Properties of special circulations (Physiology)
Session summary There are lots of special circulations in the body eg. cerebral, pulmonary, skeletal muscle, renal, gastro-intestinal etc. We will focus on the coronary circulation and the skin especially with regard to the particular requirements of these circulations and their special features. Finally, specific clinical problems associating with coronary and cutaneous circulations will be explored. For example, why does occlusion of the coronary circulation can produce angina? Why does a very rapid heartbeat actually reduce coronary blood flow, and why does skin paradoxically undergo vasodilation in prolonged cold conditions etc? Learning outcomes At the end of this session you will be able to: Appreciate special requirements that must be met by coronary circulation and cutaneous circulation. Understand special structural or functional features of the cardiac and cutaneous circulation. Describe specific problems relating to the special circulations considered
-
What is coronary heart bypass?
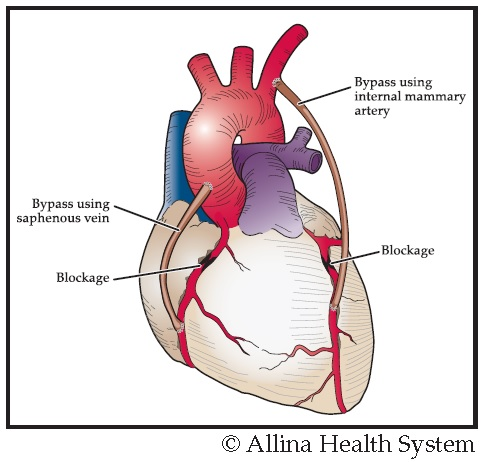
A surgical procedure used to treat coronary heart disease. It diverts blood around narrowed or clogged parts of the major arteries to improve blood flow and oxygen supply to the heart
-
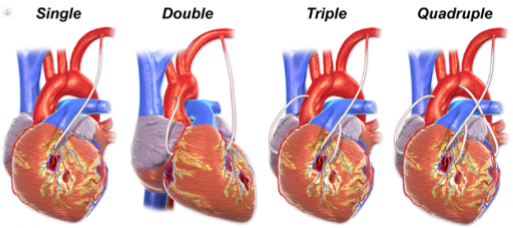
How many stages are there relating to coronary heart bypass?
-
How many coronary arteries originate from the left side of the heart, and from where do they arise?
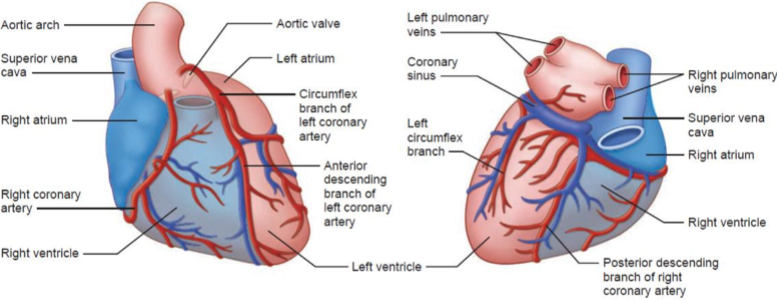
Two coronary arteries originate from the left side of the heart.
They are the Left Main Coronary Artery (LMCA) and the Left Anterior Descending Artery (LAD).
The LMCA arises from the left coronary sinus of the aorta.
The LAD branches off from the LMCA and runs along the interventricular groove toward the apex of the heart.
-
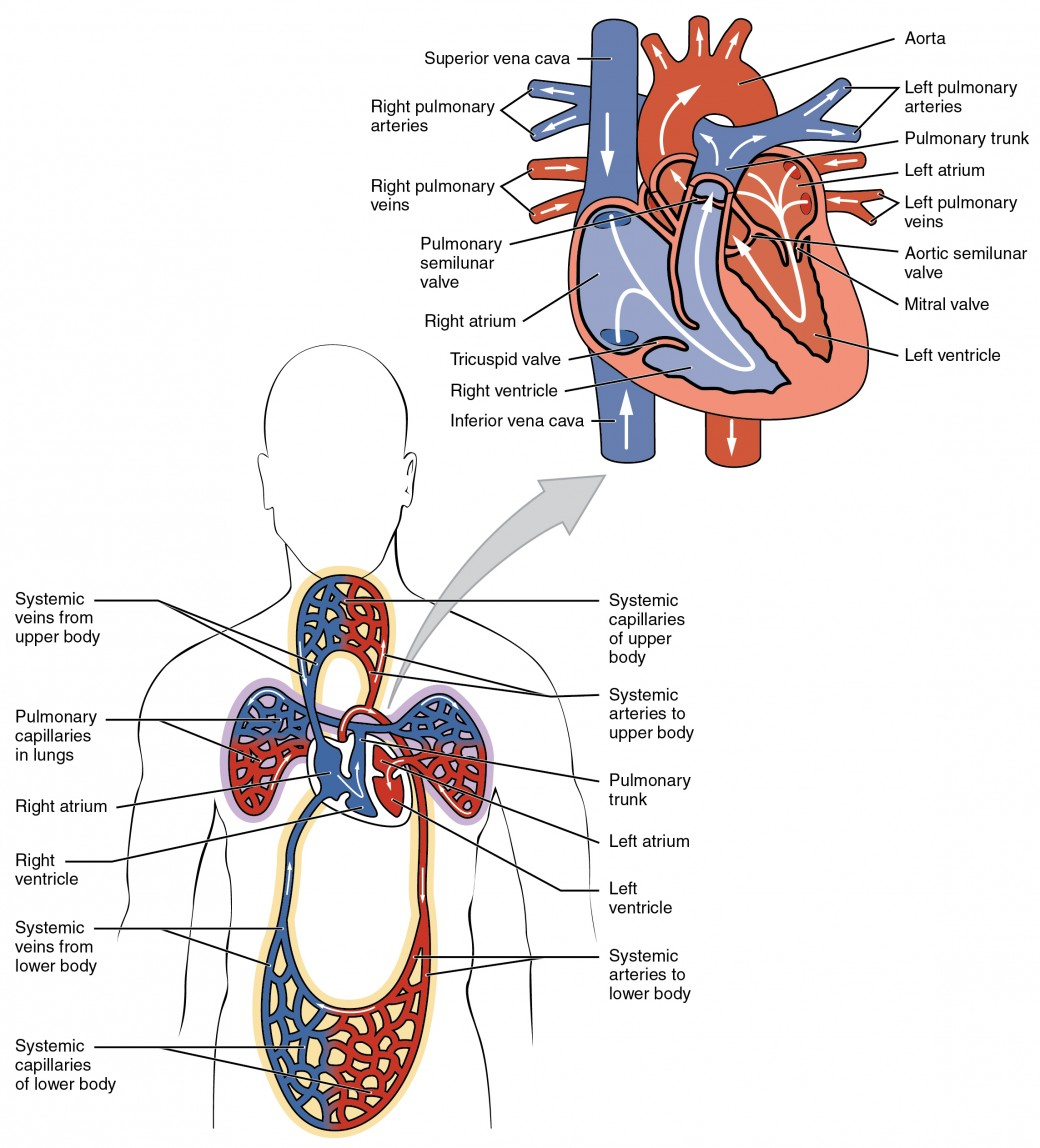
What is the function of cardiac veins mentioned in the text?
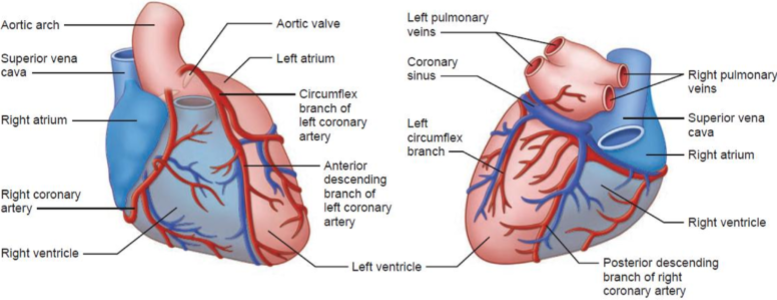
Carry blood with a poor level of oxygen from the myocardium to the right atrium
-
Where does most of the blood from the coronary veins return?
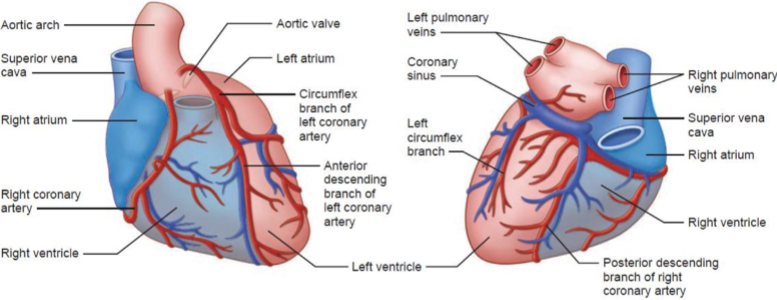
Most of the blood of the coronary veins returns through the coronary sinus
-
What are the special requirements of coronary circulation?
-Requires a high basal supply of oxygen, approximately 20 times more than resting skeletal muscle
-It also needs to increase oxygen supply in proportion to increased demand or cardiac work
-
What are some special structural features of coronary circulation mentioned in the text?
High capillary density and a large surface area for oxygen transfer
-
How do the special structural features of coronary circulation contribute to efficient oxygen transport?
-The high capillary density and large surface area for oxygen transfer in coronary circulation reduce the diffusion distance to myocytes
-This reduction in diffusion distance is crucial because diffusion time is proportional to distance squared, allowing for fast oxygen transport to the heart muscles
-
What is the fibre diameter (μm) and capillary area (mm^2) in skeletal muscle?
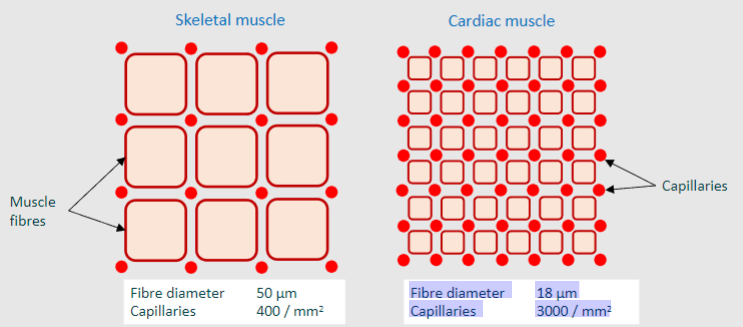
-Fibre diameter 50 μm-Capillaries 400 / mm2
-
What is the fibre diameter (μm) and capillary area (mm^2) in Cardiac muscle?
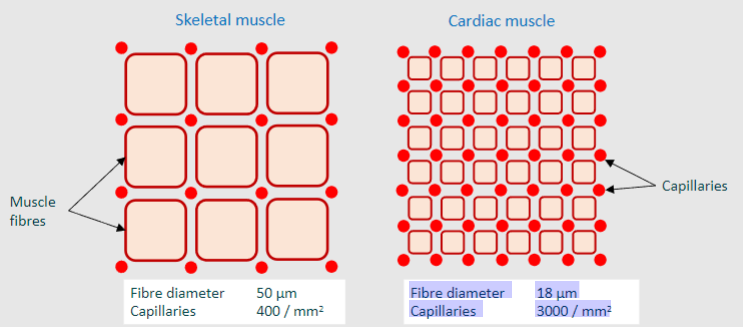
-Fibre diameter 18 μm-Capillaries 3000 / mm^2
-
What are some special functional features of coronary circulation during normal activity?
-During normal activity, coronary circulation experiences high blood flow, approximately 10 times the flow per weight of the rest of the body
-It also has relatively sparse sympathetic innervation, high nitric oxide release leading to vasodilatation, and high oxygen extraction (75%), compared to the average of 25% in the body
-
How does coronary blood flow respond to increased demand?
During increased demand, coronary blood flow increases in proportion to demands
-
How do vasodilators influence coronary circulation during increased demand?
During increased demand, the production of vasodilators such as adenosine, potassium ions (K+), and acidosis out-compete relatively low sympathetic vasoconstriction
-
How does adrenaline affect coronary vessels during increased demand?
Circulating adrenaline dilates coronary vessels during increased demand due to the abundance of β2-adrenoceptors
-
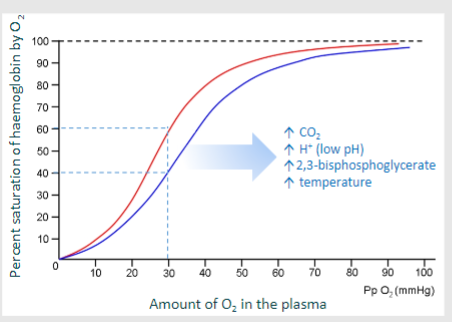
Picture demonstrating haemoglobin oxygen binding:
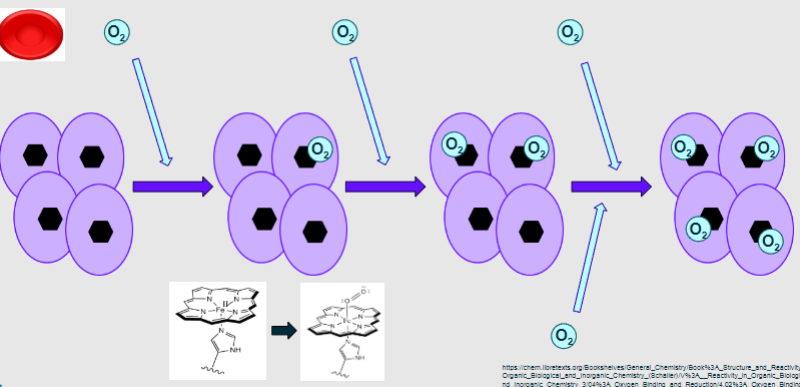
-
What does the Oxygen Haemoglobin Dissociation Curve measure?
Is a measure of the uptake and removal of oxygen by hemoglobin under different partial pressures
-
In simple terms, what does the Oxygen Haemoglobin Dissociation Curve indicate?
Shows how much oxygen pressure leads to what percentage of oxygen saturation of blood hemoglobin
-
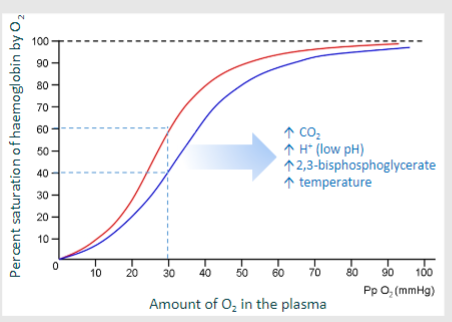
A left shift of the oxygen haemoglobin curve leads to increased or decreased affinity?
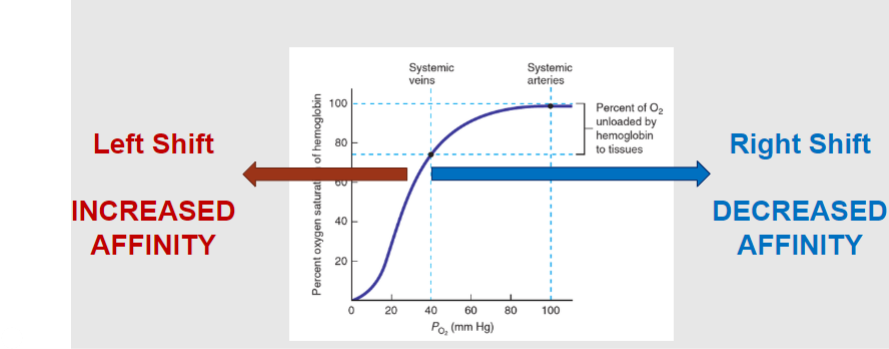
Increased affinity
-
A right shift of the oxygen haemoglobin curve leads to increased or decreased affinity?
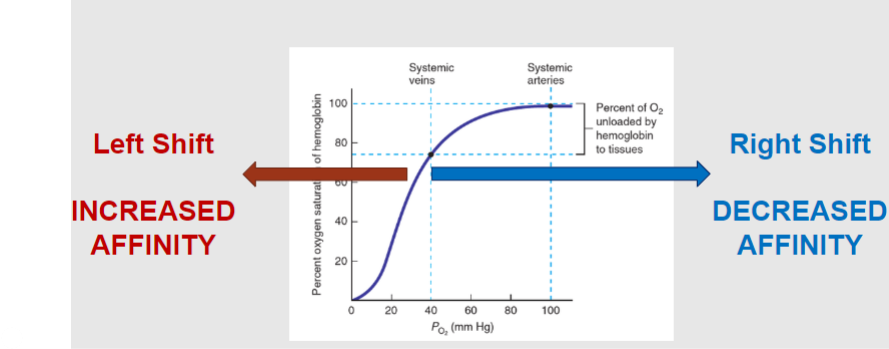
Decreased affinity
-
What is the process of oxygen unloading to the myocardium during normal activity referred to as?
The Bohr shift
-
How does the Bohr shift influence oxygen unloading to the myocardium?
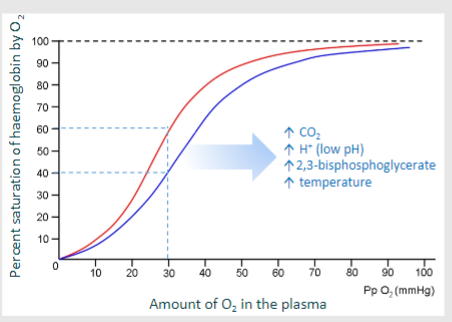
-The Bohr shift occurs when coronary sinus blood returning to the right atrium from myocardial tissue has a greater carbon dioxide content due to high capillary density, surface area, and small diffusion difference
-This high CO2 and low pH shift the oxygen dissociation curve to the right, meaning that hemoglobin has less affinity for oxygen, leading to more oxygen being released to the myocardial tissues
-
What percentage of oxygen is typically extracted by the myocardium, and how does this compare to other tissues?
The myocardium is able to extract 75% of the oxygen, whereas typically, other tissues extract around 25% of the oxygen
-
What occurs in response to an increased oxygen requirement according to the text?
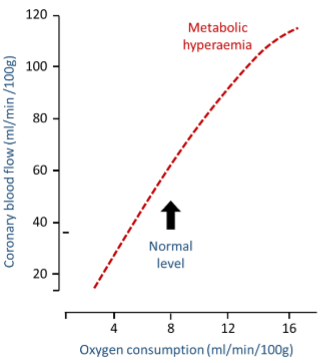
An increased oxygen requirement produces increased blood flow
-
Why is increasing blood flow necessary to meet increased oxygen demand?
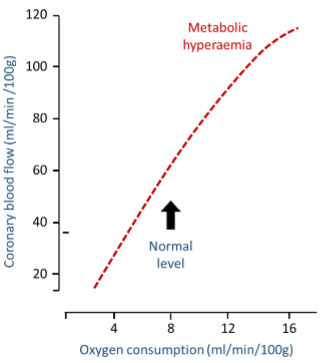
Extraction of oxygen is near maximal during normal activity, so to provide more oxygen during demand, increasing blood flow is necessary
-
How does myocardium metabolism contribute to increasing blood flow during increased oxygen demand?
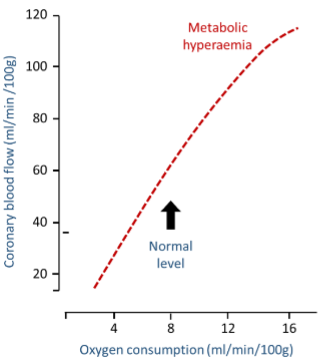
-Myocardium metabolism generates metabolites that produce vasodilatation, leading to increased blood flow, a phenomenon known as metabolic hyperaemia
-Examples of such metabolites include adenosine, produced by ATP metabolism and released from cardiac myocytes, as well as increases in pCO2, H+, and K+ levels
-
What are functional end-arteries, and why are they significant in the context of Ischaemic Heart Disease?
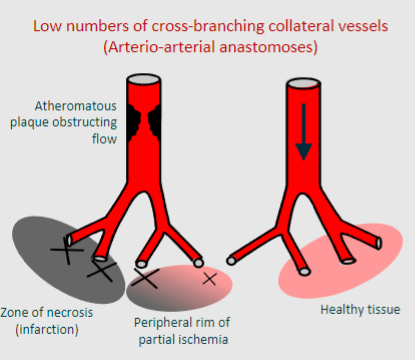
-Functional end-arteries are arteries where decreased perfusion in one of them can cause major problems because they do not have adequate collateral circulation
-This is significant in Ischaemic Heart Disease because decreased perfusion in one of these arteries can lead to severe consequences
-
What are the two main types of obstructions that can affect the heart, and what conditions do they lead to?
-The heart is susceptible to both sudden and slow obstructions
-Sudden obstructions, such as acute thrombosis, can produce myocardial infarction
-Slow obstructions, such as atheroma (sub-endothelial lipid plaques) causing chronic narrowing of the lumen, produce angina
-
What physiological process obstructs coronary blood flow during systole?
Systole obstructs coronary blood flow
-
What is thrombosis?
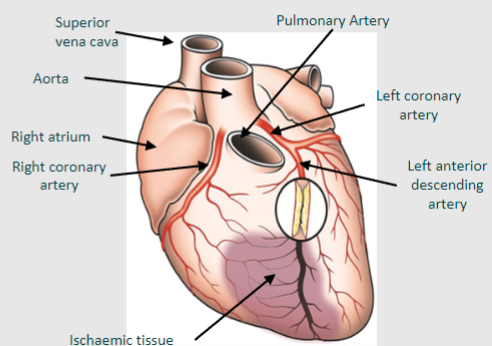
Thrombosis refers to the total occlusion of the left anterior descending coronary artery
-
What are the consequences of occlusion in the left anterior descending coronary artery?
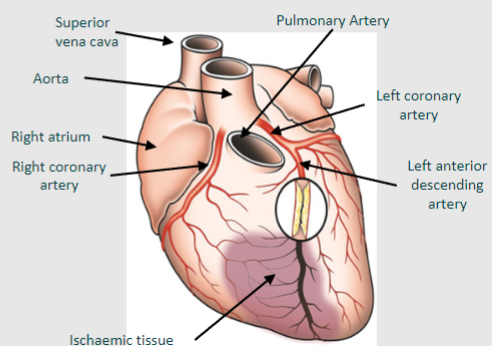
Occlusion in this artery leads to obstruction of blood flow to the anterior (front) left ventricle, resulting in myocardial infarction
-
What are the effects of myocardial infarction? (7)
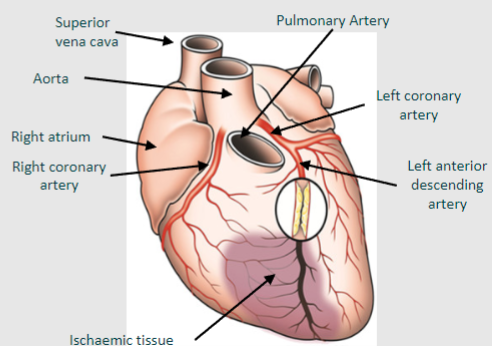
Myocardial infarction leads to various consequences such as ischemic tissue, acidosis, pain (stimulation of C-fibres), impaired contractility, sympathetic activation, arrhythmias, and cell death (necrosis)
-
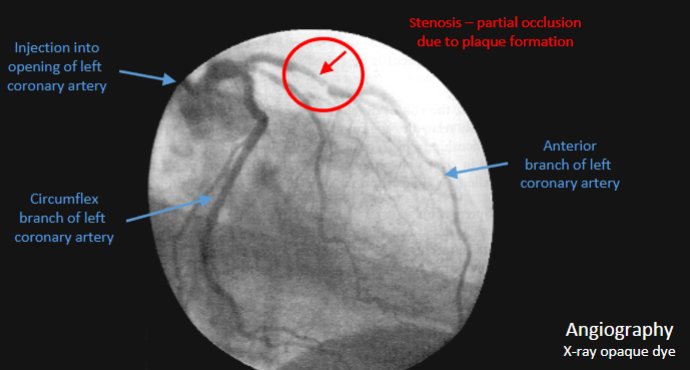
What is Angiograthy?
Type of X-ray used to check blood vessels
-
Picture demonstrating the partial occlusion of left coronary arteries- angina upon exercise:
-
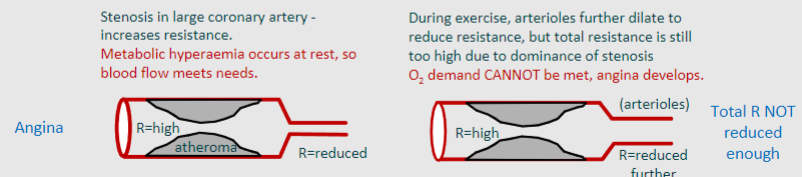
What is Angina?
Chest pain caused by reduced blood flow to the heart muscle
-
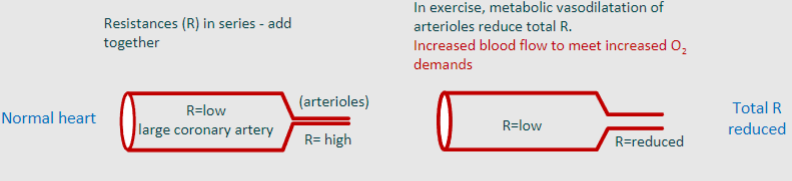
Picture demonstrating resistance in a normal heart, during relaxation and exercise:
-
Picture demonstrating resistance in a heart suffering angina, during relaxation and exercise:
-
What are the mechanical factors that can reduce coronary blood flow during diastole?
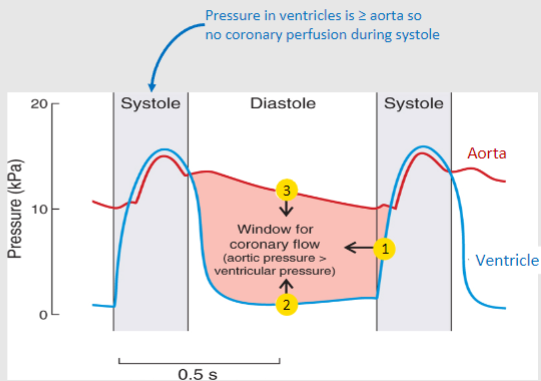
Mechanical factors that reduce coronary flow during diastole include shortening diastole (e.g., high heart rate), increased ventricular end-diastolic pressure (e.g., heart failure, aortic stenosis, stiffening of the ventricle), and reduced diastolic arterial pressure (e.g., hypotension, aortic regurgitation).
-
How does high heart rate affect coronary blood flow during diastole?
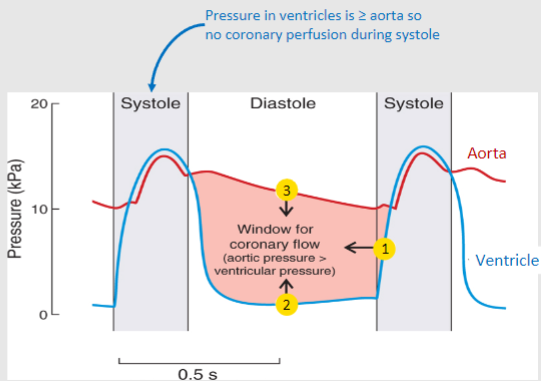
High heart rate shortens diastole, which can reduce coronary blood flow.
-
What effect does heart failure have on coronary blood flow during diastole?
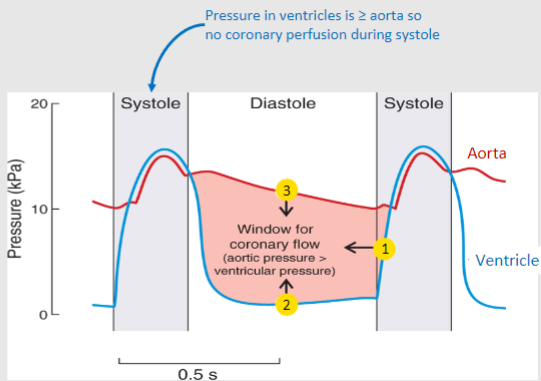
Heart failure increases ventricular end-diastolic pressure, thereby reducing coronary blood flow during diastole
-
What is the impact of hypotension on coronary blood flow during diastole?

Hypotension reduces diastolic arterial pressure, which can decrease coronary blood flow during diastole
-
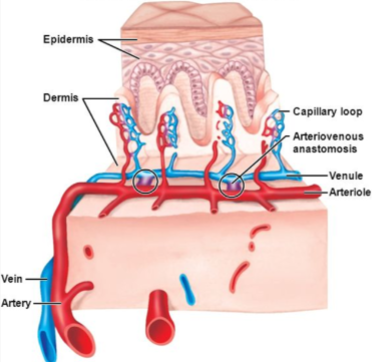
Picture demonstrating Cutaneous circulation
-
What are the special properties of the cutaneous circulation?
Include defence against the environment, the Lewis triple response to trauma leading to increased blood flow, and temperature regulation.
-
How does the cutaneous circulation defend against the environment?
Cutaneous circulation serves as a defence mechanism against the environment by responding to trauma with the Lewis triple response, which involves increased blood flow to the affected area
-
What role does the cutaneous circulation play in temperature regulation?
By delivering heat from the body core through conduction, radiation (infrared proportional to skin temperature), convection (heat carried away by the air), and sweating (latent heat of evaporation)
-
Is the skin considered poikilothermic or homeothermic? Why?
The skin is considered poikilothermic because it can tolerate a wide range of temperatures (from 0°C to 40°C briefly) without damage, unlike homeothermic organisms which maintain a constant temperature
-
What factors influence skin temperature?
Skin temperature depends on factors such as skin blood flow and ambient temperature
-
What does Poikilothermic mean?

Organisms whose body temperature varies with the temperature of their environment
-
What does Homeothermic mean?

Organisms that regulate their body temperature internally to maintain a relatively constant temperature regardless of external conditions.
-
What are the special structural features of the cutaneous circulation? (2)
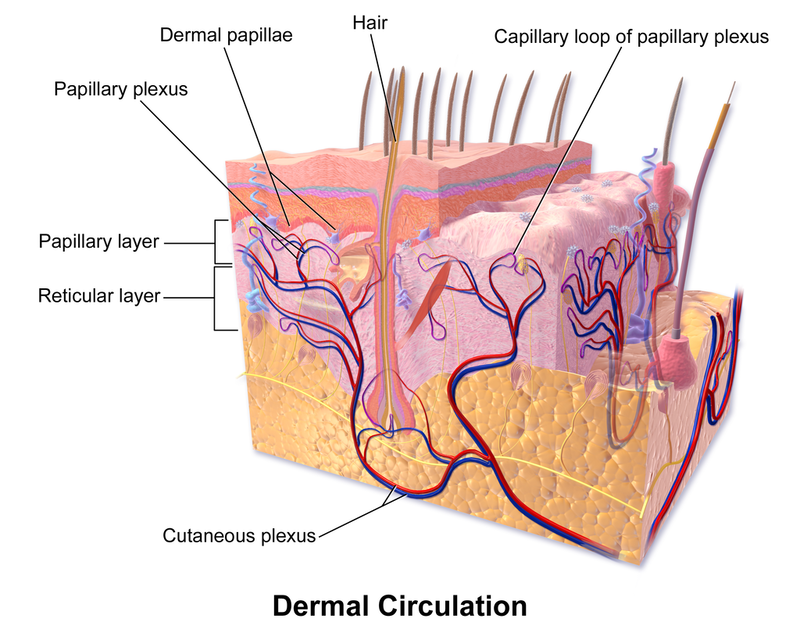
-The special structural features include sympathetic vasoconstrictor fibres: releasing noradrenaline acting on α1 receptors
-Sudomotor vasodilator fibres: releasing acetylcholine acting on endothelium to produce nitric oxide, and arterio-venous anastomoses (AVAs)
-
How do sympathetic vasoconstrictor fibres affect cutaneous circulation?
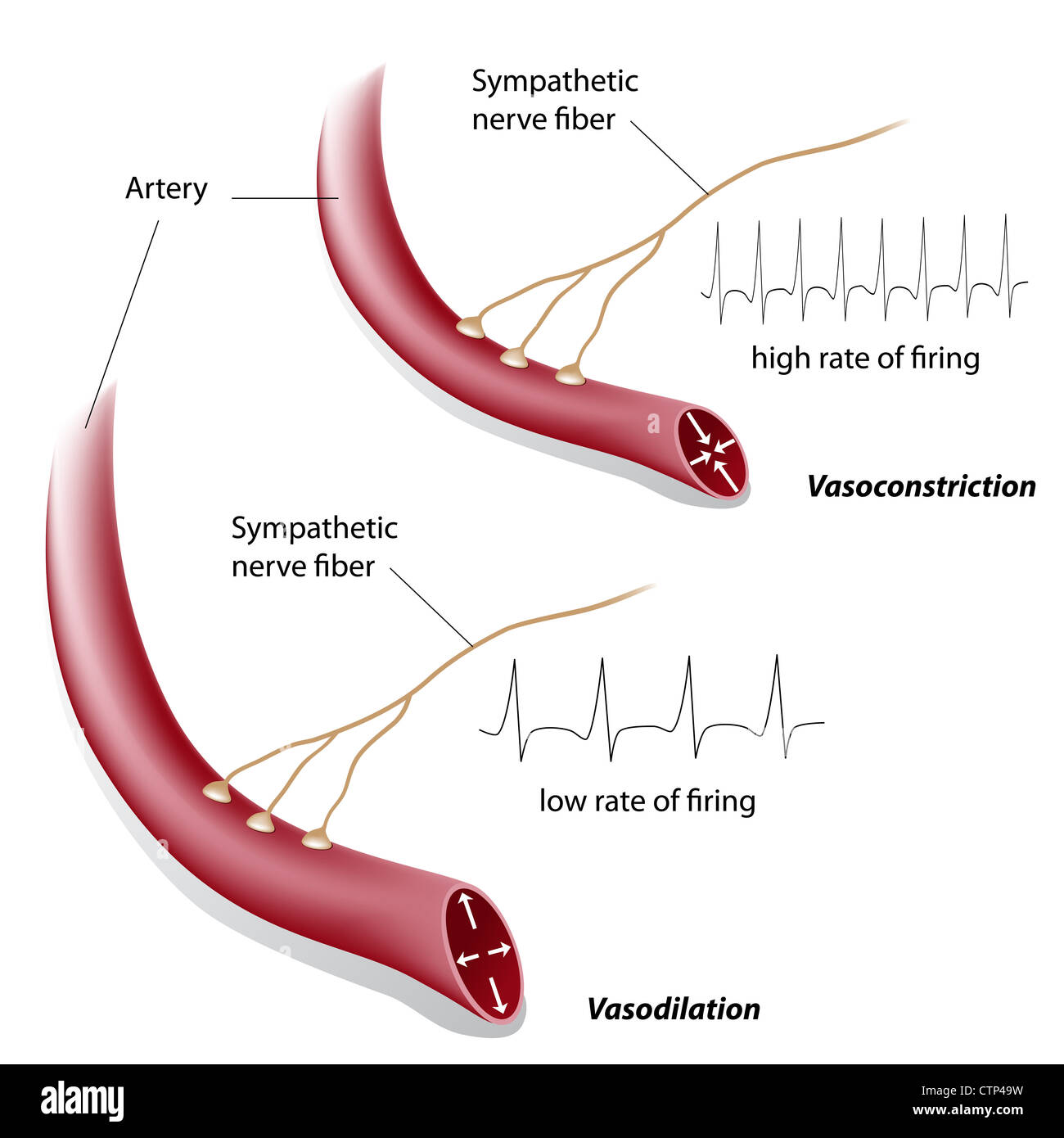
Sympathetic vasoconstrictor fibres release noradrenaline, which acts on α1 receptors to induce vasoconstriction in cutaneous blood vessels
-
What role do sudomotor vasodilator fibres play in cutaneous circulation?
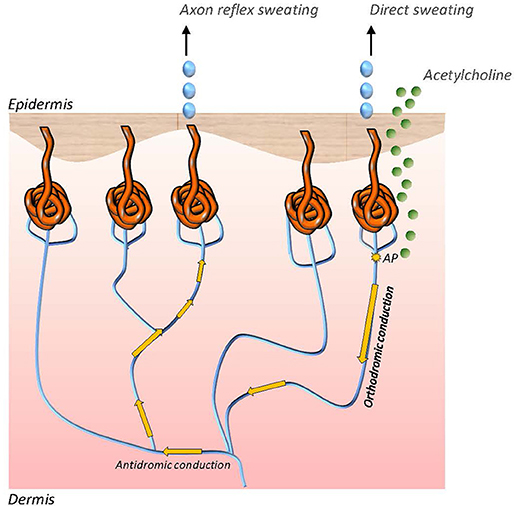
Sudomotor vasodilator fibres release acetylcholine, which acts on the endothelium to produce nitric oxide, leading to vasodilation in cutaneous blood vessels
-
What drives the activity of temperature regulation nerves in the hypothalamus?
Temperature regulation nerves in the hypothalamus drive the activity of sudomotor vasodilator fibers and sympathetic vasoconstrictor fibers, influencing cutaneous circulation
-
What are arterio-venous anastomoses (AVAs) and what function do they serve?
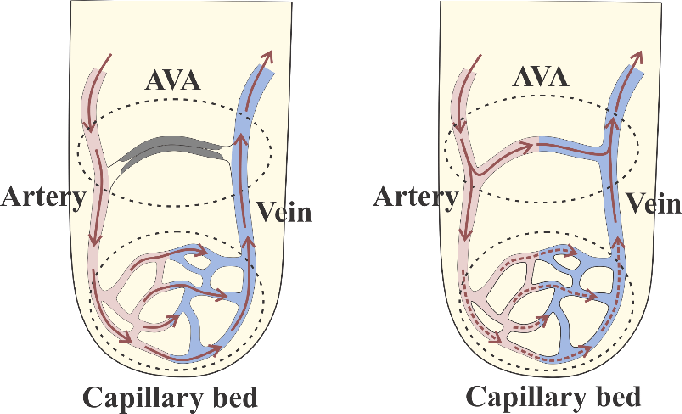
Arterio-venous anastomoses are direct connections between arterioles and venules that expose blood to regions of high surface area, facilitating heat exchange through convection, conduction, radiation, and evaporation in cutaneous circulation
-
What are the special functional features of cutaneous circulation?
The special functional features include responsiveness to ambient and core temperatures, aiding in both heat loss and heat conservation
-
How does cutaneous circulation help with heat loss?
Cutaneous circulation increases vasodilation and venodilation in response to an increase in ambient temperature, facilitating heat loss from the body
-
How does cutaneous circulation help conserve heat?
Cutaneous circulation increases vasoconstriction and venoconstriction in response to a decrease in ambient temperature, helping to conserve heat within the body.
-
What is "paradoxical cold vasodilatation"?
Severe cold can sometimes trigger paradoxical cold vasodilatation, where blood vessels in the skin dilate despite the cold temperature, possibly as a protective mechanism to prevent tissue damage.
-
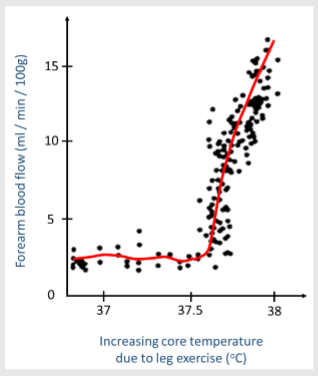
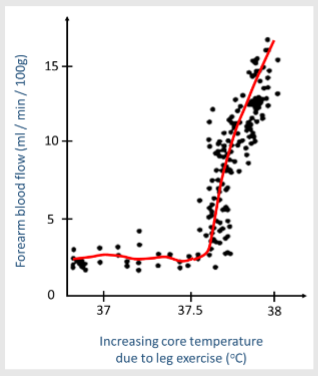
How is skin blood flow regulated based on core temperature?
Core temperature receptors in the hypothalamus control sympathetic activity to the skin, thereby regulating skin blood flow in response to changes in core temperature.
-
What is the purpose of cold-induced vasoconstriction? How does it occur?
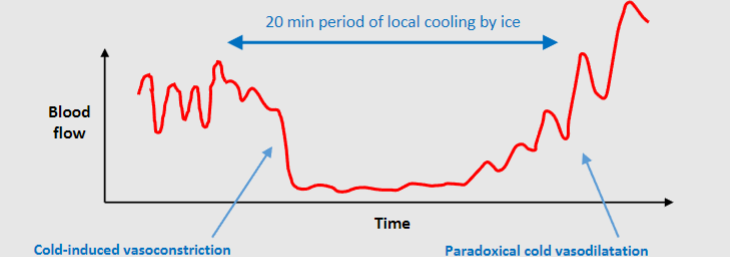
Conserves heat• Sympathetic nerves react to local cold by releasing noradrenaline, which binds to a2 receptors on vascular smooth muscle in skin.
• a2 receptors bind NA at lower temperatures than a1receptors
-
What is the purpose of paradoxical cold vasodilation? How does it occur?
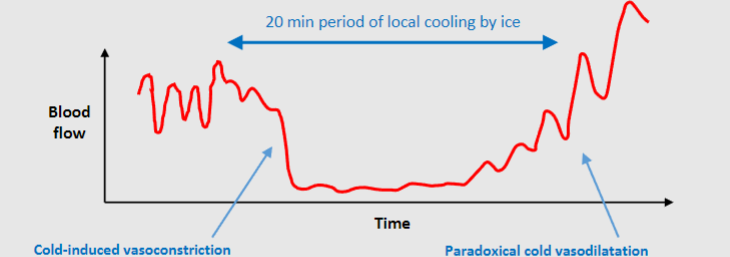
Protects against skin damage• Caused by paralysis of sympathetic transmission• Long-term exposure leads to oscillations ofcontract/relax
-
What happens to cutaneous perfusion when core temperature increases?
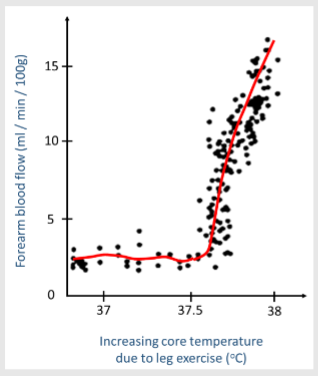
Increased core temperature stimulates temperature receptors in the anterior hypothalamus
This leads to:
Sweating and increased sympathetic activity to sweat glands, mediated by acetylcholine
Vasodilation due to increased sympathetic sudomotor activity
Acetylcholine acts on endothelium to produce nitric oxide (NO), dilating arterioles in the extremities.
Resulting in increased cutaneous perfusion
-
How does the body respond to increased core temperature?
Increased core temperature stimulates:
Sweating and enhances sympathetic activity to sweat glands, both mediated by acetylcholine
Vasodilation in the extremities due to increased sympathetic sudomotor activity
This leads to increased cutaneous perfusion
-
What role does the anterior hypothalamus play in regulating cutaneous perfusion?
The anterior hypothalamus contains temperature receptors.
Stimulation by increased core temperature initiates responses such as:
Sweating
Increased sympathetic activity to sweat glands
These contribute to enhanced cutaneous perfusion
-
How is vasodilation achieved in the extremities during increased core temperature?
Increased sympathetic sudomotor activity causes:
Acetylcholine to act on endothelium, producing nitric oxide (NO)
NO dilates arterioles in the extremities
This results in vasodilation and increased cutaneous perfusion
-
What are the other functional specializations of cutaneous circulation?
Baroreflex/RAAS/ADH-stimulated vasoconstriction of skin blood vessels occurs during conditions such as hemorrhage, sepsis, and acute cardiac failure.
This redirects blood to more important organs/tissues following loss of blood pressure.
Mediated by sympathetic vasoconstrictor fibers, adrenaline, vasopressin, and angiotensin II.
This response is responsible for the pale, cold skin observed in patients in shock
-
Why might warming up the body too quickly during hemorrhage be potentially dangerous?
During hemorrhage, warming up the body too quickly may reduce cutaneous vasoconstriction.
Cutaneous vasoconstriction is essential for redirecting blood flow to vital organs/tissues rather than the skin
-
How does cutaneous circulation contribute to emotional communication?
Cutaneous circulation plays a role in emotional communication, such as blushing
Blushing involves activation of sympathetic sudomotor nerves
-
What is the Lewis triple response and how does it relate to cutaneous circulation?
The Lewis triple response is a response to skin injury
It involves three stages: redness (due to arteriolar dilation), flare (surrounding vasodilation), and wheal (localized edema)
This response demonstrates the complex involvement of cutaneous circulation in the body's response to injury
-
What is the Lewis triple response of the skin to trauma?

The Lewis triple response is the skin's response to trauma.
It involves three stages:
Redness, caused by capillary vasodilation
Flare, a redness in the surrounding area due to arteriolar dilation mediated by axon reflex
Wheal, exudation of extracellular fluid from capillaries and venules
-
How does the Lewis triple response help in dealing with invading pathogens?
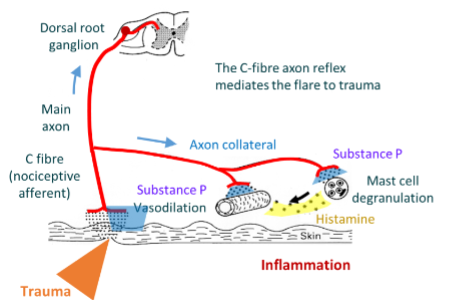
The Lewis triple response facilitates increased delivery of immune cells and antibodies to the site of damage caused by trauma
This helps the body deal with invading pathogens effectively
-
What are the special problems associated with cutaneous circulation?
Prolonged obstruction of flow by compression can lead to severe tissue necrosis, such as bed sores in areas like heels, buttocks, and weight-bearing areas
These problems can be avoided by shifting position or turning, causing reactive hyperemia upon the removal of compression
The skin has high tolerance to ischemia
-
How does gravity contribute to postural hypotension and edema?
Postural hypotension and edema can occur due to gravity, especially when standing for long periods in hot weather
This can lead to a decrease in central venous pressure (hypotension) and increased capillary permeability (edema)
-
What are some symptoms of postural hypotension?
Standing for long periods in hot weather can lead to symptoms such as feeling faint and tighter rings on the fingers

