
Red Blood Cell production and Survival (Pathology)
Topics covered: The origin and control of red blood cell production The central role of iron in haemoglobin structure, and in erythropoiesis Causes of iron deficiency and their clinical effects Role of vitamin B12 and folic acid in erythropoiesis B12 and folate deficiency disorders Other causes of failure of red cell production. The normal red cell life span and the consequence of red cell destruction Factors affecting red cell survival Classification of haemolytic anaemia. Session resources 1. Hoffbrand 's Essential Haematology: Hoffbrand and Moss. Wiley-Blackwell, 7th Edition, 2016 2. Haematology - Lecture Notes: Hatton, Hughes-Jones, Hay and Keeling, 9th Ed, 2013.
-
How much RBC are produced a day in the average human body?
2x10^11
-
What is the first recognisable RBC precursor in marrow?
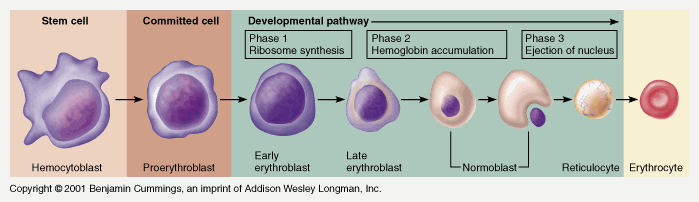
Proerythroblast
-
FILL IN THE BLANKS:
Regulation of RBC production
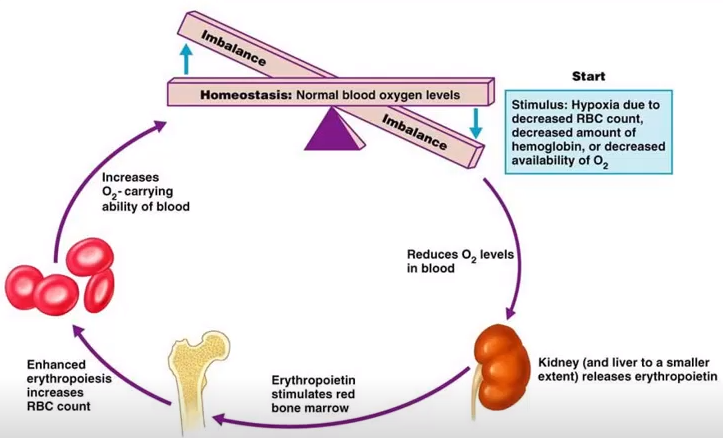
Number of RBC is _________ related to ambient O2 pressure. A key regulator of the feedback loop is _____
1)Inversely
2)EPO (Erythropoietin)
-
Picture demonstrating the feedback loop
-
Studies of EPO regulation led to the discovery of what?
Hypoxia-inducible factor (HIF) is a sensor of hypoxia and a regulator of the cellular hypoxic response
-
HIF enhances the expression of what gene?
An iron-absorbing gene
-
What is Iron regulated by?
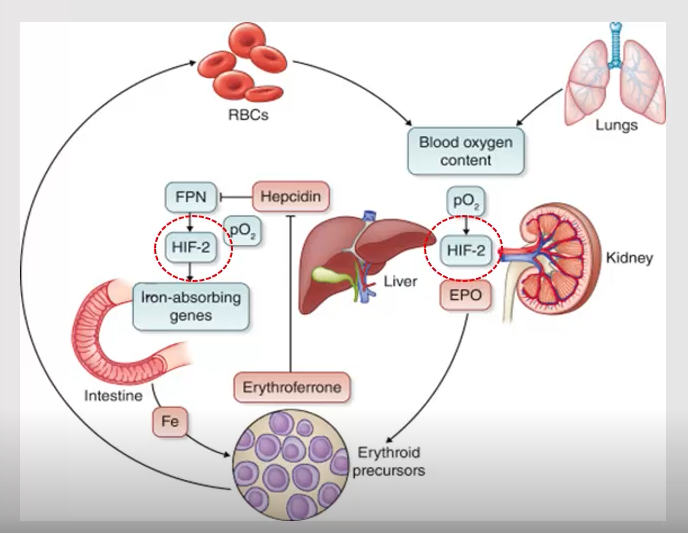
Hepcidin
-
What are some foods that are sources of Iron?
Meat, eggs, vegetables, dairy foods
-
How much iron does the western diet provide daily?
15mg daily
-
FILL IN THE BLANKS:
Absorption
-5-10% absorbed (1mg) principally in __________ and __________.-Gastric secretion (HCl) and _________ _______ help absorption.-__________ and __________ regulate absorption
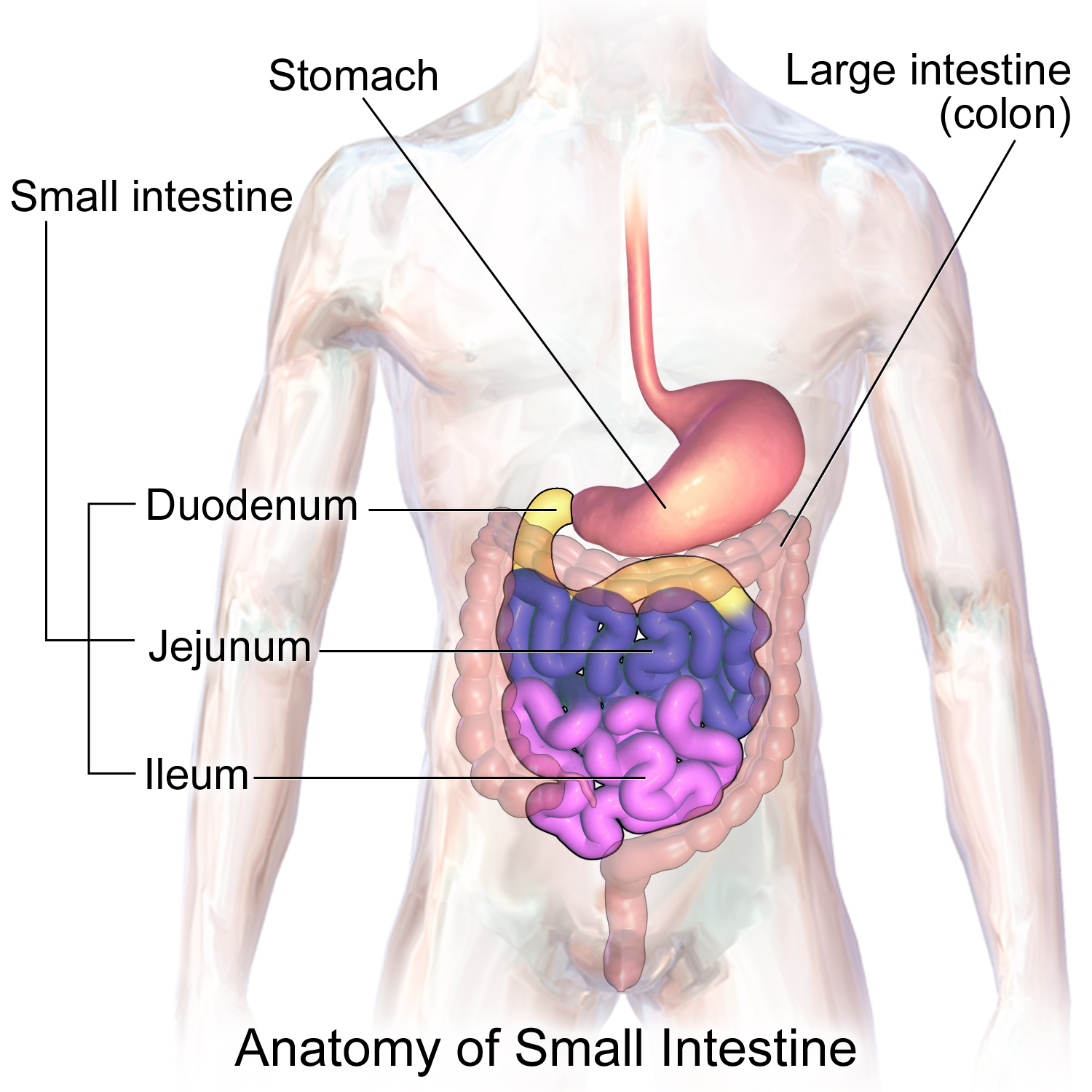
-5-10% absorbed (1mg) principally in duodenum and jejunum.-Gastric secretion (HCl) and ascorbic acid help absorption.-DMT-1 and ferroportin regulate absorption
-
What is the role of iron in haemoglobin?
-Role: in haemoglobin, binds to O2
-
What are the four main causes of Iron deficiency?
1)Poor diet
+Inadequate intake
+Malabsorption
2)Increased demand
+Pregnancy
+Growth spurt
3)Chronic blood loss
+GI bleed
+Excess loss in menses
4)Malabsorption
+Food intolerance e.g. lactose
+Illness
-
What foods can B12 be found in?
B12, is found in liver, meat, fish and dairy products,fruits & vegetables.
-
B12 is absorbed where? Bound to what factor?
It is absorbed in the ileum, bound to intrinsic factor (IF)
-
Folate is absorbed where? In what form is it absorbed in?
Folate is absorbed in duodenum & jejunum in the form of MTHF
-
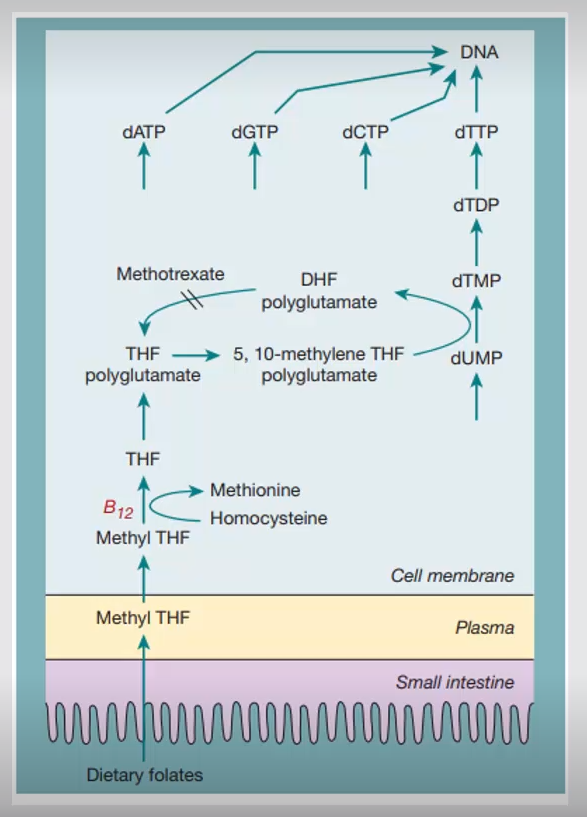
What is B12 and Folate both essential and needed for?
-Both essential for DNA synthesis & RBC maturation.-Both needed for formation of thymidine triphosphate
-
B12 is also a coenzyme for what?
Methione synthase in methylation of homocysteine to methionine
-
STATEMENT: B12 deficiency leads to a failure of nuclear maturation
Is this True or false?
TRUE
-
Picture demonstrating the role of B12 and folate in Erythropoiesis
-
What are the three main causes of Vitamin B12 deficiency?
1)Inadequate intake
+Vegans
2)Absorption defect
+Tropical Sprue (a malabsorption syndrome)
+Coeliac dx (parts of the digestive system become inflamed)
3)IF deficiency
+Pernicious anaemia
+Crohn's
+Gastrectomy and Others
-
What are the three main causes of Vitamin Folate deficiency?
1)Inadequate intake
+Poor nutrition
2)Absorption defect
+Coeliac disease
+Chrons dx
+Tropical sprue
3)AN INCREASE in either Demand/Losses
+Pregnancy
+Haemolysis
+Cancer
4)Drugs
+Anticonvulsants
-
What else can affect RBC production?
-Renal dx - ineffective erythropoieses
-Reduced BM (Bone Marrow) erythroid Cells
-
FILL IN THE BLANKS:
RBC Metabolism and Survival
-Components needed for function and survival are present in _________ _______.-Function does not require the _________ of much energy.-RBC are capable of _________ metabolic activity.
-Components needed for function and survival are present in matured RBC.-Function does not require the consumption of much energy.-RBC are capable of limited metabolic activity.
-
Metabolic processes include? (3)
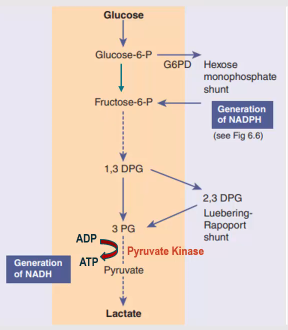
-Glycolytic (Embden-Meyerhof) pathway
-Hexose Monophosphate shunt (or PPP)
-Rapoport-Luebering shunt
-
What are the three main purposes of the Glycolytic (Embden-Meyerhof) pathway ?
-Generates energy in ATP;-To maintain red cell shape and deformability, flexibility-To regulate intracellular cation conc. via cation pumps(Na/K pump).
-
Outline the Glycolytic (Embden-Meyerhof) pathway
-
What happens during a Pyruvate Kinase (PK) deficiency?
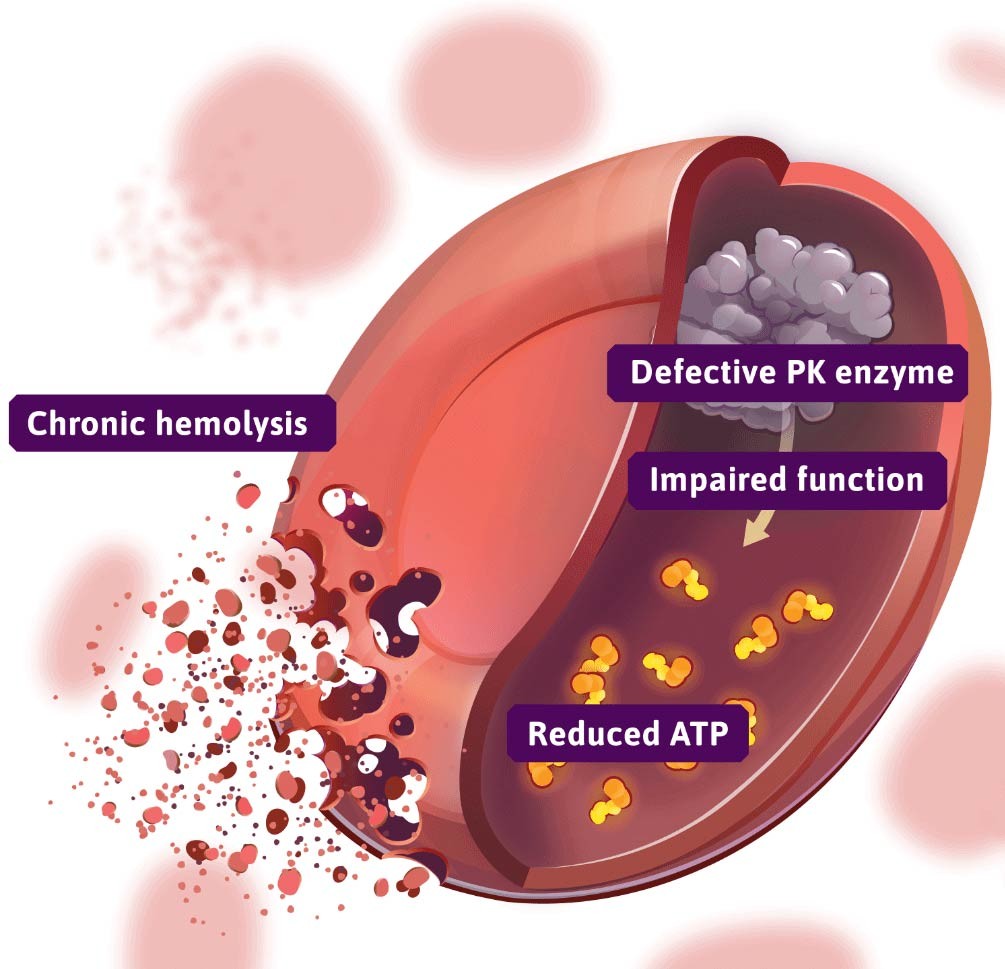
-ATP is depleted
-Cells lose large amount of potassium & water, becoming dehydrated & rigid.
-Causes chronic non-spherocytic haemolytic anaemia
-
What are the purposes of the Hexose Monophosphate shunt (or PPP/Pentose phosphate pathway)?
-The HMP shunt is an alternative pathway to glycolysis and is used to produce ribose-5-phosphate and nicotinamide adenine dinucleotide phosphate (NADPH).
-
Outline the Hexose Monophosphate shunt (or PPP)
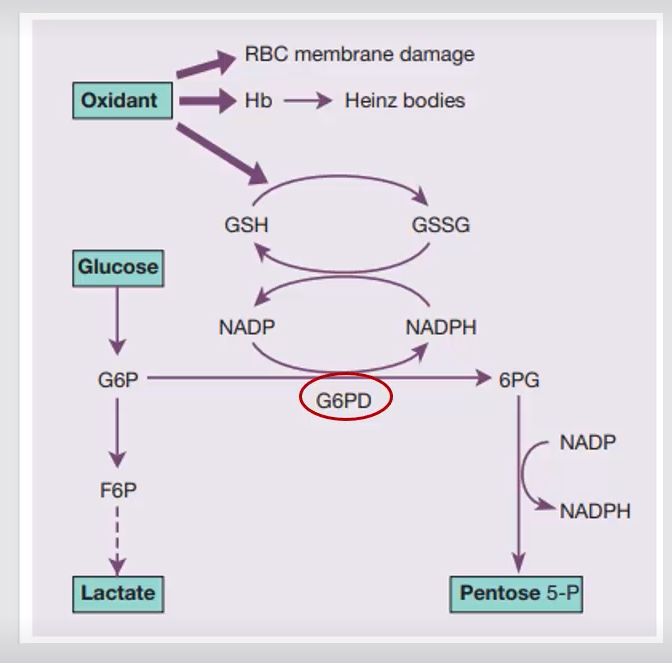
GSH-glutathione
GSSG-Glutathione disulfide
G6DP-Glucose-6-phosphate dehydrogenase
6PG-6-phosphogluconate
-
What happens during a G6PD deficiency?
-NADPH and GSH generation impaired-Acute haemolysis on exposure to oxidant stress: oxidative drugs, fava (broad) beans or infections-Hb precipitation – Heinz bodies
-G6PD deficiency most common known enzymopathy, estimated toaffect 400 million people worldwide
-
What are haemolytic anaemias?
-Anaemias resulting from an increase in the rate of red cell destruction
Haemolytic anaemias can be....
Hereditary/Congenital Vs AcquiredIntrinsic Vs Extrinsic
Intravascular vs Extravascular
-
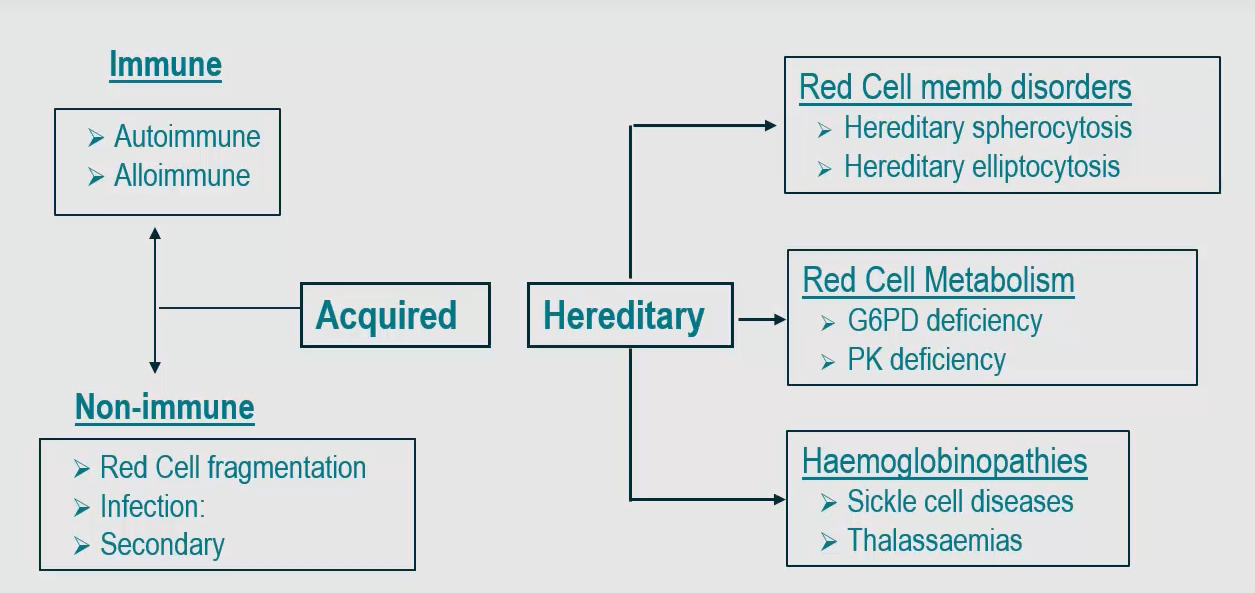
Name what Acquired and Hereditary haemolytic disorders consist of and these examples
-
Name 2 Red cell membrane disorders
1)Hereditary Spherocytosis
2)Hereditary Elliptocytosis
-
What is Hereditary Spherocytosis?
-Causes a loss of membrane integrity, the RBCs become spherical-Common hereditary haemolytic anaemia in N. Europ.+Deficiency in proteins with vertical interactions between themembrane skeleton and the lipid bilayer: e.g. ankyrin def
-
What is Hereditary Elliptocytosis?
-Causes oval shape of RBC
-Caused by mutations in horizontal interactions e.g. spectrin, ankyrin;actin, protein 4.1 deficiency
-
What are Haemoglobinopathies?
Mutations or deletions in globin genes
a) Sickle Cell Diseases: - Abnormal synthesis of globin chain.b) Thalassaemia.: - Reduced rate of synthesis of normal globin
-
What are the two metabolic red cell disorders?
a) G6-PD Deficiencyb) Pyruvate Kinase Deficiency
-
General summary:
-Erythropoiesis occurs in bone marrow-Tissue oxygenation, essential regulator of RBC production.-Dietary factors; iron, B12 and Folate required for effective erythropoiesis-Deficiencies lead to decreased RBC production or low Hb level, or both (anaemia)-3 things intrinsic to RBC are crucial for their survival and function.-Features of haemolysis includes:-Reticulocytosis, unconjugated hyperbilirubinemia

