-
What are some factors that contribute to eating disorders?
Genetic, social psychological, Family, individual, etc.
-
Family influence on ED
- history in dieting
- depression/anxiety, etc
- history of obeisity
-
Individual influence on ED
- female
- genetics
- premature birth
- low self esteem
- perfectionism
- depression/anxiety
- previous obesity
- diabetes
-
Possible triggers for EDs
- puberty
- socio-cultural pressures
- family
- pressure to achieve
- comments about weight
-
Clinical diagnosis of anorexia
- refuse to maintain body weight at 85% of expected
- intense fear of gaining weight
- disturbance in body image
- amenorrhea (absence of 3 consecutive menstrual cycles)
- restricting type or binge eating/purging type
-
Physical consequences of anorexia
• Anemia
• Low bone density
• Depression
• Amenorrhea – absence of menstruation
• Impaired immune response
• Sensitivity to cold
• Soft, thick facial hair, thinning scalp hair
• Low blood pressure
• Irregular slow heart rate, loss of muscle tissue
-
Features of anorexia
• Individuals with anorexia nervosa typically severely restrict their food intake and may exercise intensely
• Some turn to self-induced vomiting after eating
• Family members and friends often report high levels of anxiety
• People with anorexia are often “model students” or “ideal children,” but in their personal lives may experience low self-esteem, social isolation, and unhappiness
-
How common is anorexia
• Approximately 1% of young women and <0.1% of young men have anorexia nervosa
• Reported in girls as young as five and women through their forties
• It usually begins during adolescence
• People at risk tend to be overly concerned about weight and food, and many attempted weight loss/dieted early
-
Anorexia treatment
• There is no treatment that cures anorexia nervosa quickly
• The disorder takes a good deal of time and professional help to treat (often years). Ongoing therapy is important for continued recovery.
• Treating the disorder is difficult because few with anorexia believe their weight needs to be increased
-
Anorexia treatment programs
Treatment programs focus on:
– Normalizing eating and exercise behaviors
– Nutritional health and body weight
– Psychological counseling for self-esteem
– Attitudes about body weight and shape
– Antidepressant or other medications
– Family therapy
-
Success of anorexia treatment
Complete success in 25-50% (depending on the study) and partially successful in others
-
Clinical Diagnosis of Bulimia Nervosa
- Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
• Eating, in a discrete period of time (e.g., a 2 hour period), an amount of food that is definitely larger than what most people would eat during a similar period of time and under similar circumstances.
• Lack of control over eating during the episode (e.g., a feeling that you cannot stop eating, or control what or how much you are eating).
- Recurrent inappropriate compensatory behavior to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise.
- The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for three months.
- Self-evaluation is unduly influenced by body shape and weight
-
Bulimia nervosa
• Bulimia nervosa occurs in 1-3% of young women and 0.5% of young men.
• Bulimia nervosa often starts with voluntary dieting to lose weight and at some point voluntary control over the dieting is lost.
• People feel compelled to engage in binge eating and vomiting
• The behaviors become cyclic, food binges are followed by guilt and/or depression, purging, and dieting
• Once a food binge starts, it is hard to stop
-
Is anorexia or bulimia more common?
Bulimia!
-
Features of Bulimia Nervosa
• Unlike those with anorexia nervosa, people with bulimia usually are not underweight or emaciated
• They tend to be normal weight or overweight
• Bulimia nervosa is common among athletes
-
Causes of Bulimia Nervosa
Exact cause not known with certainty
• Depression
• Feast-famine cycles: fasts and restrained eating (purposeful restriction in food to control weight) may cause feelings of deprivation that trigger binge
• Abnormal mechanisms controlling food intake
*A way for a person with bulimia to feel more in control over their lives
-
Treatment of bulimia nervosa
• Nutrition and counseling to break feast/famine cycles
• Eating regular meals
• Psychological counseling to improve self-esteem and attitudes toward body weight and shape
• Antidepressants may be useful
• Full recovery of women is higher than for anorexia
• Most women with bulimia achieve partial recovery
• 1/3 relapse to bingeing and purging within seven years
-
Binge-Eating Disorder
• Individuals are likely to have overweight or obesity, ⅓ are male
• Individuals eat several thousand calories’ worth of food during a solitary binge (within 2 hrs), feel a lack of control over the binges, and experience distress or depression after the binges occur
• People with binge-eating disorder do not vomit, use laxatives, fast, or exercise excessively in
an attempt to control weight gain = no compensatory behavior(s)
• Must have binges once a week over six months to be diagnosed
-
Binge eating episodes associated with 3 (or more) of the following:
1. Eating much more rapidly than normal
2. Eating until uncomfortably full
3. Eating large amounts when not physically hungry
4. Eating alone because of feeling embarrassed by quantity of food being consumed
5. Feeling disgusted with self, depressed or guilty
-
Binge-Eating Disorder populations
• 9-30% of people in weight-control programs and 30-90% of individuals with obesity have binge-eating disorder
• Condition is far less common (2 to 5%) in the general population
-
Binge-Eating disorder causes
• Stress, depression, anger, anxiety, and other negative emotions prompt episodes
• Binge eating disorder may be related to genetic mutation that impairs normal eating behavior
– MC4R gene mutation in 5% of individuals with the disorder
-
Binge-Eating Disorder Treatment
• Treatment focuses on disordered eating and underlying psychological issues
• Persons will be asked to record food intake and note feelings, circumstances, and thoughts related to each eating event
– Information identifies circumstances that prompt binge eating and alternative behaviors to prevent it
-
Pica
craving for non-food substances
-
What is Pica?
The word pica comes from the Latin word for magpie, a bird known for its unusual eating habits.
- clay or dirt (geophagia)
- ice cubes (pagophagia) - one case study 10kg
- purified starch (amylophagia)
-
Where do we see pica?
• Largely found in children and pregnant women
• Direct or indirect cause or symptom of iron deficiency anemia
-
Eating disorder resources
• Information and services for eating disorders are available
• Services delivered by health care teams specializing and experienced
• Primary care physician, dietitian, or nurse practitioner is good start to the process
• Reliable sources for eating disorders, support groups, and treatment:
– Eating Disorder Support Network of Alberta https://edsna.ca
– Alberta Health Services https://www.albertahealthservices.ca/findhealth/service.aspx?Id=1080429&facilityid=1002752
– UCalgary Students Union Wellness Centre https://www.ucalgary.ca/wellness-services/services/mental-health-services
-
Is enriched wheat flower or whole grain whole wheat flower better?
Whole grain whole wheat flower
-
What are the two major types of carbohydrates?
complex = good: vegetables, oats, whole grain bread, fruit, potatoes, etc.
simple = bad: donuts, pop, gummies, cookies, chocolate, white bread, fries, etc.
-
Simple carbohydrate Monosaccharides
- Monosaccharides
• Glucose (blood sugar or dextrose), Fructose (fruit sugar), Galactose
• Most abundant and nutritionally relevant is glucose
• Only monosaccharides are absorbed into bloodstream
-
Simple carbohydrate Disaccharides
- Disaccharides
• Two monosaccharides joined by a covalent bond
-
Simple sugars
refers to monosaccharides and/or disaccharides
- Few are made by animals; most are plant sourced
-
Health risk of simple carbohydrates (simple sugars)
Health Risk: rapidly absorbed into blood stream, increased insulin resistance and inflammation
-
Disaccharides
sucrose, maltose and lactose
• Sucrose (cane sugar, beet sugar) is the most widely used natural sweetener
- Glucose + Fructose
• Maltose is formed from the partial breakdown of starch & is often used in malt beverages (e.g. beer = barley is malted, maltose is formed, bacteria ferment the maltose and make alcohol)
- Glucose + Glucose
• Lactose is “milk sugar,” one of the only animal sugars besides glucose
- Glucose + Galactose
-
Complex carbohydrates Oligosaccharides
- Oligosaccharides (most ~3 monosaccharide units)
• Short chains of monosaccharides joined by bonds that cannot be broken by human enzymes (i.e. they are a fiber source)
• Fructans and galacto-oligosaccharides
• Garlic, onions, wheat, artichokes, beans, lentils, chickpeas, inulin
-
Complex carbohydrates Polysaccharies
- Polysaccharides (up to 1000’s)
• Long chains of monosaccharides joined by bonds (some digestible and some not) •
• Include glycogen, starch, and cellulose
• Potato, rice, pasta, corn, cereal, bread, apple peel, seeds, nuts
-
The 3 primary nutritional polysaccharides:
Starch – Energy storage in plants (digestible)
Glycogen – Energy storage in animals (digestible)
Cellulose – Provides structure in plants (non-digestible)
-
What polysaccharides are digestible vs. non-digestible
- Starch and glycogen are digestible = glucose polymers bonded with α glycosidic bonds that CAN be broken down by enzymes
- Cellulose is non-digestible = connected via β glycosidic bonds that can NOT be broken down by human enzymes
-
Fiber in the Intestine
*Fiber is important to our health because of what happens to it in the colon.
COLON: Bacterial enzymes can break down fiber to form short chain fatty acids and gas as a byproduct.
*Fiber feeds our gut microbiota.
-
Gut microbiota in disease
Brain: anxiety, depression, parkinson's
Intestinal: crohn's, ulcerative colitis, IBS
Metabolism: obesity, type 2 diabetes, fatty liver disease
Pathogens: clostridium difficile infection
-
What diet causes microbiota symbiosis vs. dysbiosis
Symbiosis: high fiber, whole natural foods
Dysbiosis: processed foods, low fiber
-
Why eat whole grain foods?
- In a grain of wheat, the outer bran layer is a rich source of dietary fiber
- The germ contains protein, unsaturated fats, thiamin, niacin, riboflavin, iron, and other nutrients
- The bran and germ are removed in the refining process (i.e. making white flour)
- The endosperm primarily contains starch, the storage form of glucose in plants = white flour
-
Soluble fiber
- Soluble fiber is good because it benefits health in several ways
- It slows down glucose absorption, thereby lowering peak blood levels of glucose, and reduces fat and cholesterol absorption
- Found in oats, barley, fruit pulp, peas, beans, citrus fruits, strawberries and psyllium - Lower calories than digestible carbohydrates (1-2 kcal/g typical)
-
Insoluble fiber
- Insoluble fiber is good because it benefits health in several ways
• Moves bulk through gut, controls gut pH, removes toxic waste, prevents constipation
- Found in vegetables, wheat bran, whole grains, flax seed, popcorn, corn bran, seeds, nuts, apple peel
-
Macronutrient effects on blood glucose
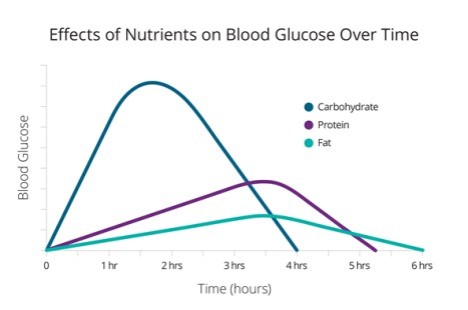
1. Blood glucose rises when you eat.
2. High blood glucose stimulates pancreas to release insulin.
3. Insulin stimulates uptake of glucose into cells and storage as glycogen in liver and muscle. It also helps convert excess glucose into fat stores.
4. As body cells use glucose, blood levels decline.
5. Low blood glucose stimulates pancreas to release glucagon.
6. Glucagon stimulates liver cells to break down glycogen and release glucose into blood.
7. Blood glucose begins to rise
-
Added sugars
- Major sources of simple sugars in most diets are added during processing of food
- Labels contain information on total sugars per serving but do not distinguish between naturally occurring and added sugars yet. ‘Added sugars’ add calories without adding nutrients
*food labels must now have all sugars together
-
The Bad Side of Sugar
- Tooth decay
- Empty calories (calories without nutrients)
- Often mixed with fats in sweets
• Limit sweet and sticky foods; replace them with vegetables and fruits
• Overall quality of diet decreases when sugar intake increases
-
Sugar alternatives
- Alcohol sugars (~2.6 kcal/g)
• Xylitol
• Mannitol
• Sorbitol
- Used in chewing gum and other candies and foods
- Can be used to mask the unpleasant aftertaste of some artificial sweeteners
- Are not well absorbed in the gut; large amounts can cause diarrhea
-
Stevia
- Herbal Alternatives: Stevia (GRAS – generally recognized as safe - status)
- Initial studies with crude whole leave extracts of stevia = reproductive, renal and cardiovascular toxicity
- Purified stevioside preparations show no toxic effects
- In 2012 Health Canada approved its use in foods
-
Aspartame (one of the most consumed)
- A dipeptide (2 amino acids = aspartic acid + phenylalanine)
- Digestion releases methanol (10%), aspartic acid (40%) and phenylalanine (50%)
- Methanol converted to formaldehyde and then formic acid
- 200 times sweeter than sucrose (sugar)
- Products containing it bear a “contains phenylalanine” label for people with PKU (phenylketonuria)
- “Nutrasweet” & “Equal”
- Acceptable daily intake 40 mg/kg BW
- Not compatible with high temperatures (> 30ºC)
-
Sucralose
- Made from sugar = chlorinated sugar (body can't break apart)
- 600x sweeter than sugar
- Safe when heated
- “Splenda”
-
Acesulfame K
- Often used in combination with other artificial sweeteners
- Stable at high temperatures
-
Saccharin
- Discovered in 1879 by accident by chemist working on coal tar derivatives
- 300x sweeter than sucrose
- Banned in Canada in 1977 due to bladder cancer fears, returned to market once it was discovered the mechanism by which it caused cancer in rats is not present in humans
*NOT GOOD
-
Maternal Artificial Sweetener Consumption During Pregnancy
• Reduced insulin sensitivity
• Altered mesolimbic reward pathway in the brain (promotes food seeking behavior)
• Altered gut microbiota composition and function
• Offspring had 25% higher fat mass at 3 weeks of age
-
Mechanism of sugar and tooth decay
* sugar is sole food for bacteria --> produce acid
* bacteria form sticky white plaque
* acid is produced by bacteria for 20 min after sugar is eaten
-
Promoters of sugar and tooth decay
- increased frequency of sticky foods
- acidic beverages
- excessive cleaning/polishing of teeth
- nursing bottle syndrom
-
Protective foods of tooth decay
- cheese (incr. pH of plaque - decr. acidity)
- protein (with calcium it strengthens enamel)
- low calorie sweeteners such as sorbitol, mannitol, xylitol (stimulate saliva)
-
Fluoride and dental health
* promote remineralization of eroded enamel
* water, toothpastes, dental rinses
* excess leads to fluorosis or “mottled” enamel during tooth development
* cosmetic condition that can only form in children ≤8 years when permanent teeth are developing
-
Fluoride in drinking water
- 2011 City of Calgary voted to remove fluoride from water supply
- 2016 study compared rates of tooth decay in grade 2 children from Calgary (removed fluoride) and Edmonton (kept fluoride)
• Compared 2004/2005 and 2013/2014 data
• Both cities had high rates of tooth decay but was increasing more rapidly in Calgary - 2021 study shows gap is widening: “Of the approximately 2,600 Grade 2 students in each city who took part in the study, 55.1% of Edmonton participants had one or more cavities in their baby teeth. In comparison, the number was 64.8% of Calgary children.”
- November 2021 City of Calgary voted to reintroduce fluoride into water supply (set to start by September 2024
-
Gestational diabetes
Only during pregnancy
-
Type 1 (insulin-dependent)
- Typically diagnosed before 40, abruptly
- Treatment is with insulin, diet and exercise
-
Type 2 (non-insulin dependent)
- Lifestyle related
- Treatment is weight reduction
-
Poorly controlled, untreated diabetes produces:
- Blurred vision
- Frequent urination
- Weight loss (usually Type 1)
- Increased susceptibility to infection
- Slow healing sores
- Extreme hunger and thirst
-
Long term, (non-controlled) diabetes may cause:
- Heart disease and stroke (type 2 commonly)
- Kidney damage (nephropathy)
- Blindness (retinopathy)
- Nerve damage (neuropathy)
- Loss of limbs due to poor circulation
- Alzheimer’s disease
-
Insulin
- Insulin is a pancreatic hormone
- Reduces blood glucose
- Facilitates passage of glucose into cells
- Low/no insulin (T1D) starves cells
- Cells can also starve if cell membranes become insulin-resistant (T2D)
-
Gestational diabetes population
- 5 to 6% of women develop gestational diabetes
- Indigenous and Black, women with obesity, women over 35 years, and women with low physical activity have greater risk
- Women with gestational diabetes are insulin resistant
- Control blood glucose levels with an individualized diet and exercise plan
-
Gestational diabetes consequence on the baby
- Infants of women with diabetes may have increased body fat at birth & have blood glucose control problems after delivery
• At greater risk for diabetes later in life
• 6 to 20% will have a physical abnormality that may threaten survival or a high quality of life
• e.g. cleft palate, club foot, heart defects
- Some women require daily insulin injections for blood glucose control
-
Gestational diabetes testing/appearance
- Gestational diabetes disappears after delivery
- But type 2 diabetes may appear later in life in the mom
- Exercise, maintenance of normal weight, and a healthy diet reduce the risk that diabetes will return
-
Type 1 Diabetes
- Type 1 diabetes results from a deficiency of insulin
- Accounts for about 5-10% of all diabetes and is increasing yearly (2x as high as children in ’80s)
- Diagnosis of type 1 peaks around the ages of 11 to 12 years and usually occurs before age 40
- Autoimmune disease that destroys pancreatic beta-cells that produces insulin
-
Type 1 Diabetes factors
- Breastfeeding for first four months may protect infants against type 1 diabetes
- Environmental factors are more important than genetics in type 1 diabetes
• Candidates have included: early exposure to cow’s milk proteins; vitamin D deficiency; early exposure to gluten; certain viruses (rubella, rotavirus, mumps, cytomegalovirus, enteroviruses); gut microbiota
-
Immune-Mediated Diseases and Microbiota (e.g. Finland)
- Finland has the highest rate of type 1 diabetes in the world. Across the border in the Karelia region of Russia, 8 times lower incidence.
- Share similar genes and language but vastly different hygiene/microbial exposure (especially antibiotic use in early life).
- Certain bacteria, when present in early life can strengthen immune response and prevent type 1 diabetes.
- Estonia, once much lower, is now catching up with Finland.
-
Managing Type 1 Diabetes
- Insulin
• Injections
• Pump
• Islet transplant
- Diet
- Exercise
-
Type 2 Diabetes
- Occurs in individuals with overweight or obesity and a sedentary lifestyle
- Most common in people over 40 – but increasingly seen in young children
- Increasingly common in children and adolescents
- Strong genetic component
-
Factors of type 2 diabetes
- Runs in families (Black, Hispanic, Indigenous and Asian); associated with ”apple” obesity
- Individuals with type 2 diabetes are insulin-resistant
- Type 2 diabetes can be managed with diet & exercise - most of the time
- If not, there are 8 different classes of diabetes medications that can be prescribed to manage diabetes
-
Prediabetes and Insulin Resistance
- Elevated fasting blood glucose levels below the cut-off point used to diagnose type 2 diabetes
- 20% of Canadian adults, and 314 million people worldwide have prediabetes - Prediabetes is a major risk factor for type 2 diabetes
-
Common risk factors for insulin resistance
- Obesity
- Low levels of physical activity
- Genetics
-
Insulin Resistance
- When blood glucose levels become high, the pancreas secretes more insulin to keep glucose levels under control
- Pancreas becomes exhausted from over-work and insulin production slows or stops
- When fasting blood glucose levels reach 7 mmol/L or higher, type 2 diabetes has developed
-
Managing Type 2 Diabetes with Diet and Exercise
- Weight loss alone significantly improves blood glucose control
- Proper diets are crucial
• Complex carbohydrates including whole-grain breads and cereals, and other high-fiber foods, vegetables, fruits, low-fat milk and meats, and fish
• Unsaturated fats
• Regular meals and snacks
• Protein at every meal (particularly bedtime)
-
Sugar Intake and Diabetes
- High intakes if simple sugars do NOT directly cause diabetes - but can contribute to obesity
- Sugar does not have to be eliminated from the diet of individuals with diabetes, but total carbs should be reduced
- High-sugar diets increase blood triglyceride levels and the risk of heart disease in people with metabolic syndrome
-
Glycemic Index
- foods that elevate blood glucose require more insulin to live glucose into cells
- foods that affect blood glucose are given a glycemic index value
• Blood glucose elevation caused by 50g of a good, compared to the elevation caused by eating 50g of glucose
- low-glycemic index foods decrease triglyceride levels and insulin needs in type 2 diabetes
-
What is high GI
70-100
-
What is medium GI
56-69
-
What is low GI
55 or lower
-
What has high GI
Jelly beans, donut
-
What has very low GI
Hummus, milk, yogurt
-
Rice differences in GI
Sticky rice: 86
Brown rice: lower
-
Alcohol is...
Both a food and a drug:
- a food because it is made from carbohydrate
- a drug because it modifies various body functions
-
How does alcohol form?
Alcohol forms when yeast ferments sugars in different foods.
• Wine - sugar in grapes
• Beer - sugar in malted barley
• Cider - sugar in apples
• Vodka - sugar in potatoes
-
Alcohol at high vs. low dose
- At low dose, acts as stimulant (e.g. increase talkativeness)
- At high dose, depresses the central nervous system (e.g. drowsiness, respiratory depression
-
Alcohol in beverages
• beer (4-6% alcohol) == 355 ml can
• wine (8-14% alcohol) ~just over half a cup == 148 ml
• distilled liquor (many around 40%) == 44 ml shot
*know percent and volume!!
-
Alcohol in the body
• requires no digestion
• 10% absorbed directly across empty stomach wall
• reach brain in 1 minute
-
Positive alcohol effects
- 1 (women) – 2 (men) standard drinks per day
- Moderate consumption (may) protect from heart disease in men over 45 and women over 55
- Increases high-density lipoprotein (HDL), the “good cholesterol” (take cholesterol out of blood stream)
- May protect against Type 2 diabetes (in nondiabetics) and ischemic stroke (but not hemorrhagic)
- Wine consumption was found to be cardioprotective but not beer (Circulation 2002;105:2836–44). More recent research, wine and beer but not spirits
-
Red wine positive pigment
- Red wine’s pigments act as an antioxidant and inhibit blood clot formation
• Purple grape juice also works
- May decrease the ability of LDL cholesterol to stick to plaques in the arteries
-
At what point do we see more negative alcohol side effects?
- Heavy drinking, ~5 or more drinks/day threatens drinkers’ health and those of others
- Alcoholism – chronic and progressive disease
-
Alcohol poisoning symptoms
- Passing out
- Semi-conscious
- Cold, pale, or bluish skin
- Vomiting while sleeping
- Slow or irregular breathing
- Seizures
*functional: drink so much body can hide it
-
Breast cancer and alcohol
Breast cancer risk increases with increased alcohol consumption
-
What else can alcohol cause
High blood pressure, stroke, heart attack, cirrhosis, throat and stomach cancer, breast and bladder cancer, vitamin and mineral deficiencies, fetal alcohol syndrome, accidents, drownings, violent behavior, etc...
-
Taking risks when you've been drinking can lead to:
- getting hurt or even death—alcohol-related injury is the major cause of death in teens and young adults
- sexual risk-taking—this includes unwanted sex, unplanned pregnancy, and sexually transmitted infections
- suicide and self-harm—higher risk in teens and young adults who drink heavily or often
-
Fetal Alcohol Spectrum Disorder (FASD)
- Children born to women who drink during pregnancy can develop fetal alcohol syndrome.
- Children with FASD experience impaired growth and mental development.
- May have distinct FASD associated facial features although this is only present in about 10% of individuals with FASD
-
Fetal Alcohol Spectrum Disorder STATS
- 4% of Canadians have FASD
- 2.5× more prevalent than autism spectrum disorder
- ~11% of Canadian mothers report consuming alcohol during pregnancy (3% report alcohol binges)
- Mental health disorders are seen in >90% of individuals with FASD, compared to 20% of general population (depression and anxiety most common)
- There is no cure for FASD, but research shows that early intervention can improve a child’s development.
-
Alcohol Intake and Diet Quality
- 7 calories/gram in pure alcohol
- For adults who drink, 3-9% of calories come from alcohol, and 50% of calories come from alcohol in heavy drinkers
- As alcohol consumption from alcohol-containing beverages increases, the quality of the diet generally decreases
- Empty calories – calories but no nutrients

