Reflex control of the circulation (Physiology)
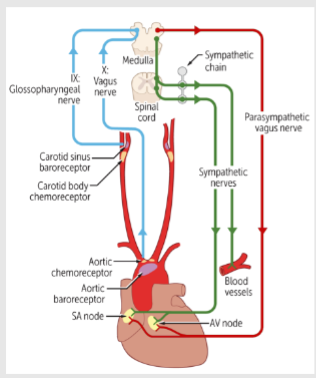
Session summary This lecture examines some of the different reflexes affecting the circulation and how they are controlled. Modulation of reflex control of the circulation by central pathways in the brain is discussed. Much of the time reflexes are trying to control or regulate blood pressure involving baroreceptors, metaboreceptors and arterial chemoreceptors. The neural pathways and mechanisms integrating these responses are explored. Learning outcomes At the end of this session you will be able to: Outline the stimulation of sensory receptors Arterial baroreceptors Cardiac receptors Arterial chemoreceptor Muscle metaboreceptors Outline the features of central pathways Medulla relay station (nucleus tractus solitarius) Vagal motor neurons (nucleus ambiguus) Pre-sympathetic neurons (RVLM) Explain the effects on BP (via sympathetic and vagus nerves) Heart - Heart Rate, Contractility Resistance vessels – TPR Veins - CVP
-
What are arterial baroreceptors?
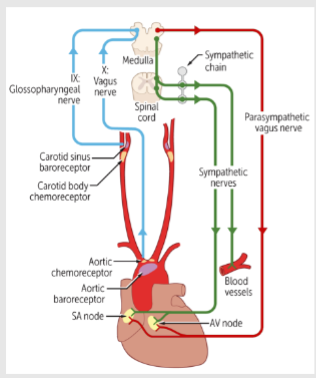
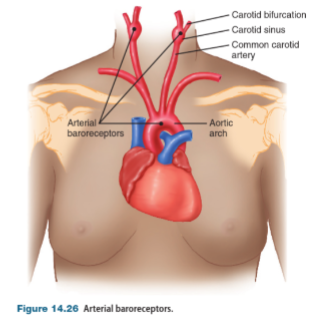
Arterial baroreceptors are blood pressure sensors located in the walls of the carotid arteries and aorta.
They inform the brain of pressure changes in these key feeder vessels by detecting arterial wall stretch
-
Why are arterial baroreceptors vital?
Arterial baroreceptors are vital for maintaining blood flow to the brain and myocardium.
They play a crucial role in regulating blood pressure by detecting changes in arterial pressure and signaling the brain to make necessary adjustments
-
What information do arterial baroreceptors provide?
Arterial baroreceptors monitor blood pressure changes, reflecting alterations in either cardiac output (CO) or total peripheral resistance (TPR).
A decrease in arterial pressure (Pa) indicates a decrease in either cardiac output or total peripheral resistance, compromising blood flow to the brain and heart.
-
How is blood flow related to arterial pressure?
Blood flow (CO) is determined by dividing arterial pressure (Pa) by total peripheral resistance (TPR).
The formula for blood flow is CO = Pa / TPR, where CO represents cardiac output.
-
How do baroreceptors respond to changes in pressure?
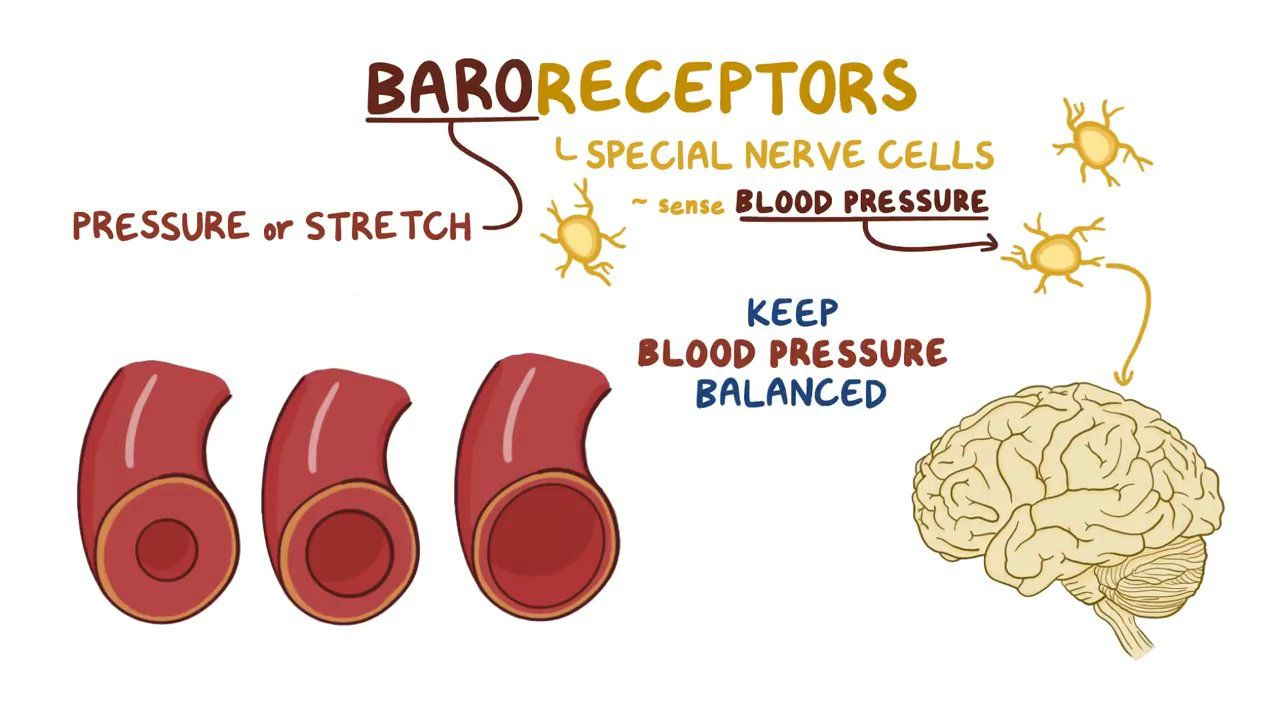
Baroreceptors respond to changes in pressure by adjusting their firing rate.
An increase in pressure initially results in minimal firing at rest, followed by fast firing which eventually slows down and becomes constant, albeit at a higher level than before, reflecting adaptation to a new normal.
-
What happens when there is a decrease in pressure?
A decrease in pressure leads to a proportionate slowing down of firing in baroreceptors
-
How does prolonged exposure to high or low pressure affect baroreceptor activation?
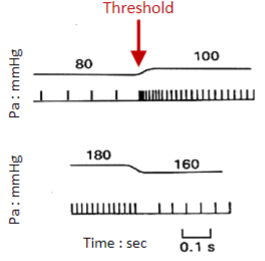
In the face of continued high or low pressure, the threshold for baroreceptor activation can change.
For example, in long-term hypertension, baroreceptors may become normalized to the new pressure level and consequently less activated
-
Picture demonstrating how baroreceptors respond to pressure:

-
Picture demonstrating the location of the Arterial baroreceptors:
-
What is the effect of increased blood pressure (BP) on the baroreflex? (4)
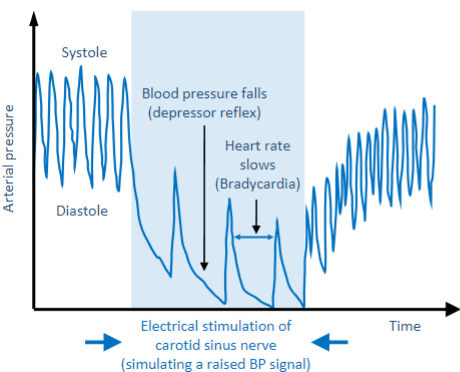
An increase in BP, termed loading (e.g., due to stress or exercise), leads to several responses:
-Pulse pressure (compliance) falls due to decreased stroke volume
-Vasodilation decreases total peripheral resistance (TPR) and BP
-There is a decrease in sympathetic nerve activity.
-Vagus nerve activity increases (parasympathetic activity)
-
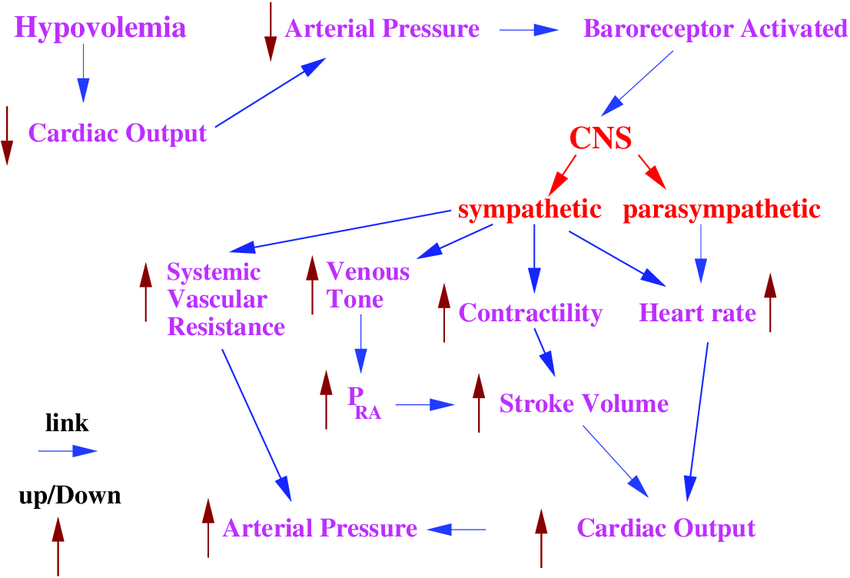
What is the effect of decreased blood pressure (BP) on the baroreflex? (4)
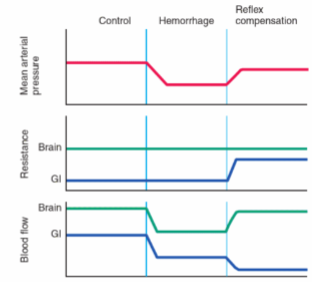
A decrease in BP, termed unloading (e.g., due to hemorrhage), results in the following responses:
-Increased sympathetic activity and decreased vagus nerve activity.
-Increased heart rate (HR) and force of contraction, leading to increased cardiac output.
-Arteriolar constriction increases total peripheral resistance (TPR).
-Venous constriction increases central venous pressure, leading to increased stroke volume and cardiac output by Starling's law.
These responses collectively maintain blood pressure and blood flow to vital organs
-
What hormonal responses occur during decreased BP?
In response to decreased BP, adrenaline secretion, vasopressin (ADH) secretion, and stimulation of the renin-angiotensin-aldosterone system (RAAS) occur.
Angiotensin II increases Na+/H2O absorption in the kidneys, raising blood volume
-
How does Arterial vasoconstriction contribute to maintaining blood volume during decreased BP?
Arterial Vasoconstriction decreases capillary pressure, which increases absorption of interstitial fluid, thereby increasing blood volume
-
A picture demonstrating baroreceptor-mediated responses to hemmorrhage:

-
A picture demonstrating the effects of a hemorrhage-induced baroreceptor reflex on mean arterial pressure, on vascular resistance, and on blood flow in the brain and gastrointestinal tract:
-
What are the cardiac receptors and afferent nerves involved in cardiovascular regulation? (4)
-Veno-atrial mechanoreceptors
-Ventricular mechanoreceptors
-Nociceptive sympathetic afferents
-Nucleus tractus solitarius (NTS)
-
Elaborate on Veno-atrial mechanoreceptors (what is it stimulated by etc) (3)
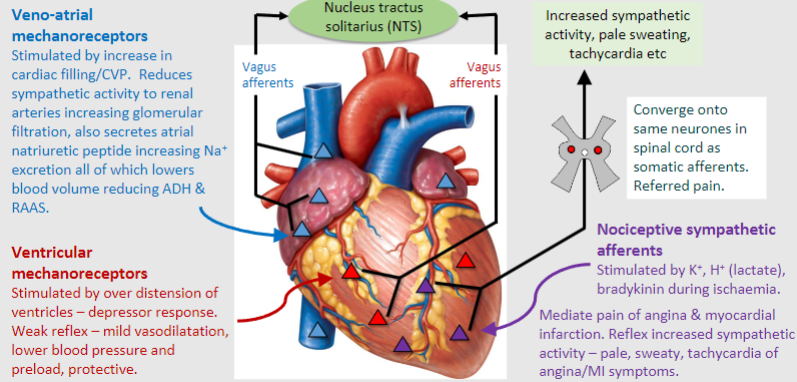
-Stimulated by an increase in cardiac filling or central venous pressure (CVP)
-Reduces sympathetic activity to renal arteries, increasing glomerular filtration
-Secretes atrial natriuretic peptide, increasing sodium excretion, which lowers blood volume and reduces ADH (antidiuretic hormone) and RAAS (renin-angiotensin-aldosterone system) activity
-
Elaborate on Ventricular mechanoreceptors (what is it stimulated by and what does it result in) (2)
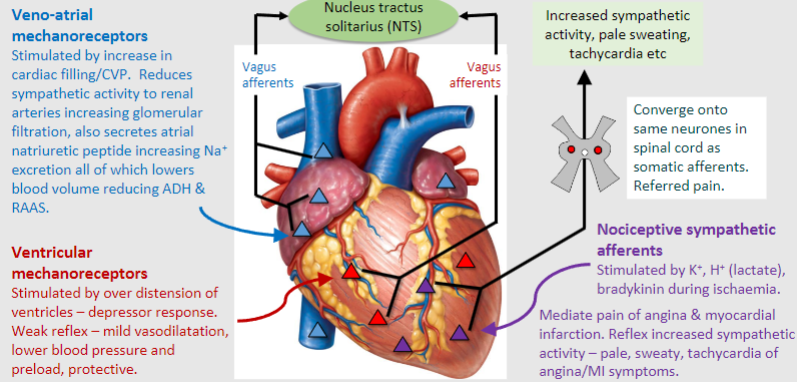
-Stimulated by over-distension of ventricles, leading to the depressor response (A response to lower blood pressure)
-Results in mild vasodilatation, lower blood pressure, and preload reduction, serving as a protective mechanism
-
Elaborate on Nociceptive sympathetic afferents (what is it stimulated by etc) (3)
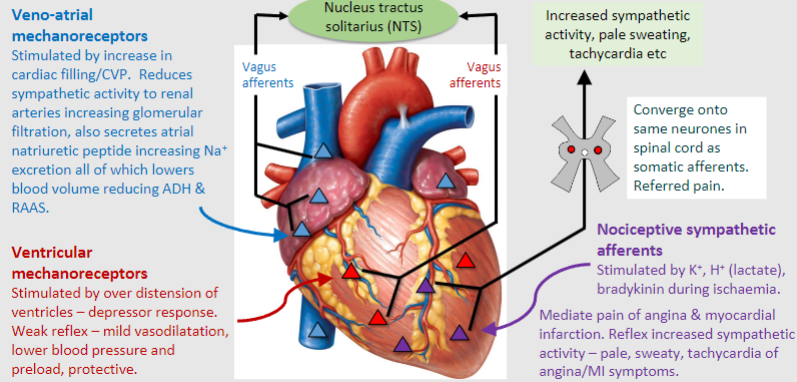
-Stimulated by substances such as potassium (K+), hydrogen ions (H+), lactate, and bradykinin during ischemia
-Converge onto the same neurons in the spinal cord as somatic afferents, leading to referred pain
-Mediate the pain of angina and myocardial infarction, and reflexively increase sympathetic activity, manifesting as symptoms like pallor, sweating, and tachycardia
-
Elaborate on Nucleus tractus solitarius (NTS) (what is it stimulated by etc) (1)
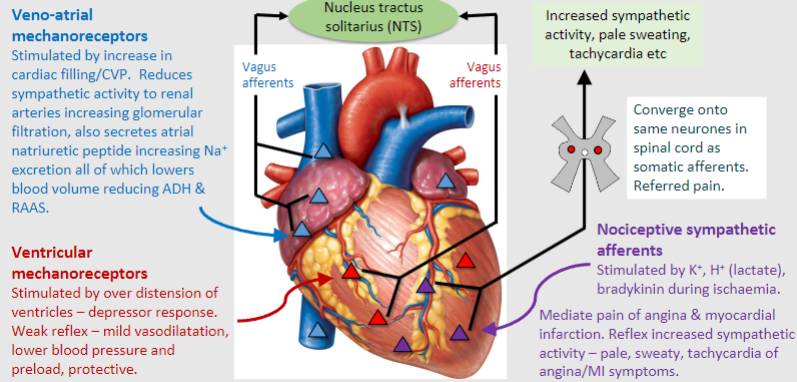
An integrative centre in the brainstem involved in cardiovascular regulation, respiratory, gustatory (taste), and visceral sensations from various organs.
-It is stimulated by Baroreceptors, Chemoreceptors, Visceral sensations and Taste sensation
-
What role do cardiovascular afferents play in stabilizing blood pressure?
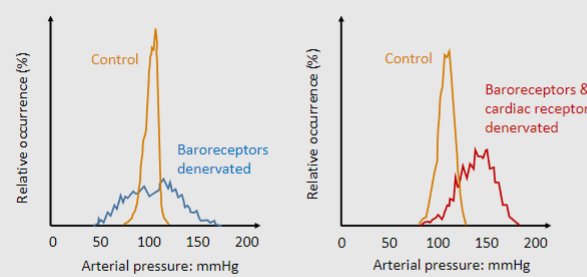
When afferent fibers from baroreceptors are removed:
-Arterial pressure varies enormously
-Means of regulation aren't significantly different
When afferent fibers from cardiac receptors are also removed:
-Arterial pressure still varies significantly
-The means of regulation become notably different
-
What are the potential consequences of deviations from normal arterial pressure? (3)
-Normally, arterial pressure remains relatively stable around 100 mmHg
-A decrease to 50 mmHg could cause insufficient perfusion to end organs
-An increase to 150 mmHg could potentially damage the cardiovascular system
-
What are the characteristics of arterial chemoreceptors?(6)
-Located in carotid and aortic bodies
-Stimulated by low O2 (hypoxia), high CO2 (hypercapnia), H+, and K+
-Well supplied with blood flow around 20 ml/g/min
Regulate ventilation and drive cardiac reflexes during:
-Asphyxia (low O2/high CO2)
-Shock (systemic hypotension)
-Haemorrhage
-
What are the functions of arterial chemoreceptors? (3)
Pressor Response (Raising Blood Pressure):
-They activate sympathetic activity, leading to increased heart rate (tachycardia) and selective constriction of arteries and veins.
-This response enhances cardiac output and blood pressure, particularly to maintain adequate blood flow to the brain.
-Even when blood pressure falls below the range of the baroreflex (the body's automatic blood pressure regulation system), chemoreceptors remain active and may compensate to stabilize blood pressure.
-
What are muscle metaboreceptors and their characteristics? (2)
Sensory fibers in Group IV motor fibers located in skeletal muscle.
Activated via metabolites: K+, lactate, adenosine.
-
What is the pressor response triggered by muscle metaboreceptors? (4)
Increase sympathetic activity.
Tachycardia.
Increase arterial/venous constriction.
Increase cardiac output/blood pressure.
-
When are muscle metaboreceptors particularly important, and what function do they serve during exercise? (4)
Important during isometric exercise.
Occurs when muscles are continually contracted without changes in joint angle or muscle length (e.g., weight lifting/handgrip).
Higher blood pressure drives blood into the contracted muscle to maintain perfusion.
These muscles undergo metabolic hyperaemia, allowing blood flow to the contracted tissue.
-
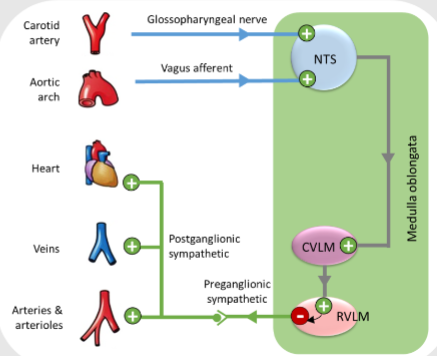
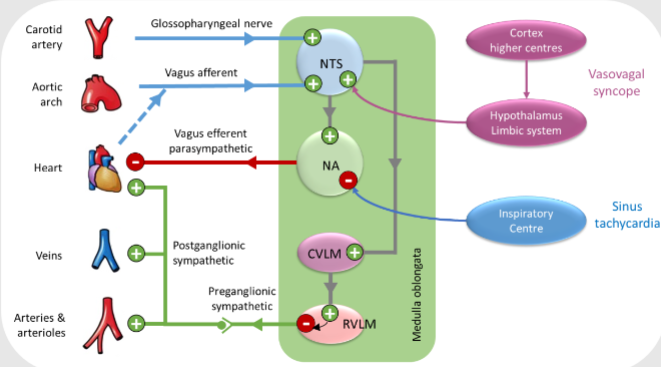
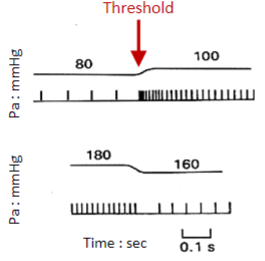
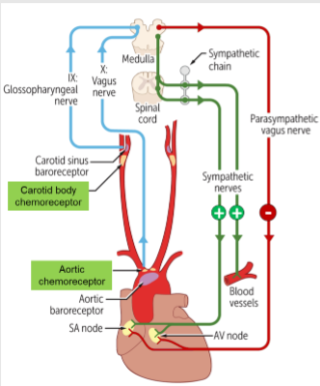
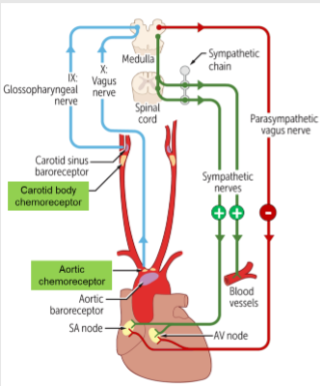
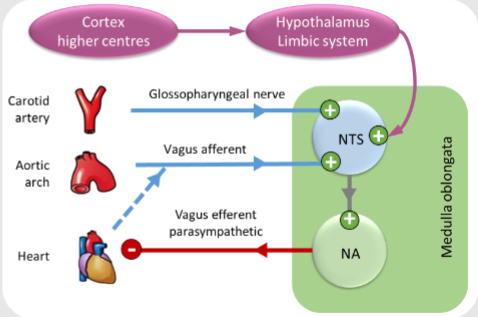
State the 5 steps of the central role of the nucleus tractus solitarius (NTS, CVLM and RVLM)
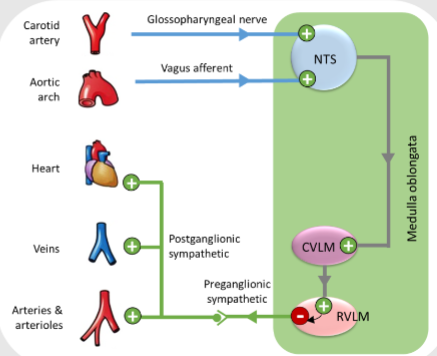
1. Signal from stretched baroreceptor sent via afferent fibres enter Nucleus Tractus Solitarius (NTS)
2. This then sends information out to the Caudal Ventrolateral Medulla (CVLM)
3. The CVLM sends information to the rostral ventrolateral medulla (RVLM)
4. This results in INHIBITION of sympathetic efferent nerves to heart and vessels
5. Less sympathetic efferent signals result in reduction in HR, less vasoconstriction, lower BP etc
-
How do vagus parasympathetic impulses influence the heart? (3)
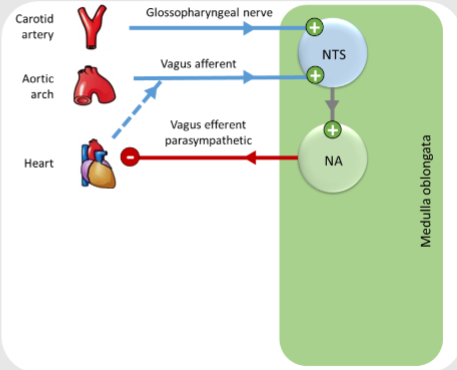
-Loading of the baroreceptors (stretching or deformation due to changes in blood pressure) stimulates the vagus nerve, activating the Nucleus Tractus Solitarius (NTS)
-The signal from the NTS stimulates the nucleus ambiguous (vagal nuclei)
-Vagal parasympathetic impulses are sent to the heart, exerting a depressor effect (a sustained and long-lasting increase in blood pressure resulting from an increase in peripheral vascular resistance)
-
How does vagal parasympathetic outflow contribute to sinus tachycardia? (4)
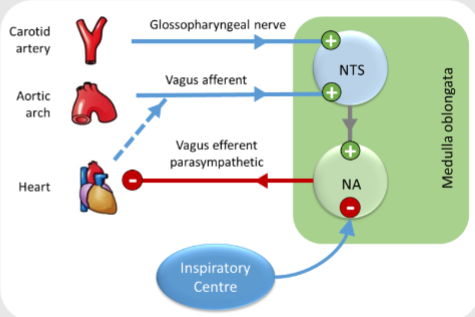
-Vagal parasympathetic outflow exerts inhibitory control over heart rate by releasing acetylcholine onto muscarinic receptors in the sinoatrial node.
-Decreased vagal tone or withdrawal of vagal input allows sympathetic influence to predominate, leading to an increase in heart rate.
-Sinus tachycardia often occurs in response to stress, exercise, or other factors that increase sympathetic activity or reduce parasympathetic tone.
-Respiratory sinus arrhythmia may modulate heart rate during the respiratory cycle, with slight increases in heart rate during inspiration due to reduced vagal activity.
-
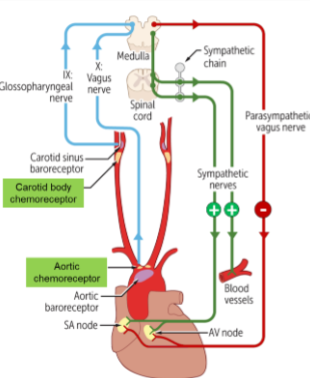
What role does the limbic system play in cardiovascular regulation?
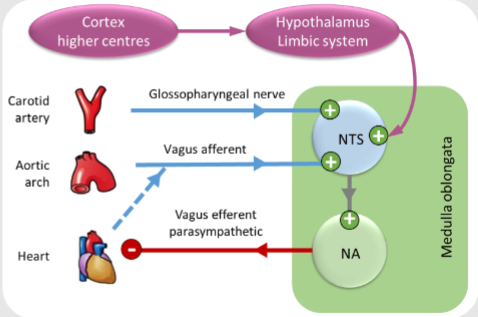
The limbic system, known as the emotional center, stimulates the Nucleus Tractus Solitarius (NTS)
The NTS then activates the nucleus ambiguus, leading to increased activity of the vagal nerve
This results in a depressor effect on the atrioventricular (AV) and sinoatrial (SA) nodes
-

How can activation of the limbic system lead to syncope (fainting)?
Activation of the limbic system can trigger a vasovagal attack
Syncope, or fainting, can occur due to a sudden drop in arterial cardiac output and blood pressure
This leads to decreased cerebral blood flow, resulting in syncope
-
A picture summary of the medulla oblongata: