Schizophrenia (Physiology 2)
Schizophrenia - Dr Alexis Bailey Lecture Outline Although their severity might be hard to fully comprehend, we all have some idea of what mood and anxiety disorders are like because they are extremes in the spectrum of brain states that are part of the normal experience. The same cannot be said for schizophrenia. This is severe mental disorder distorts thought and perceptions in ways that healthy people find difficult to understand. In this you will learn about the different symptom classes associated with schizophrenia, the hypotheses regarding its manifestation, and treatment options for patients suffering with the disorder. Desired Learning Outcomes By the end of this lecture, students should be able to: Describe symptoms of schizophrenia –Positive, negative, cognitive Identify the phases of schizophrenia –Prodrome, acute, remission, relapse Discuss the potential causes of schizophrenia –Genes and/or environmental factors Discuss the potential pathophysiological mechanisms behind schizophrenia Identify the major differences between typical and atypical antipsychotics Explain how antipsychotic side effects are mediated Session Resources Download the lecture slidesDownload Download the lecture slides Session Activities (panopto available after the end of the session) Quiz Test your knowledge with this QuizLinks to an external site. and this QuizLinks to an external site. Further Reading 'Neuroscience: Exploring the Brain' by Bear, Connors, Paradiso Chapter 22 'Pharmacology Condensed' by Dale and Haylett Chapter 39 Glossary Anhedonia – The inability to feel pleasure in normally pleasurable activities. Aetiology - The cause, set of causes, or manner of causation of a disease or condition. Candidate gene – Any gene thought likely to cause a disease. Risk gene – see ‘Candidate Gene’ Cognitive behavioural therapy – A type of psychotherapy in which negative patterns of thought about the self and the world are challenged in order to alter unwanted behaviour patterns or treat mood disorders such as depression. Electroconvulsive therapy – A treatment that involves sending an electric current through the brain to trigger an epileptic seizure to relieve the symptoms of some mental health problem. Mesocortical pathway - A dopaminergic pathway that connects the ventral tegmentum to the prefrontal cortex. Mesolimbic pathway - A dopaminergic pathway that connects the ventral tegmental area in the midbrain, to the ventral striatum of the basal ganglia in the forebrain. Nigrostriatal pathway - A dopaminergic pathway that connects the substantia nigra pars compacta (SNc) with the dorsal striatum (i.e., the caudate nucleus and putamen). Tuberophypophyseal pathway – A population of dopamine neurons that project from the arcuate nucleus ( a.k.a. the "infundibular nucleus") in the tuberal region of the hypothalamus to the median eminence. Prolactin – A hormone released from the anterior pituitary gland that stimulates milk production after childbirth. Antipsychotic – A class of drugs designed to treat a severe psychiatric condition known as schizophrenia. Extra-pyramidal side effects – Serious side-effects of antipsychotic and other drugs affecting movement. Agranulocytosis - A deficiency of granulocytes in the blood, causing increased vulnerability to infection.
-
What are major psychotic disorders and provide examples? (3)
Psychotic disorders are conditions characterized by a mental state that is out of touch with reality.
Examples include schizophrenia, schizoaffective disorder (schizophrenia + bipolar disorder), and delusional disorder.
Some depressive and manic illnesses also involve psychotic features.
-
Why is schizophrenia considered the most important psychotic disorder? (3)
Early onset: Schizophrenia often develops in late adolescence or early adulthood.
Prevalent: It affects around 1% of the population.
Disabling and chronic: It leads to long-term disability and often requires lifelong care.
-
What are the main features of schizophrenia? (3)
Mental state: Out of touch with reality.
Abnormalities in perception, thought, and ideas: Distorted thinking and hallucinations.
Altered behaviour: Profound changes, including bizarre and alienating behaviours.
-
What is the prevalence of schizophrenia and what factors influence it? (3)
Prevalence: Affects up to 1% of the population.
Influencing factors: Culture, ethnicity, background, and socioeconomic status can influence diagnosis and understanding.
Urban areas: Schizophrenia is more common in urban environments.
-
How does schizophrenia differ between the sexes? (3)
Men: Earlier onset, higher propensity to negative symptoms, lower social functioning, and more co-morbid substance abuse.
Women: Later onset, more affective symptoms.
These differences in progression and symptoms highlight the diverse nature of the disorder.
-
What are the early signs of schizophrenia before it is recognized? (2)
Late teenage years: Often associated with social isolation, interest in fringe cults, and social withdrawal.
These symptoms may go unnoticed or be misinterpreted as typical adolescent behavior.
-
What is the cost of treating schizophrenia in the UK? (2)
The cost of treating schizophrenia is approximately six times higher than the cost of treating heart disease.
Schizophrenia is a chronically disabling condition, with significant impacts on quality of life and morbidity.
-
What are the three classes of symptoms in schizophrenia? (3)
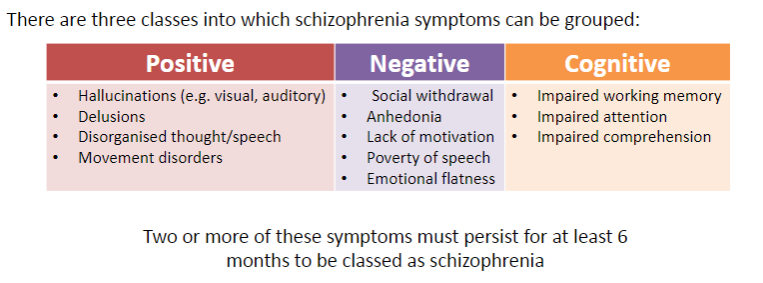
Positive
Cognitive
Negative
-
What are examples of positive symptoms of schizophrenia? (4)
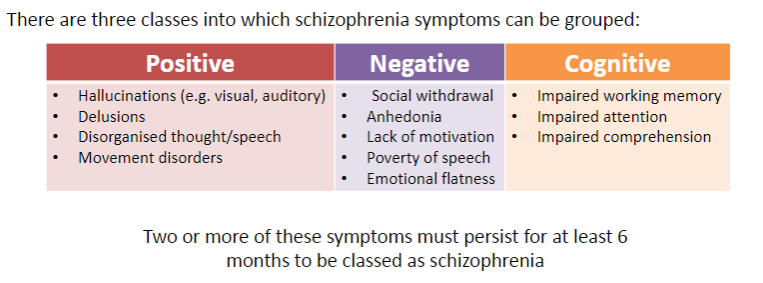
Hallucinations (e.g., visual, auditory)
Delusions
Disorganized thought/speech
Movement disorders
-
What are examples of cognitive symptoms of schizophrenia? (3)
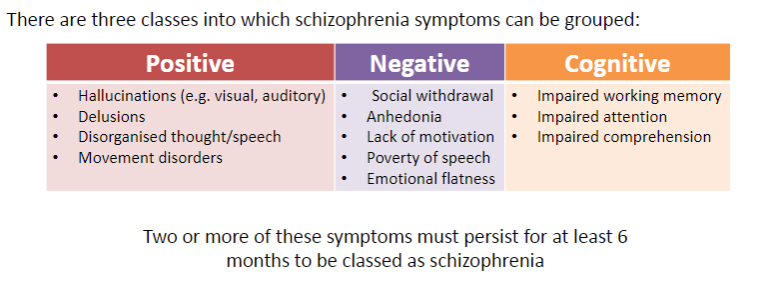
Impaired working memory
Impaired attention
Impaired comprehension
-
What are examples of negative symptoms of schizophrenia? (5)
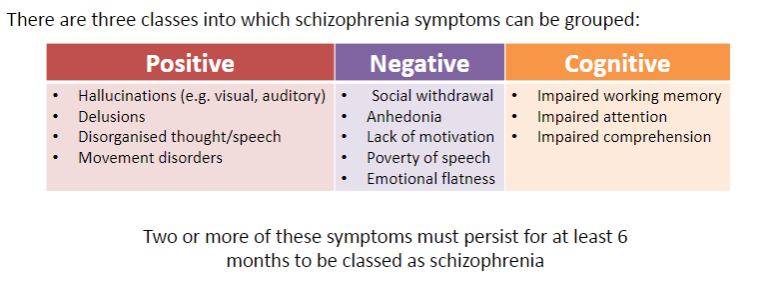
Social withdrawal
Anhedonia (lack of pleasure)
Lack of motivation
Poverty of speech
Emotional flatness
-
How long must symptoms persist for a diagnosis of schizophrenia? (1)
Two or more symptoms must persist for at least 6 months to be classed as schizophrenia.
-
What are hallucinations and how are they experienced? (2)
Hallucinations are perceptions experienced without a stimulus (functional hallucination).
Most commonly auditory.
-
What are examples of auditory hallucinations in schizophrenia? (4)
Voices talking about them (third person)
Voices talking to them
Voices giving a running commentary
Voices echoing their thoughts (thought echo)
-
How might patients respond to auditory hallucinations? (2)
Patients may engage in a dialogue with the voices.
Patients may obey the commands given by the voices.
-
What are delusions in schizophrenia? (2)
A fixed/unshakable belief not consistent with cultural/social norms.
Often paranoid, such as the belief that they are under the control of an external influence.
-
Give an example of a common paranoid delusion. (1)
Believing there is a conspiracy to harm them.
-
What are the various motor, volitional, and behavioral disorders in schizophrenia? (6)
Peculiar forms of motility
Stupor
Mutism
Stereotypy (purposeless, repetitive acts)
Mannerism (bizarre postures, strange mannerisms)
Spontaneous automatism (impulsivity)
-
What are stereotypies in schizophrenia? (1)
Stereotypies are purposeless, repetitive acts.
-
What are examples of bizarre behaviors and motor disturbances in schizophrenia? (2)
Bizarre postures and strange mannerisms
Altered facial expression, such as grimacing
-
Describe the state of catatonia in schizophrenia. (2)
Motionless, mute, expressionless
May adopt uncomfortable or contorted postures
-
What is catalepsy in schizophrenia? (1)
Catalepsy is characterized by a waxy flexible state
-
What are some motor behaviors associated with extreme states in schizophrenia? (2)
Bouts of extreme hyperactivity, such as destructiveness
Impulsive behavior
-
Is schizophrenia a violent disorder? (1)
Schizophrenia is NOT a violent disorder. While some individuals may engage in violent behavior, this is often due to untreated symptoms or co-occurring issues like substance abuse.
-
What is formal thought disorder in schizophrenia? (4)
Disorder of conceptual thinking
Reflected in speech that is difficult to understand
Rapid shifts from one subject to another
New words (neologisms) invented
-
What is social withdrawal in schizophrenia? (1)
Patients withdraw from their families and friends and spend a lot of time alone.
-
What does lack of initiative or motivation look like in schizophrenia? (2)
Patients do not want to do anything
No longer interested in things that used to interest them
-
What is formal thought disorder in schizophrenia and its key characteristics? (4)
Disturbances in thinking leading to unintelligible speech
Derailment of speech (e.g., jumping from topic to topic)
Loosening of associations; failure to follow the train of thought
Poverty of speech (speech fails to convey sense/information), manifested as distorted or illogical speech
-
What are the cognitive deficits and affective changes seen in schizophrenia? (3)
Cognitive deficits in selective attention, problem-solving, and memory
Blunted affect (decreased responsiveness to emotional issues)
Incongruous affect (expression of emotion inappropriate to circumstances)
-
What is the role of insight in schizophrenia? (2)
Insight is an understanding of what is wrong.
Insight is typically lacking in schizophrenia, as patients often do not accept that anything is wrong or that treatment is necessary.
-
What are the four phases of schizophrenia? (4)
The Prodrome
Occurs in late teens/early twenties, often mistaken for depression or anxiety.
Can be triggered by stress.
The Active/Acute Phase
Onset of positive symptoms.
Differentiation of what is real and not real becomes difficult.
Remission
Treatment leads to a return to ‘normality.’
Relapse
Schizophreniform positive symptoms persist for at least a month but less than 6 months.
-
What are the main causes (aetiology) of schizophrenia? (4)
Genetics
Schizophrenia has a genetic component, with higher risk if a close family member has the disorder.
Multiple genes contribute to susceptibility.
Environmental Factors
Stressful life events, prenatal infections, or complications during birth can contribute to the development of schizophrenia.
Drug use, especially during adolescence, can also trigger or worsen the condition.
-
What do twin studies suggest about the genetic risk of developing schizophrenia? (2)

Monozygotic twins (identical twins)
If one twin is diagnosed with schizophrenia, there is a 50% chance the other twin will develop it as well.
Dizygotic twins (fraternal twins)
If one twin is diagnosed with schizophrenia, the risk for the other twin is around 14%.
-
What are 'candidate' genes in the context of schizophrenia and their role? (3)
Sickle-cell disease, cystic fibrosis, and colour blindness
These disorders have known genetic anomalies that lead to their development.
Candidate genes for schizophrenia
Examples include COMT, DISC1, and GRM3.
Genetic risk
Possessing these abnormal genes does not guarantee the development of schizophrenia. Likewise, some individuals with schizophrenia may not have these specific genetic abnormalities.
-
What are the pregnancy and birth complications linked to schizophrenia risk? (3)
Season of birth
Exposure to influenza during pregnancy, such as during the 1957 epidemic, increases schizophrenia risk.
Birth complications
Low birth weight, premature birth, and asphyxia during birth are associated with early-life stress and an increased risk of schizophrenia.
Pregnancy-related recommendations
Pregnant women in the UK are advised to be vaccinated against seasonal flu to reduce the risk.
-
What types of early-life stress can contribute to schizophrenia risk? (4)
Moving country
Refugee immigrants are at higher risk than non-refugee immigrants (Swedish study).
Early-life bereavement
Loss of a first-degree relative during childhood increases risk.
Loss of job/home/relationship
Major life stressors in early life may trigger schizophrenia.
Abuse
Physical, emotional, or sexual abuse increases the risk of schizophrenia.
-
How does drug use relate to schizophrenia? (3)
How does drug use relate to schizophrenia? (3)
-
What are the main factors in the aetiology of schizophrenia? (2)
Genetics
Schizophrenia isn’t directly inherited, but it can run in families.
Risk genes include gene deletions and mutations.
Environmental Factors
Pregnancy/birth complications, stress, and drug use can contribute to schizophrenia risk.
-
What is the Nature vs. Nurture debate in schizophrenia? (2)
Nature
Genetic factors play a significant role in the risk of developing schizophrenia.
Nurture
Environmental factors like stress and drug use also contribute to the development of schizophrenia.
-
What are the main components of the pathophysiology of schizophrenia? (5)
Dopamine Hypothesis
Abnormal dopamine activity in certain brain regions is implicated in schizophrenia.
Brain Structure Differences
Structural abnormalities in the brain, such as enlarged ventricles, are observed.
Hypofrontality
Reduced activity in the prefrontal cortex, linked to cognitive and negative symptoms.
NMDA Receptor Hypofunction
Dysfunction in NMDA receptors can contribute to psychotic symptoms.
Oxidative Stress and Neuroinflammation
Increased oxidative stress and neuroinflammation may play a role in the development of schizophrenia.
-
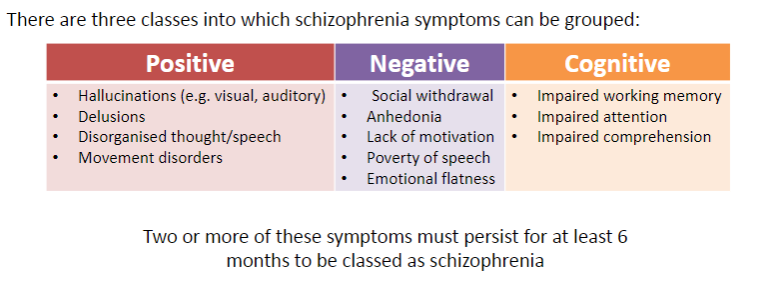
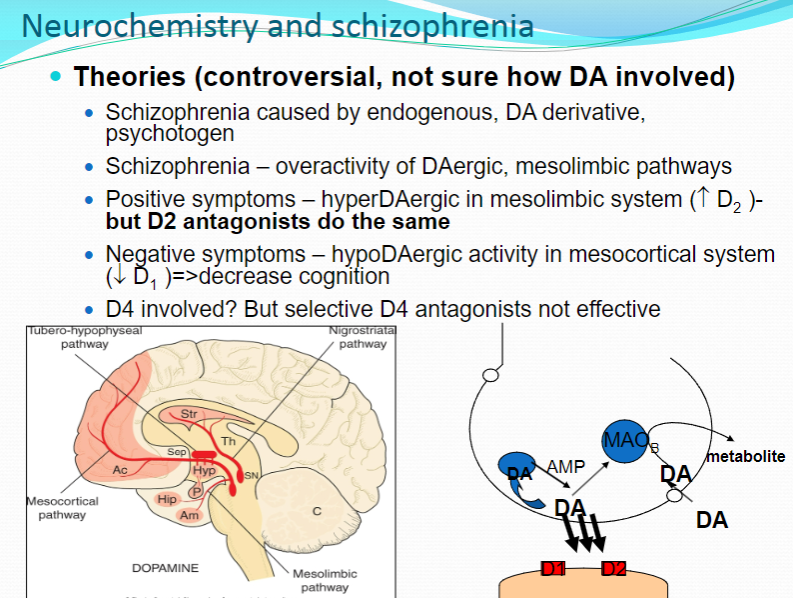
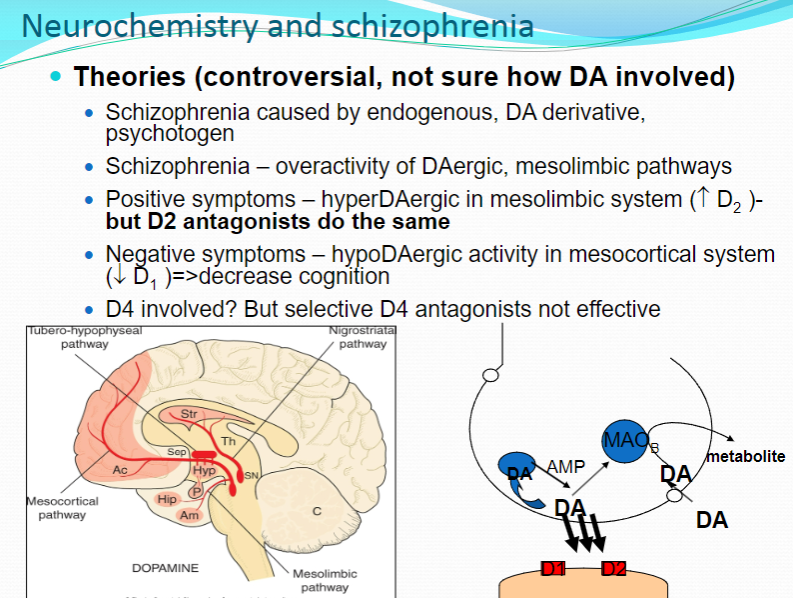
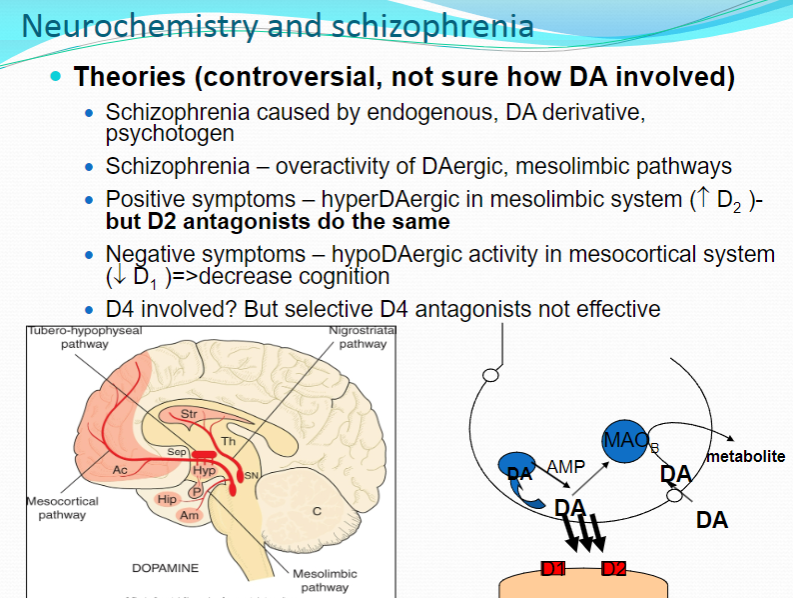
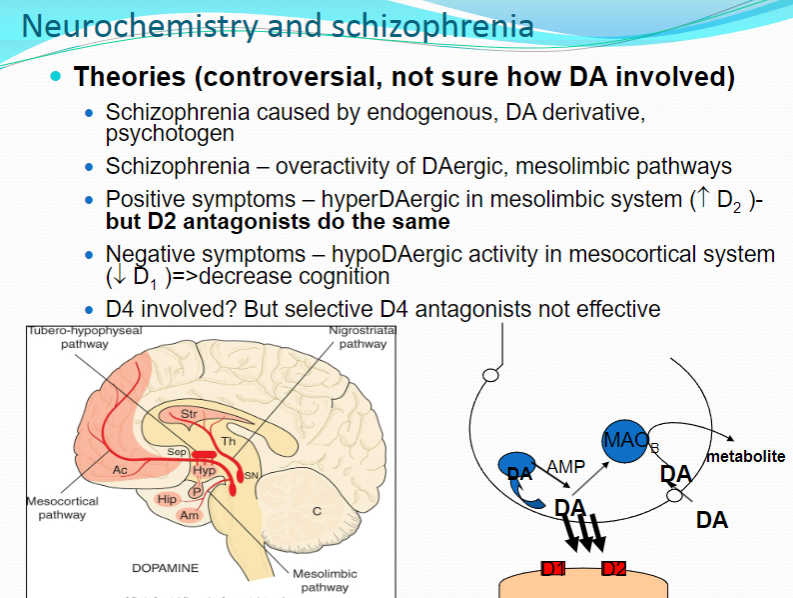
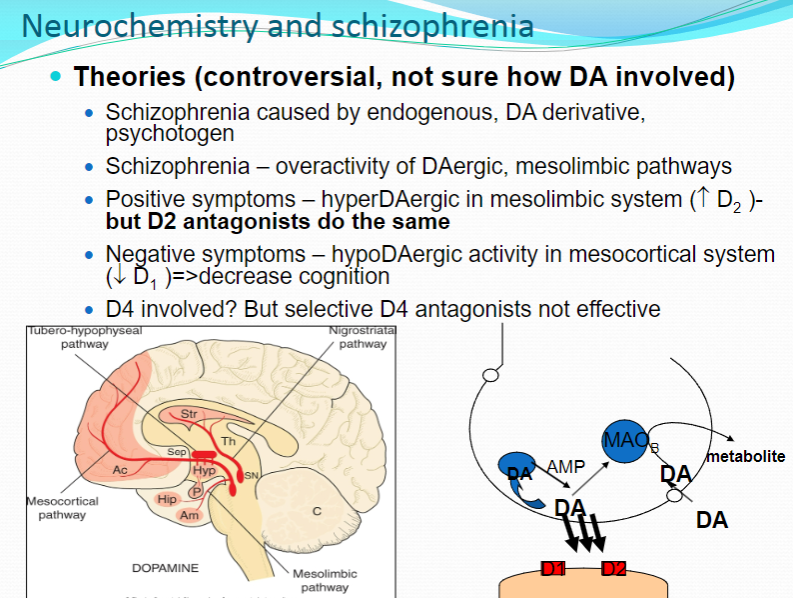
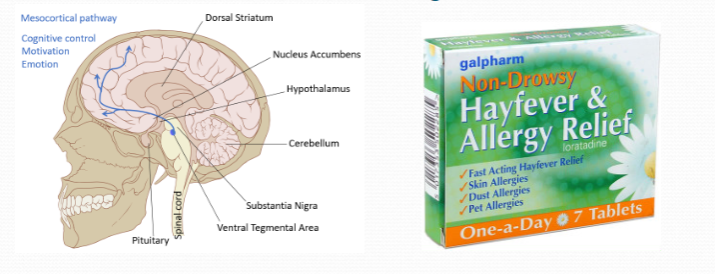
What are the main dopamine pathways and their functions? (5)
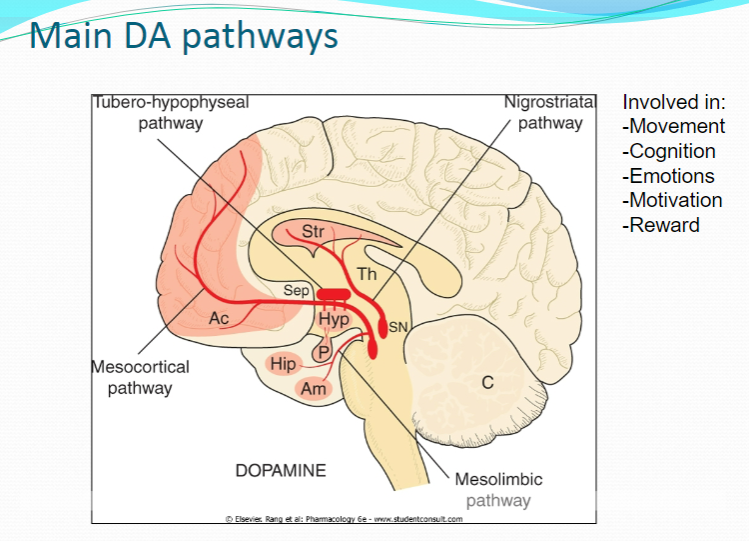
Movement
Dopamine is essential for motor control, with dysfunction linked to movement disorders like Parkinson's disease.
Cognition
Dopamine plays a role in cognitive processes, including attention, memory, and problem-solving.
Emotions
Dopamine is involved in regulating emotional responses, affecting mood and emotional stability.
Motivation
Dopamine influences motivation and goal-directed behavior, impacting drive and reward-seeking actions.
Reward
Dopamine is central to the brain's reward system, reinforcing behaviors by releasing dopamine in response to pleasurable stimuli.
-
What is the dopamine hypothesis of schizophrenia? (1)
Schizophrenia is associated with overactivity of dopamine (DA) in specific brain regions, particularly in the mesolimbic pathways, leading to positive symptoms such as hallucinations and delusions.
-
What is the role of hyperdopaminergic activity in the mesolimbic system in schizophrenia? (3)
Hyperdopaminergic activity in the mesolimbic system is linked to positive symptoms (e.g., hallucinations, delusions).
Increased D2 receptor activity is a key feature of this overactivity.
D2 antagonists, like antipsychotic drugs, work by blocking these receptors, reducing the positive symptoms.
-
How does hypodopaminergic activity in the mesocortical system contribute to negative symptoms in schizophrenia? (2)
Hypodopaminergic activity (low dopamine levels) in the mesocortical system is associated with negative symptoms of schizophrenia, including cognitive deficits and emotional flatness.
This is linked to decreased D1 receptor activity, contributing to impaired cognition and motivation.
-
What is the role of the D4 receptor in schizophrenia? (1)
The D4 receptor may be involved in schizophrenia, but selective D4 antagonists have not been effective in treating the disorder, suggesting that its role might not be as significant as previously thought.
-
What is the theory involving endogenous dopamine derivatives or psychotogens in schizophrenia? (2)
One theory suggests that schizophrenia could be caused by an endogenous dopamine derivative or a psychotogen (a substance that induces psychosis).
However, this theory remains controversial and the exact mechanism is not yet fully understood.
-
How does amphetamine contribute to the understanding of dopamine's role in schizophrenia? (2)
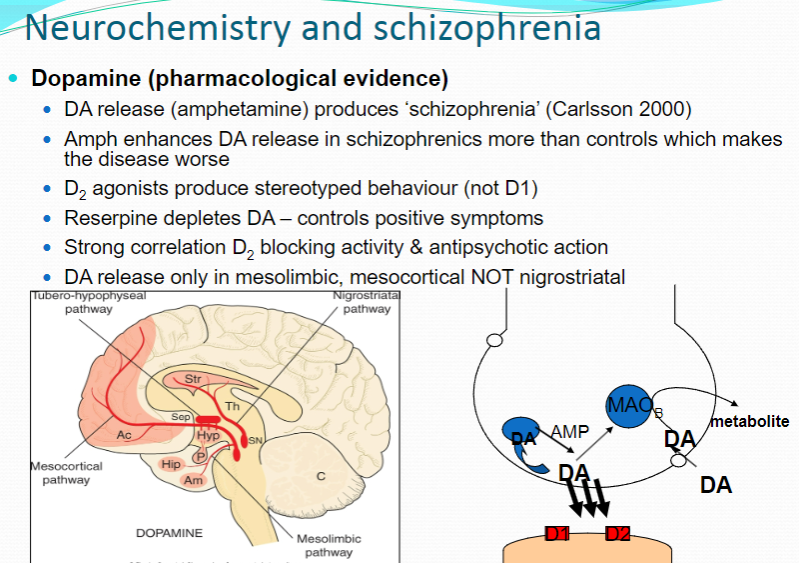
Amphetamine enhances dopamine (DA) release and produces schizophrenia-like symptoms (Carlsson 2000).
In schizophrenic patients, amphetamine enhances DA release more than in controls, which worsens the disease.
-
How do D2 agonists affect behavior in schizophrenia? (2)
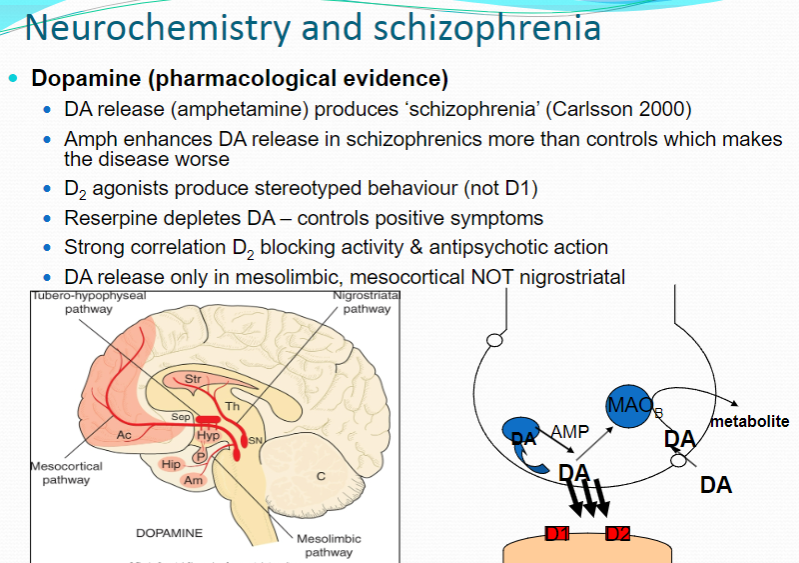
D2 agonists produce stereotyped behavior, which is characteristic of the overactivity of dopamine, particularly in the mesolimbic system.
D1 agonists do not cause this stereotyped behavior.
-
How does reserpine influence dopamine in the treatment of schizophrenia? (1)
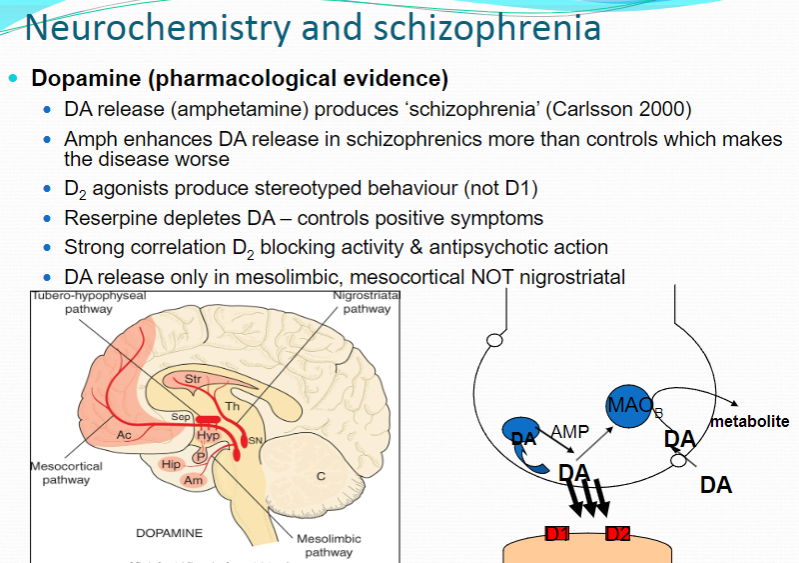
Reserpine depletes dopamine levels, which controls positive symptoms of schizophrenia by reducing dopamine activity in the brain.
-
What is the correlation between D2 receptor blocking and antipsychotic action in schizophrenia? (1)
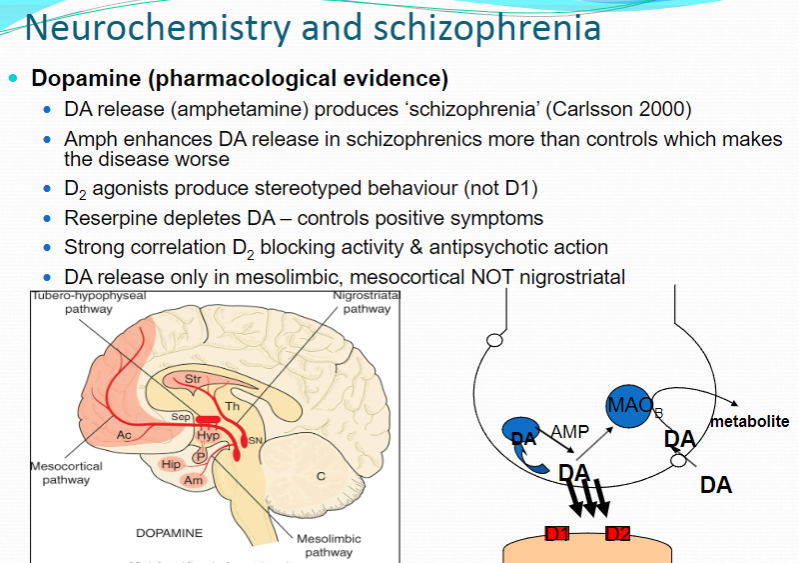
There is a strong correlation between D2 receptor blocking activity and the antipsychotic action of drugs used to treat schizophrenia.
-
How does dopamine release differ in the brain regions of schizophrenic patients? (1)
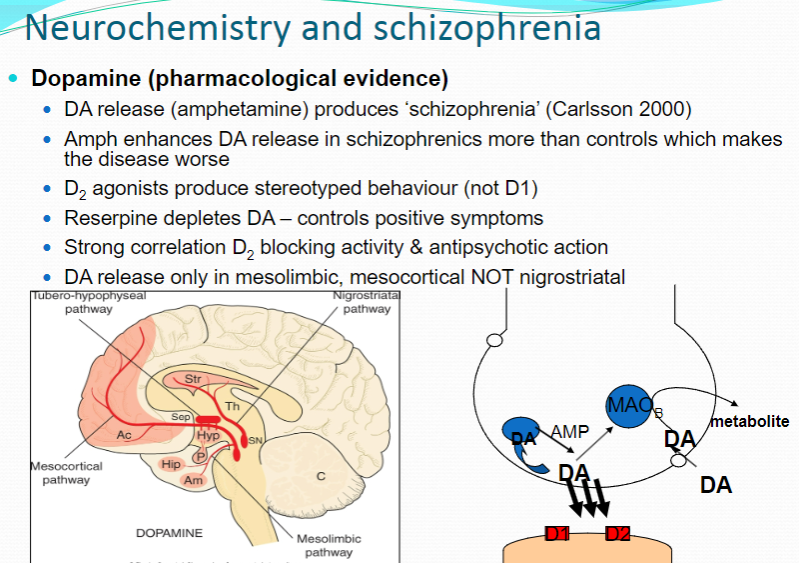
Dopamine release occurs specifically in the mesolimbic and mesocortical regions of the brain in schizophrenic patients, but not in the nigrostriatal pathway, which is involved in movement regulation
-
What is the evidence against the dopamine hypothesis of schizophrenia? (3)
No clear change in CSF HVA (Homovanillic Acid) concentration (a marker of dopamine activity).
No change in dopamine (DA) receptors in drug-free patients.
The increase in D2 receptors in samples is often attributed to drug treatment rather than intrinsic changes in the brain.
-
What are the key components of the pathophysiology of schizophrenia? (6)
Dopamine hypothesis
Brain structure differences
Hypofrontality (decreased activity in the prefrontal cortex)
NMDA receptor hypofunction (impaired glutamate signaling)
Serotonin involvement
Oxidative stress and neuroinflammation (damage to brain cells caused by inflammation and oxidative damage).
-
What are the overall brain structure abnormalities in schizophrenia? (3)
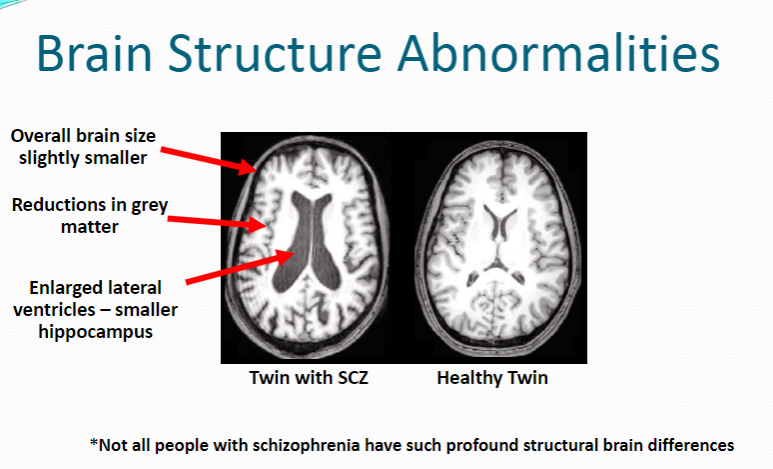
Slightly smaller brain size
Reductions in grey matter
Enlarged lateral ventricles and smaller hippocampus
-
How do brain structure abnormalities in schizophrenia compare between twins? (2)
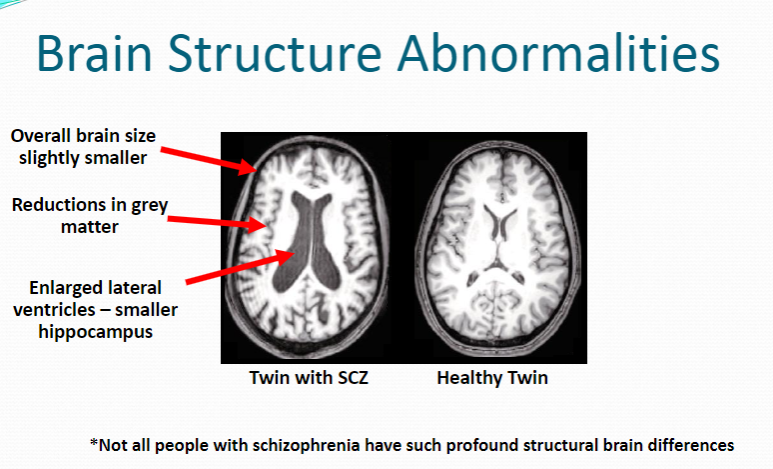
The twin with schizophrenia (SCZ) shows larger lateral ventricles and reduced grey matter.
The healthy twin does not show these significant structural differences.
-
What are the key components of the pathophysiology of schizophrenia? (6)
Dopamine hypothesis
Brain structure differences
Hypofrontality
NMDA receptor hypofunction
Oxidative stress
Neuroinflammation
-
What is hypofrontality in schizophrenia and what is its impact? (2)
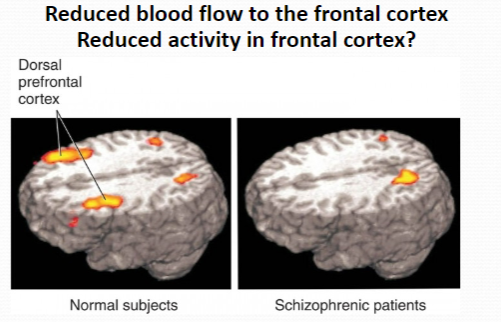
Reduced blood flow to the frontal cortex
Reduced activity in the frontal cortex
-
What is the role of the frontal cortex, and how could its reduced activity explain some symptoms in schizophrenia? (3)
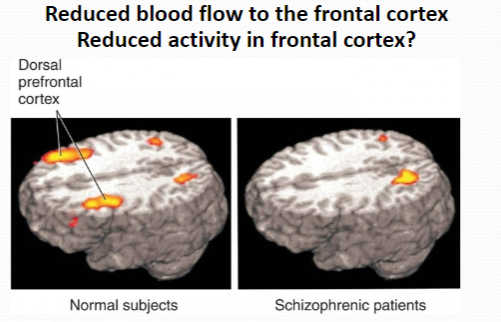
Role of the frontal cortex: Involved in higher cognitive functions, including decision making, planning, social behavior, and working memory.
Symptoms related to reduced frontal activity:
Cognitive deficits (e.g., impaired memory and attention)
Negative symptoms (e.g., lack of motivation, social withdrawal)
Difficulty with executive functioning (e.g., poor decision making, inability to plan or organize)
-
What is the role of glutamate in schizophrenia, and where does it act? (2)
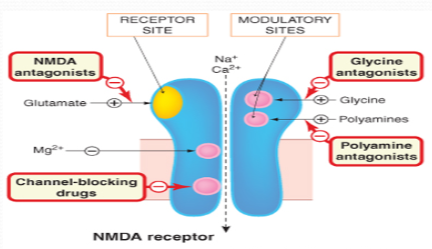
Neurotransmitter involved: Glutamate
Action: Acts on NMDA receptors in the prefrontal cortex and other brain regions.
-
How do NMDA antagonists like ketamine and phencyclidine (PCP) relate to psychotic symptoms in schizophrenia? (3)
Psychotic symptoms: Induce hallucinations and thought disorders similar to those seen in schizophrenia
Mechanism: Block NMDA receptors, leading to a reduction in glutamate activity
Symptoms observed: Stereotyped behaviors, social withdrawal, and cognitive disturbances.
-
How does glutamate dysfunction contribute to schizophrenia? (3)
Decreased glutamate levels and reduced glutamate receptor density in the prefrontal cortex
Transgenic mice with reduced NMDA receptor expression show symptoms similar to schizophrenia, including:
Stereotyped behavior
Decreased social interaction
Responsiveness to antipsychotics
-
What is the role of serotonin (5-HT) in schizophrenia, based on current evidence? (3)
LSD: A partial 5-HT agonist known to induce hallucinations, demonstrating serotonin’s role in psychosis.
Antipsychotics: Many target and antagonize 5-HT receptors, suggesting serotonin's involvement in the pathophysiology of schizophrenia.
Current theory: Overstimulation of mesolimbic D2 receptors, hypoactivity of frontal cortical D1 receptors, and reduced prefrontal glutaminergic activity are key mechanisms in schizophrenia, with 5-HT playing a role in this dysfunction.
-
What are some drugs used to treat schizophrenia, and how do they work? (2)
Antipsychotics: D2 receptor antagonists and 5-HT receptor antagonists help treat symptoms.
Example drugs: Atypical antipsychotics (e.g., clozapine, risperidone) target both dopamine and serotonin receptors to balance the activity of these neurotransmitters.
-
What are the types of treatment for schizophrenia? (2)
Pharmacological: Includes antipsychotics that target dopamine and serotonin receptors.
Psychotherapeutic: Cognitive Behavioral Therapy (CBT) aims to help patients manage symptoms and reduce the distress caused by hallucinations or delusions.
-
What are the current and future therapies for schizophrenia? (2)
Current therapies: Antipsychotic medications (e.g., atypical and typical antipsychotics) to manage positive symptoms (hallucinations, delusions).
Future therapies: Research is ongoing for targeted treatments involving glutamate, serotonin, and novel drug classes that may offer better symptom management with fewer side effects.
-
How does Electroconvulsive Therapy (ECT) play a role in treating schizophrenia? (1)
ECT is used in severe cases of schizophrenia, particularly when medications are ineffective or symptoms are life-threatening, and it involves applying electrical currents to induce controlled seizures, which may help reset brain activity.
-
What are typical (first-generation) antipsychotics, and how do they work? (2)
Typical antipsychotics: Also known as first-generation antipsychotics, developed in the 1950s.
Mechanism: Primarily antagonize D2 receptors, which helps reduce positive symptoms of schizophrenia.
-
What are atypical (second-generation) antipsychotics, and how do they work? (2)
Atypical antipsychotics: Also known as second-generation antipsychotics, developed in the 1980s.
Mechanism: Primarily antagonize both D2 and 5-HT2A receptors, targeting both dopamine and serotonin systems to manage positive and negative symptoms.
-
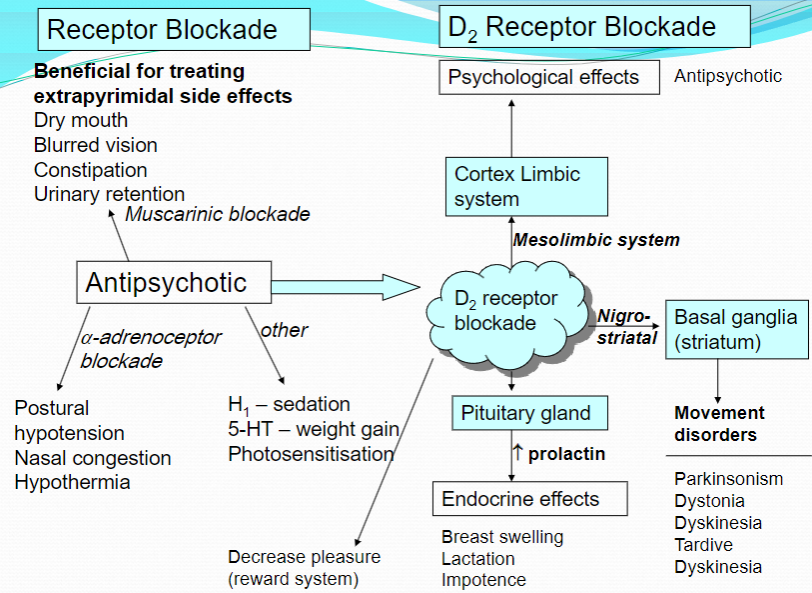
Picture demonstrating Receptor blockades and their effects:
-
What causes sedation in antipsychotics? (2)
D2 receptor antagonism: Blocking D2 receptors can lead to sedation due to its effects on dopamine-related pathways.
Central H1 receptor antagonism: Antagonizing histamine H1 receptors in the central nervous system also contributes to sedative effects.
-
What are the side effects of antipsychotics related to prolactin? (4)
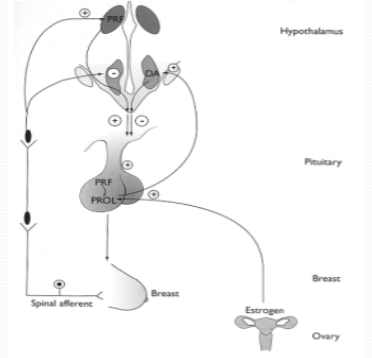
Increased prolactin secretion: Antipsychotics can cause an increase in prolactin levels.
Gynaecomastia: Increased prolactin can lead to the development of breast tissue in males.
Milk secretion: Prolactin increases can cause galactorrhea, or spontaneous milk secretion.
Menstrual irregularities and impotence: Women may experience menstrual cycle disruptions, and men may have impotence due to the hormonal imbalance.
-
How does hypotension occur as a side effect of antipsychotics? (2)
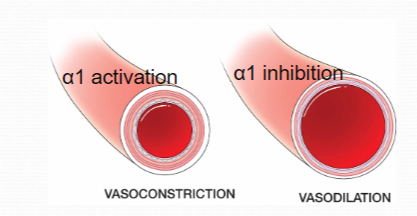
α1-adrenoceptor antagonism: Antipsychotics can block α1-adrenoceptors, which are involved in vasoconstriction.
Leads to hypotension: Blocking these receptors can cause dilation of blood vessels, resulting in lower blood pressure (hypotension).
-
What are the anticholinergic effects of antipsychotics? (5)

Dry mouth: Muscarinic acetylcholine receptor (mAChR) antagonism decreases salivary secretions.
Blurred vision: Pupillary muscles are affected by the blockade, causing blurred vision.
Constipation and Urinary retention: Smooth muscle contraction is reduced, leading to constipation and urinary retention.
Alleviation of EPSE symptoms: Blockade of mAChRs at the neuromuscular junction helps alleviate extrapyramidal symptoms (EPSEs) like tremors and rigidity.
Cognitive impact: Anticholinergics may have a detrimental impact on cognition, reducing mental clarity.
-
What is Anhedonia? (1)
Anhedonia is the inability to feel pleasure in normally pleasurable activities
-
What is the definition of Aetiology? (1)
Aetiology refers to the cause or set of causes that lead to a disease or condition.
-
What is a Candidate Gene? (1)
A candidate gene is any gene thought to be likely to cause a disease.
-
What is the difference between Candidate Gene and Risk Gene? (1)
A risk gene is essentially a candidate gene that increases the likelihood of developing a particular condition or disease.
-
What is Cognitive Behavioural Therapy (CBT)? (1)
CBT is a type of psychotherapy in which negative thought patterns about oneself and the world are challenged in order to alter unwanted behavior patterns or treat mood disorders like depression.
-
What is Electroconvulsive Therapy (ECT)? (1)
ECT is a treatment that involves sending an electric current through the brain to trigger an epileptic seizure to relieve symptoms of some mental health conditions.
-
What is the Mesocortical Pathway? (1)
The mesocortical pathway is a dopaminergic pathway that connects the ventral tegmentum to the prefrontal cortex.
-
What is the Mesolimbic Pathway? (1)
The mesolimbic pathway is a dopaminergic pathway that connects the ventral tegmental area in the midbrain to the ventral striatum of the basal ganglia in the forebrain.
-
What is the Nigrostriatal Pathway? (1)
The nigrostriatal pathway is a dopaminergic pathway that connects the substantia nigra pars compacta (SNc) with the dorsal striatum (caudate nucleus and putamen).
-
What is the Tuberoinfundibular Pathway? (1)
The tuberoinfundibular pathway consists of dopamine neurons that project from the arcuate nucleus (infundibular nucleus) in the tuberal region of the hypothalamus to the median eminence.
-
What is Prolactin? (1)
Prolactin is a hormone released from the anterior pituitary gland that stimulates milk production after childbirth.
-
What are Antipsychotics? (1)
Antipsychotics are a class of drugs designed to treat severe psychiatric conditions such as schizophrenia.
-
What are Extra-pyramidal Side Effects (EPSEs)? (1)
EPSEs are serious side-effects of antipsychotic and other drugs that affect movement
-
What is Agranulocytosis? (1)
Agranulocytosis is a deficiency of granulocytes in the blood, which causes an increased vulnerability to infection.

