-
Give examples of the body's first, second and third lines of defense.
First: skin, mucus, saliva
Second: phagocytosis (and the cells associated with it), inflammation, interferons
Third: antibodies and lymphocytes after exposure of specific substances
-
Vasodilation ___ blood flow.
Vasodilation increases blood flow.
-
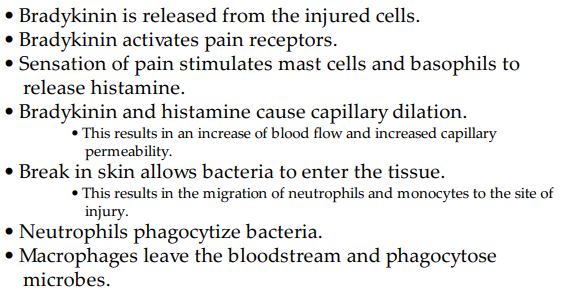
List the steps of the inflammation response.
1. Injury
2. Release of chemical mediators
3. Vasodilation
4. Increased capillary permeability
5. Leukocytes move to site of injury
6. Phagocytosis - removal of debris
-
What kind of defense mechanism is inflammation?
It's a normal, nonspecific defense mechanism.
-
What are the cardinal signs of inflammation?
- redness (from increased blood flow)
- pain (pressure of fluid on the nerves)
- heat (from increased blood flow)
- swelling (edema)
- immobility from loss of function (if the cells lack nutrients, or the swelling is causing too much damage)
OR PRISH
-
What are the steps of inflammation?
-
Name some ways chemical mediators might affect blood vessels and nerves in the damaged area.
- vasodilation (to allow lots of wbcs to go to injured site)
- hyperemia (^blood flow, causes redness)
- ^capillary permeability
- chemotaxis (migration of cells, microbes)
-
What is exudate?
Interstitial fluid in the inflamed area.
-
What are the different characteristics of exudate?
Serous: watery, from allergic reactions or burns.
Fibrinous: thick and sticky, have a high fibrin content.
Purulent: think, yellow-green colour, usually indicates infection, often known as pus.
-
What are the systemic effects of inflammation?
- mild fever (pyrexia)
- malaise (feeling of unwell)
- fatigue
- headache
- anorexia (loss of appetite)
-
What are the characteristics of chronic inflammation?
- less swelling
- ^ in lymphocytes, macrophages and fibroblasts
- formation of scar tissue
-
What is a potential complication of chronic inflammation?
- deep ulcer
-
What is an NSAID, and give some examples.
It's a Non-Steroidal Anti-Inflammatory Drug, it reduces inflammation, pain and fever.
- Aspirin
- ibuprofen
- Advil
- Motrin
-
What are some first-aid measures that can be used to treat inflammation?
R-rest
I-ice (constricts blood flow which reduces swelling)
C-compression
E-elevation
-
What are the 3 types of healing? Describe them.
1. Resolution: No open wound, quick healing.
2. Regeneration: Deeper wounds and heals by replacing the damaged ones. Ex. damage to the epithelium, but not necessarily an open wound.
3. Replacement: An open wound that is filled and formed with connective tissue and fills in the damaged cells when they are unable to undergo mitosis. Forms scar tissue.
- First Intention; wound is clean and manually closed by someone.
- Second Intention; wound is left to heal on its own, bigger scar tissue and more inflammation.
-
What are the 4 steps in the healing process?
1. Hemostasis: formation of a blood clot in the area.
2. Inflammation: inflammation develops in the area, and foreign material are removed by wbcs.
3. Proliferation of new tissues: formed from granulation tissue, epithelial cells, fibroblasts and collagen.
4. Maturation: cross linking and shortening of the collagen fibers create a tight, strong scar.
-
What are some factors promoting healing?
- youth
- clean, undisturbed wound
- good nutrition
- no infection or further trauma to the site
-
What are some factors delaying healing?
- advanced age
- anemia
- poor nutrition, dehydration
- other disorders like diabetes, cancer
-
Describe the process of healing.

-
What are some complications that can occur during scar formation?
1. Loss of function
2. Contractures and obstructions: scar tissue tightening which may result in restricted movement.
3. Adhesions: Bands of scar tissue joining two surfaces that are normally separated.
4. Hypertrophic scar tissue: overgrowth of fibrous tissue due to excess collagen deposits.
5. Ulceration: blood supply restricted around the scar.
-
What is a burn?
An injury to the body causing acute inflammation and tissue destruction.
-
ANY burn injury causes an inflammatory response. True or false?
True, it also causes major fluid shifts, edema, and a decrease in blood volume.
-
Describe first, second, third and fourth degree burns.
First Degree: superficial, damages the epidermis but will quickly without scar tissue.
Second Degree: partial thickness will be applied to trauma site, a destruction of the epidermis and part of the dermis.
Third/fourth Degree: destruction of all skin layers, and in 4th degree burns, often underlying tissue. Area is charred, edema, painless at the direct site but pain persists around the burn.
-
Name some complications that may occur from burns.
- shock (because of hypovolemia)
- respiratory problems (from the inhalation of toxic fumes)
- pain
- infection (depending on the severity, bacteria can easily penetrate the skin)
- increased metabolic needs (due to the damage done to the body, to heal it increases it's metabolic needs)
-
What is diapedesis?
The migration of cells, particularly leukocytes to the site of inflammation.
-
How can infection occur in inflamed tissue?
Microbes can invade the skin where it's damaged and where blood supply is low; some can even resist phagocytosis and exudate is a good medium for bacterial growth.
-
Skeletal muscle spasms or muscle contractions may be initiated by inflammation. True or false?
True. In fact if a spasm is strong enough it can force the bone out of joints of normal alignment, increasing the pressure on the nerves, thus increasing the pain.
-
Of these drugs, which is not an NSAID: Advil, Tylenol, Aspirin and Motrin.
Tylenol
-
Which would heal more rapidly, a surgical incision in which the edges have been stapled closely together or a large, jagged tear in the skin and subcutaneous tissue? Why?
Healing by first intention aka with the surgical incision. Because the wound heals from the bottom down upwards, and by having the surface stapled, we're doing a little bit of the work that would normally be already done later on. Meaning that it'll heal faster.
-
How do you treat small superficial burns?
Using nonstick dressings.
-
Physiotherapy and occupational therapy are used for what?
To reduce the effects of scar tissue and to increase their function.
-
How does the reduction in blood flow through the burn promote infection and make an infection harder to treat once it develops?
Because not as much wbcs travel to the trauma site, therefore if a microbe enters the skin, it likely won't be fought off.

