-
Heparin NC
1. Monitor VS, signs of bleeding, nurse assessment
2. Platelets > 100,000
3. Baseline labs: aPTT, CBC (platelets, hematocrit/hemoglobin rbc)
4. SC administration - 2 inches away from umbilicus
5. Patient teaching - electric razer, soft toothbrush, bleed more, blood stool, things are getting worse
6. High Alert Med: 2 RN check
-
Heparin
1. Anticoagulant: Both a Factor Xa and Thrombin Inhibitor
2. SC, IV
3. aPTT
4. Protamine IV for heparin reversal
5. SE: bleeding/hemorrhage, thrombocytopenia, allergy (rash, hives, itching)
6. Contraindications: uncontrolled bleeding, thrombocytopenia, invasive procedures or surgery, pregnancy, concurrent use of aspirin or NSAIDs.
-
enoxaparin (Lovenox)
1. Anticoagulant: Factor Xa specific
2. Low molecular weight heparin - longer half life, lasts longer than heparin
3. Home use, does not require regular blood work. more predictable
4. SE: Bleeding, injection site irritation/bruising
5. Contra: major bleeding, history of heparin induced thrombocytopenia, pregnancy, concurrent use of aspirin or NSAIDs.
6. SC route lower abdomen preferred
7. Do not expel the air bubble from the prefilled syringes before the injection, to avoid loss of drug.
8. Do not rub on site after injection to prevent bruising etc
-
warfarin (Coumadin)
1. Anticoagulant: Vit. K antagonist
2. route: PO
3. INR (international normalized ratio) therapeutic target: 2-3, once a week checkup for labs
4. Full therapeutic effect in 3-5 days
5. SE: bleeding
6. Reversal: Vitamin K
7. Contraindications: Pregnancy, bleeding, invasive procedures, surgery, pregnancy, vitamin K deficiency.
-
warfarin NC
1. Monitor VS, nurse assessment, signs of bleeding
2. Patient teaching
3. Monitor intake of food high in Vitamin K: dark green leafy vegetables. Consistent and moderate intake
4. Many drug interactions, check with provider on new medications. Highly-protein bound
5. Monitor INR.
-
Categories of Antiplatelet Drugs
1. Salicylates
2. Adenosine diphosphate receptor (ADP) inhibitors
3. Glycoprotein inhibitors
4. Arterial vasodilates
-
Aspirin (salicylate)
1. Prevent cardiovascular and cerebrovascular events
2. Long term anticoagulation therapy
3. Side effects: GI distress, bleeding
4. Contra: children w/ flu symptoms can cause reyes syndrome, last trimester of pregnancy, in combination with NSAIDs or anticoagulants, foods containing salicylates (spinach, brocolli)
-
Salicylate Nursing Considerations
1. Antiplatelet effect for 7-10 days (non-reversible effect)
2. Small amount needed for antiplatelet effect
3. Avoid alcohol
4. D/c prior to invasive procedures, surgery/dental
5. Take with food: GI upset
6. Monitor for signs of bleeding
7. Patients w/ asthma 20% also have sensitivity to salicylate
-
Salicylate posioning
1. inc temp
2. tinnitus
3. n/v
4. lethargy/excitability
5. hyperventilation leading to respiratory alkalosis
6. severe toxicity = metabolic acidosis, seizures.
7. Toxic level for 30lb kid = 12 adult or 48 baby aspirins.
-
clopidogrel (Plavix)
1. Antiplatelet: ADP inhibitor
2. Mech of action: blocks ADP receptors of platelets
3. PO once daily
4. Irreversible effect on the platelet. 7-10 days
5. SE: GI upset, bleeding, thrombocytopenic purpura (TTP)
-
clopidogrel (Plavix) NC
1. take with food to minizmie GI effects. Can be taken without food
2. discontinue 5-7 days prior to surgery
3. patient teaching
4. monitor for bleeding / periodic platelet count
5. Contra: peptic ulcer disease, bleeding disorders, thrombocytopenia, intracranial bleeding.
6. Proton pump inhibitors reduce effects
7. Herbal supplements increase bleeding risk
-
Heart Failure
1. Heart unable to pump blood effectively through the body
2. Pulmonary edema
3. Peripheral edema
4. Left sided HF - fluid in lungs, sob, cough, difficulty breathing, crackles in lungs
5. Right sided HF - fluid backs up into extremities and abdomen.
6. Fatigue, cough, plural effusion (fluid outside lung), swollen leg/ankles
-
Diuretics
1. Thiazides
2. Potassium-sparing
3. Loop diuretics
-
Hydrochlorothiazide
1. Thiazide diuretic
2. PO
3. SE: Hypokalemia
4. pts should Eats food rich in potassium, can cause Hyperglycemia
5. Monitor for symptoms of electrolye imbalance (K, Na)
6. SE: Electrolyte imbalance, dehydration, increased uric acid levels (gout), confusion numbness, cramps, constipation
6.5: Low sodium = seizures/death, confusion, headache, muscle weakness
7. Caution: pregnancy, breastfeeding, renal or hepatic disorders, older adults
8. Not used in emergency situations, does not work quickly
-
furosemide (Lasix)
1. Loop diuretic
2. PO, IM, or IV
3. Hypokalemia: potassium supplement
4. Black box warning: fluid and electrolyte depletion
5. Orthostatic hypotension
6. Ototoxicity: tinnitus
7. SE: dehydration, hyperglycemia, hyperuricemia
8. Caution in diabetes, older adults, pregnancy/lactation, renal/hepatic impairment.
9. emergent use
-
spironolactone (Aldactone)
1. Potassium-sparing diuretic
2. PO
3. Increased urine output is minimal
4. may be combined with thiazide or loop diuretic
5. SE: hyperkalemia, endocrine related side effects.
6. Take with food, can crush or chew
7. Avoid high K+ foods
8. Contraindications: pregnancy, renal insuffiency
9. Slow acting, not for emergencys.
-
Diuretics NC
1. Give dose in the morning
2. caution in older adults
3. monitor electrolyte values and assess for symptoms
4. dehydration assessment including VS (low bp, skin turgor would tent, mucous membranes dry)
5. hypotension
6. monitor response
7. pt education on symptoms to report.
-
Heart Failure Pathophysiology
1. Heart muscle weakens and enlarges ventricle
2. Inability to to pump blood
3. Increase in preload (volume in ventricle pre pump) and after load (volume in ventricle post pump).
4. Reduced cardiac output. (heart is demanding more oxygen)
-
Left Sided Heart Failure
1. Blood backs up into lungs. (heard as crackles)
-
Right sided HF
1. Blood backs up into the peripheral tissues. (edema in legs, puffy)
-
Cardiac Glycosides
1. Naturally occurring cardiac glycosides are found in plants: Digitalis
2. Inhibits the Na-K pump (allows Ca to go into the cells, allowing for actin myosin muscles to contract in heart, forcing a bigger contraction/squeeze)
3. Positive inotropic action (contract with more force)
4. Negative chronotropic action (decreased HR, slowing conduction of electricity)
5. Negative dromotropic action
(decreases velocity of conduction speed of electical impulse in heart)
-
digoxin (Lanoxin)
1. Cardiac glycoside
2. Treats HF and atrial fibrillation (not a first line drug)
3. Half-life = 30 to 40 hours
4. Therapeutic serum levels = 0.8-2 ng/mL
5. Route = PO or IV
6. Pediatric - elixir form or IV
7. Antidote (can reverse toxicity) = digoxin immune fab (Digibind)
8. Adverse reaction: Cardiac dysrhythmias
-
digoxin Toxicty
1. Blood levels above 2 ng/mL
2. Bradycardia
3. nausea/vomiting, headache, blurred vision, visual illusions confusion.
-
Digoxin and Potassium
1. Normal K levels 3.5-5 mEq/L
2. Hypokalemia increases the effects of digoxin (pt will become toxic)
3. Low potassium levels = dig. toxicity
4. Drugs that cause hypokalemia = Potassium wasting diuretics (hydrochlorothiazide and furosemide) and cortisone preparations
5. Eat food high in potassium to combat potential toxicity.
-
Digoxin Assessment and Teaching
1. Drug and herbal history: St. John warts reduces absorption of digoxin.
2. Baseline heart rate (>60 HR to give digoxin in adults) (>90 HR to give to infants)
3. Foods high in K are: banana, avocado, broccoli, lima beans, beets, dark greens, sweet potato.
4. Monitor digoxin levels
-
Digoxin Drug Card
1. Classification/MoA: improves contractility by allowing Ca into the cell
2. Indications: HF, afib
3. Contra: bradycardia (<60, <90 infants), Hypokalemia (K range 3.5-5 mEq/L)
4. 0.8 - 2 ng/mL = therapetuic levels
-
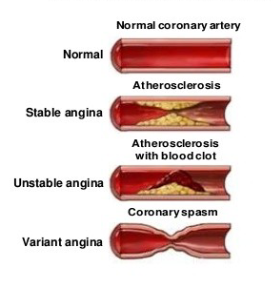
Three types of Angina
1. Stable angina or Classic Angina or Effort angina
2. Unstable angina (Crescendo)
3. Variant angina (Prinzmetal)
4. Atherosclerosis is the buildup of fats, cholesterol and other substances in and on the artery walls. This buildup is called plaque. The plaque can cause arteries to narrow, blocking blood flow.
-
Nitrates
1. Generalized vascular and coronary vasodilation
2. Indications: angina (treatment and prophylaxis)
3. SE: hypotension, headaches, dizziness, syncope, flushing (reflex tachycardia if given too rapidly)
4. Drug interaction: Erectile dysfunction medications.
5. Large first pass effect (oral administration is not optimal)
-
Nitrate Sublingual route
1. Cannot be exposed to light or heat
2. If no relief after 5 mins, call 911 and may take second tablet; max of 3 tablets in 5 minute increments.
3. Place under tongue; do not swallow or chew.
-
Nitrate Topical (patch + ointment)
1. Wear gloves
2. Remove old ointment; do NOT massage
3. Apply to upper arms or chest (non-hairy)
4. Rotate sites; remove at bedtime. Never put on a implanted defibulator. (this is to avoid a nitroglycerin tolerance)
-
Nitrate Oral Route
1. Prophalyatic, need moisture in mouth to be effective
2. Translingual spray (mouth spray)
3. IV solution
-
Hypertension
1. known as "silent killer"
2. major risk factor for stroke, cardiovascular disease, and renal failure
3. Defined as 140/90 and above
4. Primary - unknown origin (90% of all cases)
5. Secondary - 10% of all cases
6. Risk factors - family history, increased age, alcohol/tobacco use/ethnicity, obesity, DM, diet, stress.
-
BP formula
BP = HR x SV (stroke volume) X PVR (peripheral vascular resistance)
-
Diuretics
1. MoA: increase removal of sodium and water by the kidnyes
2. First line therapy for HTN
3. Indications: HTN
4. Adverse effects: hypotension, hypo/hyperkalemia, tinnitus
5. Examples: thiazide - hydrochlorothiazide (HCTZ), loop - furosemide (Lasix), Potassium sparing - spironolactone (Aldactone)
6. Diuretics lower stroke volume to lower BP
-
Beta1 and Beta2 BP considerations
1. Beta1: found on heart muscle, epi binds to b1 and increases hr and strength of contractility
2. Beta2: skeletal muscle (tremors), bronchioles of the lungs(bronchodilation), large arteries of the legs (vasodilation)
3. Non-selective: blocks beta1 and beta 2
4. Selective: block b1 only.
-
Beta Adrenergic blockers (-olol, ilol)
1.MoA: block sympathetic nervous system repsonse
2. indications:
3. se: bradycardia
4. non-selective: propranolol (inderal), carvedilol (coreg)
5. selective: atentolol (tenormoin_, metoprolol (lopressor)
6. don't stop abruptly.
-
Angiotensin Converting Inhibitors (ACE inhibitors) (-pril)
1. MoA: inhibits the formation angiotensin II (vaso constrictor) and blocks release of aldosterone.
2. SE: dry cough, hypotension, hyperkalemia.
ACE = Angioedema (swelling underneath skin), cough, elevated potassium, neutropenia (low wbc)
3. Changes PVR (peripheral vascular resistance) to lower BP.
4. Can't give ACE inhibitors to pregnant women as it reduces blood flow the the placenta.
5. NSAIDS (ibuprofen, advil) decrease effectiveness of ACE inhibitors.
6. can cause lithium toxicity if taking lithium
-
Angiotensin Receptor Blockers (-sartan)
1. MoA: block angiotensin II and release aldosterone
2. SE: hypotension, hyperkalemia
3. Adverse effects- angioedema
4. doesn't cause the cough that ACE inhibitors cause.
5. Works on SV and PVC to lower BP.
6. can't give to pregnant woman.
-
Calcium channel blockers (-dipine)
1. MoA: blocks calcium channels in vascular smooth muscle
2. Relax peripheral arterioles, relax coronary artery spasm, negative inotropic effect.
3. Ends in (-dipine), Verapamil (Calan), diltiazem (Cardizem)
4. SE: headache, hypotension, dizziness, flushing, reflex tachycardia, edema, constipiation, gingival hyperplasia.
5. Do NOT take with grapefruit juice
6. Do not stop taking abruptly. (rebound hypertension)
7. Lowers BP by relaxing PVR.
-
Cultural Considerations for treating HTN
1. Beta blockers and ACEI are not the best option for african-americans unless combined with a diuretic
2. Alpha1 blockers (rarely used) and calcium channel blockers are effective for African americans.
3. Asian americans are more sensitive to beta blockers.
4. Native americans have lower response to beta blockers.
-
General Teaching for HTN meds
1. Side effects - orthostatic hyptoension; erectile dysfunction, change position slowly
2. Don't take OTC cold medications without consulting the health care provider.
3. Don't stop drugs abruptly (rebound hypertension)
4. Therapy is often life-long
5. Monitor your BP weekly
6. Avoid grapefruit juice
7. Can be on multiple antihypertensive medications (usually 2+)
-
Bile Acid Sequestrants
1. Cholestramine (Questran) = powder
2. Colesevelam (Welchol) = tablet
3. Reduces LDL
4. Binds with bile acid in the intestine
5. Powder mixed with juice or water
6. SE: GI upset; constipation; bloating, increase fluids, bulk foods; fiber.
-
Fibrates
1. Gemfibrozil (Lopid)
2. Reduces triglyceride and VLDL levels.
3. Don't take with anticoagulants (increase bleeding)
4. SE: abdominal discomfort; headache; prolonged PT/INR time; increased risk for gallstones.
-
Nicotinic Acid
1. Niacin (Vit. B3)
2. Reduces VLDL and LDL
3. Takes with meals
4. Numerous side effects: flushing, careful titration and patient teaching, concomitant use of aspirin, vasodilation.
-
Sttatins: HMG CoA Reductase Inhibitors (-statins)
1. Avorvastatin (Lipitor), Rosuvastatin (Crestor), Simvastatin (Zocor)
2. Inhibit cholesterol synthesis in the liver.
3. Decreases cholesterol concentration and LDL and increases HDL.
4. SE: GI disturbances, headaches, muscle cramps (rhabodymyasis), fatigue.
5. Monitor liver enzymes, annual eye exam (cataracts), lifelong therapy, pregancy cat x drug.
-
Cholingergics
1. Stimulate PNS = Cholinergic Agonist
2. Block PNS = Cholinergic Blockers
-
Cholinergic Receptors
1. Muscarinic - stimulates smooth muscle and slows the heart rate
2. Nicotinic - stimulates skeletal muscle and excitatory response
-
Types of Cholinergic Drugs
1. Direct acting / Cholinergic Agonsits - bind or act on receptors to activate a response.
2. Indirect acting / Anticholinesterase - inhibit the action of the enzyme cholinesterase.
-
Direct Acting Cholinergic Agonists
1. bethanechol (urecholine) and pilocarpine (pilocar, ispto carpine)
-
bethanechol (Urecholine)
1. DIRECT acting cholinergic agonist
2. Indications: Urinary retention
3. SE: hypotension, bradycardia, blurred vision, excessive salivation, diaphoresis, diarrhea (fecal incontinence), bronchoconstriction, dizziness/fainting
4. Contraindications: ulcer, asthma, cad, hypotension, bradycardia
5. STUPID: syncope, tearing, urgency, prior to meals, I/O, diaphoresis
-
pilocarpine (Pilocar, Isopto Carpine)
1. Direct Acting Cholinergic agonist
2. Indication: Glaucoma
3. SE: decreased visual acuity, headaches, systemic effects
4. Apply pressure to nasolacrimal sac after eye drops
5. Use caution: Chronic respiratory conditions and hypertension.
6. Contra: Acute eye disorders, retinal detachment.
-
echothiophate (Phospholine Iodide)
1. Cholinesterase Inhibitor
2. Indication: Glaucoma
3. SE: myopia (decreased visual acuity), long term use = cataracts, systemic absorbtion
4. Apply pressure to nasolacrimal sac after eye drops
5. Contra: retinal detachment
6. NI: administer infection prevention, at night, each eye 5 mins apart, safety at night (can't see)
-
Cholinergic Nursing Considerations
1. Baseline VS: orthostatic hypotension, heart rate
2. Assess urine output: report less than 30 mL/hr
3. Assess lung sounds
4. Give 1 hour before or 2 hours after meal
5. Monitor liver enzymes
6. Antidote.
-
Cholinergic Crisis / Poisoning: SLUDGE-M
1. SlUDGE-M2. Salvation
3. Lacrimation
4. Urination
5. Defecation
6. Gastric upset
7. Emesis
8. Miosis
-
Cholinergic Antagonists
1. Inhibit the aciton of acetylcholine
2. Heart: Increase HR
3. Lungs: Bronchodilation and decreased secretions
4. GI: decreased motility
5. Bladder: decrease in bladder contractions = retention
6. Eyes: Pupil dilation (mydriasis)
7. Decreased salvation
8. CNS: reduced muscle rigidity and tremors.
-
atropine (atropen)
1. Cholinergic Antagonist (antidote)
2. Anticholinergic, acts on muscarinic receptors
3. Indications: Bradycardia, antidote for cholinergic poisoning, preop: decreased salvation
4. SE: tachycardia, palpations, photophobia, blurred vision, dry mouth, urine retention, abdominal distension, impotence.
5. Contraindications: Glaucoma
-
Anti-Cholinergic Side Effects
1. Confusion
2. Pupillary dilation
3. Tachycardia (chest pain, possible MI)
4. Decreased salvation (dry mouth)
5. Decreased peristalsis (constipation)
6. Tightening of the urinary sphincter (urine retention)
7. Can't pee, see, shit, spit
-
Nursing Interventions Anticholinergics
1. Contraindicated in narrow-angle glaucoma and BPH (benign-prostate hypertrophy)
2. Avoid hot temperature
3. Avoid activities that require alertness
4. Oral care
5. Avoid alcohol
6. Prevent constipation
7. Hard candy for dry mouth
-
oxybutynin (Ditropan)
1. Anticholinergic
2. Muscarinic receptors
3. Indication: urinary incontinence
4. SE: dry mouth, constipation, mydriasis, blurred vision, urinary retention, headache, dizziness, heat exhaustion
5. Contraindications: glaucoma, myasthenia gravis (A weakness and rapid fatigue of muscles under voluntary control.), GI/GU obstruction, cardiac dysfunction
-
Cholinergic Summary
1. Cholinergic: stimulate PNS
2. Copies action of Ach (acetylcholine)
3. Treats glaucoma
4. Helps with urinary retention issues (makes them pee)
1. Anticholinergics block PNS
2. Block action of ach
3. antidote for toxicity (atropine)
4. overactive bladder (can make them stop peeing)
-
What is cancer?
1. Body cells grow uncontroably and spread to other parts of the body.
2. Cells ignore signals to stop divison or die.
3. Cells tell blood vessels to grow tumors
4. Cells hide from or trick the immune system
5. Changes in cell chromosomes
6. Rely in a different way on nutrients than normal cells.
-
Drug categories to treat cancer
1. Chemotherapy
2. Hormonal therapy
3. Immunotherapy
4. Targeting therapy
-
Goals of cancer treatment
1. Cancer prevention
2. Cure
3. Control
4. Pallative
-
Cell growth cycle
1. Healthy and malignant cells reproduce the same
2. G1: First phase prepares to make DNA
3. S: makes dna for replication
3. G2: dna synthesis complete, prepares for mitosis
4. M: mitosis occurs
-
How does chemotherapy work?
1. Interferes with cell cycle
2. Halts cell growth and divison of cells
3. leads to cell death
4. cell cycle specific or nonspecific
5. can't tell difference between a healthy cell and a malignant cell
-
Common side effects of chemotherapy
1. Bone marrow suppression (myleosuppression)
2. Nausea / vomitting
3. hair loss
4. fatigue
5. diarrhea or constpiation
6. anorexia, taste, and smell changes
7. nerve damage (neuropathy)
8. Mouth sores (mucosistis)
9. "Chemobrain"
10. Skin and nail changes
-
Bone marrow suppression (myelosuppresion)
1. rbc (anemia)
2. wbc (leukopenia)
3. neutrophils (neutropenia)
4. (platelets (thrombocytopenia)
5. nadir
-
Neutropenia
1. abnormally low count of neutrophils
2. absolute neutrophil count (ANC)
3. Complete blood count (CBC) with differential
4. Mild neutropenia: ANC < 1500 mm^3
5. Servere neutropenia: ANC < 500 mm^3
-
Neutropenic precautions
1. Hand hygiene and daily personal hygiene
2. Report and monitor temperature
3. inpatient reverse isolation
4. wash produce, no raw or undercooked meat
5. no dried flowers or gardening without gloves
6. mask
7. no picking up pet feces
8. avoid those that are ill and avoid crows
9. protect skin
10. avoid others that have had live vaccinations in the last 30 days.
-
Nausea/vomiting: Nursing Interventions
1. Antiemetics administered 30-60 minutes prior to treatment
2. PRN oral antiemetics
3. Food at room temperature, small and frequent meals
4. Frequent mouth care
5. Relaxation or distraction therapy
6. Avoid foods that are a turnoff due to taste or smell
7. Be aware of anticipatory nausea
-
doxorubicin (Adriamycin)
1. Antitumor antibiotic / Anthracycline: Non cell cycle specific
2. Red in color
3. Vesicant (may causes severe and/or irreversible tissue injury and necrosis)
4. IV
5. Red tingered urine and tears x 48 hrs
6. Cardiac toxicity, routine echos required
-
cyclophosphamide nursing considerations
1. bladder toxicty and hemmorhagic cystistis with high doses
2. mesna (drug to reduce hemorrhages)
3. aggressive pre and post hydration for high doses
4. Temporary maxillary burning during infusion
5. PO and IV
-
Cisplatin: Nursing considerations
1. severe nephrotoxicty
2. pre and post hydrations
3. encourage oral fluids
4. tinnitus and high frequency hearing loss
5. hypomagnesemia
6. delayed n/v
-
Methotrexate (MTX)
1. folic acid analog
2. IM, IT, IV, PO, SC
3. Take multivitamin with folic acid
4. leucovorin resuce with high doses
5. strict mouth care
6. Pregnancy category X: during preg and 6 months after
-
Vincristine: nursing considerations
1. Fatal if given any other route than IV
2. vesicant
3. neurotoxicity: dose limiting toxicity (paresthesia, motor weakness, peripheral neuropathy) nerves
4. constipation
-
paclitaxel (taxol)
1. bark of yew tree
2. sensitivity reactions /anaphylaxis
3. premedication to prevent infusion reactions
4. nurse observation for first 15-30 minutes
5. in line filter and non-pvc tubing
-
Chemotherapy is a hazardous drug
1. drugs are considered hazardous if the demonstrate one or more of the following: carcinogenicity (causes cancer)2. teratogenicity: disturbs development of a fetus
3. reproductive toxicity
4. organ toxicity
5. genotoxicity (damage to genetic info)
6. a safe level of occupational exposure to hazardous drugs is unknown. OSHA
-
Routes of occupational exposure
1. absorption through the skin
2. contaminated needlestick
3. inhalation of drug aerosols
4. ingestion by hand to mouth behavior
-
Why do i need to know about chemotherapy safety
1. Patients on active therapy are seen in diverse environments
2. patients living longer on active treatment
3. chemotherapy is in body fluids for up to 48 hrs after treatment
4. you may work near an area where hazardous drugs are mixed or administered.
-
Oral chemotherapy safety considerations
1. Store away from children and pets
2. Never dispose in trash or toilet. Return unused medication to pharmacy or discuss with oncology health care team.
3. Was hand's after handling medication. Do not CRUSH, CHEW or BREAK open capsules.
4. don't double up if you miss a dose
5. adherence is key to effectiveness
6. take at same time of day
7. keep in original container.
-
Immunotherapy
1. Uses the patient's own immune system to manage or eradicate cancer
2. Immunotherapy helps immune system to act better against cancer
3. Immunotherapy categories:
Immune checkpoint inhibitors, treatment vaccines, immune system modulators, t-cell transfer therapy, monoclonal antibodies.
-
Trastuzumab (herceptin) NC
1. targets her2 proteins
2. cardiac toxicity, monitor ejection fraction
3. infusion reactions
4. flu like symptoms after first infusion
5. often used in combination with chemotherapy
6. contraindicated during pregnancy and breast feeding 6 months post treatment.
7. iv and sc
-
Hormonal Therapy
1. hormone-sensitive cancers
2. slows or stops the growth of cancer that use hormones to grow
3. decreases levels of a specific hormone
4. prostate: testorone
5. breast: estrogen receptor (er) and progesterone receptor (pr)
6. side effects impact quality of life
7. primarily oral
-
leuprolide (Lupron)
1. prostate cancer treatment
2. SE: hot flashes, decreased libido, erectile dysfunction and gynecomastia.
3. IM, SC
4. Bone density testing
5. supplement calcium and vit D.
-
tamoxifen NC
1. Breast cancer treatment
2. estrogen receptor blocker
3. PO
4. Prevention and treatment of breast cancer
5. black box warning: thromboembolic events, uterine malignancy
6. SE: mood changes, hot flashs and other menopausal symptoms
-
Targeted Therapy
1. targets proteins that control how a cancer cell grows
2. cancer will have a target for a certain drug
3. little or no effect on normal tissues
4. nontraditional side effect profile: acneiform rash, cardiotoxicity, hepatoxicity, hypertension, metabolic abnormalities
-
Imatinib mesylate (gleevec)
1. protein tyrosine kinase inhibitor
2. PO
3. SE: fluid retention, n/v, myelosuppression, muscle cramps, musculoskeletal pain, diarrhea rash, fatigue, abdominal pain.
4. Contraindicated during pregnancy and lactation
5. Take with a meal and a full glass of water
6. Tablets can be dissolved in a glass of water.
-
Urinary Tract Infection (UTI)
1. infection of the urinary tract
2. more common in women
3. symptoms: dysuria, frequency, hematuria, pressure or cramping, fever, lower back pain, n/v
4. considerations for older adults
5. cranberry juice is used to prevent but is not useful in treating.
-
Urinary tract antiseptics
1. broad spectrum anitbiotics
2. not effective outside the urinary tract
3. bacteriostatic or bactericidal
4. pass in the urine allowing them to kill bacteria directly
5. common se: n/v, diarrhea
-
nitrofurantoin (macrodantin)
1. therapeutic class: antibiotics
2. indication: acute uti or uti prevention
3. se: gi, respiratory, peripherally neuropathy, low blood cells, dizziness, headache, drowsiness, photosensitivity
4. Contraindications: renal impairment, history of jaundice related to gallbladder disease, peripheral neuropathy, pregnancy >38 weeks breastfeeding.
-
nitrofurantoin (macrodantin) considerations
1. take with food or milks to minimize gi upset
2. complete the full course and take capsules whole
3. report gi, respiratory, neuropathy symptoms, fatigue, bursining, and infections
4. liquid suspension causes tooth staining: dilute in milk or juice, rinse mouth
4. do not take with antacids
5. causses brownish urine. urine color change is not dangerous.
-
Was the medications effective?
1. symptoms of uti resloved
2. negative urine cultures
-
phenazopyridine (Pyridium)
1. urinary angalgesic
2. indications: dysuria
3. se: n/v, diarrhea, headache and rash, red-orange body fluids
4. contraindications: liver or renal impairment, breastfeeding
5. changes in urine color are not harmful
6. compatible with antimicrobial therapy
7. therapy should not exceed 2 days
-
benign prostatic hypertrophy (BPH)
1. symptoms: frequency, hesitancy, urgency, and nocturia.
2. bladder does not empty with each void
3. men over 60
-
Drug categories for BPH
1. 5-Alpha reductase inhibitor: shirnk prostate by preventing hormonal changes, 6-12 months to be effective, finasteride (propecia)
2. Alpha-adrenergic receptor antagonists: relaxes smooth muscle in the neck of the bladder and prostate, results up to 2-4 weeks, tamsulosin (flomax)
-
finasteride (proscar)
1. 5-alpha reductase inhibitor
2. indicaiton: bph
3. te: shrinks prostate to increase flow of urine
4. se: decreased libido and reduced ejaculate volume, gynecomastia
5. contradicinations: females, children and pregnancy,
6. oral tablets, taken with or without food and can crush
7. women of childbearing age should not handle medication
-
Tamsulosin (flomax)
1. alpha-adrenergic receptor antagonist
2. indications: benign prostatic hypertrophy (bph)
3. Te: increase in urine flow. decrease urgency, frequency, and nocturia
4. SE: bradycardia, dizziness, headaches, hypotension, altered ejaculations', retrograde ejaculation's
5. contraindications: women, children, concurrent with Viagra
6. interaction: concurrent use of antihypertensive medications
7. monitor bp and hr
8. take 30 mins after a meal, swallow whole, do not crush or chew.

