-
Anti-infective Agents Overview
1. Broad spectrum vs narrow spectrum: how many organisms they affect.
2. Antibiotics cannot treat viruses, parasites, or fungal infections.
-
Bactericidal vs Bacteriostatic
1. Bactericidal - kills bacteria
2. Bacteriostatic - prevents further growth of bacteria.
3. Goal of antibiotic therapy is to stop infection, giving body to a chance to fight the infection off on its own, brining bacterial load down.
-
What to watch for with Antibiotics/infectives?
1. Allergic reaction
2. Kidney/Liver damage
3. GI toxicity
4. Superinfections
-
How antibiotic resistance happens?
1. Antibiotics kill bacteria causing illness, as well as good bacteria protecting the body from infection.
2. Drug-resistant bacteria are now allowed to grow and take over.
3. Some bacteria give drug resistance to other bacteria.
-
Gram positive vs. Gram negative bacteria
1. Gram-Positive = soft tissue infections.
2. Gram-Negative = GU/GI system
3. s/s of infection are fever, swelling, redness, purlent drainage, wbc elevation.
-
Aminoglycosides
1. Bactericidal antibiotic (broad spectrum)
2. -mycin
3. Watch for: ototoxicity and nephrotoxicity
4. Ex: Gentamycin, tobramycin, streptomycin.
-
Gentamicin
1. Aminoglycoside antibiotic
2. Given IM or IV for: serious Gram-Negative infections (GI/GU).
3. Watch for: kidney issues, loss of hearing, GI upset.
4. GI upset alone is not cause to d/c antibiotics, allergic reactions may be weighed against how severe infection is.
-
Carbapenems
1. Bactericidal Antibiotic
2. Broad spectrum
3. -enem ending
4. Use: skin, UTI, intrabdominal, gynecological infections.
5. Can cause: Fatal GI toxicities, Pseudomembranous colitis, seizures.
6. Ex: Etrapenem, Meropenem
-
Cephalosporins
1. Both bacteriostatic and bactericidal
2. Cef- in name
3. Use: Meningitis, pneumonia, UTIs, sepsis
4. S/e: GI upset, superinfection
5. Super infection = superinfection (multiple infections, gut flora is killed off and new bacteria infects where good bacteria was originally; superinfections seen in oral cavity, skin folds, urinary tract, anywhere it is moist and warm) opportunistic infection based off the killing of good bacteria.
6. Ex: Rocephin, Ominicef
-
Fluoroquinolones
1. Bactericidal Antibiotic
2. Resistant strands emerging
3. -oxacin ending
4. Use: UTI, respiratory, skin infections
5. s/e: CNS: HA, dizziness, insomnia, depression, tendonitis/tendon rupture, GI upset
6. Ex: Ciprofloxacin, Levofloxacin
-
Ciprofloxacin
1. Given IM or IV for: multiple gram-negative infections, anthrax
2. Watch for: GI upset, CNS effects
-
Penicillins
1. Broad-spectrum antibiotic
2. Lots of resistant bacterial strains
3. Interfere with cell-wall building
4. Lots of pts w/ allergies to penicillins
5. Use: respiratory infection and syphilis
6. S/e: GI upset / allergy
-
Amoxicillin
1. Given IM or IV for: respiratory infections, UTIs, oral infections, H-pylori, prophylactic
2. Watch for: GI upset, bone marrow suppression, rash / allergy
-
Sulfonamides
1. Bacteriostatic antibiotic
2. Not used often, but work for UTIs
3. Many pts allergic to sulfa drugs
4. Low cost option
5. S/e: Crystalluria/hematuria, GI upset
6. Ex: Cotrimoxazole
-
Tetracyclines
1. Bacteriostatic antibiotic
2. Significant resistance
3. Becomes Toxic when expired
4. -cycline ending
5. Use: Acne, GU infections
6. S/e: damage to teeth and bones, gi upset
7. Ex: tetracycline, doxycycline
-
Antimycobacterial
1. Interfere with DNA and RNA
2. Use: TB and Leprosy
3. S/e: CNS dysfunction: HA, dizziness, hallucinations, GI upset, liver toxicity.
4. Ex: Leprosy = dapsone, TB 1st line = Isoniazid, rifapentine, TB 2nd line = ethionamide, rifabutin.
-
Isoniazid
1. Antimycobacterial
2. Given PO: first line treatment for TB given in a multidrug treatment. Long treatment time is required.
3. Watch for: liver dysfunction, peripheral neuropathy, GI upset.
-
Ketolides
1. Given for pneumonia
2. GI/CNS effects
3. EX: telithromycin
-
Lincosamides
1. Similiar, but more toxic than macrolides.
2. Ex: Clindamycin
-
Lipoglycopeptides
1. Given for skin infections and staph infections
2. Ex: Vancomycin
-
Macrolides
1. Given for respiratory infections and UTIs
2. Ex: erythromycin
-
Oxazolidinones
1. Used for skin and respiratory infections
2. MAO inhibitors
3. Ex: azithromycin
-
Monobactam antibiotics
1. Very little cross resistance
2. Liver toxicity
3. Ex: aztreonam
-
Vancomycin
1. Lipoglycopeptide drug
2. one of our few remaining defenses against MRSA.
3. High risk to fetus.
4. Get trough lab draw if ordered as it has a narrow therapeutic window.
5. Watch for: Prolonged QT interval, Foamy urine, GI upset
-
Antibiotic nursing considerations
GI upset
Continue full course
Small meals
Skin assessments for fungal infections.
Monitor for allergies
IV assess
Monitor effectivness
Always get culture and sens before starting antibiotic.
Encourage fluid intake
Assess for super infections.
Caution in pregnancy or breastfeeding.
-
Antifungal Agents Overview
1. Spores can travel through the air.
2. Primary (inhaling) or opportunistic infections (part of body's flora, can be due to immunocompromise)
3. Rigid cell walls (why antibiotics dont work)
4. Like warm, moist places and sugars
5. Systemic infections can affect lungs, CNS, and abdomen.
6. Immunocompromised patients
-
Antifungal Agents
1. Systemtic antifungals: azole antifungals, polyenes
2. Topical antifungals: "-zole" ending
-
Azole Antifungals
1. Work by blocking sterol in the fungal wall
2. Can be toxic to the patient.
3. Many drug-to-drug interactions
4. Can interferer with normal human steroids
5. Ex: fluconazole*, ketoconzaole (1st one), Itraconazole.
-
Fluconazole
1. Azole antifungal
2. Given PO or IV: used for systematic yeast infections as well as more topical infections such as vaginal, oropharyngeal, etc.
3. Watch for: liver toxicity
4. Labs need to be drawn for liver toxicity if more than one dose. typically only 1 dose given.
-
Polyenes Antifungals
1. Treat fungal infections by binding to fungal cells.
2. Ex: Amphotericin B - severe systemic infections (hard on kidneys) , Nystatin* - topical infections such as candidiasis
-
Nystatin
1. Polyene antifungal
2. Given PO or IV: for candida infections. topical, powder, cream, suspension - swish and spit, swish and swallow.
3. Things to watch for: Skin irritation, GI upset
4. Teach administration
5. Perform Oral care afterwards and swish around for 2 minutes. Spit out or swallow depending on order.
6. Can be placed on broken skin. avoid incisions where it could be systemic.
-
Topical Antifungals
1. Alter cell permeability of the fungal cells.
2. Creams, sprays, suppositories, and powders.
3. Monitor skin integrity.
4. Ex: Clotrimazole (Lotrimin)
-
Antifungal Nursing Considerations
1. Labs for anything systematic and long term: kidney and liver function.
2. Common S/e: n/v, hyperglycemia, lethargy/sleepiness, rash.
3. Interventions: assess skin/mucus membranes, good hygiene, pillowcases between skin, apply creams in a thin layer, monitor nutrition status, watch those who are immunocompromised, d/c with pain or burning.
-
What is a virus?
1. Segments of DNA and RNA encased in a protein coat-noncellular.
2. Must enter a cell to survive.
3. Use a tail or spike proteins to enter the cell.
4. Hard outer shells that are resistant to antibiotics.
-
Influenza and Respiratory Agents (viruses)
1. Common respiratory virsues: Influenza A, B, RSV
2. Unknown MoA, most likely uncoating the virus.
3. Children and elderly most at risk.
4. Watch for: renal dysfunction, contraindicated with pregnancy, cns: dizziness, insomnia, orthostatic hypotension.
5. Ex: Rimantadine, Amantadine, Zanamivir
-
Rimantadine
1. Antiviral
2. Given PO: influenza A - prophylactically or to treat
3. Watch for: CNS: dizziness, insomnia, depression, Orthostatic hypotension.
-
Herpes and Cytomegalovirus Agents
1. Given for multiple herpes infections, viral eye, respiratory and liver infections.
2. Affect viral substrates to break the DNA into fragments.
3. Don't affect host cells as much, different substrates.
4. Watch for: tremors, CNS: HA, depression, vertigo, nephrotoxicity
-
Acyclovir
1. Herpes agent / antiviral
2. Given PO and topically for: herpes simplex, genital herpes, shingles and chicken pox.
3. Watch for: CNS: dizziness, insomnia, depression, orthostatic hypotension
-
HIV Overview
1. transmission: unprotected sex, needles, mother-child, blood.
2. RiskFactors: unprotected sex, multiple partners, drug use, STIs, anal sex,
3. Testing: Antibody, antigen, Nucleic acid tests
4. Stages/Classification: acute=initial stage of flu like symptoms, Clinical latency (chronic) stage = virus is active but reproduces are low levels. AIDS = final stage where immune system is severely damaged.
5. Prognosis: hiv is a manageable chronic conditions Antiretroviral therapy is primary treatment.
-
Agents for HIV and AIDs
1. Given for HIV
2. The virus attacks the CD4 (helper T cells)
3. These drugs work in multiple ways to block the virus from replicating.
4. Without a healthy immune system, the body is prone to opportunistic infections: TB, yeast, etc.
-
Classes of HIV drugs
1. Non-nucleoside Reverse transcriptase inhibitors
2. Nucleoside reverse transcriptase inhibitors
3. Protease inhibitors
4. Fusion inhibitors
5. Integrase inhibitors
-
Nonnucleoside ReverseTranscriptase Inhibitors (NNRTIs)
1. Bind directly to HIV reverse transcriptase and prevent the formation of HIV DNA.
2. Ex: nevirapine, efavirenz
3. Watch for: flu symptoms, loss of appetitie, CNS effects
-
Nucleoside ReverseTranscriptase Inhibitors (NRTIs)
1. Compete with the body's natural nucleosides needed for viral development.
2. Ex: zidovudine, abacavir, tenofovir
3. Watch for: hepatomegaly, bone marrow suppression / anemias.
-
Zidovudine
1. NRTI
2. watch for: bone marrow suppression, neutropenia, anemia, liver dysfunction, lipodystrophy
3. can help prevent maternal/fetal transmission
-
Protease inhibitors
1. PIs
2. Block the protease needed for HIV maturation.
3. Ex: fosamprenavir, atazanavir
3. Watch for: CNS: mood changes, fat redistribution - buffalo hump
-
Fusion inhibitors
1. Block the receptor site on the CD4 cell, preventing the virus from entering the cell.
2. Ex: enfuvitridie
3. Watch for: CNS: insomnia, depression, neuropathy.
-
CCR5 coreceptor antagonists
1. Block the receptor site on the CD4 cell, preventing the virus from entering the cell.
2. Ex: maraviroc
3. Watch for: CNS: dizziness, hepatoxicity
-
Integrase inhibitors
1. Block the enzyme needed to insert viral DNA replication
2. Examples: Raltegravir, dolutegravir
3. Watch for: CNS: HA, dizziness, rhabdomylosis
-
Anti-Hepatitis B Agents
1. Hepatitis B is spread through blood, sexual contract and contaminated needles.
2. 3 Primary antiviral drugs that inhibit transcriptase. Pts need to keep taking the antiviral for the entire course.
3. Watch for: CNS: HA, dizziness, monitor liver function, nephrotoxicity.
4. Ex: Adefovir, Entecavir
-
Anti-Hepatitis C Agents
1. Hepatitis C is spread through blood, mother/fetal transmission, sexual contact, and contaminated needles.
2. New drugs are protease inhibitors used in combination with other antiviral agents.
3. Cost of course is very expensive.
4. Watch for: severe skin rash, fatigue.
5. Examples: simpeprevir, daclatasvir
-
Nursing Considerations for Antiviral Agents
1. HIV: compliance to prevent resistance - 95% or greater. Pill count to determine compliance. Assess for opportunistic infections (leading cause of death), assess for s/e, assess for illegal or other drug interactions
2. Other antivirals: finish the course, watch for CNS issues, monitor liver and kidney function.
-
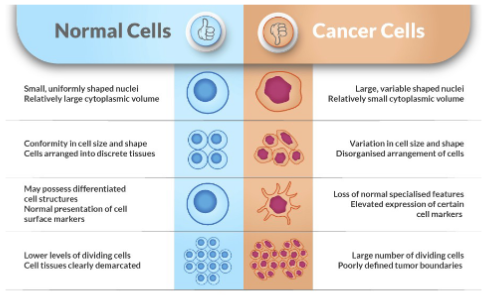
Normal cells vs cancer cells
-
Cancer overview
1. Causes of cancer: genetic, environmental, lifestyle, infections, hormones, age
2. Solid tumors: Carcinomas = cancers that originate from epithelial cells which line the surface of organs and tissues. They are the most common type of cancer.
Sarcomas develop in connective tissues, including bones, muscles, fat, blood vessels, and cartilage. Less common.
3. Hematological malignancies -blood cancers, originate in the bone marrow and affect the blood, bone marrow, and lymphatic system. They include leukemia, lymphoma, and myeloma.
4. Metastasis- development of secondary malignant growths at a distance from a primary site of cancer.
-
Cell Cycle
1. Cell-cycle specific drugs
2. Cell-cycle non specific drugs
3. Growth fraction, how many cells
4. Doubling time, how fast
-
Antineoplastic treatment overview
1. Kill fast growing cells or boost immune system.
2. Combination chemotherapy
3. Adjuvant chemotherapy
4. Neoadjuvant chemotherapy
5. Palliative chemotherapy
6. Purpose of chemotherapy
-
Side effects of neoplastic agents
1. Chemotherapy is most effective on fast growing cells.
2. Which cells grow fast? skin, hair, gi tract, mucous membranes, bone marrow, reproductive system- fetuses etc.
3. Nadir lowest blood count 7-10 days after treatment.
-
Alkylating Drugs
1. Cause damage to the cell's DNA preventing reproduction through intra-strand and cross-linking connections.
2. Work in the G0 Phase, good for slow growing cancers- wide variety of cancers, severe vesicants
3. Ex: chlorambucil
4. Watch for: hepatic and renal toxicity - hemorrhagic cystitis, contraindicated with pregnancy, maxillary burning with infusion.
-
Antimetabolites
Mimic natural metabolites to suppressgrowth and division• Work in the S phase, good for fastgrowing cancers• Cell resistance limits usefulness –combination therapyExamples: Methotrexate, 5-FluoroucilWatch for:Toxic GI effectsPulmonary toxicityCNS: fatigue, dizzinessPregnancy Category X
-
Methotrexate
Inhibits folic acid reductaseGiven PO or IV forMany cancersThings to watch for:Ulcerative Stomatitis (mouth)Hepatic and renal toxicityPregnancy category X
Severe bone marrow suppression
-
Antineoplastic Antibiotics
Interfere with DNA links and prevent replication Are effective in all phases of the cell cycle Effective with fast growing cellsExamples: Doxorubicin, BleomycinWatch for: Respiratory toxicity Cardiac toxicity Severe vesicants
-
Doxorubicin
Antitumor AntibioticGiven IV forBreast, gastric, and ovarian cancers, as well assarcomas, leukemias, and lymphomasThings to watch for:Irreversible cardiomyopathy – routineechocardiogramsSevere VesicantRed tinged urine and tears for 48 hours afterwardsFlu-like symptoms
-
Miotic Inhibitors
Block or alter DNA synthesis during mitosis(division)Effective in the M phase, good for fastgrowing cellsExamples: Vincristine, PaclitaxelWatch for: Ataxia (poor muscle control), musclewasting Neurotoxicity – stocking glove syndromePacific Yew Tree -Paclitaxel
-
Vincristine
Miotic Inhibitor derived from the MadagascarperiwinkleGiven IV forHodgkin disease, non-Hodgkin lymphoma,neuroblastoma rhabdomyosarcomas, Wilms tumors,and lymphocytic leukemiaThings to watch for: Neurotoxicity – Neuropathy in the hands or feet,seizures, sensory loss/ vision
Gi - paralytic ileus
-
Hormones and HormoneModulators
Not true chemotherapy, but blockhormonal receptor sitesEffective for cancers that useestrogen to growTreat breast, prostate cancer, etc.Examples: Tamoxifen, LetrozoleWatch for: Hypercalcemia Menopausal symptoms Increased clotting: CVA, MI, PE
-
Tamoxifen
Selective Estrogen ReceptorModulatorGiven PO forBreast cancerThings to watch for:Increase risk of clotting – PE, stroke,MIFatigue, Pain – dose limitingVaginal bleeding/ irregular menses
-
Cell Specific Agents(Targeted Therapies)
Cytostatic rather than cytotoxicTarget proteins and genes in cancer cellsTarget molecules involved in tumorgrowth, progression, and spreadTargeted rather than killing all fast-growing cells
-
Protein Tyrosine KinaseInhibitors
Gene mutation in cells create abnormalactive BCR-ABL tyrosine kinase enzyme Philadelphia chromosome must bepresent Doesn’t affect healthy cellsExamples: Imatinib, gefitinibWatch for: New cancers Cardiac toxicity Bone marrow suppression
-
Imatinib
Tyrosine Kinase Inhibitor given PO forleukemia, other blood cell cancers, GI tumordermatofibrosarcoma protuberansThings to watch for: Periorbital edema Muscle and bone pain Heart failure (hypokalemia)
-
Other Cell-Specific Inhibitor
Proteasome inhibitors –multienzyme complexes that degradeproteins inside the cell that leads to celldeathExample: BortezomibWatch for: Serious multisystemeffectsAngiogenesis Inhibitors – blocksVEGF to prevent the growth of new bloodvessels and inhibit tumor growthExample: Bevacizumab
Watch for: poor wound healing
-
Toxicityand Ports
Vesication – blistering oftissueTissue necrosisRashesCellulitis
-
Nursing Considerations forAdministration
Avoiding exposurePPE for hanging anddisconnecting:Gloves (double)GownGogglesFull face shieldRespiratory barrier
-
Neutropenic precautions
Strict hand hygienePrivate room with door closedPt should wash handsBathe dailyBrush teeth twice dailyPrevent constipationDo not use tampons or douchesDo not share personal items with anyoneAvoid fresh flowers, live plants and standing waterDon’t clean up after your petNo raw foods – cook foods thoroughlyClean kitchen surfaces wellNo sick visitors
-
New Treatments for Cancer
Microbiome treatments Using gut flora to boost the immune system Strain of E. Coli that infiltrates cancerous tumors and releasedanti-cancer drugs when stimulated with ultrasoundPersonalized vaccines – Messenger RNACRISPR – gene editing

