
Pharmacological Basis for Treatment of GI Disorders (Physiology) UNFINISHED
Session summary The pair of lectures will provide you with information on how some common gastrointestinal disorders may be treated with drugs. For each drug or class of drug studied you should know what type of disorder it is used for, its pharmacological mechanism of action and what insights the action of the drug gives into the underlying disease process. You should be aware that drugs may be used alone or in combination with other types of therapy (e.g., dietary advice, surgery). Teams link: Join Pharmacological basis of treatment (Microsoft Teams Meeting)Links to an external site. Why it is important? Most treatments are based upon an understanding of the underlying physiology and pharmacology of the control mechanisms and where possible upon a knowledge of the pathophysiology of a disease. Learning outcomes This first part of the session will address: The pharmacological effects and identify the site of action of two drugs acting on histamine 2 (H2) receptors (e.g. cimetidine, ranitidine) The pharmacological basis of the action of anti-secretory drugs acting on the 'proton' pump (e.g. omeprazole) The major mechanism(s) by which metoclopramide stimulates gastric motility and the emptying of the stomach in patients in which it is delayed Two conditions in which metoclopramide may be used The second part will deal with: The mechanism of action of two spasmolytics which are used to treat spasms of the smooth muscle of the lower bowel (which are responsible for some types of 'colicky' pain) The mechanism of action of two pharmacological treatments for heartburn or gastroesophageal reflux disease The pharmacological treatment of H. pylori infections Constipation: The mechanism of action of two different types of laxative agent Diarrhoea: The mechanism of action of one anti-diarrhoeal agent Session resources Download the lecture slides: Pharmacological basis for treatment of GI disorders 2023-2024
-
What is the daily volume of gastric juice secreted for gastric acid secretion?
2.5 liters per day
-
What physiological process involves the expulsion of stomach contents through the mouth?
Vomiting
-
Name one function of the gastrointestinal tract (GIT) that is of pharmacological importance.
Gut motility
-
What process involves the production and release of bile?
Bile formation & excretion
-
What are examples of H2 receptor antagonists?
Cimetidine
Famotidine
-
What are the clinical uses of H2 receptor antagonists?
Treatment of peptic ulcer
Management of reflux esophagitis
-
How do H2 receptor antagonists reduce gastric acid secretion?
Inhibit histamine-, ACh- and gastrin-stimulated acid secretion on parietal cells
-
What is one consequence of reducing gastric acid secretion by H2 receptor antagonists?
Reduction in pepsin secretion
-
Can H2 receptor antagonists decrease basal and food-stimulated acid secretion, and by what percentage?
Yes, by up to 90%
-
What do H2 receptor antagonists promote in terms of ulcer healing?
Healing of duodenal ulcers
-
What happens if treatment with H2 receptor antagonists is discontinued?
Relapse of symptoms may occur
-
What effect do H2 receptor antagonists have on the healing of duodenal ulcers?
They promote the healing of duodenal ulcers.
-
What is a potential consequence of stopping treatment with H2 receptor antagonists?
Relapse of symptoms may occur.
-
What are some of the unwanted effects associated with H2 receptor antagonists?
Diarrhea
Muscle cramps
Transient rashes
Hypergastrinaemia
-
What specific adverse effect is associated with cimetidine in men?
Gynaecomastia (enlargement of breast tissue in men)
-
How does cimetidine affect the metabolism of certain drugs?
Cimetidine inhibits P450 enzymes, leading to decreased metabolism of drugs metabolized by these enzymes.
-
Name examples of drugs whose metabolism is decreased by cimetidine due to its inhibition of P450 enzymes.
Anticoagulants
Tricyclic antidepressants (e.g., imipramine, dosulepin, amitriptyline)
-
Picture to demonstrate Anti-secretory agents: effects of famotidine and cimetidine on inhibition of acid secretion
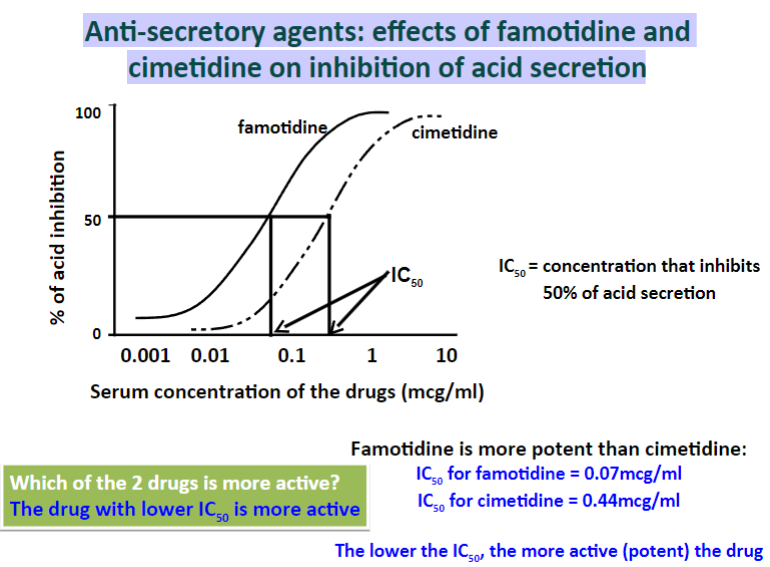
Lower IC50 values suggest increased potency
-
What are examples of proton pump inhibitors?
Omeprazole
Lansoprazole
Pantoprazole
Rabeprazole
-
What are the clinical uses of proton pump inhibitors?
Treatment of peptic ulcer
Management of reflux esophagitis
Component of therapy for H. pylori infection
Treatment of Zollinger-Ellison syndrome
-
In which condition are proton pump inhibitors considered the drugs of choice, especially if hyper-secretion of acid occurs?
Zollinger-Ellison syndrome
-
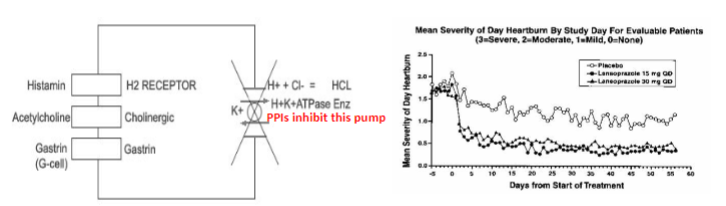
How do proton pump inhibitors work?
They irreversibly inhibit the proton pump (H+/K+ ATPase) in the gastric parietal cells, thus blocking the final step of acid secretion.
-
Besides peptic ulcer and reflux esophagitis, what other condition can proton pump inhibitors be used to treat?
Zollinger-Ellison syndrome
-
What is the mechanism of action of proton pump inhibitors in the treatment of gastric ulcers?
They reduce gastric acid secretion by irreversibly inhibiting the proton pump in the gastric parietal cells.
-
What is the mechanism of action of proton pump inhibitors?
They are weak bases that are inactive at neutral pH and irreversibly inhibit the H+/K+-ATPase pump.
-
How do proton pump inhibitors affect gastric acid secretion?
They decrease both basal and food-stimulated gastric acid secretion.
-
What type of enzyme do proton pump inhibitors irreversibly inhibit?
H+/K+-ATPase pump
-
What is the pH condition under which proton pump inhibitors are inactive?
They are inactive at neutral pH.
-
What is the significance of proton pump inhibitors being weak bases?
Being weak bases allows them to accumulate and become activated in the acidic environment of the stomach.
-
How do proton pump inhibitors contribute to the treatment of gastric ulcers?
By reducing gastric acid secretion through irreversible inhibition of the proton pump, thus aiding in the healing of gastric ulcers.
-
What are some of the unwanted effects associated with proton pump inhibitors?
Headache
Diarrhea
Mental confusion
Rashes
Somnolence (drowsiness)
Impotence
Gynaecomastia (enlargement of breast tissue in men)
Dizziness
-
Picture demonstrating Proton pump inhibitors in the treatment of gastric ulcers
-
What substances are considered gastroprotective for the gastric mucosa?
Prostaglandins (PGE2 and PGI2)
-
How do prostaglandins contribute to gastroprotection?
They increase mucosal blood flow and can augment the secretion of HCO3- and mucus.
-
What is the mode of action of misoprostol, a stable analogue of PGE1?
It inhibits basal- and food-stimulated gastric acid secretion.
It inhibits histamine-, and caffeine-induced gastric acid secretion.
It inhibits the activity of parietal cells.
It increases mucosal blood flow and can augment the secretion of HCO3- and mucus
-
What caution should be exercised when using misoprostol?
It can induce labor or abortion.
-
Besides inhibiting gastric acid secretion, what other effect does misoprostol have on the stomach?
It increases mucosal blood flow and can augment the secretion of bicarbonate (HCO3-) and mucus.
-
What is misoprostol's relationship to PGE1?
Misoprostol is a stable analogue of PGE1.
-
What are the effects of metoclopramide on gastric motility and emptying?
Metoclopramide has mixed effects. It inhibits pre- and post-synaptic dopamine (D2) receptors as well as 5-HT3 receptors in the CNS, which inhibits vomiting. It also stimulates 5-HT4 receptors in the enteric nervous system (ENS), which promotes gastric motility.
-
How does metoclopramide affect dopamine receptors?
It inhibits both pre- and post-synaptic dopamine (D2) receptors.
-
What is the effect of metoclopramide on 5-HT3 receptors?
It inhibits 5-HT3 receptors in the central nervous system (CNS).
-
What effect does metoclopramide have on vomiting?
Metoclopramide inhibits vomiting by blocking dopamine (D2) receptors in the CNS.
-
Which receptors in the enteric nervous system does metoclopramide stimulate?
It stimulates 5-HT4 receptors in the enteric nervous system (ENS).
-
What is the term for a drug that promotes gastric motility?
Prokinetic
-
What are the relaxant effects of dopamine on the gut?
Dopamine activates D2 receptors in the lower esophageal sphincter and stomach (fundus and antrum), leading to relaxation.
-
What is the overall effect of dopamine on the gut?
Dopamine has mixed effects on the gut. It may induce contraction in the proximal small intestine but relaxation in the distal small intestine.
-
How does dopamine inhibit the release of acetylcholine (ACh)?
Dopamine inhibits the release of ACh from intrinsic myenteric cholinergic neurons by activating pre-synaptic D2 receptors.
-
Which receptors does dopamine activate in the lower esophageal sphincter and stomach?
Dopamine activates D2 receptors.
-
What is the consequence of dopamine activation on D2 receptors in the lower esophageal sphincter and stomach?
It leads to relaxation of the lower esophageal sphincter and stomach (fundus and antrum)
-
What is the term for the neurotransmitter released by intrinsic myenteric cholinergic neurons?
Acetylcholine (ACh)
-
How does metoclopramide affect gastric motility?
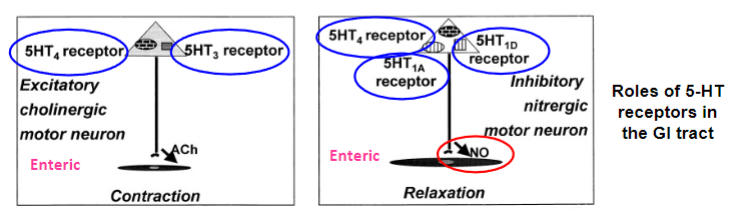
Metoclopramide stimulates presynaptic excitatory 5-HT receptors and inhibits nitregeric neurons, promoting coordinated gastric motility.
-
What are the effects of dopamine on the gut?
Dopamine relaxes the lower esophageal sphincter and stomach (fundus and antrum) by activating D2 receptors. It also inhibits the release of acetylcholine from intrinsic myenteric cholinergic neurons by activating pre-synaptic D2 receptors.
-
Besides its effects on gastric motility, what other utility does metoclopramide have?
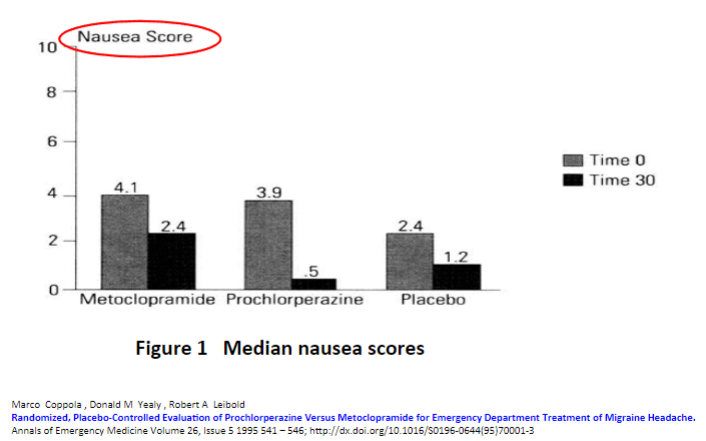
Metoclopramide exhibits antiemetic properties via central effects.
-
Besides its effects on gastric motility and antiemetic properties, what other utility does metoclopramide have?
Metoclopramide relieves headache via central effects.
-
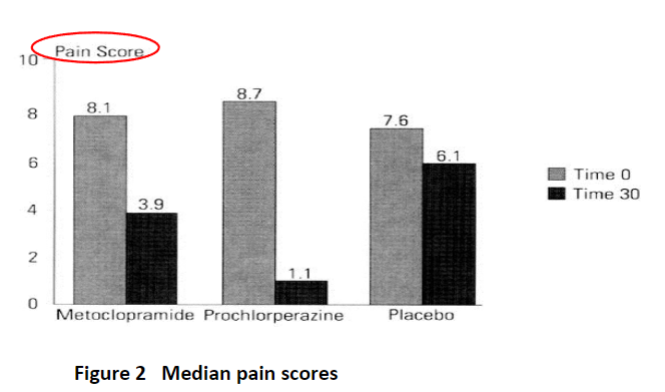
What are the clinical utilities of metoclopramide?
Anti-emetic effects (for nausea due to surgery or cancer) via central pathways
Treatment of gastro-oesophageal reflux disease (GORD)
Relief of symptoms of gastroparesis by promoting gastric emptying and stimulating gastric motility
Pain-killing effects
-
Here's a simplified summary of the effects of metoclopramide:
Here's a simplified summary of the effects of metoclopramide:
Inhibits D2 receptors.
Stimulates the release of ACh / SP from enteric neurons.
Has mixed effects on 5-HT receptors, stimulating excitatory 5-HT4 receptors but inhibiting 5-HT3 receptors.
Stimulates inhibitory nitregic neurons, leading to NO release.
Increases intragastric pressure by increasing lower esophageal sphincter (LOS) and gastric tones.
Stimulates gut motility, improving antro-duodenal coordination and accelerating gastric emptying.
-
What are examples of antispasmodic agents?
Propantheline
Dicloxerine (Dicyclomine)
Mebeverine
-
What is the action of antispasmodic agents on the gastrointestinal tract (GIT)?
They reduce spasms in the bowel by relaxing smooth muscle in the GIT.
-
What is the mechanism of antimuscarinic agents like propantheline, dicyclomine, and mebeverine?
They inhibit parasympathetic activity, thereby reducing spasm in the bowel and inhibiting peristalsis.
-
In which conditions may antimuscarinic agents be useful?
Irritable bowel syndrome and diverticular disease, which can be associated with bacterial overgrowth.
-
What specific gastrointestinal condition may benefit from the use of antimuscarinic agents?
Jejunal diverticular disease.
-
What are the goals of pharmacological intervention in the management of gastric ulcers?
Reduce acid secretion with H2 receptor antagonists (e.g., famotidine).
Neutralize secreted acid with antacids (e.g., Gaviscon).
Attempt to eradicate H. pylori infection.
-
How does inhibition of acid secretion contribute to ulcer healing?
Inhibition of acid secretion removes constant irritation, allowing the ulcer to heal.
-
For which conditions can drugs be used to inhibit or neutralize gastric acid secretion?
Peptic ulcer
Reflux esophagitis
Zollinger-Ellison syndrome
-
What is a risk factor for the development of gastric ulcers?
H. pylori infection
-
What is the role of H. pylori infection in the development of gastric ulcers?
H. pylori, a Gram-negative bacillus, causes chronic gastritis, which can lead to duodenal ulcer formation.
-
What is the general mechanism of action of antacids?
Antacids neutralize gastric acid.
They increase the pH of gastric acid (peptic activity stops at pH 5).
-
What is the potential outcome of prolonged dosing with antacids?
Prolonged dosing can lead to healing of duodenal ulcers, although they are less effective for gastric ulcers.
-
What are the effects of bismuth chelate (Pepto Bismol) on bowel fluid secretion?
Bismuth chelate decreases fluid secretion in the bowel.
-
How does bismuth chelate protect the gastric mucosa?
It forms a protective base over the crater of the ulcer.
It adsorbs pepsin.
It increases secretion of bicarbonate (HCO3-) and prostaglandins
-
What is the action of bismuth chelate against H. pylori?
Bismuth chelate is toxic against H. pylori and is used as part of triple therapy to eradicate it.
-
What are the potential side effects of bismuth chelate?
It may blacken stool and tongue.
-
Who is bismuth chelate suitable for?
Bismuth chelate is suitable for children aged 12 years and over.
-
When should bismuth chelate not be used in children?
It should not be used in children with chickenpox or flu-like symptoms as it can cause Reye syndrome, affecting the brain and liver.
-
What is the combination therapy used for the treatment of H. pylori infection?
Omeprazole, amoxicillin, and metronidazole
Omeprazole, clarithromycin, and amoxicillin or tetracycline, metronidazole, and bismuth chelates
Lansoprazole, clarithromycin, tinidazole, and bismuth chelates
-
How do drugs like bismuth chelate protect the gastric mucosa?
They provide a physical barrier over the surface/base of the ulcer.
They enhance local synthesis of prostaglandins (PGs).
They promote bicarbonate secretion.
Bismuth chelate has toxic effects on H. pylori, preventing its adherence to the mucosa or inhibiting its proteolytic activity. It also stimulates bicarbonate secretion, increases PG synthesis, and adsorbs pepsin.
-
What are the unwanted effects of bismuth chelate?
Nausea, vomiting, blackening of tongue and feces.
-
What caution should be exercised when administering bismuth chelate to patients with renal impairment?
If a patient has renal impairment, plasma levels of bismuth chelate may rise, causing encephalopathy.
-
What warning should be heeded when using bismuth chelate?
Do not exceed the recommended dose.
-
What advice should be given to patients regarding the use of metronidazole for H. pylori infection?
Adhere to the treatment regimen.
Be aware of the possibility of resistance to metronidazole.
Avoid alcohol consumption while taking metronidazole to prevent a disulfiram-like reaction.
Disulfiram-like reaction can cause severe illness, including unpleasant flushing and nausea due to acetaldehyde buildup.
Do not take metronidazole during the first trimester of pregnancy.
-
What is constipation?
Constipation is a subjective complaint often associated with infrequent or difficult bowel movements.
-
What is considered a normal frequency of bowel movements?
Normal bowel opening ranges from 1 to 3 times per day, although this varies greatly among individuals.
-
Is regularity necessary for normal bowel function?
No, one does not have to be regular to have physiologically adequate bowel function.
-
What are the consequences of constipation resulting from rectal distension?
Headache
Loss of appetite
Nausea
Abdominal distension and stomach pain
-
How does holding fecal matter contribute to the exacerbation of constipation?
Holding fecal matter leads to increased water loss and drier feces, making defecation more painful and difficult.
-
What are some causes of constipation related to decreased motility of the large intestine?
Old age
Damage to the enteric nervous system of the colon, which may affect the initiation of the vago-vagal reflex.
-
What factors can increase colonic motility and improve symptoms of constipation?
Increasing intake of fiber, cellulose, and complex polysaccharides
Consuming bran, certain fruits, and vegetables high in fiber
Using laxatives, although excessive use may lead to decreased responsiveness
Using mineral oil, which lubricates feces
Using castor oil, which stimulates motility of the colon
-
What is the purpose of purgatives in the treatment of constipation?
Purgatives can modulate or hasten food transit in the intestine.
-
What are the types of laxatives used to stimulate the motility of the gastrointestinal (GI) tract?
Bulk-forming laxatives
Osmotic laxatives
-
How do bulk laxatives work?
Bulk laxatives such as methylcellulose and plant gums retain water in the gut lumen, promoting peristalsis. They increase the stool's solid content.
-
What are some examples of plant gums used as bulk laxatives?
Sterculia
Agar agar
Linseed
Bran
Ispaghula husk
-
What are some potential side effects of bulk laxatives?
Bloating and flatulence
-
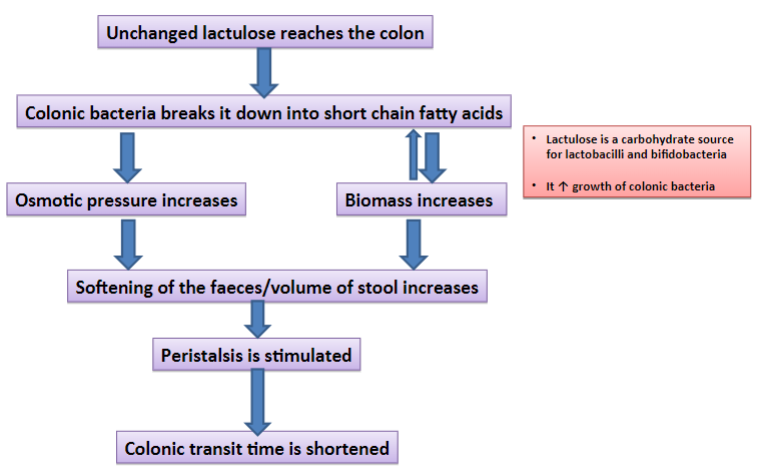
What is the mechanism of action of osmotic laxatives such as lactulose?
Osmotic laxatives like lactulose increase and maintain the volume of fluid in the lumen of the bowel by osmosis.
-
How do osmotic laxatives like lactulose affect gut contents?
They increase the transfer of gut contents into the intestine, leading to an increased volume of gut content entering the colon.
-
What is the consequence of increased volume of gut content entering the colon due to osmotic laxatives?
It causes distension and purgation within approximately 1 hour.
-
What are some potential side effects of high doses of osmotic laxatives like lactulose?
Flatulence, cramps, diarrhea, vomiting, and tolerance may occur with high doses.
-
Picture demonstrating the mode of action of lactulose in constipation: summary
-
What are the general management strategies for diarrhea?
Maintain body fluids and electrolytes.
Identify the causal organism and, if possible, treat with antibiotics (e.g., erythromycin for Campylobacter jejuni).
Modify secretion/absorption balance.
-
What is diarrhea?
Diarrhea is characterized by frequent or very frequent passage of liquid feces.

