Steroids of the Adrenal Cortex (Physiology)
Steroids of the adrenal cortex - Dr Peter Skorupski Session summary The most important adrenal steroids in humans are cortisol and aldosterone. Cortisol, although widely known as the 'stress hormone', is essential to life. It has widespread metabolic, cardiovascular and immunosuppressive actions, affecting virtually every cell in the body. Glucocorticoids (cortisol or cortisol-mimicking drugs) are widely prescribed in a variety of clinical settings, because of their potent anti-inflammatory effects. Aldosterone controls salt balance, which serves to maintain normal blood volume in order to ensure adequate blood pressure for tissue perfusion. Learning outcomes At the end of this session you will be able to: Outline synthesis of adrenal steroids and relation to zonation of adrenal cortex Explain mineralocorticoid function Describe the principal effects of cortisol Explain feedback control of the adrenal cortex via the hypothalamic-pituitary axis Explain disorders of adrenocortical function in relation to the physiology of cortisol and aldosterone
-
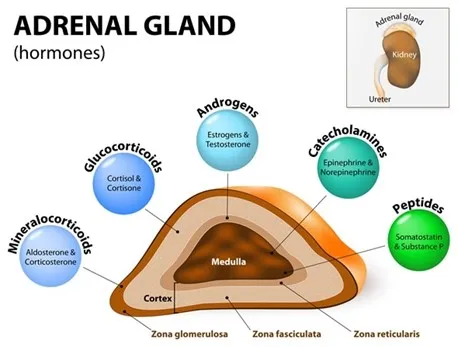
What are the three main types of steroids produced by the adrenal cortex?
The steroids of the adrenal cortex include glucocorticoids (principally cortisol), mineralocorticoids (aldosterone), and androgens.
-
What is the principal glucocorticoid produced by the adrenal cortex in mammals?
The principal glucocorticoid produced by the adrenal cortex in mammals is cortisol.
-
What is the main mineralocorticoid produced by the adrenal cortex?
The main mineralocorticoid produced by the adrenal cortex is aldosterone.
-
What are the consequences of excess cortisol production?
Excess cortisol production leads to a condition called Cushing’s syndrome.
-
What condition is associated with adrenal insufficiency?
Adrenal insufficiency, specifically primary adrenal insufficiency, is associated with Addison’s disease.
-
Describe the direction of blood flow in the adrenal gland from the cortex to the medulla.
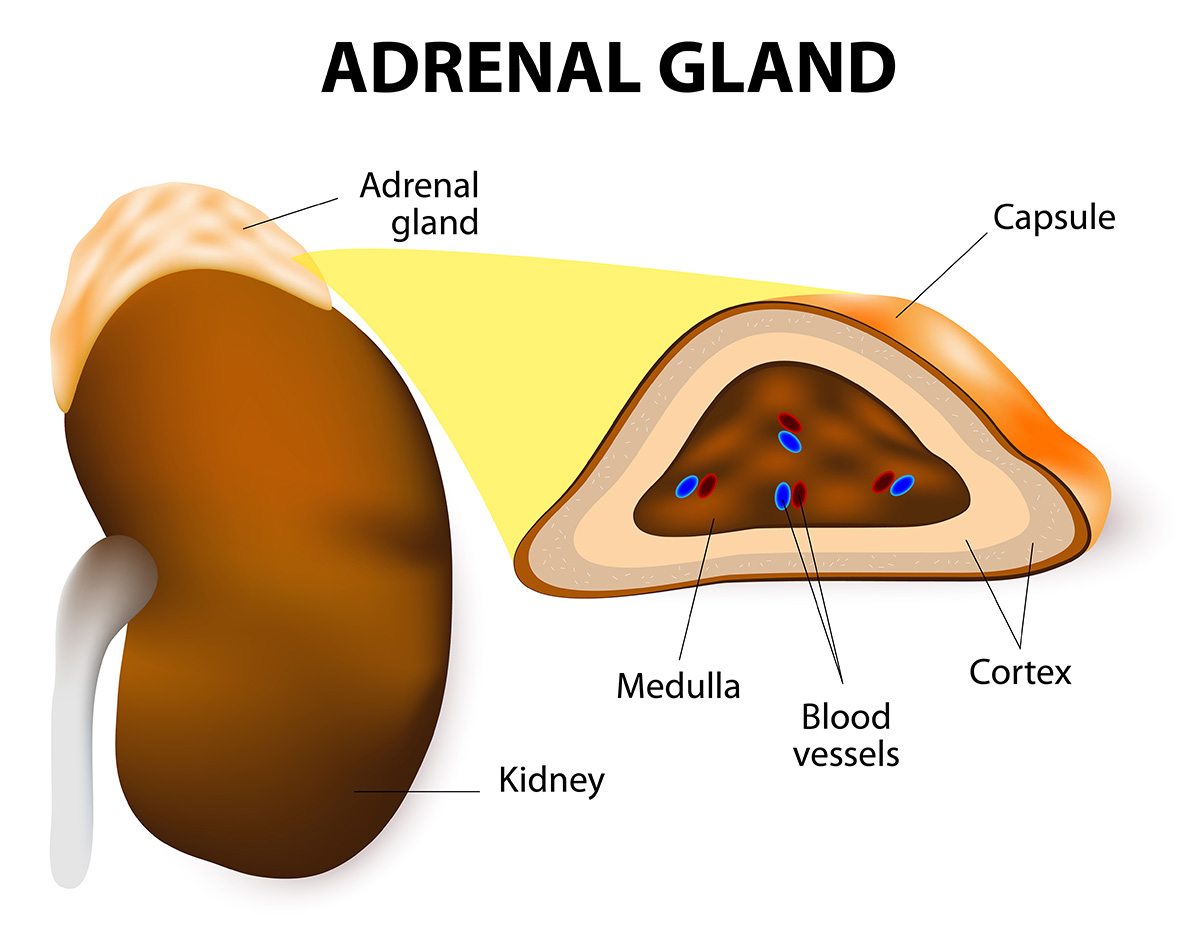
Blood flows from the outer cortex to the inner medulla in the adrenal gland.
-
How does the adrenal cortex exhibit functional zonation?
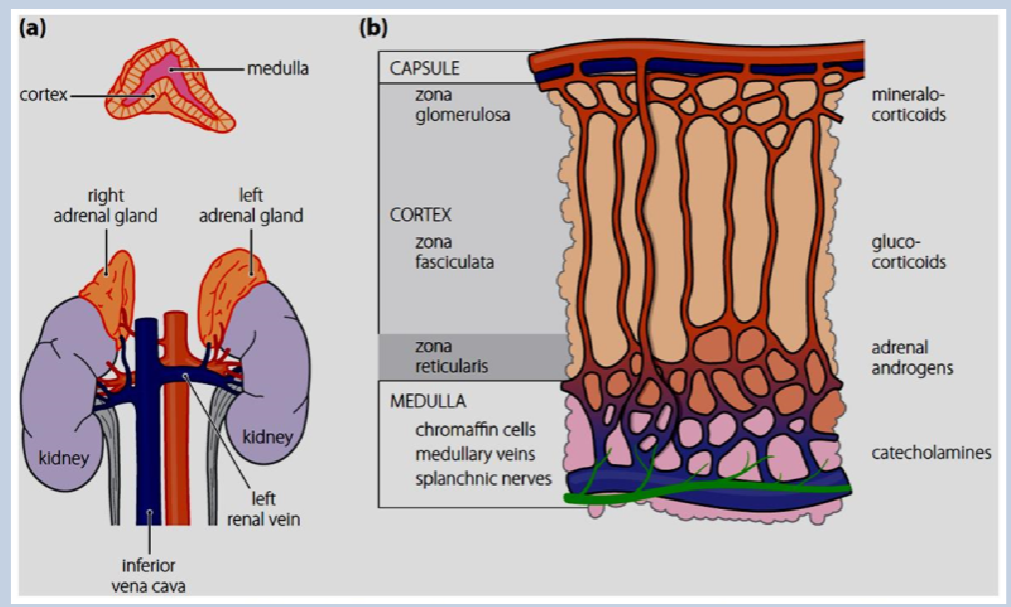
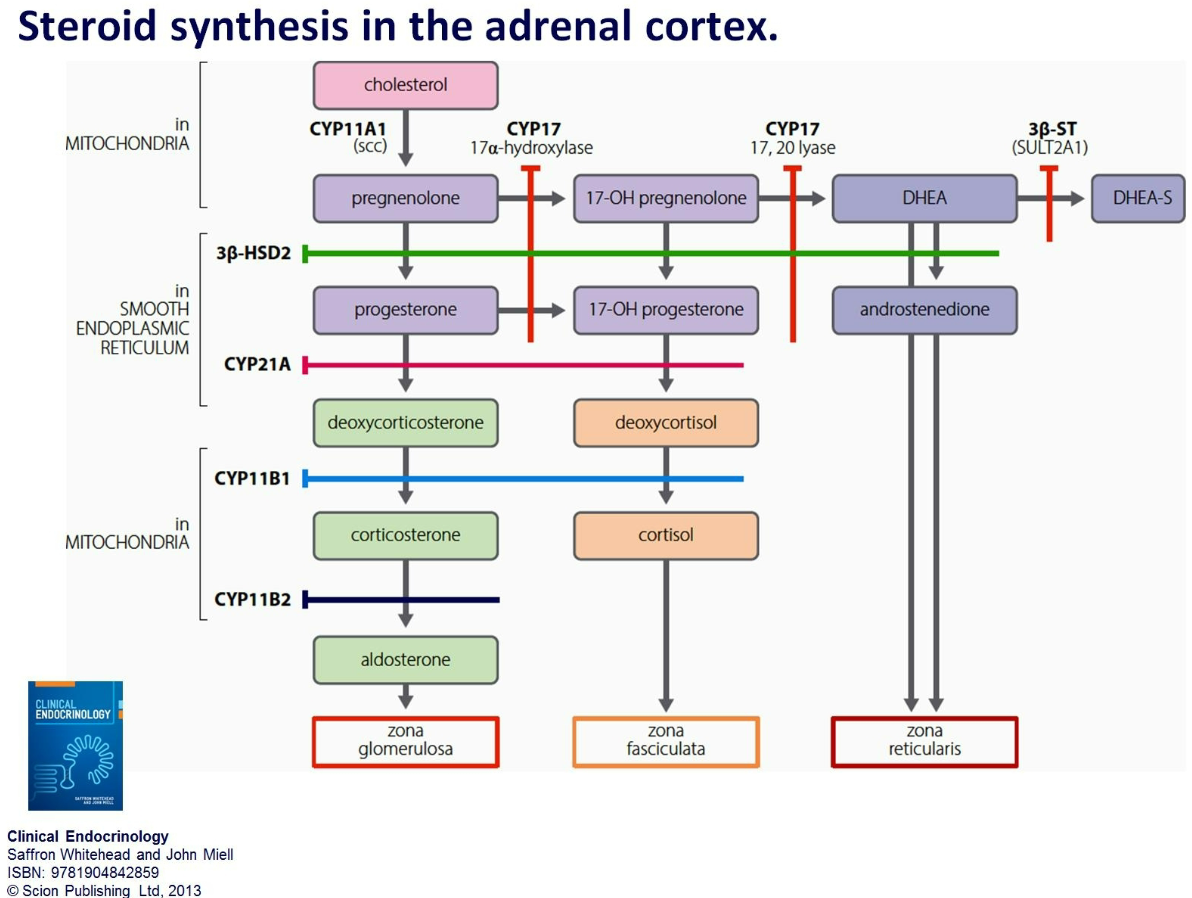
The adrenal cortex exhibits functional zonation due to layer-specific enzymes and the inhibition of different enzymes in subsequent layers during steroid synthesis.
-
What is the result of functional zonation in the adrenal cortex?
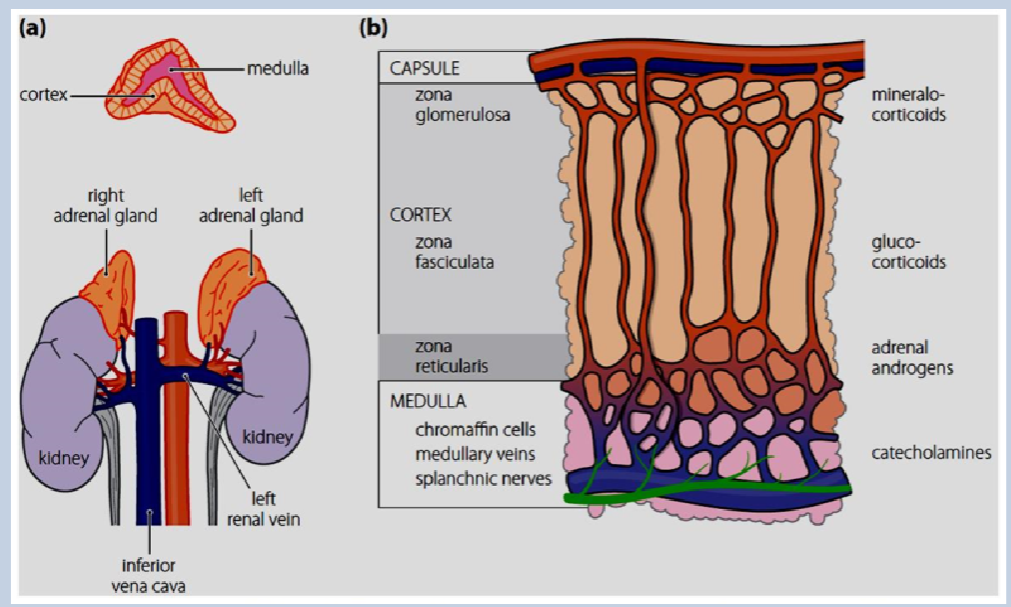
Functional zonation in the adrenal cortex leads to the production of different hormones in each layer.
-
Picture demonstrating steroid synthesis in the adrenal cortex:
-
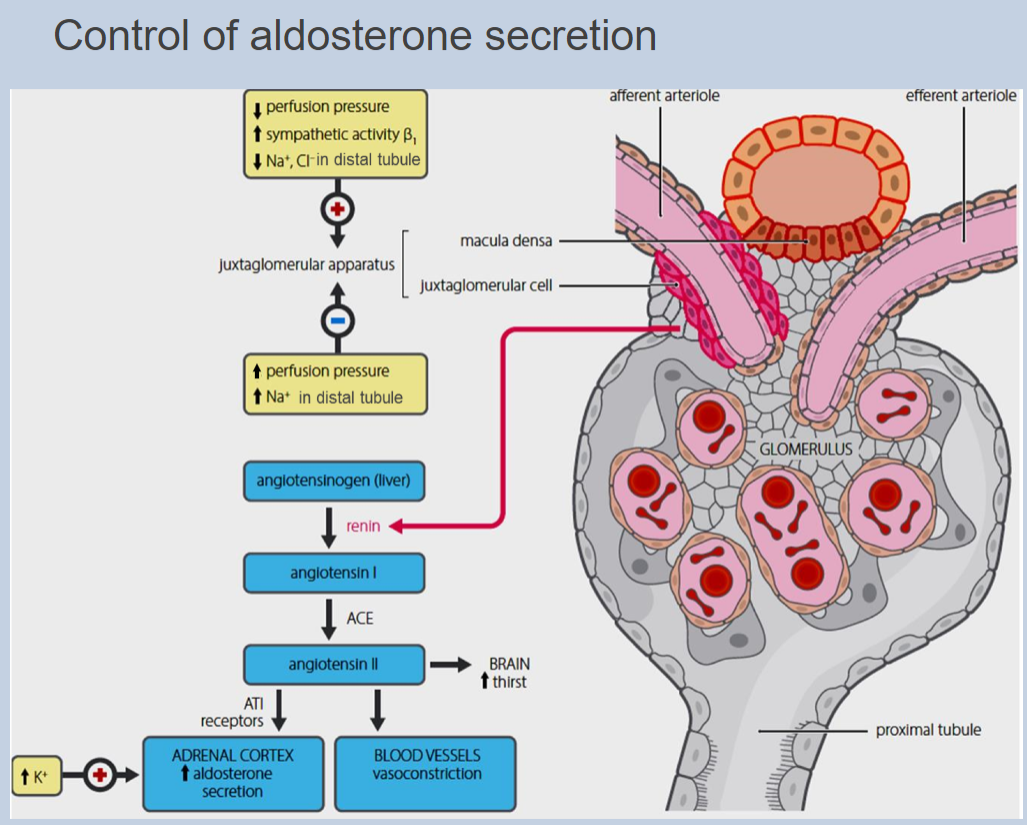
What is the primary role of mineralocorticoids?
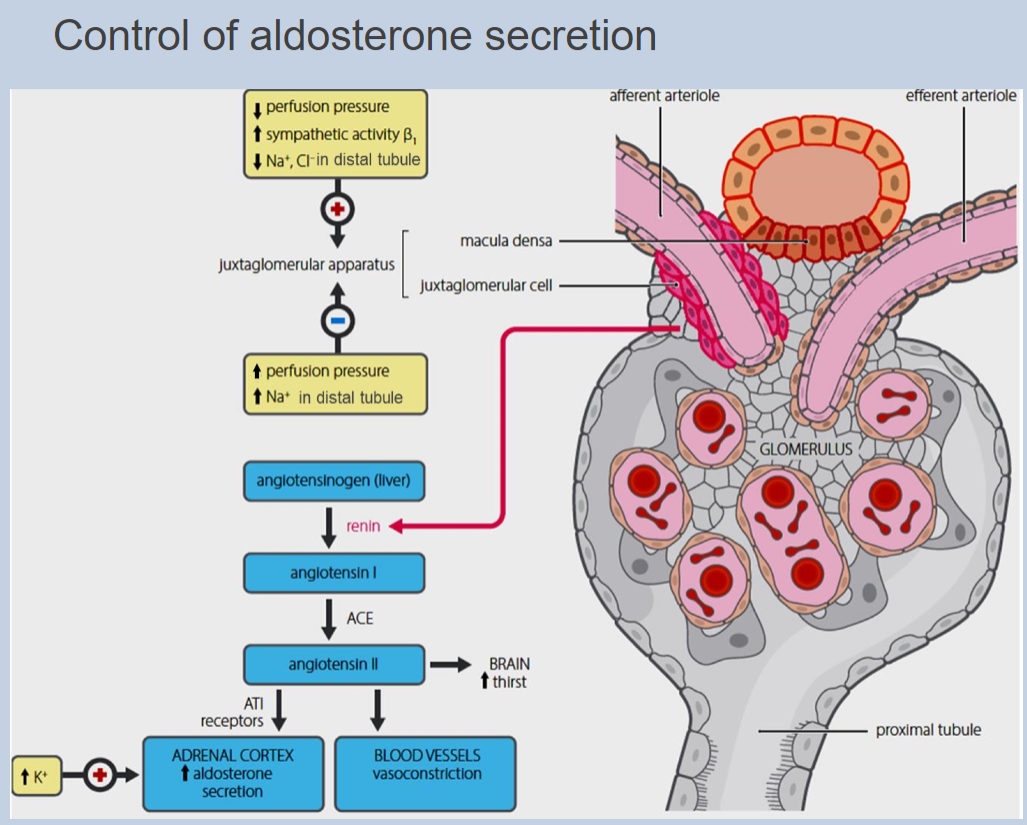
Mineralocorticoids regulate salt and water balance in the body.
-
What are the main functions of glucocorticoids?
Glucocorticoids regulate metabolism and immune function.
-
How does stress affect the release of adrenal steroids?
Stress increases the release of adrenal steroids, but minimal levels are essential for normal function.
-
What is the role of androgens produced by the adrenal cortex?
Androgens produced by the adrenal cortex, often called "weak androgens," contribute to various physiological processes in the body.
-
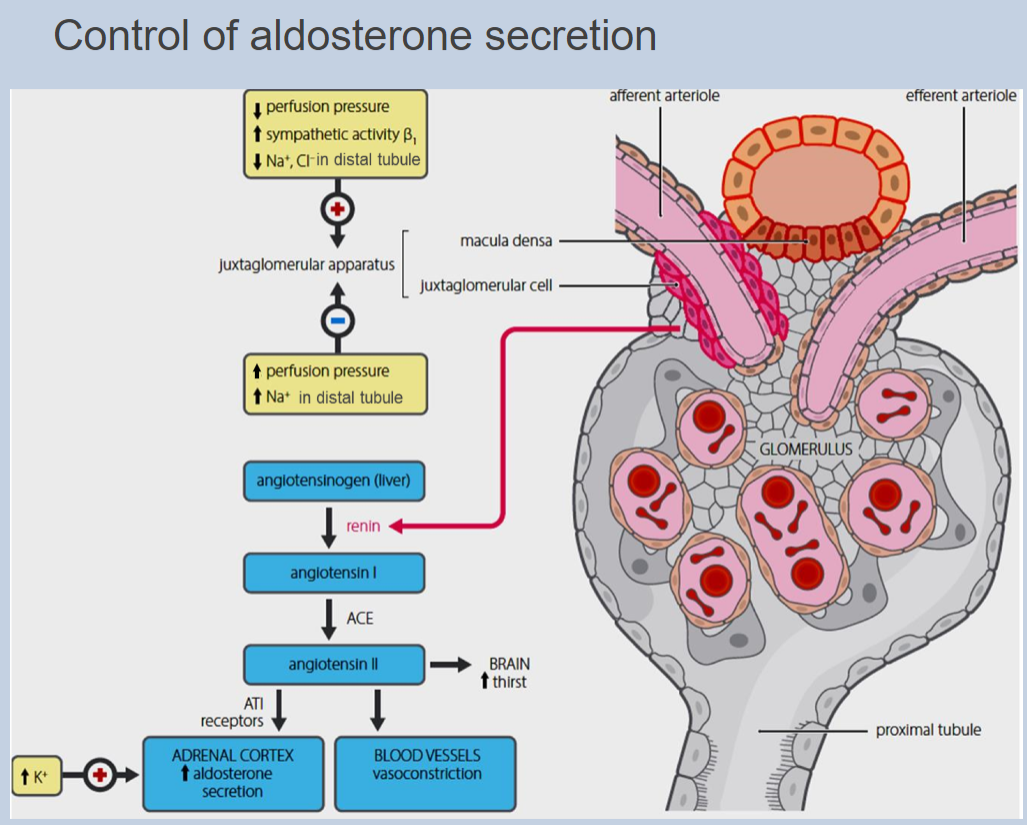
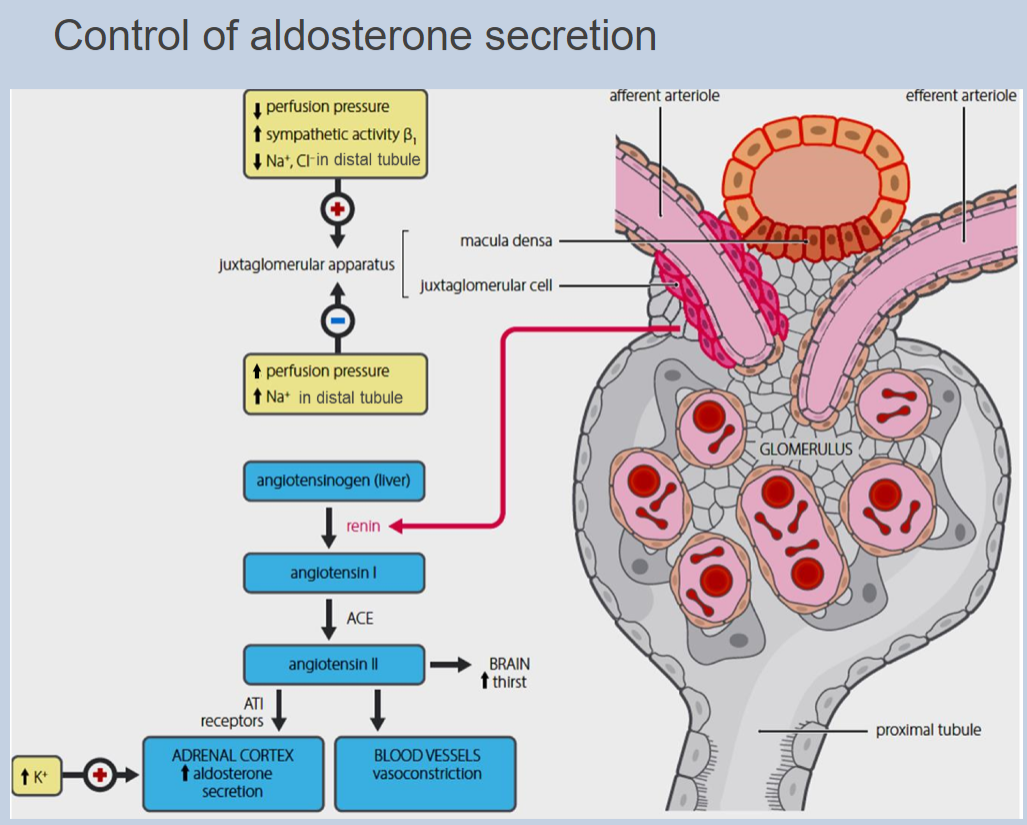
Picture demonstrating the Actions of aldosterone on the ascending loop of Henle, distal convoluted tubule and cortical collecting ducts of the kidney controlling the reabsorption of salt (Na+) and water:
-
Do cortisol and aldosterone have similar affinity for the aldosterone receptor?
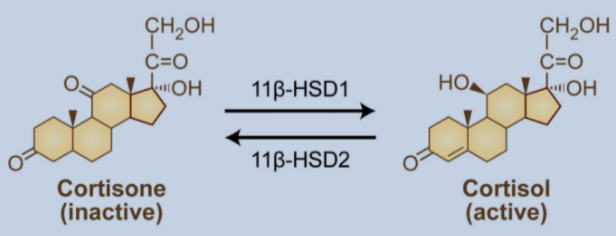
Yes, cortisol and aldosterone have similar affinity for the aldosterone receptor.
-
Despite having higher circulating concentrations, why doesn't cortisol stimulate salt and water retention like aldosterone?
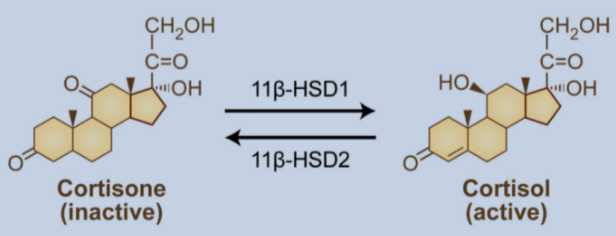
Cortisol doesn't stimulate salt and water retention like aldosterone because it is rapidly metabolized to inactive cortisone in the kidney.
-
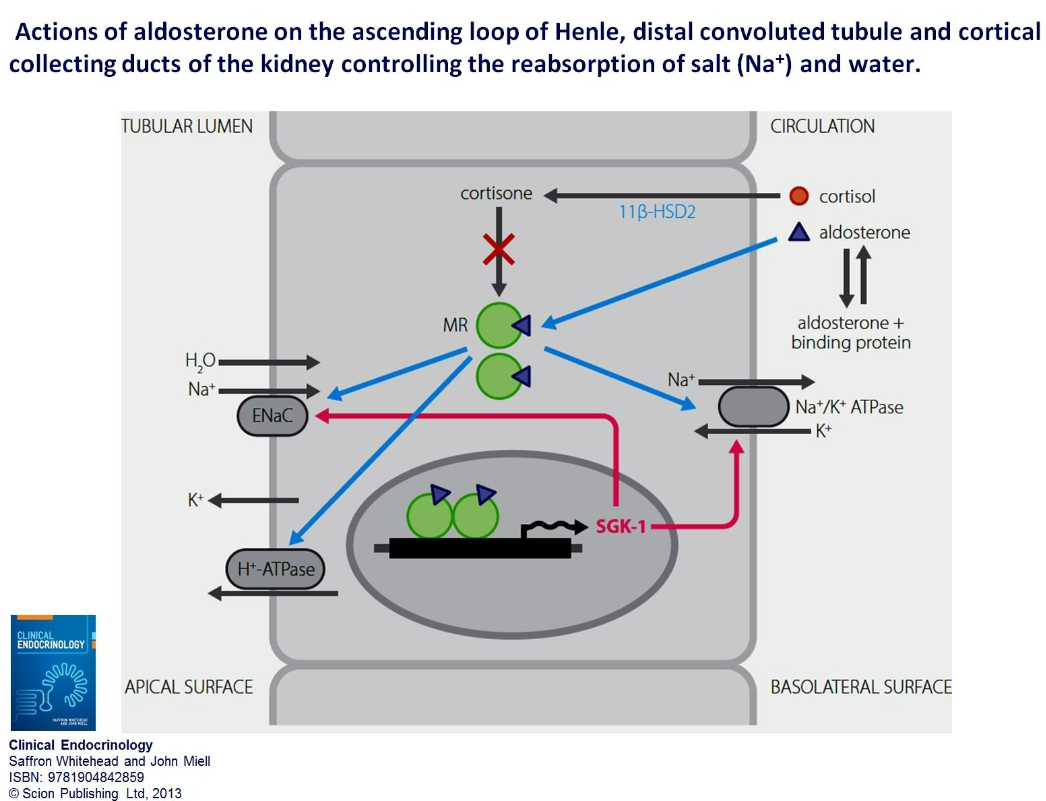
What enzyme is required for the metabolism of cortisol to cortisone in the kidney?
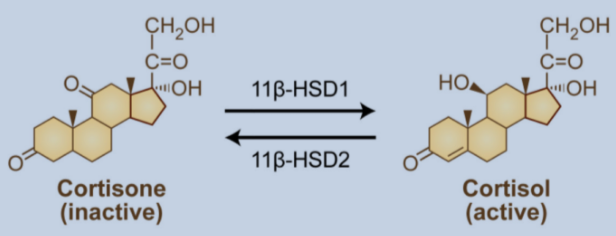
The enzyme required for the metabolism of cortisol to cortisone in the kidney is 11beta-hydroxysteroid dehydrogenase type 2 (11B-HSD2).
-
What rare condition is associated with a mutation of 11B-HSD2?
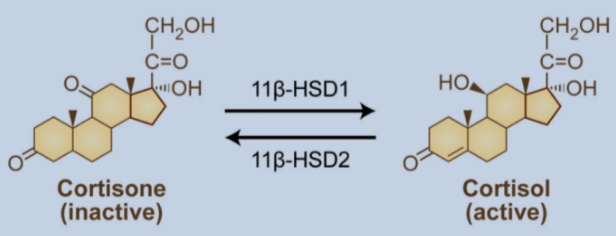
A rare inactivating mutation of 11B-HSD2 leads to a syndrome called apparent mineralocorticoid excess (AME).
-

What substance found in liquorice blocks the enzyme 11B-HSD2?
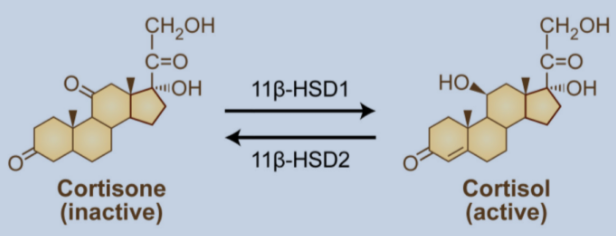
Liquorice contains a compound called glycyrrhizinic acid that blocks the enzyme 11B-HSD2, leading to increased cortisol activity and potential mineralocorticoid effects.
-
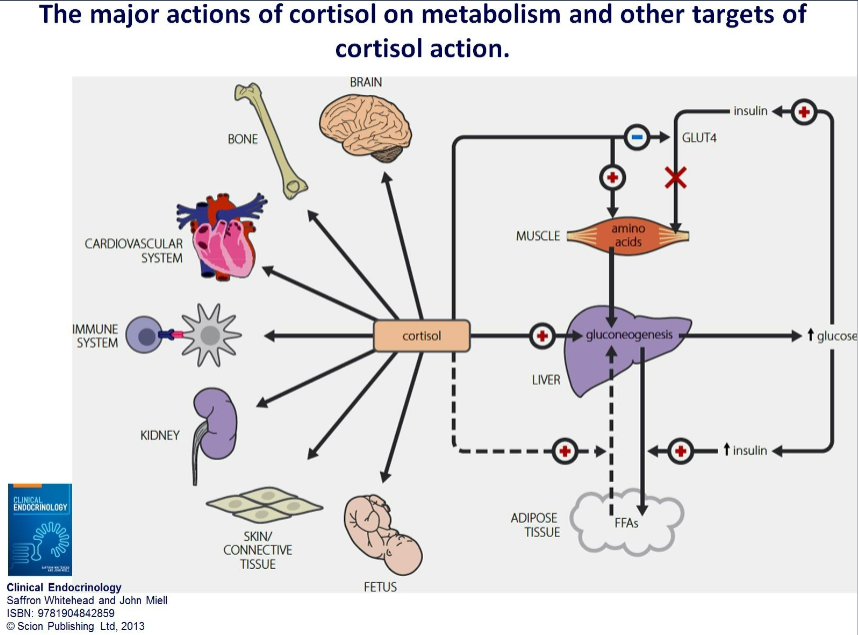
Picture demonstrating the major actions of cortisol on metabolism and other targets of cortisol action:
-
How do glucocorticoids affect glucose utilization?
Glucocorticoids decrease glucose utilization, a process known as glucose sparing.
-
What metabolic processes are promoted by glucocorticoids to maintain plasma glucose concentration?
Glucocorticoids promote lipolysis, gluconeogenesis (to maintain plasma glucose concentration), and proteolysis (to supply amino acid substrates for gluconeogenesis).
-
What is the overall role of glucocorticoids in glucose metabolism?
Glucocorticoids play a vital role in the maintenance of blood glucose levels, which is essential for survival during fasting.
-
What is the role of glucocorticoids in cardiovascular function?
Glucocorticoids are required for vascular integrity.
-
How does hypocortisolism affect cardiovascular function?
Hypocortisolism leads to inappropriate vasodilation and hypotension.
-
How does hypercortisolism affect cardiovascular function?
Hypercortisolism leads to hypertension.
-
What are the effects of glucocorticoids on inflammation and the immune system?
Glucocorticoids have anti-inflammatory and immunosuppressive effects.
-
How long have glucocorticoids been used in therapy?
Glucocorticoids have been used in therapy for over 60 years.
-
What are the implications of glucocorticoid therapy?
Glucocorticoid therapy is highly profitable and extremely effective, but it can have unintended side effects, making it a double-edged sword.
-
Picture demonstrating The effects of glucocorticoids on inflammatory mediators derived from arachidonic acid:
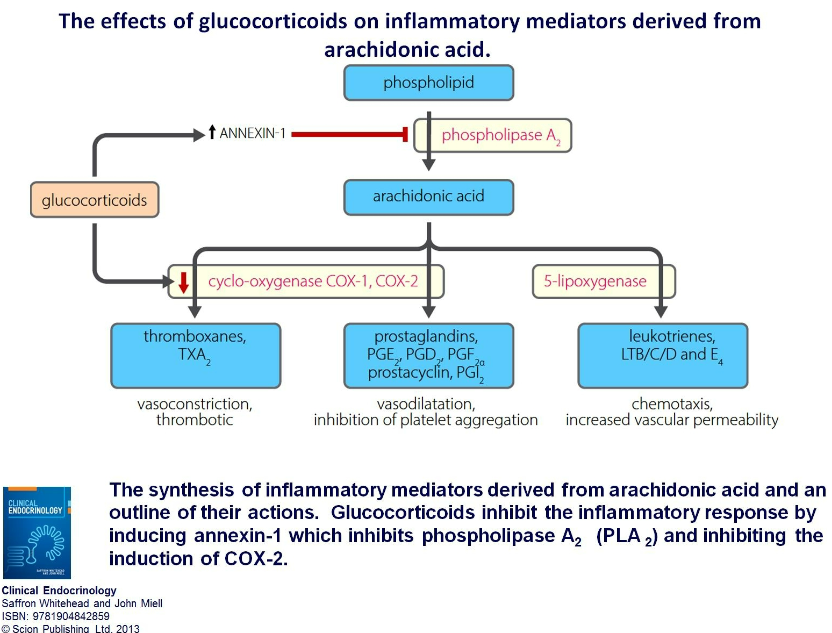
-
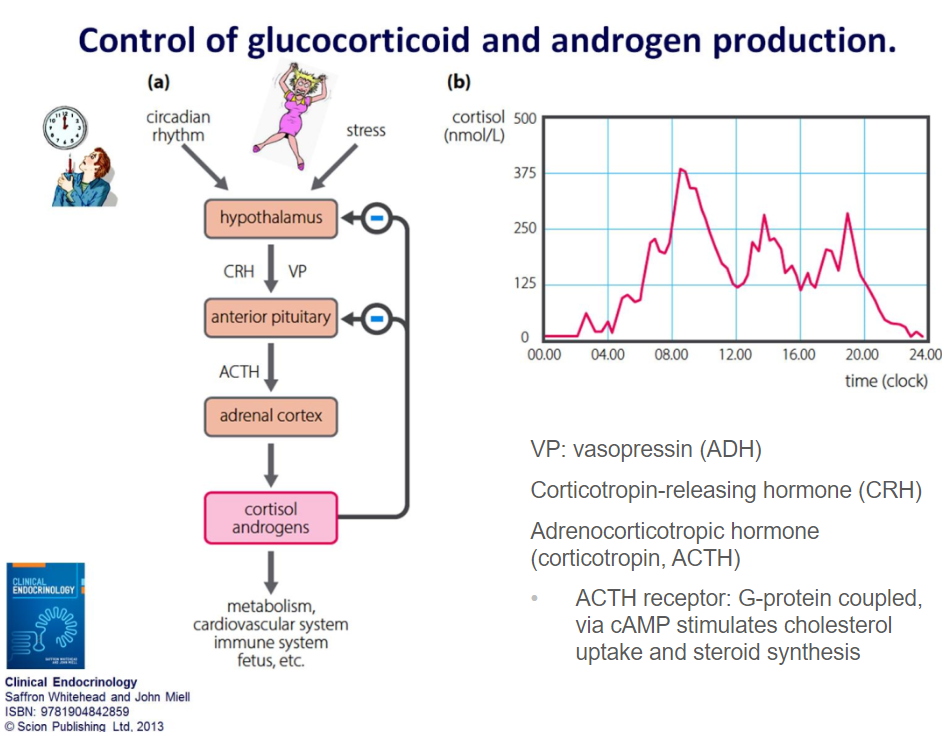
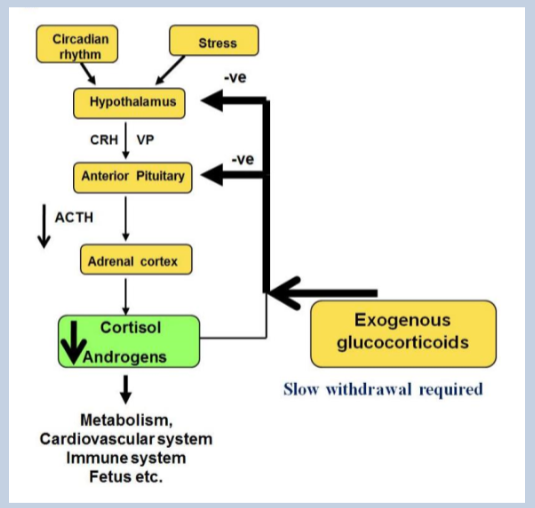
Picture demonstrating Control of glucocorticoid and androgen production:
-
What prohormone is ACTH synthesized from?
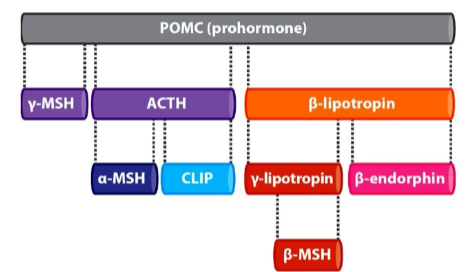
ACTH is synthesized from pro-opiomelanocortin (POMC) prohormone.
-
To which group of receptors does the ACTH receptor belong?
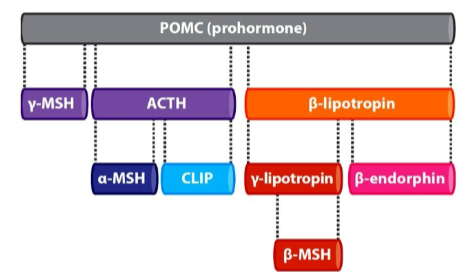
The ACTH receptor belongs to the melanocortin group of receptors.
-
What are the different forms of melanocyte-stimulating hormones that can bind to melanocortin receptors?
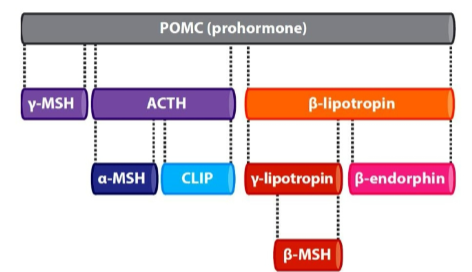
Different forms of melanocyte-stimulating hormones can bind to melanocortin receptors, including alpha-, beta-, and gamma-melanocyte-stimulating hormones.
-
Besides the ACTH receptor, where else can ACTH bind?
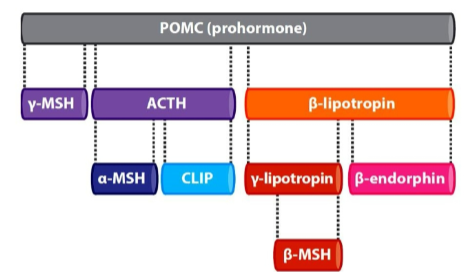
Besides the ACTH receptor, ACTH can also bind to other melanocortin receptors.
-
What can excess circulating ACTH cause?
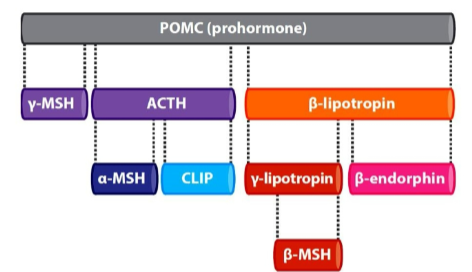
Excess circulating ACTH may cause skin pigmentation due to its effects on melanocytes.
-
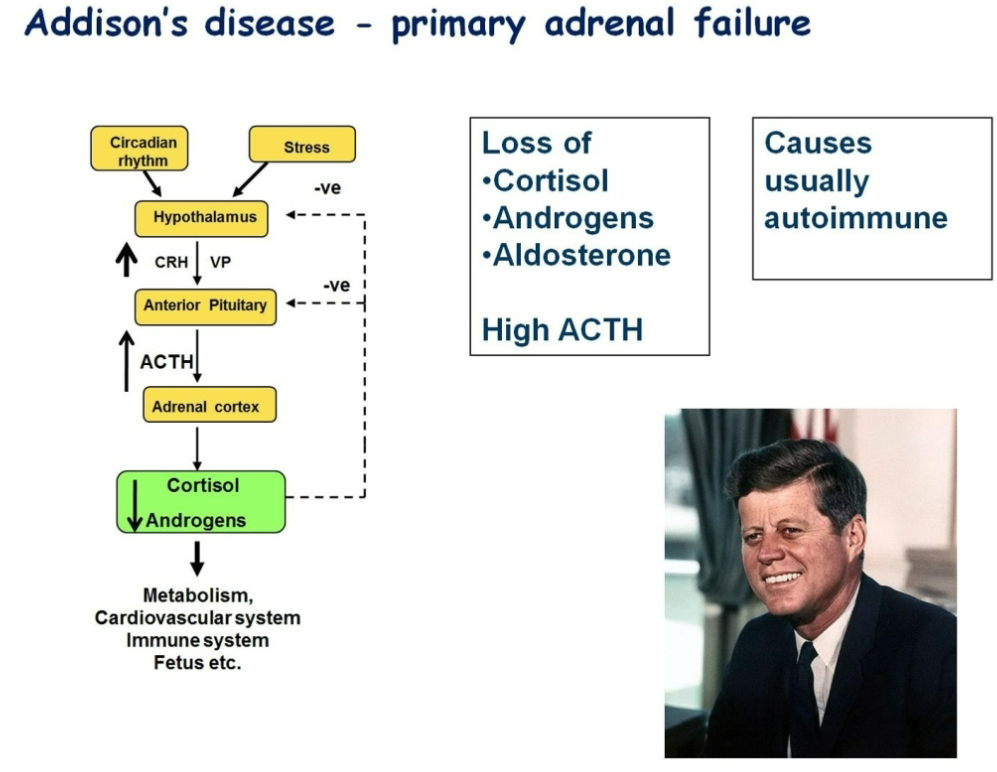
Picture demonstrating Addisons disease:
-
What are the clinical features of primary adrenal insufficiency, such as Addison's disease?
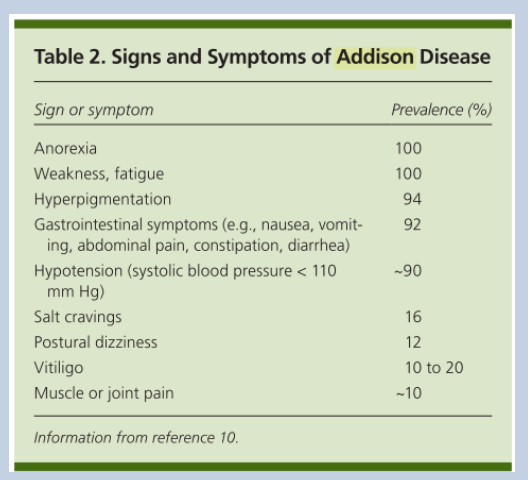
Clinical features of primary adrenal insufficiency include low circulating adrenal steroids, high ACTH levels, normal to low plasma sodium (Na+), normal to high plasma potassium (K+), and elevated plasma renin. It may be unmasked by significant stress or illness, leading to adrenal crisis.
-
What are the potential causes of adrenal insufficiency?
Adrenal insufficiency can be caused by Addison's disease (primary adrenal insufficiency), hypopituitarism (secondary hypocortisolism), failure in the renin-angiotensin-aldosterone system (secondary hypoaldosteronism), or enzyme defects in steroid synthesis pathways.
-
What is Cushing's syndrome characterized by?
Cushing's syndrome is characterized by excess glucocorticoid levels.
-
What are the main causes of Cushing's syndrome?
Cushing's syndrome can be ACTH-dependent, such as in Cushing's disease due to increased ACTH secretion (typically due to a pituitary adenoma), or ACTH-independent, such as adrenal adenoma or carcinoma, ectopic ACTH-secreting tumors, or iatrogenic causes (exogenous glucocorticoid therapy).
-
What are some clinical features of hypercortisolism (Cushing's syndrome)?
Clinical features of hypercortisolism include hypertension, hyperglycemia, truncal obesity, fatigue, muscle weakness, virilization (hirsutism in females), and mood or psychiatric disturbances.
-
What are the diagnostic steps for confirming hypersecretion of cortisol in suspected Cushing's syndrome?
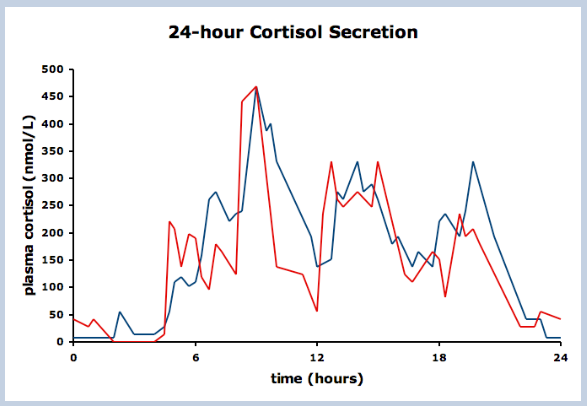
The first step is to confirm hypersecretion of cortisol through tests such as 24-hour urinary cortisol measurement or cortisol measurement at the nadir of secretion (around midnight).
-
How is the cause of Cushing's syndrome determined?
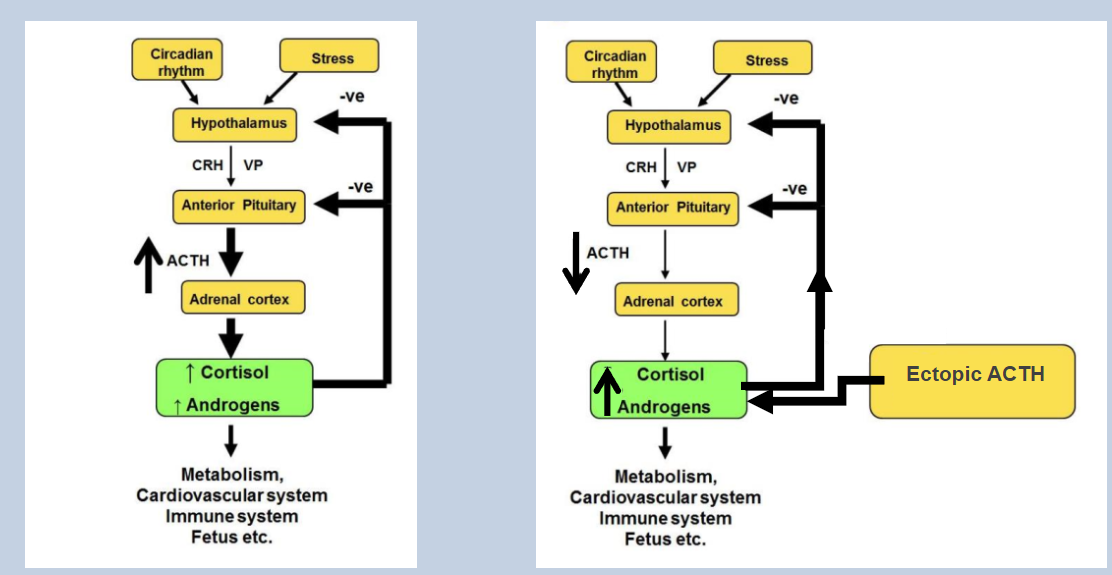
The cause of Cushing's syndrome is determined by assessing plasma ACTH levels and performing the dexamethasone suppression test.
-
What does the failure of cortisol suppression in the dexamethasone suppression test suggest?
Failure of cortisol suppression in response to both low and high doses of dexamethasone suggests an ectopic source of ACTH secretion, such as an ACTH-secreting tumor elsewhere in the body.
-
What is the most common cause of Cushing's syndrome?
The most common cause of Cushing's syndrome is iatrogenic, which is typically due to the administration of exogenous glucocorticoids.
-
How do exogenous glucocorticoids contribute to iatrogenic Cushing's syndrome?
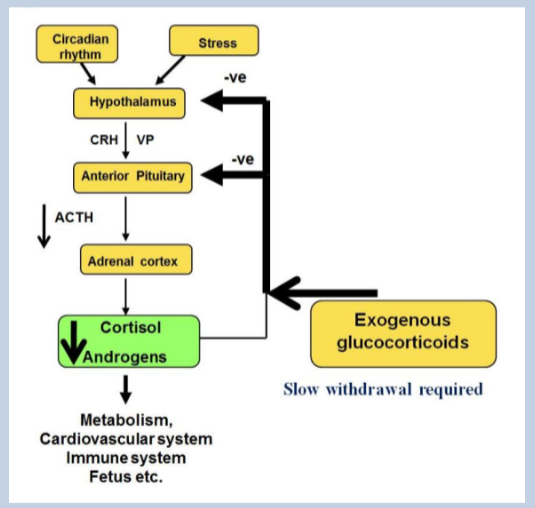
Exogenous glucocorticoids activate the cortisol receptor. At high doses, they can suppress the hypothalamic-pituitary-adrenal (HPA) axis, leading to adrenal cortex atrophy due to lack of adrenocorticotropic hormone (ACTH) stimulation.
-
What is the consequence of adrenal cortex atrophy in response to high doses of exogenous glucocorticoids?
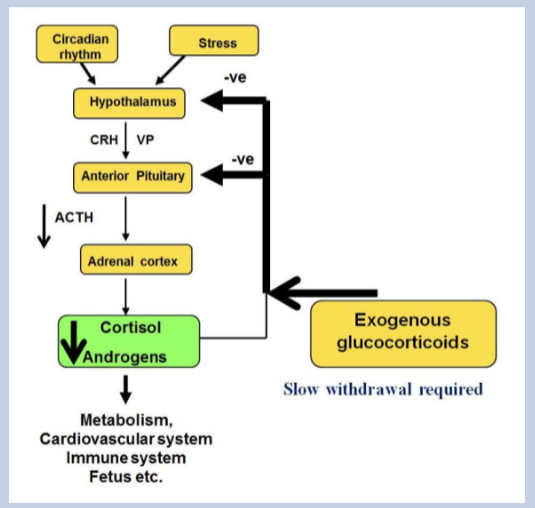
Adrenal cortex atrophy reduces the responsiveness of the adrenal glands to ACTH. After cessation of exogenous glucocorticoid therapy, it may take several days for the adrenal glands to become responsive to ACTH again.

