogen production.
-
What is ovulation and what triggers it? (2)
Ovulation is the release of a mature haploid oocyte from the dominant follicle.
It occurs in response to a surge in LH.
-
What is the luteal phase of the menstrual cycle? (2)
The luteal phase is associated with the formation of the corpus luteum after ovulation.
It is characterized by progesterone production.
-
What is the dominant follicle? (1)
The dominant follicle is the follicle selected from the growing cohort of antral follicles to become the pre-ovulatory follicle and release a mature egg at ovulation.
-
What is the corpus luteum and how is it formed? (2)
The corpus luteum is formed from the granulosa and theca cells of the follicle after ovulation.
Its formation is triggered by the surge in LH and causes luteinisation of the granulosa and theca cells.
-
What is menses? (1)
Menses is the shedding of the endometrial tissue lining along with blood.
-
What is the polar body? (1)
The polar body is a small structure that contains half the chromosomes after the completion of meiosis I.

