Pulmonary Ventilation (Physiology)
Session summary This session introduces the physiological processes that underlie the mechanics of breathing – i.e. how the respiratory system functions to move air between the atmosphere and alveoli in order to ventilate gas exchange surfaces. Topics discussed include the calculation of alveolar ventilation, the basic mechanism by which the respiratory system moves air, the role of pleura, as well as a specific clinical condition in which these processes are adversely affected (pneumothorax). Learning Outcomes Use relevant data to calculate alveolar ventilation. Describe how the respiratory system functions to move air between the atmosphere and alveoli. Describe the function of the pleural cavity in respiration and explain what occurs in the event of pneumothorax.
-
What is the primary function of the respiratory system? (2)
꩜ To supply respiring tissues with oxygen
꩜ To remove excess carbon dioxide
-
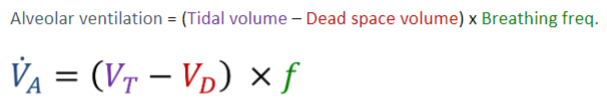
How does the respiratory system ensure gas exchange within the lungs? (2)
꩜ By maintaining partial pressure gradients between alveolar air and blood
꩜ By ventilating gas exchange surfaces, which involves moving air from the atmosphere to the alveoli and then out again
-
Why is maintaining partial pressure gradients important for gas exchange? (1)
꩜ Gas exchange relies on partial pressure gradients, ensuring that oxygen is supplied to alveoli and carbon dioxide does not accumulate.
-
Picture demonstrating gas exchange in the lungs (partial pressure)
-
How does changing metabolic demands affect gas exchange in the body? (2)
꩜ Changing metabolic demands require varying levels of gas exchange to supply oxygen and remove carbon dioxide.
꩜ This is achieved by changing the rate of alveolar ventilation to modulate partial pressure gradients between the alveoli and blood.
-
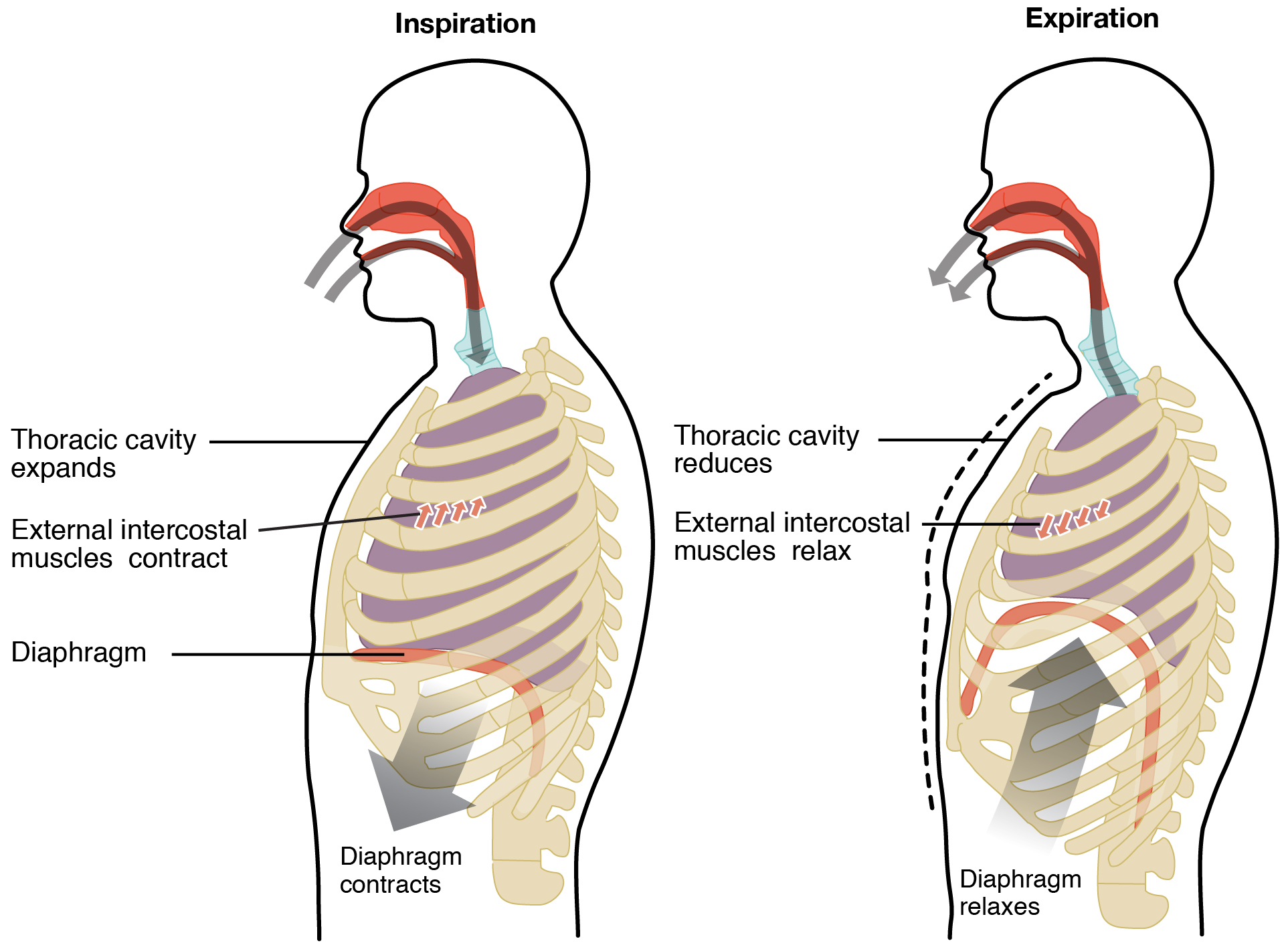
What are hypoventilation and hyperventilation, and how are they identified? (2)
꩜ Hypoventilation and hyperventilation are defined as insufficient or excessive levels of breathing relative to metabolic demands.
꩜ They can be identified by the level of CO2 present within the blood.
-
What are the consequences of hypoventilation and hyperventilation on arterial blood CO2 levels? (2)
Hypoventilation results in excessive levels of CO2 within arterial blood (PaCO2 > 6.0 kPa).
Hyperventilation results in reduced levels of CO2 within arterial blood (PaCO2 < 4.9 kPa).
-
How does increasing or decreasing the rate of ventilation affect alveolar oxygen and carbon dioxide partial pressures? (2)
꩜ Increasing the rate of ventilation increases alveolar oxygen partial pressure (PAO2) and decreases alveolar carbon dioxide partial pressure (PACO2).
꩜ Decreasing the rate of ventilation has the opposite effects.
-
Why is the focus on CO2 rather than O2 in determining ventilation? (2)
꩜ Due to CO2's role in acid-base balance
꩜ Because of the complexities of oxygen exchange and transport
-
Picture of hyperventilation and hypoventilation for kPa of Oxygen and Carbon dioxide
-
Why is quantifying pulmonary ventilation important? (2)
꩜ The total volume of air moved into and out of the lungs during inspiration and expiration is crucial for the quantity of oxygen reaching alveolar surfaces and participating in gas exchange.
꩜ Total lung volumes vary between individuals based on factors such as height, sex, age, and the presence of specific respiratory diseases.
-
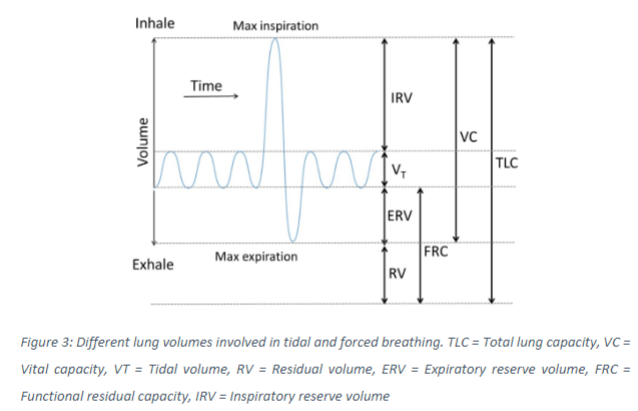
What are the different lung volumes used to describe respiratory function? (7)
꩜ Tidal Volume (VT): Volume of air moved in and out of the lungs during quiet breathing.
꩜ Inspiratory Reserve Volume (IRV): Additional volume of air that can be inhaled after a normal inspiration.
꩜ Expiratory Reserve Volume (ERV): Additional volume of air that can be exhaled after a normal expiration.
꩜ Residual Volume (RV): Volume of air remaining in the lungs after maximal expiration.
꩜ Total Lung Capacity (TLC): Total volume of air the lungs can hold after maximal inspiration.
꩜ Vital Capacity (VC): Maximum volume of air that can be exhaled after a maximal inspiration.
꩜ Functional Residual Capacity (FRC): Volume of air remaining in the lungs after a normal expiration.
-
Picture demonstrating different lung volumes involved in tidal and forced breathing:
-
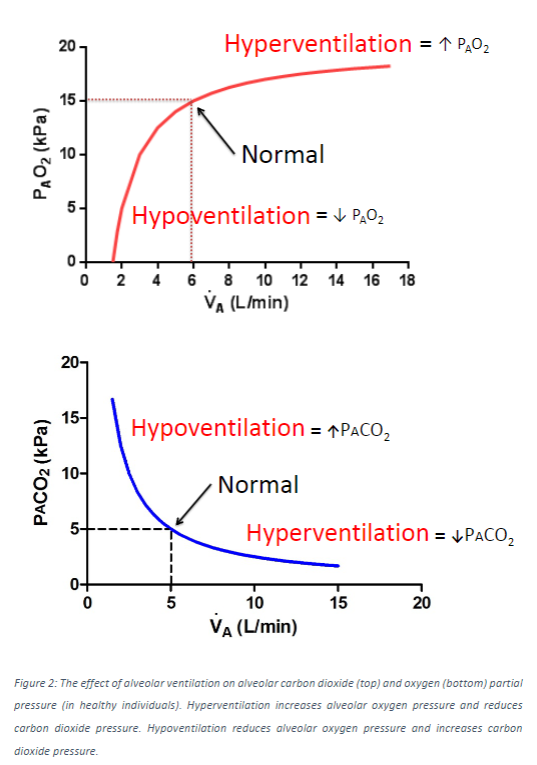
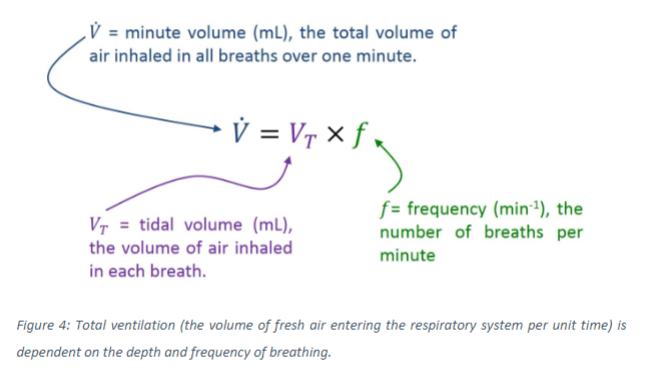
What does ventilation refer to? (1)
Ventilation refers to the volume of fresh air that reaches respiratory surfaces over a given time.
-
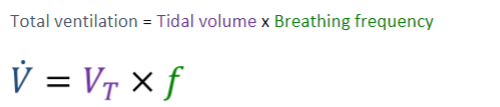
How is the total level of ventilation determined? (2)
꩜ It depends on both the volume of air inspired during each breath.
꩜ It also depends on the frequency of breathing, also known as respiratory rate, which indicates how many breaths occur per minute.
-
Picture demonstrating the total ventilation, which depends on the depth and frequency of breathing:
-
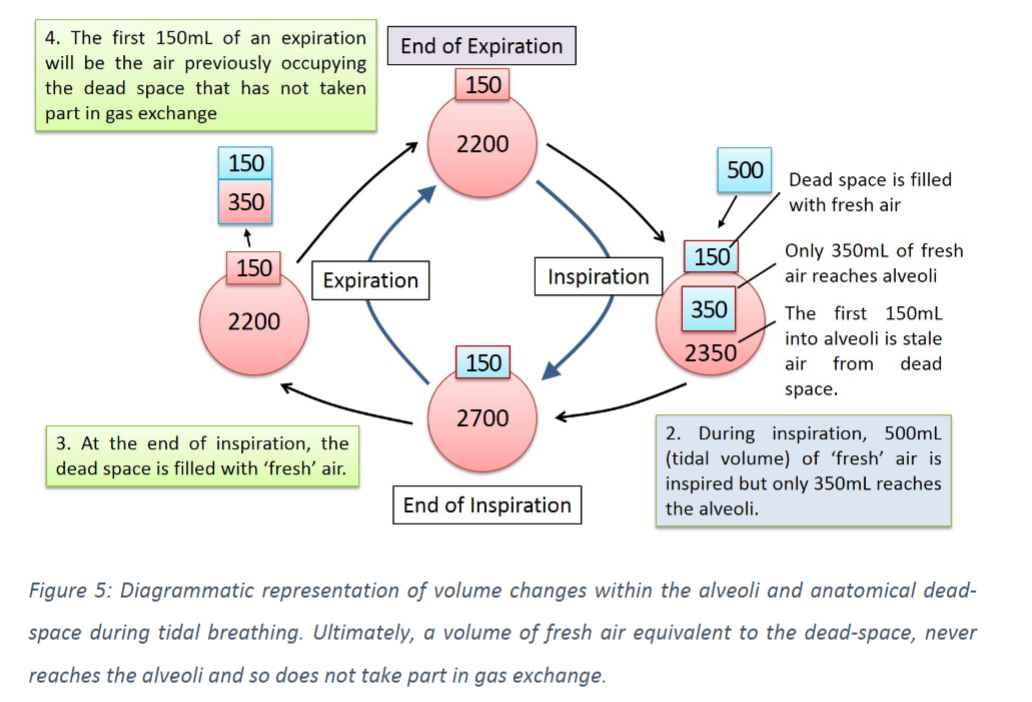
How does total ventilation differ from the volume of air reaching respiratory surfaces? (2)
꩜ Total ventilation represents the total volume of air inspired over a given time, but it doesn't perfectly reflect the volume of air reaching respiratory surfaces and participating in gas exchange.
꩜ Gas exchange only occurs in alveoli, not in the airways, so not all inspired air contributes to gas exchange.
-
Why does the respiratory system not completely empty even after maximal forced expiration? (2)
꩜ Air is required to occupy the airways, which do not contribute to gas exchange, known as the "dead space."
꩜ Alveoli do not completely collapse at the end of expiration, leaving a residual volume of air in the lungs.
-
What mixture of air do alveoli contain at any given point? (2)
Alveoli contain a mixture of "stale" air, which has already participated in gas exchange, and "fresh" air, which has not yet participated in gas exchange.
-
How does the two-way system of the respiratory system affect gas exchange? (2)
꩜ The fact that air enters and exits via the same path means that approximately 150mL of air from each inspiration, equivalent to the volume of the dead space, never reaches the alveoli or participates in gas exchange.
꩜ This air is the first to leave the respiratory system at the beginning of the next expiration.
-
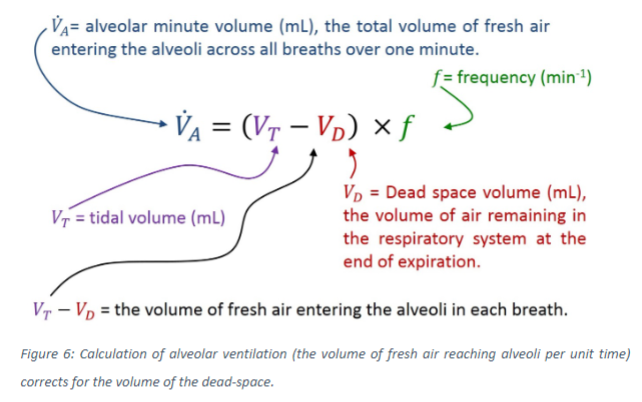
Why is it necessary to make an adjustment when calculating the volume of air reaching respiratory surfaces? (2)
꩜ To accurately calculate the volume of air reaching respiratory surfaces (alveolar ventilation), an adjustment needs to be made to account for the volume of air that does not reach the alveoli, known as the dead-space volume.
-
What is the approximate volume of the dead space in adults? (1)
The dead-space volume is typically around 150mL in adults.
-
Picture demonstrating a diagrammatic representation of volume changes within the alveoli and anatomical dead-space during tidal breathing
-
Picture demonstrating a calculation of alveolar ventilation:
-
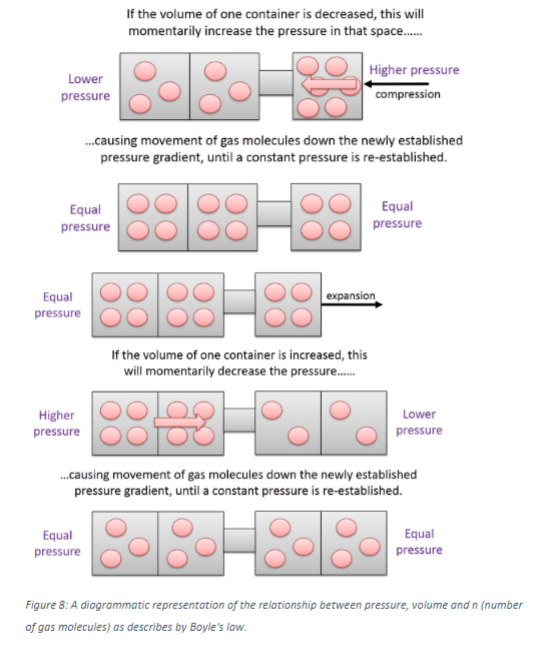
What is Boyle's Law, and how does it relate to the behaviour of gases? (3)
꩜ Boyle's Law states that at a constant temperature, the pressure of a gas is inversely proportional to its volume.
꩜ In other words, as the volume of a gas decreases, its pressure increases, and vice versa.
꩜ This law helps us understand how changes in volume affect pressure within a closed system, such as the respiratory system.
-
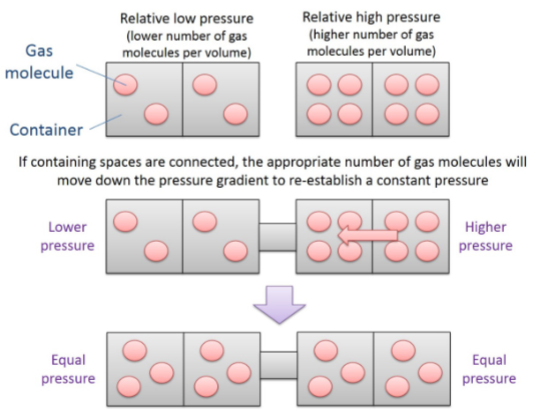
How does pressure relate to the behaviour of gases? (2)
꩜ Pressure is the force exerted by gas molecules on the surfaces of the space in which they are contained.
꩜ Gases naturally move from areas of high pressure to areas of low pressure until an equilibrium is reached.
-
How can gases be moved between connected spaces? (1)
꩜ Gases can be moved between connected spaces by creating a pressure gradient, where there is a difference in pressure between the two spaces.
-
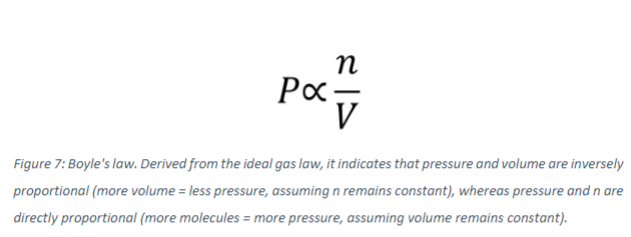
What is the formula for Boyle's law?
-
What does Boyle's Law describe? (1)
꩜ Boyle's Law describes the relationship between pressure (P), volume (V), and molar quantity (n) of gas molecules present.
-
How is Boyle's Law derived? (1)
꩜ Boyle's Law is derived from the ideal gas law, which describes the behavior of gases under various conditions.
-
What are the variables involved in Boyle's Law? (3)
꩜ Pressure (P)
꩜ Volume (V)
꩜ Molar quantity (n), representing the number of gas molecules present.
-
What is the relationship described by Boyle's Law? (1)
꩜ Boyle's Law states that at a constant temperature, the pressure of a gas is inversely proportional to its volume.
-
Picture demonstrating gas at low and high pressures:
-
Picture demonstrating how a decrease in volume will increase pressure:
-
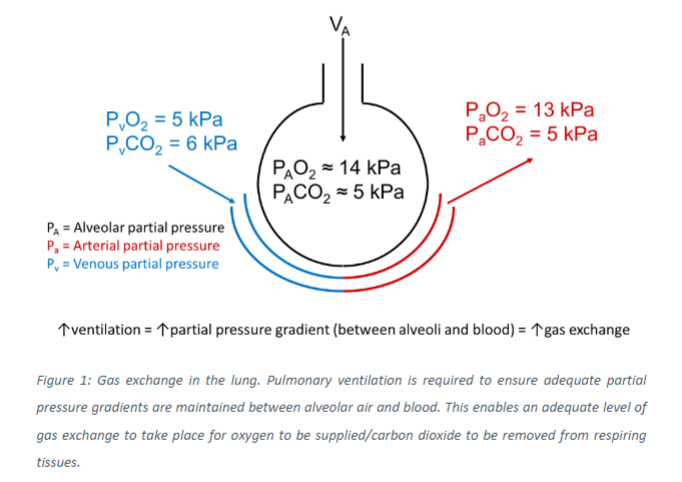
What is the role of changing alveolar pressure in the movement of air between the atmosphere and lungs? (2)
꩜ Humans cannot naturally modulate the pressure of the atmosphere, so the movement of air between the atmosphere and lungs relies solely on changing alveolar pressure.
꩜ To move air into the lungs during inspiration, alveolar pressure must fall below atmospheric pressure (creating a pressure gradient), and during expiration, alveolar pressure must rise above atmospheric pressure.
-
How are these pressure changes achieved? (2)
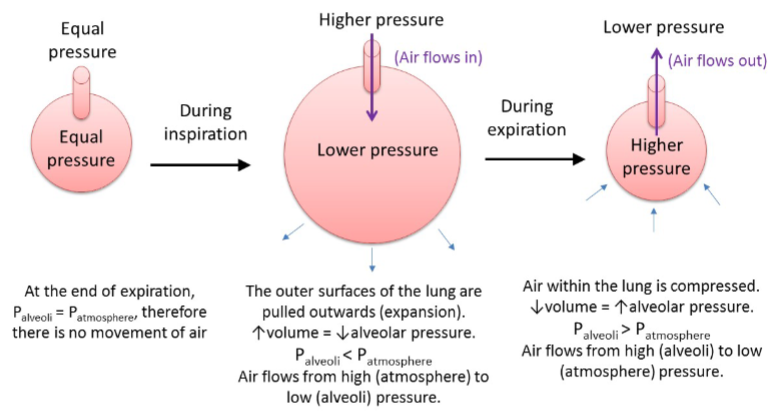
꩜ These pressure changes are achieved by contraction and relaxation of respiratory muscles, altering the volume of the thoracic cavity, which in turn affects alveolar pressure.
-
What happens during inspiration and expiration in terms of lung volume, alveolar pressure, and airflow? (3)
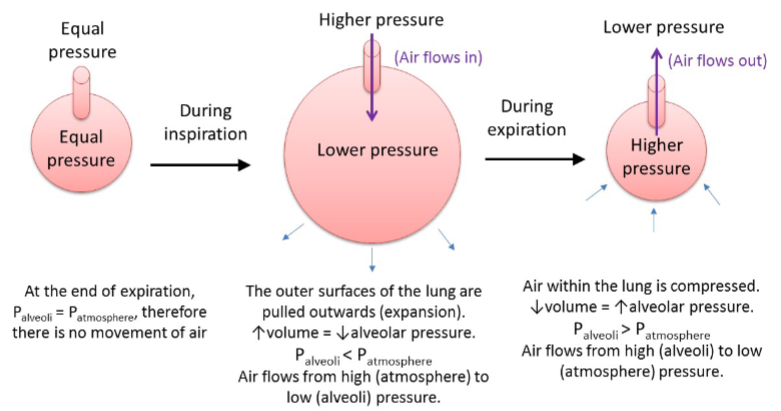
꩜ During inspiration, increases in lung volume decrease alveolar pressure, generating a pressure gradient between the alveoli and the atmosphere.
꩜ Air moves from the area of high pressure (atmosphere) to low pressure (alveoli).
꩜ The process reverses during expiration.
-
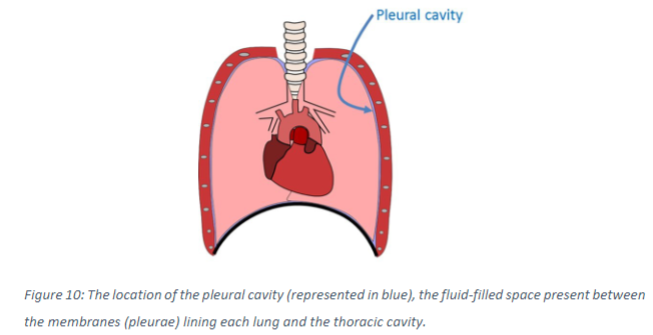
What separates the lungs from the chest wall? (1)
The lungs and chest wall are separated by a pair of serous membranes known as pleurae (singular = pleura).
-
Picture demonstrating the pleural cavity location:
-
What are the characteristics of the visceral and parietal pleurae? (3)
꩜ The visceral pleura lines each lung, while the parietal pleura lines the thoracic cavity, surrounding the chest, diaphragm, and mediastinum.
꩜ Between the two pleurae is the sealed, fluid-filled pleural cavity.
-
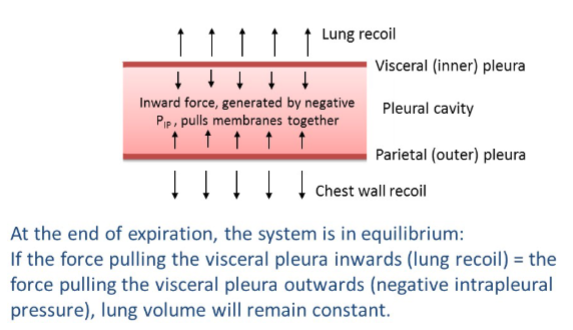
How do the elastic properties of the tissues attached to each pleura affect the pleural cavity? (2)
꩜ The tissues attached to each pleura recoil in opposite directions due to their elastic properties.
꩜ This stretches the sealed pleural cavity between them, decreasing the pressure within the pleural space.
-
What is the significance of negative intrapleural pressure? (3)
꩜ Negative intrapleural pressure is naturally sub-atmospheric due to the opposing recoil of the chest wall and lungs.
꩜ Within an enclosed space, negative pressure generates a collapsing force, pulling the surfaces of the contained space together.
꩜ Negative intrapleural pressure acts to pull the two pleurae (and consequently the lungs and chest wall) together.
-
What role does the level of negative intrapleural pressure play in breathing? (2)
꩜ The level of negative intrapleural pressure determines the force acting to pull the pleura together, which affects lung and chest wall expansion and compression.
꩜ Negative intrapleural pressure plays a key role in breathing by influencing the balance of forces acting on the lungs and chest wall.
-
How can the expansion and compression of the lungs and chest wall be conceptualized? (1)
꩜ Expansion and compression of the lungs and chest wall can be conceptualized as a tug-of-war between various forces acting upon them.
-
What forces are involved in the tug-of-war during breathing? (3)
꩜ Elastic (outward) recoil of the chest wall and inspiratory respiratory muscle contraction (e.g., contraction of the diaphragm) pull the chest wall outwards and expand the thoracic cavity.
꩜ Elastic recoil of the lungs pulls the visceral pleura inwards and compresses lung volume.
꩜ Negative intrapleural pressure acts to pull the lungs and chest wall together.
-
What determines whether the lungs expand or compress at a given time? (1)
꩜ The balance between these three forces determines whether the lungs expand or compress at a given time.
-
Picture demonstrating what happens in the pleura at the end of expiration:
-
What happens at the beginning of inspiration in terms of respiratory muscle contraction and intrapleural pressure? (2)
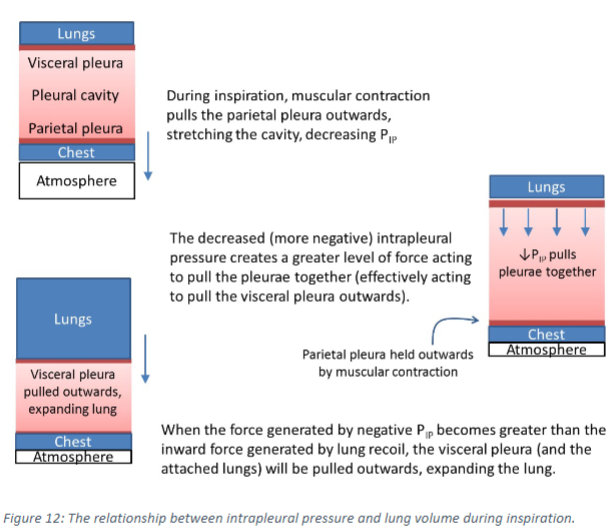
꩜ Contraction of respiratory muscles, such as the diaphragm, generates sufficient force to pull the parietal pleura outwards.
꩜ This action stretches the pleural cavity, decreasing intrapleural pressure.
-
How does the change in intrapleural pressure affect the force pulling the pleurae together? (1)
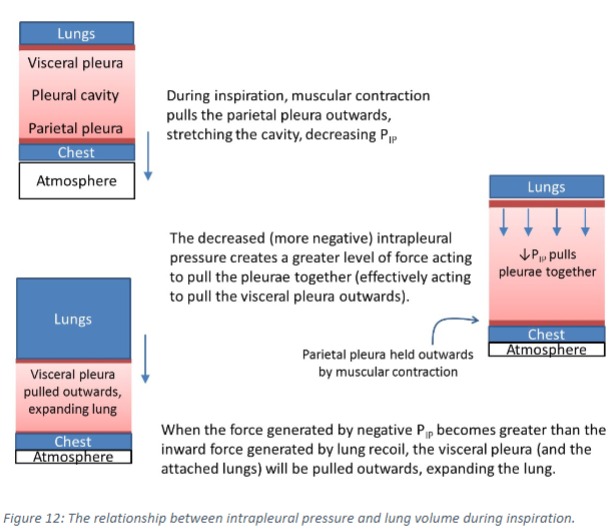
꩜ As intrapleural pressure becomes more negative, the force pulling the two pleurae together increases.
-
What happens when the force pulling the pleurae together exceeds the force generated by lung recoil? (1)
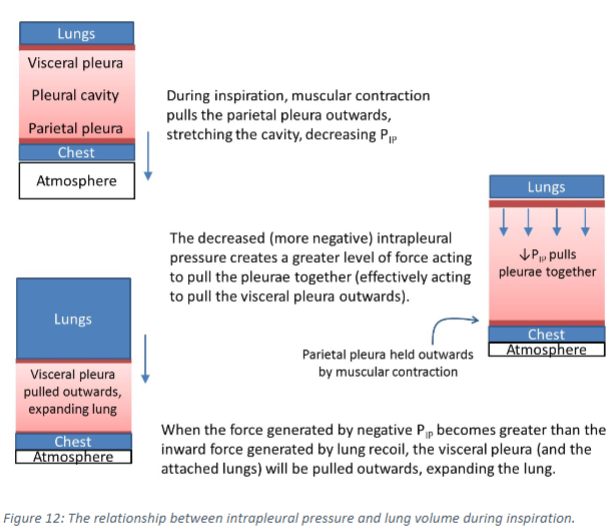
꩜ When the force pulling the pleurae together becomes greater than the force generated by the elastic recoil (due to elastic tissue) of the lung, the visceral pleura is pulled outward, expanding the lung.
-
What happens during passive expiration in terms of respiratory muscle relaxation and intrapleural pressure? (2)
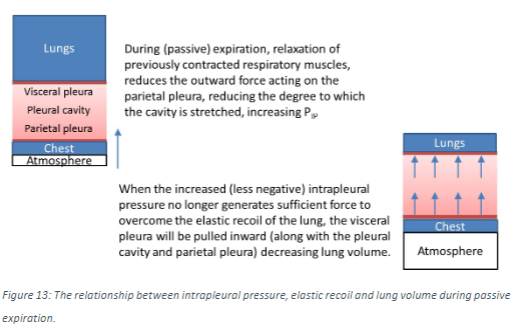
꩜ Relaxation of inspiratory respiratory muscles results in decreased outward force acting on the parietal pleura.
꩜ This reduces the force acting to stretch the pleural cavity, increasing intrapleural pressure.
-
How does the change in intrapleural pressure affect the force pulling the pleurae together and lung volume? (2)
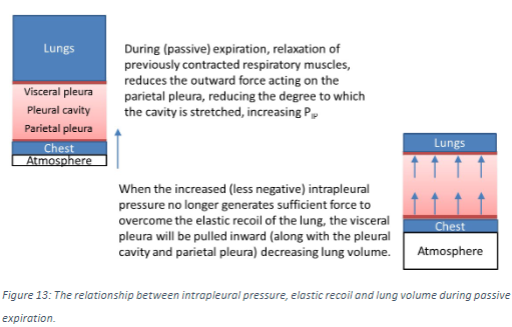
꩜ The increased (less negative) intrapleural pressure no longer generates sufficient force to overcome the elastic recoil of the lung.
꩜ As a result, the visceral pleura is pulled inward along with the pleural cavity and parietal pleura, decreasing lung volume.
-
What happens during a forced expiration in terms of muscle contraction and pleural cavity compression? (3)
꩜ During a forced expiration, respiratory muscles such as the abdominals actively contract to compress the volume of the thoracic cavity.
꩜ Muscle contraction generates inward force on the parietal pleura, compressing the pleural cavity further and increasing intrapleural pressure (PIP).
꩜ This results in a more pronounced decline in lung volume, in terms of both speed and magnitude.
-
What is the overall function of the respiratory system in terms of the mechanics of breathing? (1)
꩜ The overall function of the respiratory system brings together the relationships described by Boyle’s law and the role of intrapleural pressure in breathing.
-
Picture demonstrating the mechanisms of inspiration and expiration:
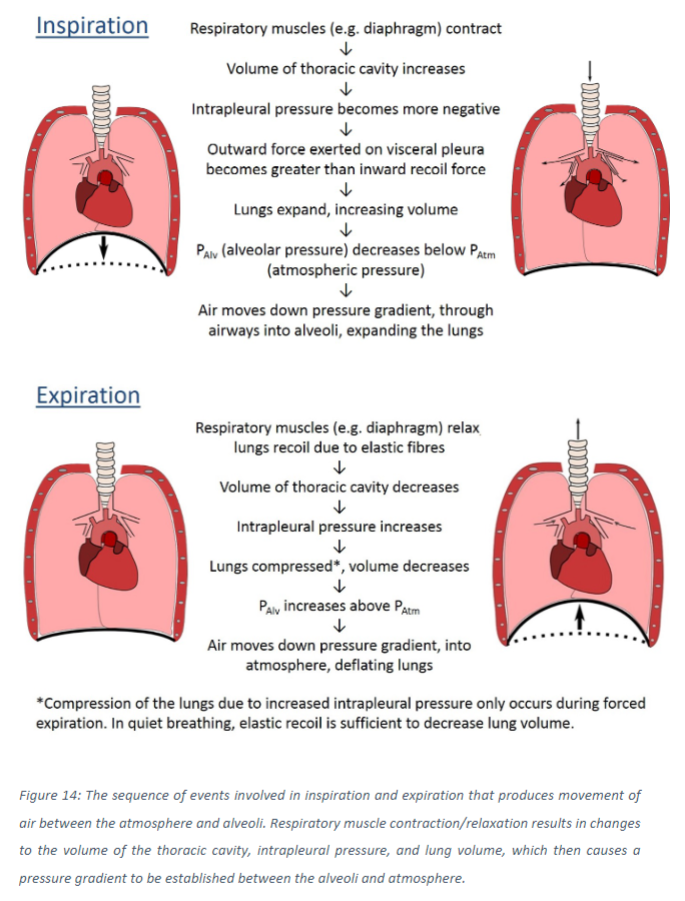
-
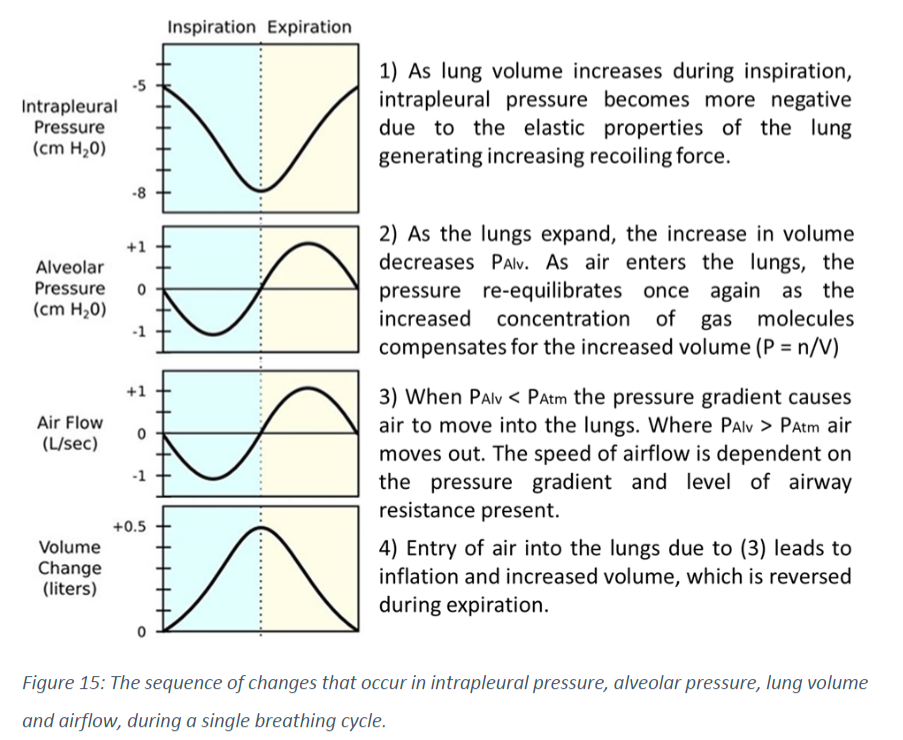
Lung volume, intrapleural pressure, alveolar pressure and airflow are thus all related to each other during breathing, as shown by the following diagram:
-
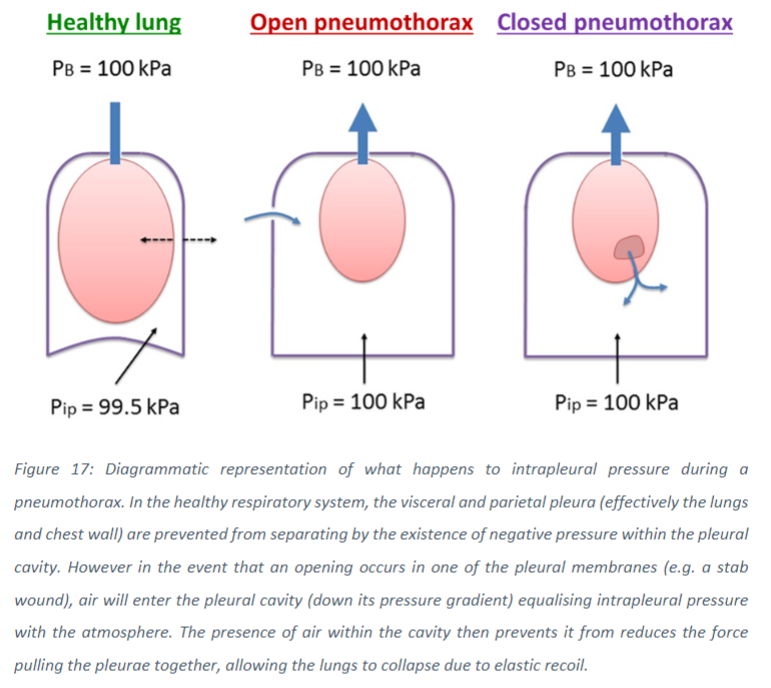
What is pneumothorax? (1)
꩜ Pneumothorax is a condition where air enters the pleural space due to a rupture in one of the pleural membranes.
-
What causes pneumothorax? (1)
꩜ Pneumothorax can be caused by trauma, bleb formation, or disease, which can rupture one of the pleural membranes.
-
How does pneumothorax affect intrapleural pressure? (1)
꩜ In pneumothorax, the entry of air into the pleural space disrupts the naturally sub-atmospheric intrapleural pressure.
-
What happens to the volume of the pleural cavity when air enters it? (1)
꩜ Entry of air into the pleural cavity results in its volume increasing, at the expense of the lung.
-
How does the recoil of the lungs and expansion of the chest wall during breathing affect air entry into the pleural cavity? (2)
꩜ Recoil of the lungs and expansion of the chest wall during breathing can potentially draw additional air into the cavity.
꩜ Simultaneously, the expansion of the chest wall during inhalation enlarges the thoracic cavity, further lowering the intrapleural pressure and potentially drawing air into the pleural cavity, especially in cases like pneumothorax.
-
Picture demonstrating the effects of pleural membrane rupture on intrapleural pressure and lung volume:
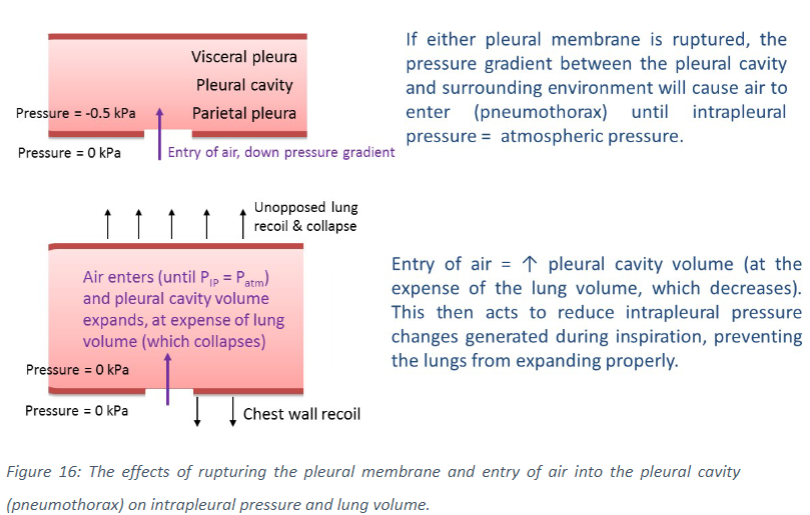
-
What happens to the elastic recoil of the chest wall and lungs in pneumothorax? (1)
꩜ With the loss of negative intrapleural pressure, elastic recoil of the chest wall and lungs is no longer resisted.
-
What effect does this have on the affected regions of the lungs? (1)
꩜ This causes affected regions of the lungs to collapse.
-
What factors influence the overall effect of lung collapse in pneumothorax? (1)
꩜ The overall effect depends on the site and extent of the injury.
-
Diagrammatic representation of what happens to intrapleural pressure during apneumothorax. In the healthy respiratory system:
-
What is total ventilation?
꩜ Total ventilation is the volume of air entering or leaving the respiratory system in a given time period.
-
What is alveolar ventilation?
꩜ Alveolar ventilation is the volume of inspired air that reaches alveoli and participates in gas exchange in a given time period.
-
What is tidal volume?
꩜ Tidal volume is the volume of air inspired or expired per breath.
-
What is breathing frequency?
꩜ Breathing frequency is the number of breaths that take place over a given time period, usually measured per minute.
-
What is dead space volume?
꩜ Deadspace volume is the volume of the anatomic dead space within the respiratory system, which essentially refers to the volume contained within the airways that doesn’t participate in gas exchange.
-
What is the formula for total ventilation?
-
What is the formula Alveolar ventilation?