-
What makes Listeria dangerous to women?
Dangerous to pregnant woman because it could cross the placenta
grows in Macrophage
-
Why is Listeria easy to contract?
•Listeria monocytogenes
–Non-endospore-forming bacillus
–Found in soil, water, and animals
–L. monocytogenes is an intracellular pathogen
–Enters body via contaminated food and drink
-
What are some major issues with women who contract listeria?
•Can cause meningitis in certain at-risk groups
•Pregnant women can transmit Listeria to their fetus
–Cause premature delivery, miscarriage, stillbirth, or meningitis in the newborn
-
Listeria grows in phagocytes often in the gallbladder and can manifest itself:
Based on where it enters. it can cause different diseases.
-
Listeria: Epidemiology
•Virulence directly related to Listeria's ability to live within cells
–actA, Listeriolysin O
-
Facts relating to Listeria in the GI tract.
Compete for nutrients with other organisms
Out compete, other neighbors,
M cell is found in Peyer's patch: lymphoid
M cell damage tissue by entering through Goblet cells
Enter through LLO PI-PLC
-
Listeria in the GI gut
Use ActA to move through host cells. Polymerizes Acta to jump from one cell to the next.
It goes into endosomes and uses phosphate
Ikka is the inhibitor of NFkB: relays phosphate signals and NfKb is free to release in cells to produce inflammatory factors. The stronger the inhibitor the signal weakens.
InlA-InlB, LLO PI-PLC, and ActA
-
How does Lysteria move within host?
ActA and VASP from bacteria as cells get long they are pushed along the bacteria.
-
This non-endospore-forming pathogen contains a waxy lipid called?
Mycolic acid: which is the virulence factor (where bacteria gets its name)
-
True or false M. Tuberculosis (TB) virulence factors are largely linked to its physiology.
True
-
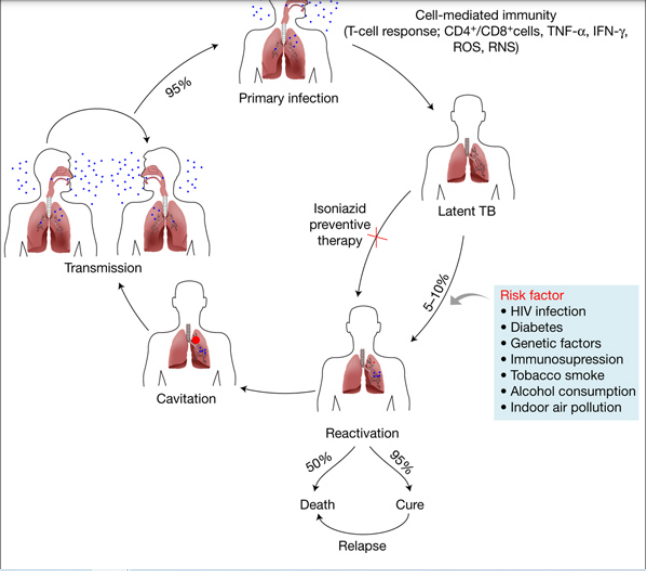
M. Tuberculosis has three types of tuberculosis:
Primary tuberculosis, Secondary or reactivated tuberculosis, and Disseminated tuberculosis
-
Process of Mycobacterium tuberculosis
-
The Mycobacterium Diagnosis Tuberculin skin test and Chest X-ray identifies for?
-Possible exposure
- individuals with active disease
-
Common and combination treatments for Mycobacterium include?
– Antimicrobials ineffective
– Months of therapy treat the disease
-
What can be done to prevent Leprosy?
–Limiting exposure to the pathogen
–BCG vaccine provides some protection
-
What are some treatments for Leprosy?
–Combination of antimicrobial drugs
–Lifelong treatment is sometimes needed
-
A person is diagnosed with Leprosy how?
–Based on signs and symptoms of disease.
-
The most severe sign of Leprosy is?
LEPTRATOMATOUS
-
The milder case of Leprosy is?
TUBERCULOID
-
It can take up to 10 years for symptoms of Leprosy to appear. What are the
Symptoms include?
●Skin growths
●Skin lesions
●Intense pain
-
●Muscle weakness ●specific to the hands and feet ●Numbness throughout the body ●Damage to nerves ●enlarged nerves ●Damage to eyes or blindness ●Ulcers that are specific to the souls of feet. These are all symptoms of:
Leprosy
-
The Pathogenesis of Mycobacterium Leprosy includes two different forms of the disease one being:
–Tuberculoid leprosy
»Nonprogressive form of the disease
»Due to a strong cell-mediated immune response
-
A more virulent form of the disease M. Leprosy is due to a weak cell-mediated immune response this is known as?
•Lepromatus leprosy
–Cases are becoming relatively rare
–Transmitted via person-to-person contact or break in the skin
-
How can a person contract M. Leprosy?
It's transmitted via person-to-person contact or break in the skin
-
M. Leprosy Prevention include:
–Immunization with BCG vaccine where TB is common
–Avoid inhaling respiratory droplets from TB patients
-
True or false "Hansen's disease"
–Caused by M. leprae
•Grows best in cooler regions of the human body
•Bacteria do not grow in cell-free culture
•Armadillos are the only known host other than humans
Ture
-
The Characteristics of Mycobacterium are
•Slow growth
•Protection from lysis after phagocytosis (protect itself against phagocytosis, because of mycolic acid)
-
Within the Mycobacterium capacity for intracellular growth in addition:
•Resistance to Gram staining, detergents, many antimicrobial drugs, and desiccation
-
What does Primary tuberculosis results from?
initial infection with M. tuberculosis
-
What leads to Secondary or reactivated tuberculosis?
–Reestablishment of active infection after a period of dormancy
-
Disseminated tuberculosis Results when infection spreads throughout the body and symptoms that arise due to, what?
–Symptoms arise due to complications at the various sites involved
-
The movement of ActA from cell to cell
1. Bacteria sites on AcatA
2. As Actin/Arp 2/3 polymerizes and interacts with VASP it pushes the cells forward.
3. The fibers solidus to filaments.
3. This function is allowing bacteria to travel from cell to cell.
4. The bacteria ends up in the endosome and starts the process and over.
-
What would happen if ActA could not move from cell to cell?
it could not cause disease. If Bacteria remain in the cell then Tcells containing CD4 and CD8 would target bacteria for apoptosis.

