The Mechanics of Breathing (Physiology)
Session summary This session continues the discussion of the mechanisms and physiological factors involved in breathing. Topics discussed include airway resistance, lung compliance, and the role of pulmonary surfactant, as well as specific clinical conditions where these aspects of lung function are adversely affected. Learning Outcomes Define airway resistance and explain how and why it affected by respiratory diseases. Define lung compliance and explain how and why it is affected by respiratory diseases. Describe the role of pulmonary surfactant in respiration and pathology that occurs if insufficient quantities are produced.
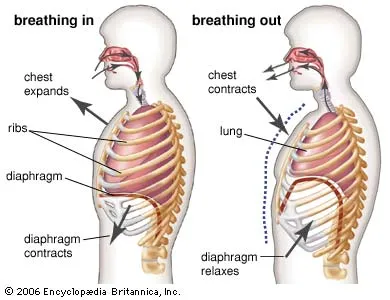
-
What is airway resistance?
Airway resistance is the opposition encountered by airflow as it moves through the airways.
-
How does airway resistance affect airflow?
Increased airway resistance leads to decreased airflow, while decreased resistance leads to increased airflow.
-
What factors determine the level of airway resistance?
The level of airway resistance is determined by factors such as the diameter of the airways, the length of the airways, the viscosity of the air, and the density of the air.
-
What happens to airflow when the pressure gradient (ΔP) increases?
When the pressure gradient increases, airflow increases.
-
How is airflow affected by increased resistance?
Increased resistance leads to decreased airflow.
-
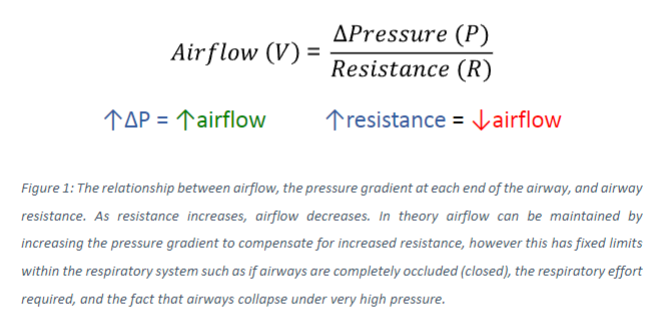
What is the formula for Airflow that includes resistance?
-
What happens to airflow as resistance increases?
As resistance increases, airflow decreases.
-
How can the decrease in airflow due to increased resistance be somewhat overcome?
The decrease in airflow due to increased resistance can be somewhat overcome by increasing the pressure difference between the two ends of the conduit.
-
What are the specific physical limitations within the respiratory system in overcoming increased resistance?
The effort or force required to increase the pressure difference may not be able to be generated, or the airway might be completely obstructed, leading to limitations in overcoming increased resistance.
-
What factors determine the level of airway resistance?
The level of airway resistance is determined by factors such as the diameter of the airways, the length of the airways, the viscosity of the air, and the density of the air.
-
What are the major variable factors within the airways?
The major variable factors within the airways are the cross-sectional area of the airway lumen and the airflow pattern.
-
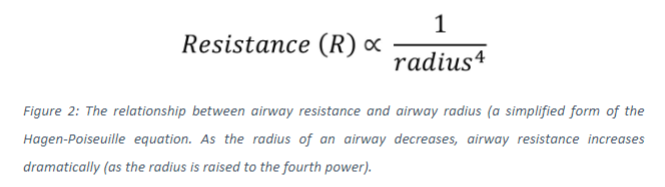
What does the Hagen-Poiseuille equation describe?
The Hagen-Poiseuille equation describes the relationship between resistance and various properties of airways and airflow.
-
What does the Hagen-Poiseuille equation show about the relationship between airway resistance and the cross-sectional radius?
The Hagen-Poiseuille equation demonstrates that the resistance of a gas flowing through a pipe is inversely proportional to the cross-sectional radius raised to the power 4.
-
How does a change in airway radius affect resistance and airflow?
A relatively small decrease in radius results in a large increase in resistance and a dramatic decrease in airflow. For example, if the airway radius is halved, airway resistance increases by a factor of 16, accompanied by a resulting proportional decrease in airflow.
-
Picture demonstrating the relationship between airway resistance and airway radius
-
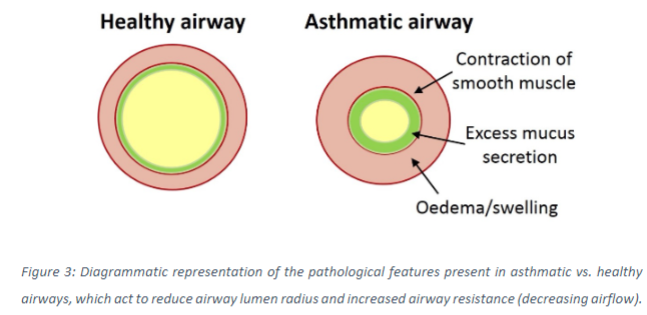
What pathological features of respiratory diseases impact the cross-sectional area of the airway lumen?
Contraction of airway smooth muscle, excessive mucus secretion, edema/swelling of the airway tissue, and damage to the integrity of the airway structure (loss of patency) all reduce the size of the airway lumen.
-
How do these pathological features affect airway resistance and airflow?
These pathological features increase airway resistance and decrease airflow by reducing the cross-sectional area of the airway lumen.
-
Picture demonstrating the pathological features in asthmatic vs healthy airways:
-
What is the second major factor that can increase airway resistance by negatively impacting airflow?
The pattern of airflow can increase airway resistance, particularly when airflow changes from a linear to a turbulent pattern.
-
When does turbulence occur in airflow?
Turbulence occurs when high velocities of airflow are achieved, such as during forced breathing maneuvers, or if there is a sudden decrease in luminal area, such as in obstructed airways.
-
What is responsible for the wheezing sound produced in patients with obstructed airways?
The vibration generated by turbulent airflow is responsible for the wheezing sound produced in patients with obstructed airways.
-
Picture demonstrating the effect of airway obstruction on flow pattern:
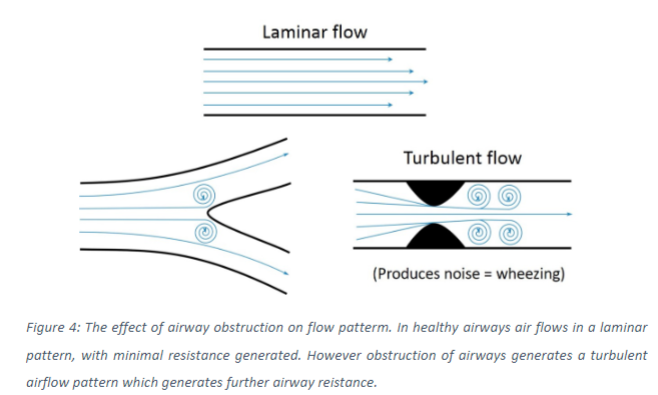
-
What is airway patency?
Airway patency refers to the state of being open or unobstructed. A loss of patency results in closing or obstruction of the airways.
-
How is the open structure of the airways maintained?
The open structure of the airways is maintained by elastic fibers within the airway wall and radial traction, which is the pulling force exerted on the airways by the surrounding lung tissue.
-
How does lung expansion during inspiration affect airway patency?
During inspiration, as the lungs expand, the lung tissue and airways contained within are stretched open.
-
Why is airway obstruction more noticeable during expiration?
Airway obstruction is often more noticeable during expiration because during expiration, the lung tissue and airways are compressed.
-
How can positive intrapleural pressure affect airway patency during forced expirations?
Positive intrapleural pressure during forced expirations can exert a collapsing force onto the airways, potentially reducing airway patency.
-
What is lung compliance?
Lung compliance refers to how much force is required to expand the lungs.
-
How is transpulmonary pressure related to lung expansion or compression?
Transpulmonary pressure, calculated as the difference between alveolar pressure and intrapleural pressure, determines the level of force acting to expand (if positive) or compress (if negative) the lungs.
-
What is lung compliance?
Lung compliance describes how easily the lungs can be distended or expanded in response to changes in transpulmonary pressure.
-
How does lung compliance relate to the change in lung volume produced by a specific change in transpulmonary pressure?
Lung compliance describes the relationship between the change in lung volume and the change in transpulmonary pressure. Higher lung compliance means that less expansive force is required to inflate the lungs, resulting in a greater volume change per transpulmonary pressure change. Lower lung compliance means that more expansive force is required to inflate the lungs, resulting in a smaller volume change per transpulmonary pressure change.
-
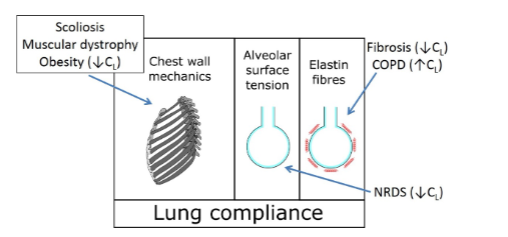
What factors can affect lung compliance?
Lung compliance can be affected by changes in the structure of lung tissue, particularly the density of elastic and structural fibers such as elastin and collagen.
-
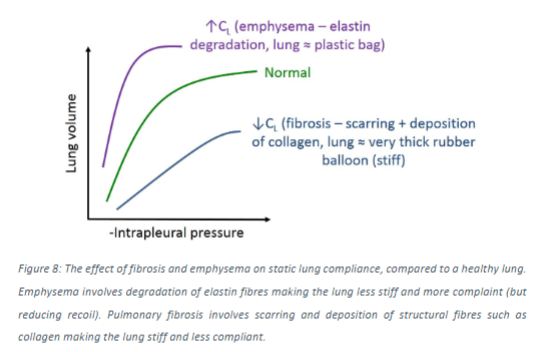
How is lung compliance represented on volume-pressure curves?
Lung compliance is represented by the gradient or slope of volume-pressure curves. Higher lung compliance is indicated by a greater (steeper) gradient, while lower lung compliance is indicated by a lower (shallower/less steep) gradient.
-
What is the formula for lung compliance that relates to pressure:
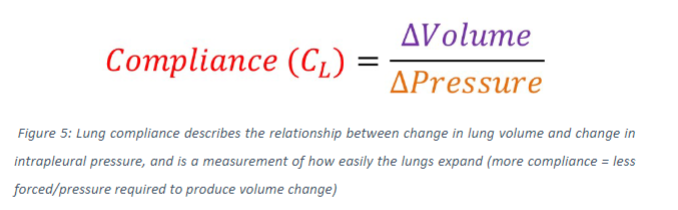
-
How is lung compliance represented graphically?
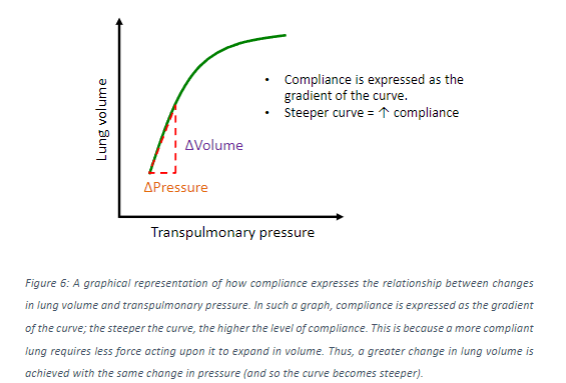
Lung compliance is represented by the gradient or slope of the curve on a graph of lung volume vs. transpulmonary pressure.
-
When is static compliance measured, and which part of the curve is used?
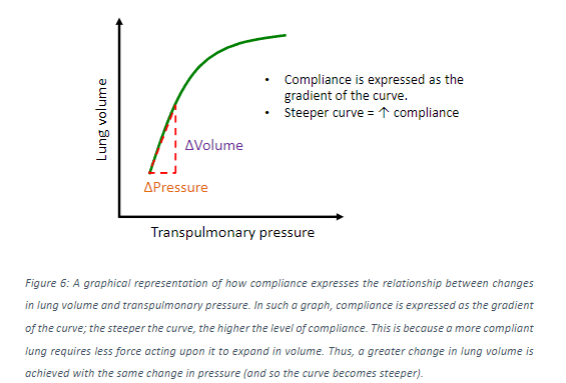
Static compliance is measured when airflow is zero, and the steepest part of the curve is used for measurement.
-
When is dynamic compliance measured, and which points on the curve are used?
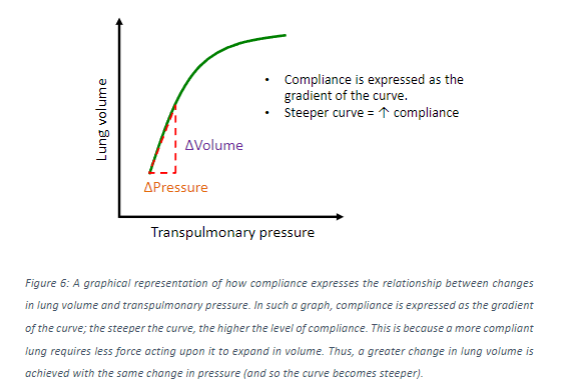
Dynamic compliance is measured in the presence of airflow, and the gradient between the end tidal inspiratory and end tidal expiratory points is used for measurement.
-
Picture demonstrating how number of diseases that affect the recoil or structure of the lungs and chest wall can lead to altered lung compliance:
-
Picture demonstrating how these changes would be affect volume-pressure curves:
-
What lines the internal surfaces of alveoli?
The internal surfaces of alveoli are lined with fluid.
-
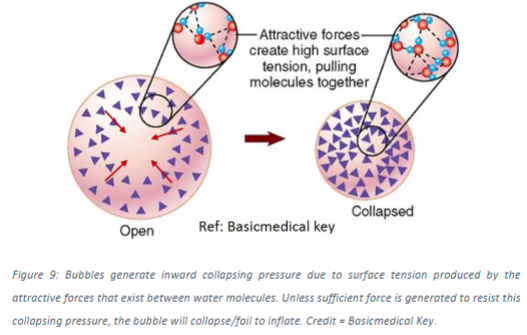
What creates surface tension within alveoli?
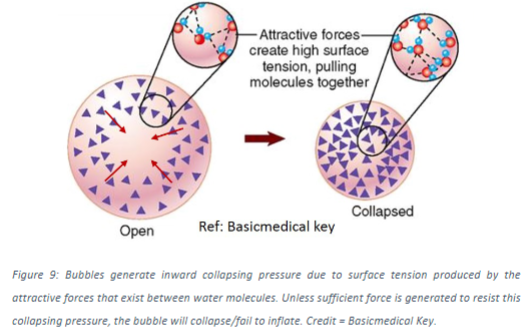
Surface tension within alveoli arises from the relative strength of hydrogen bonds between water molecules, exerting an overall collapsing force toward the centre of the alveolar bubble.
-
How is pressure generated within alveoli?
Pressure is generated within alveoli due to the collapsing force produced at the water-fluid interface.
-
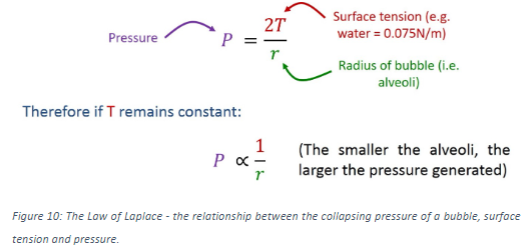
What law describes the relationship between collapsing pressure, the radius of the bubble, and surface tension?
The Law of Laplace describes the relationship between collapsing pressure, the radius of the bubble, and surface tension.
-
Picture demonstrating the Law of Laplace:
-
How does pressure relate to bubble radius?
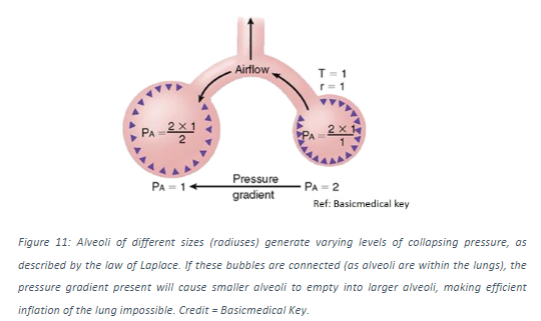
Pressure and bubble radius are inversely proportional, meaning that pressure increases as radius decreases. Smaller bubbles generate greater pressure than larger ones.
-
What happens when bubbles of varying size are connected?
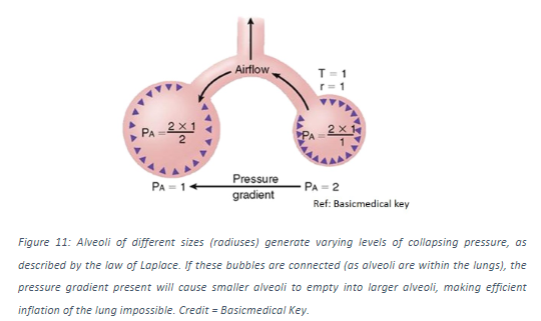
When bubbles of varying size are connected, such as different-sized alveoli connected by airways, the smaller bubble will empty into the larger ones due to the pressure gradient.
-
What is the role of pulmonary surfactant in the lungs?
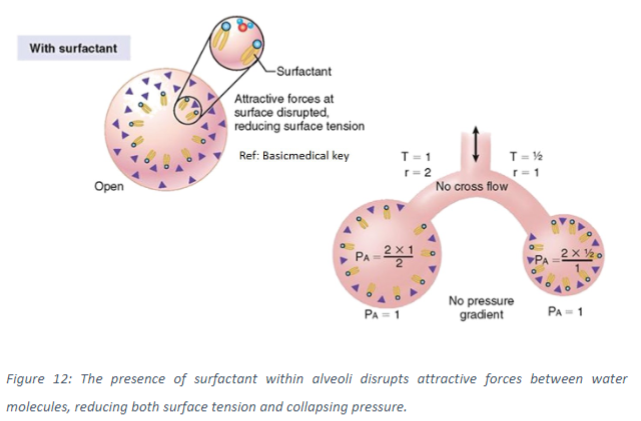
Pulmonary surfactant, secreted by type II pneumocytes (alveolar cells), reduces surface tension at the air-liquid interface in the alveoli. This reduces the collapsing pressure generated, preventing smaller alveoli from collapsing into larger ones.
-
What are the characteristics of surfactant molecules?
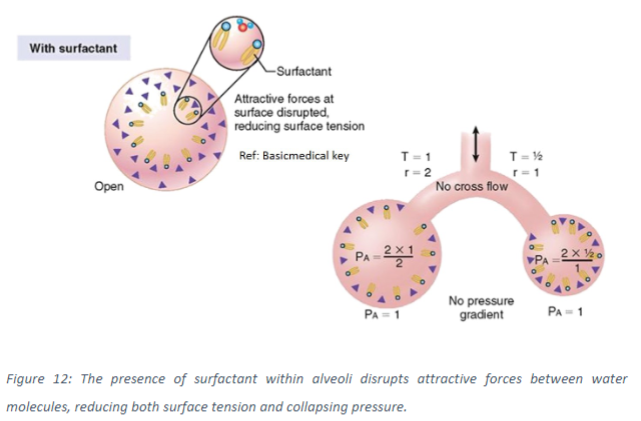
Surfactant molecules are amphipathic, possessing hydrophilic head and hydrophobic tail regions, allowing them to naturally position themselves at the air-liquid interface.
-
How does surfactant reduce surface tension?
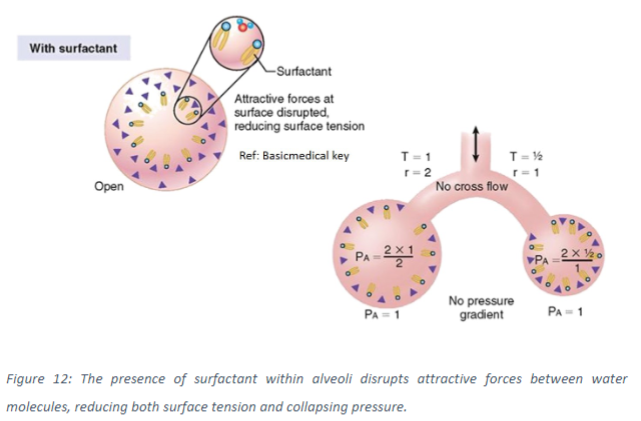
Surfactant disrupts the attractive forces between water molecules, thereby reducing surface tension.
-
How does pulmonary surfactant help equalize pressure between alveoli of varying sizes?
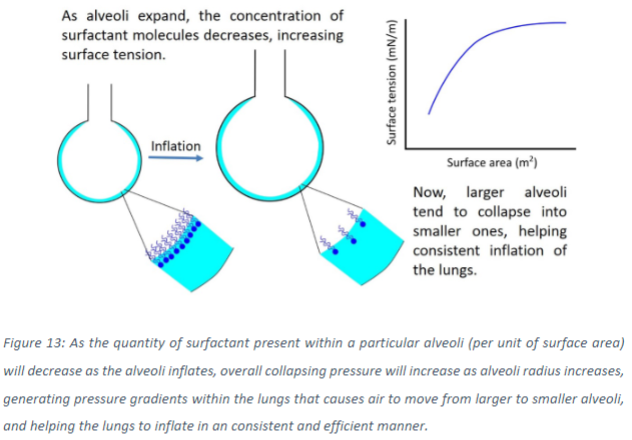
Pulmonary surfactant reduces surface tension at the air-liquid interface, which equalizes pressure between alveoli of varying sizes. During inflation, as alveolar size increases, the concentration of surfactant molecules at the interface decreases. This results in an increase in surface tension and pressure with increasing alveolar surface area.
-
What is the effect of surfactant on airflow between alveoli during inspiration?
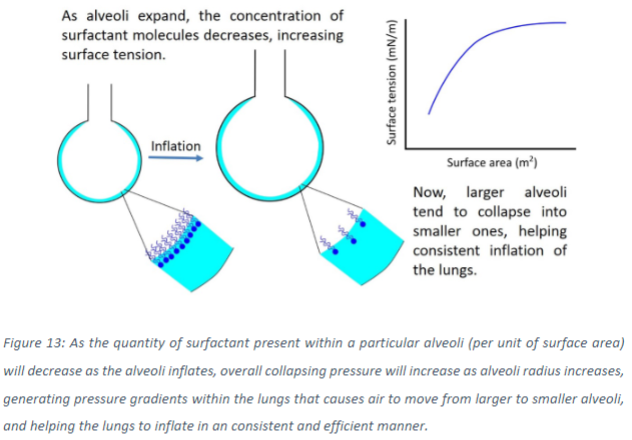
With the presence of surfactant, air naturally flows from larger, more inflated alveoli to smaller ones, helping to distribute air across the lung during inspiration.
-
How does surface tension at the air-liquid interface affect hydrostatic pressure in alveolar tissue?
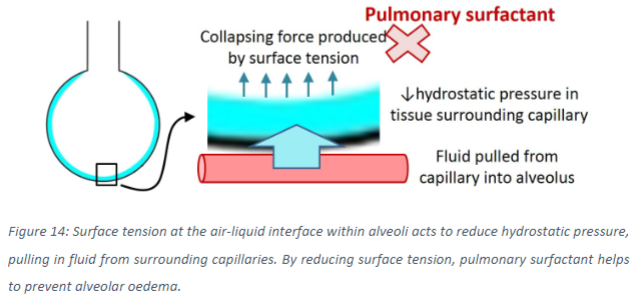
Surface tension at the air-liquid interface reduces hydrostatic pressure in the alveolar tissue. This pressure reduction pulls fluid out of the surrounding pulmonary capillaries and into the alveoli and interstitial tissue.
-
How does pulmonary surfactant help prevent alveolar oedema?
Pulmonary surfactant reduces surface tension, which helps prevent alveolar edema by reducing the excessive fluid pulled from capillaries into the alveoli and interstitial tissue.
-
What happens in patients with insufficient levels of pulmonary surfactant?
Patients with insufficient levels of pulmonary surfactant may experience pathology related to alveolar oedema due to the inability to adequately reduce surface tension.
-
What is Neonatal Respiratory Distress Syndrome (NRDS)?
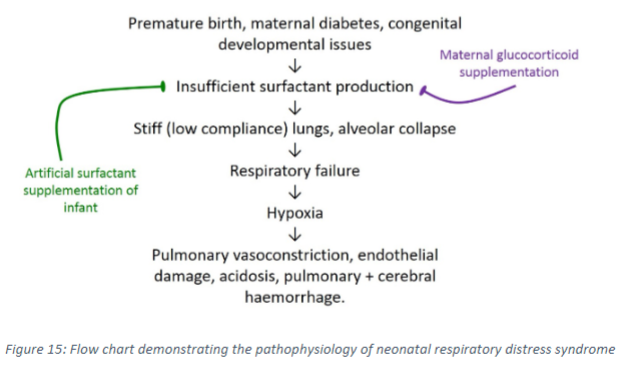
Neonatal Respiratory Distress Syndrome is a condition that occurs in infants born prematurely who produce insufficient levels of pulmonary surfactant. This deficiency leads to respiratory failure due to alveolar collapse, decreased lung compliance, and increased risk of alveolar oedema.
-
What are the consequences of insufficient pulmonary surfactant production in NRDS?
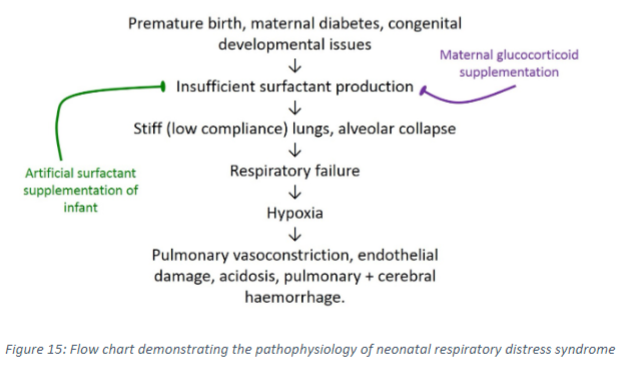
Insufficient pulmonary surfactant production in NRDS results in decreased lung compliance, making the lungs stiffer and more prone to collapse during inspiration. It also increases the likelihood of alveolar oedema, reducing the rate of gas exchange. Additionally, increased forces and pressures within the lungs can potentially damage alveoli and capillaries, further impairing respiratory function.
-
How is NRDS treated?
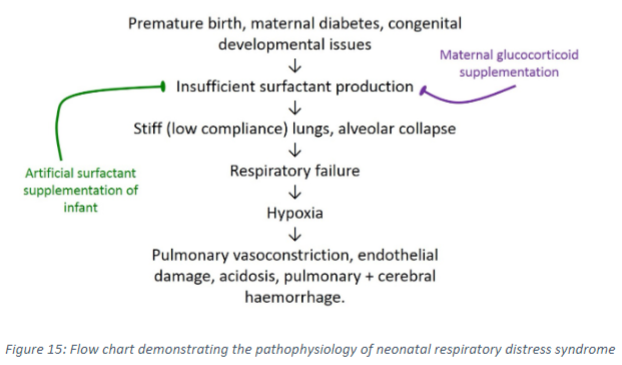
NRDS is treated by supplementing affected infants with artificial surfactant and/or administering glucocorticoids to mothers at high risk of premature birth. Glucocorticoids increase surfactant production by maturing type 2 pneumocytes.

